Abstract
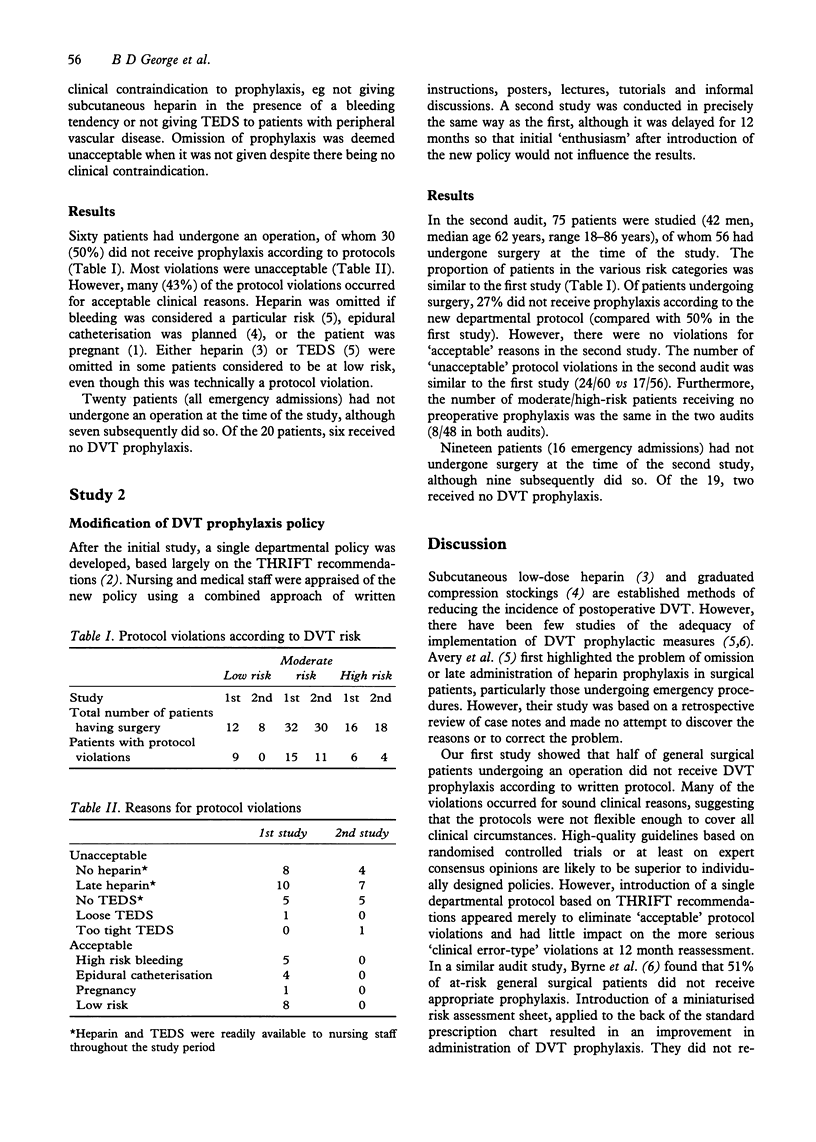
This study aimed to determine how closely deep vein thrombosis (DVT) prophylactic policies are adhered to in routine general surgical practice, to identify reasons for policy violations and to assess the effects of policy modification. Eight adult patients, sixty of whom had undergone an operation, under the care of six general surgeons, each with their own written DVT protocol, were studied on one weekday. Thirty patients (50%) did not receive DVT prophylaxis according to the policy of the relevant consultant. Most violations occurred for unacceptable reasons, mainly starting low-dose subcutaneous heparin or using thromboembolic stockings postoperatively. However, 43% of protocol violations occurred for acceptable clinical reasons. Following the initial study, a uniform departmental DVT prophylaxis policy was introduced. Nursing and medical staff were thoroughly appraised of the new policy. In a repeat study of 75 patients 1 year later, there were 15 protocol violations among 58 patients who had undergone an operation (27%). However, there were no violations for acceptable reasons. The number of unacceptable protocol violations in the two studies was similar (24/60 and 17/56). The number of patients at moderate or high DVT risk who received no preoperative prophylaxis was the same in both studies (8/48 in both audits). DVT protocol violations are common in routine general surgical practice. Policy modification and unification results in fewer violations, but made little impact on the level of thromboprophylactic care.
Full text
PDF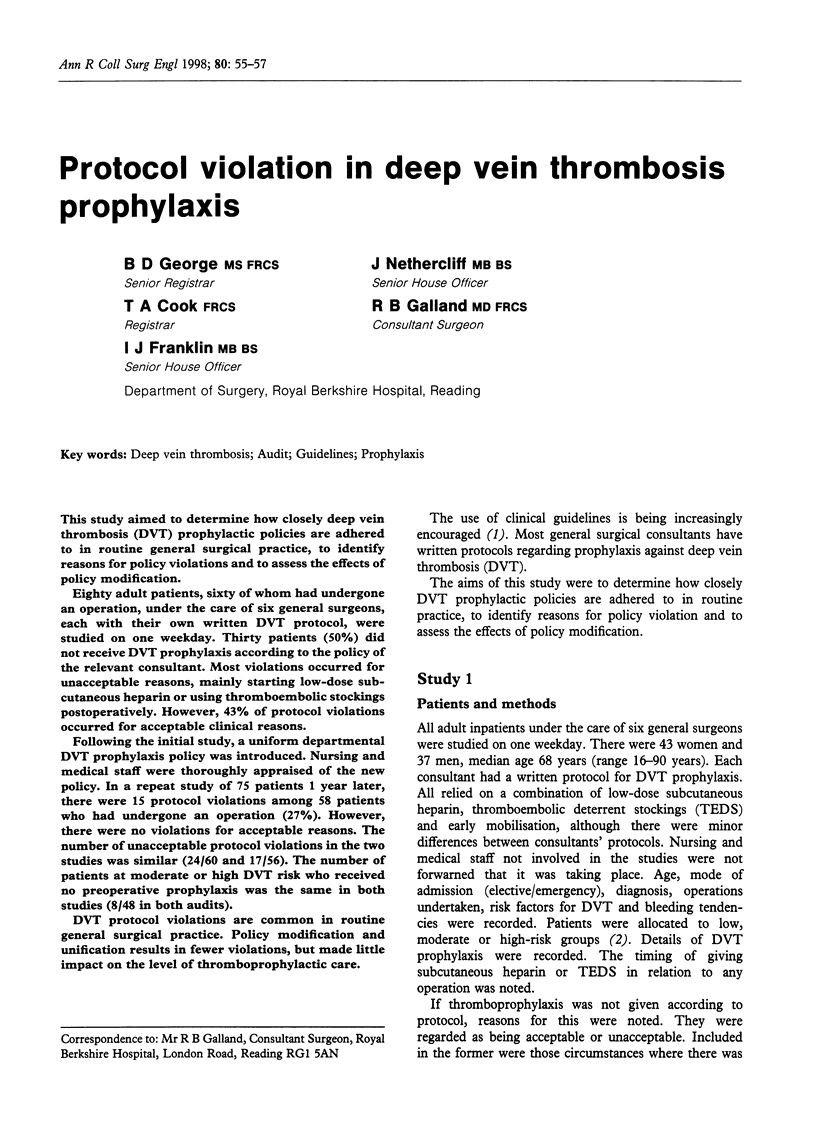

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Allan A., Williams J. T., Bolton J. P., Le Quesne L. P. The use of graduated compression stockings in the prevention of postoperative deep vein thrombosis. Br J Surg. 1983 Mar;70(3):172–174. doi: 10.1002/bjs.1800700311. [DOI] [PubMed] [Google Scholar]
- Avery C. M., Jamieson N. V., Calne R. Y. Administration of heparin and antibiotic prophylaxis. Br J Surg. 1994 Jul;81(7):987–988. doi: 10.1002/bjs.1800810719. [DOI] [PubMed] [Google Scholar]
- Byrne G. J., McCarthy M. J., Silverman S. H. Improving uptake of prophylaxis for venous thromboembolism in general surgical patients using prospective audit. BMJ. 1996 Oct 12;313(7062):917–917. doi: 10.1136/bmj.313.7062.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins R., Scrimgeour A., Yusuf S., Peto R. Reduction in fatal pulmonary embolism and venous thrombosis by perioperative administration of subcutaneous heparin. Overview of results of randomized trials in general, orthopedic, and urologic surgery. N Engl J Med. 1988 May 5;318(18):1162–1173. doi: 10.1056/NEJM198805053181805. [DOI] [PubMed] [Google Scholar]
- Grimshaw J. M., Russell I. T. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993 Nov 27;342(8883):1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- Hurwitz B. Clinical guidelines and the law. BMJ. 1995 Dec 9;311(7019):1517–1518. doi: 10.1136/bmj.311.7019.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]


