Abstract
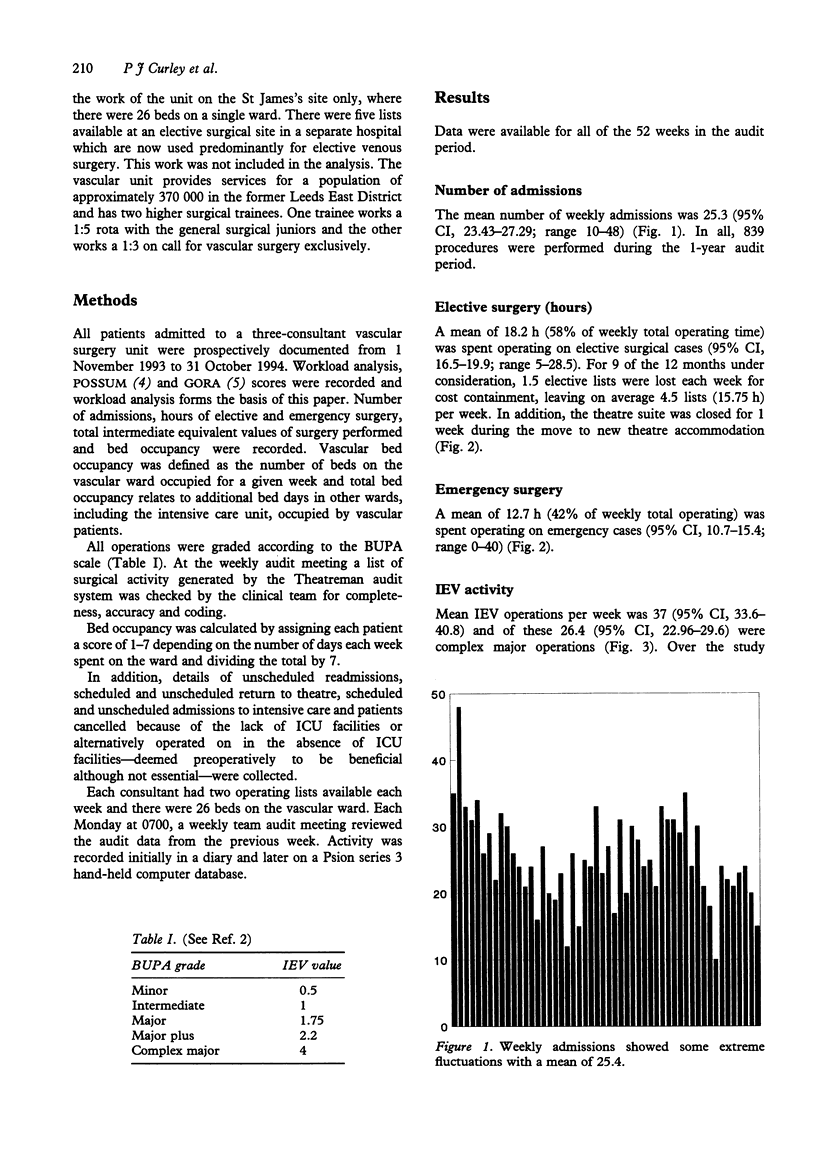
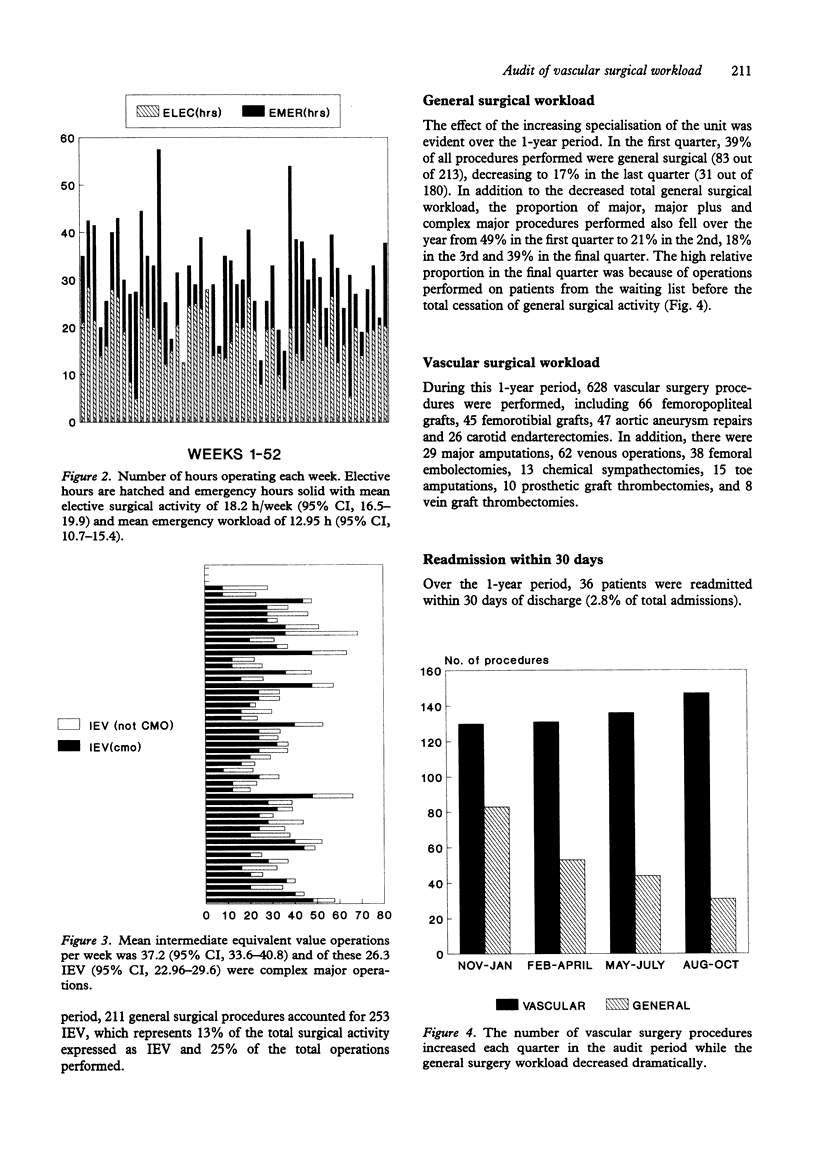
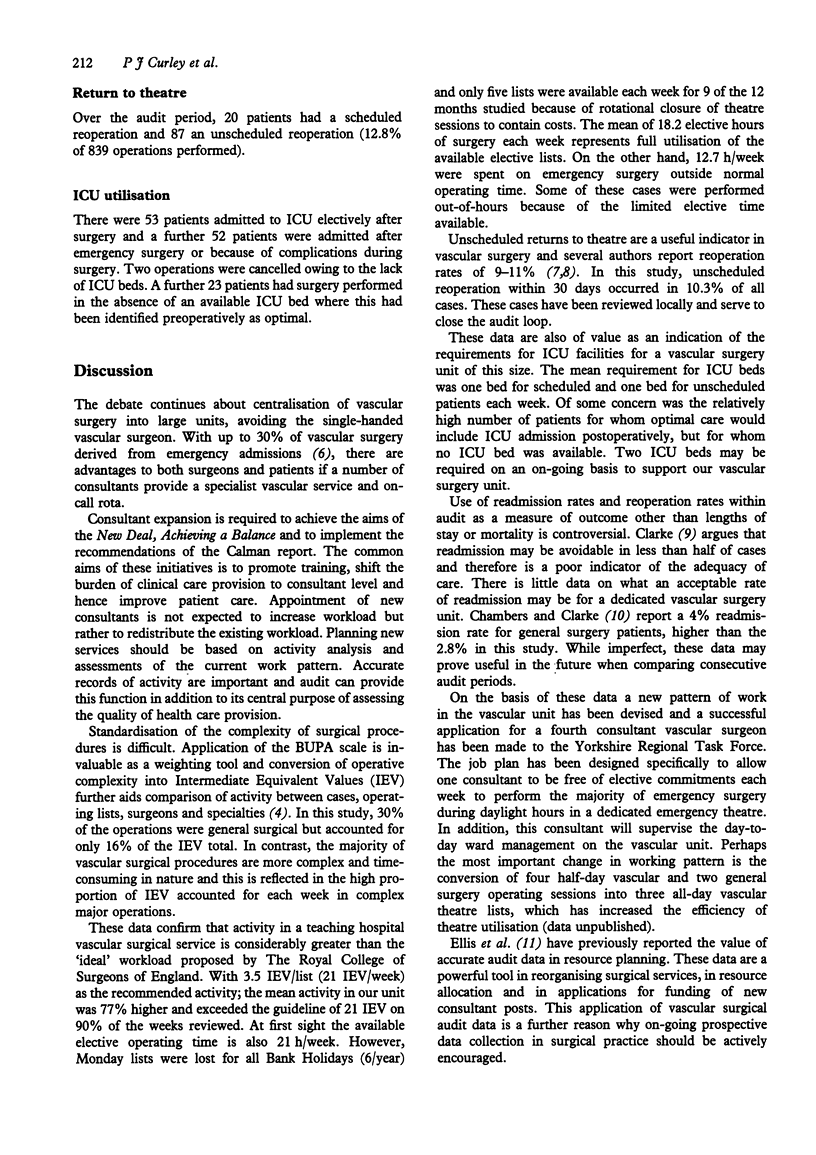
The power of surgical audit lies in the ability to clearly record complications and to compare case mix from year to year and between centres in order to compare results. In addition, accurate data about surgical activity is vital for the development of new services. We have analysed 52 weeks of activity in a developing pure vascular surgical service and compared activity against the recommendations previously published for consultant surgical workload. During the 12-month period the mean number of admissions per week was 25.3 (95% CI, 23.43-27.29). Mean elective surgical activity was 18.2 h/week (95% CI, 16.5-19.9) and mean emergency workload 12.7 h (95% CI, 10.7-15.4). Mean intermediate equivalent value (IEV) operations per week was 37 (95% CI, 33.6-40.8) and of these 26.4 IEV (95% CI, 22.96-29.6) were complex major operations. Finally, the mean bed occupancy of vascular patients on the unit was 23.3 (95% CI, 21.15-24.97).
The recommendations for surgical activity are 3.5 IEV/list. In our unit this would equate to 21 IEV/week compared with 37.2 in our practice. This data forms the basis of a powerful bid for increased consultant manpower and theatre resources.
Surgical audit is time-consuming and should be consultant led, but the benefits are tangible and the data generated can be used to support bids for resource re-allocation.
Keywords: Audit, Vascular surgery, Workload
Full text
PDF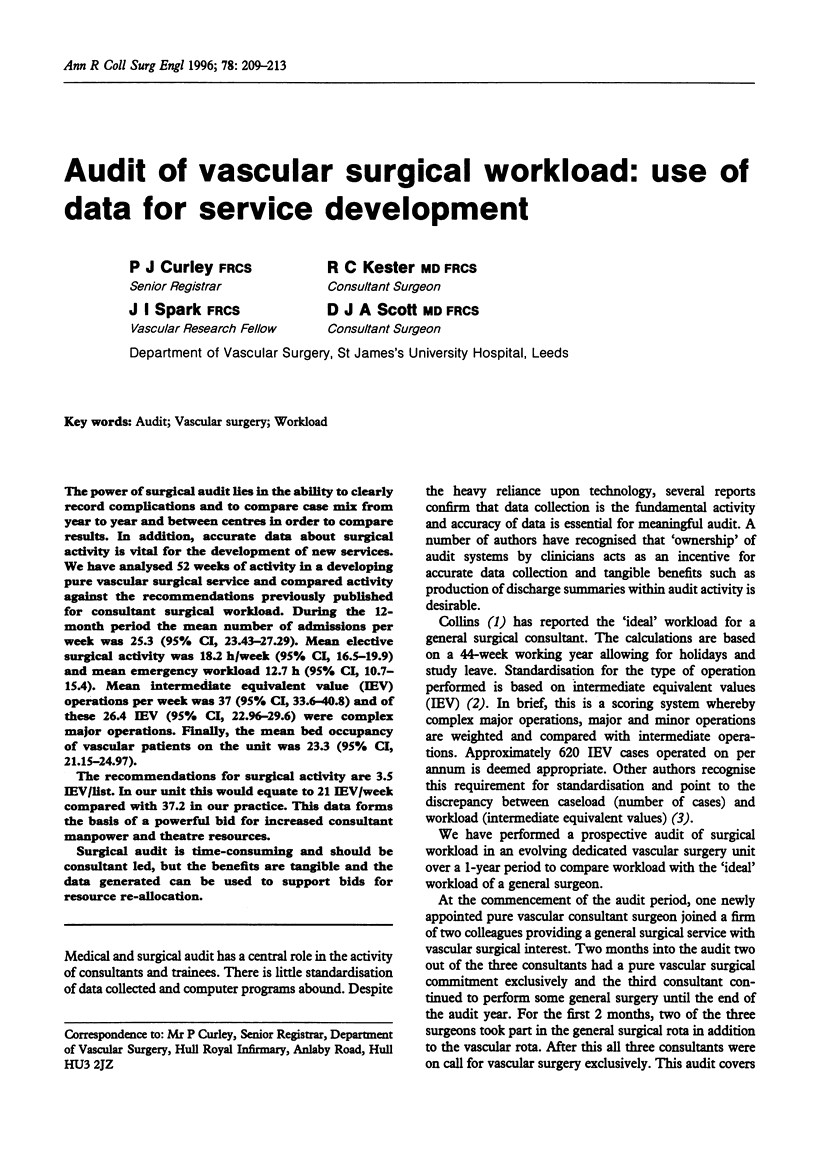

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chambers M., Clarke A. Measuring readmission rates. BMJ. 1990 Nov 17;301(6761):1134–1136. doi: 10.1136/bmj.301.6761.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke A. Are readmissions avoidable? BMJ. 1990 Nov 17;301(6761):1136–1138. doi: 10.1136/bmj.301.6761.1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins C. Providing the ideal surgical service. Ann R Coll Surg Engl. 1992 Sep;74(5 Suppl):126–129. [PMC free article] [PubMed] [Google Scholar]
- Collins C. Recommended values for use in surgical audit and surgical workload analysis. Ann R Coll Surg Engl. 1991 Sep;73(5 Suppl):94–94. [PubMed] [Google Scholar]
- Copeland G. P., Edwards P., Wilcox A., Wake P. N., Harris P. L. GORA: a scoring system for the quantification of risk of graft occlusion. Ann R Coll Surg Engl. 1994 Mar;76(2):132–135. [PMC free article] [PubMed] [Google Scholar]
- Copeland G. P., Jones D., Wilcox A., Harris P. L. Comparative vascular audit using the POSSUM scoring system. Ann R Coll Surg Engl. 1993 May;75(3):175–177. [PMC free article] [PubMed] [Google Scholar]
- Earnshaw J. J., Hayward J. K., Horrocks M., Baird R. N. The importance of vascular surgical audit to surgeons, patients and purchasers. Eur J Vasc Surg. 1992 Sep;6(5):540–544. doi: 10.1016/s0950-821x(05)80630-9. [DOI] [PubMed] [Google Scholar]
- Ellis B. W., Rivett R. C., Dudley H. A. Extending the use of clinical audit data: a resource planning model. BMJ. 1990 Jul 21;301(6744):159–162. doi: 10.1136/bmj.301.6744.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones S. M., Collins C. D. Caseload or workload? Scoring complexity of operative procedures as a means of analysing workload. BMJ. 1990 Aug 11;301(6747):324–325. doi: 10.1136/bmj.301.6747.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng R. L., Davies A. H., Magee T. R., Tennant S., Horrocks M., Baird R. N. Early reoperation rates after arterial surgery. Eur J Vasc Surg. 1994 Jan;8(1):78–82. doi: 10.1016/s0950-821x(05)80125-2. [DOI] [PubMed] [Google Scholar]


