Abstract
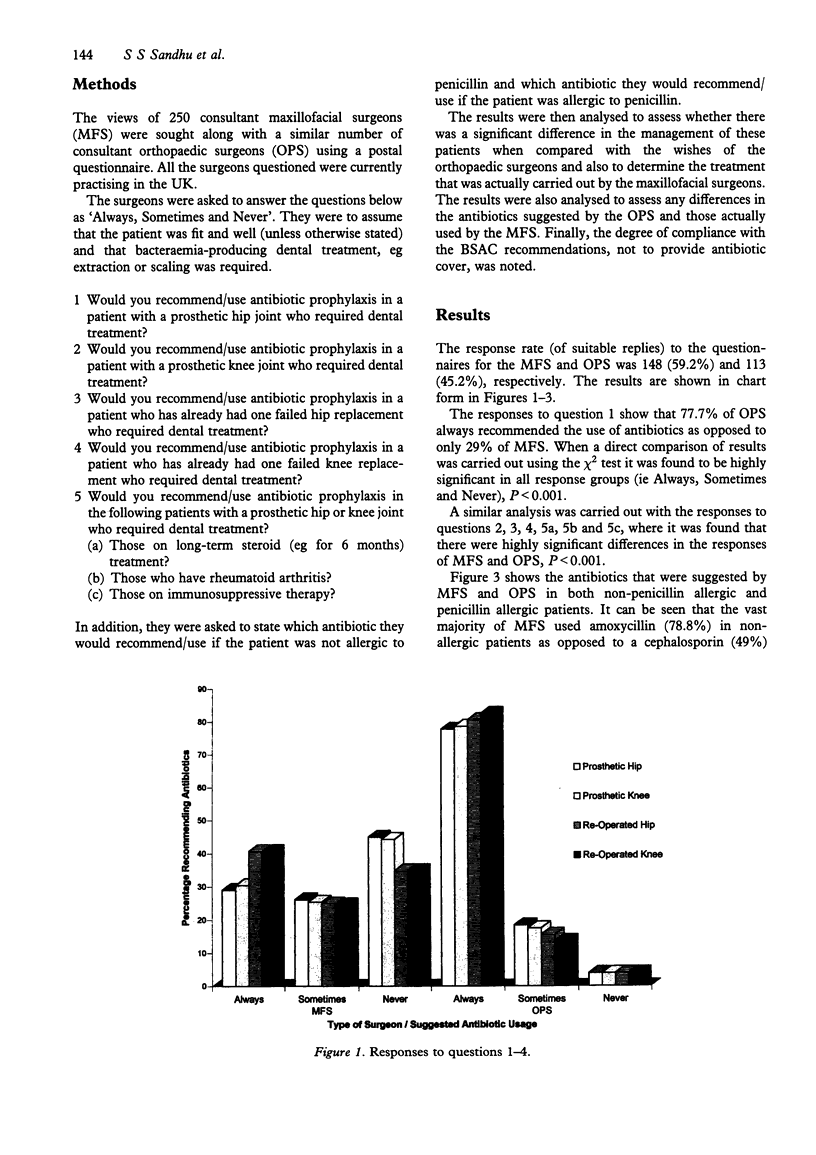
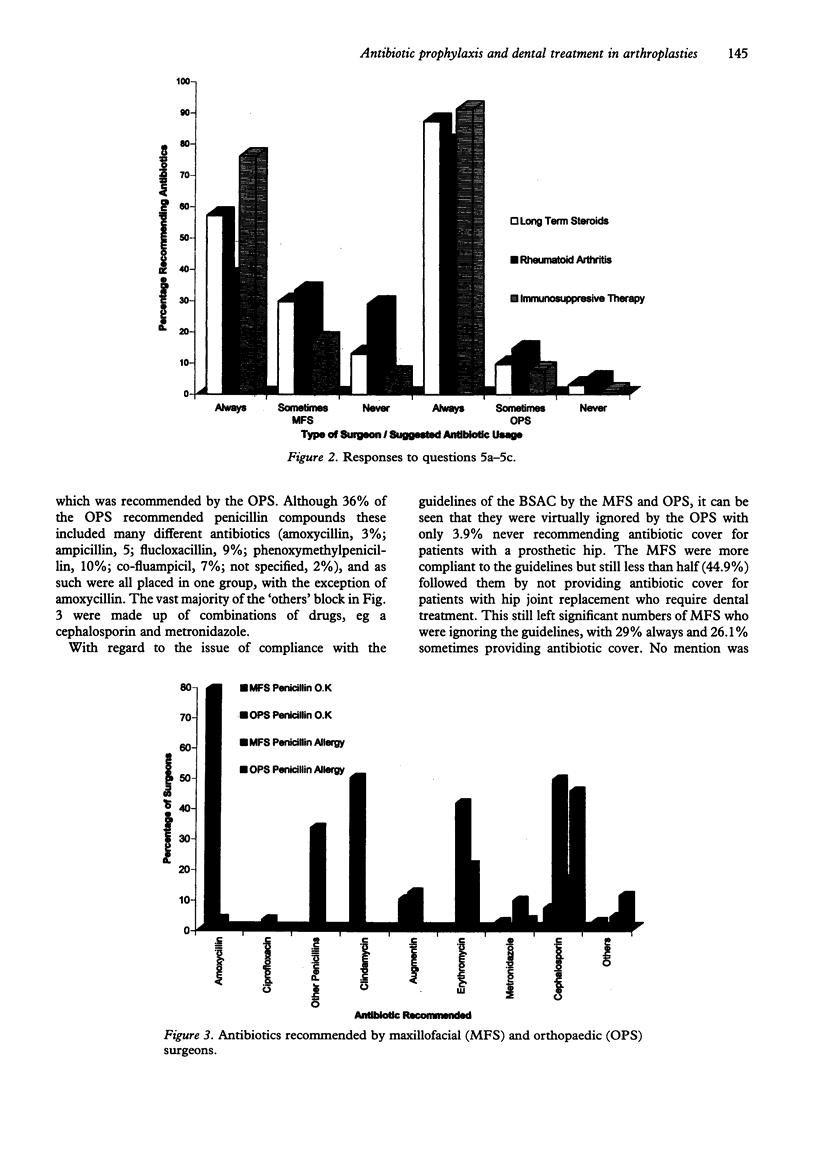
The role of antibiotic prophylaxis in patients with prosthetic joints who require dental treatment is controversial. A Working Party of the British Society for Antimicrobial Chemotherapy (BSAC) recently suggested that there was no evidence to support the use of antibiotic prophylaxis in these patients. The purpose of this study was to determine how closely these recommendations were being followed by maxillofacial surgeons (MFS), and to see if there was any consensus on the management of these patients between MFS and orthopaedic surgeons (OPS). With the aid of a postal questionnaire, the opinions of 250 consultant MFS and OPS were sought, response rates were 148 (59.2%) and 113 (41.2%), respectively. Of the OPS, 77.7% always recommended the use of antibiotic prophylaxis as opposed to only 29% of MFS. There were also wide differences in opinion with regard to the antibiotic that should be used in these patients, with the majority of OPS suggesting a cephalosporin, although this may not be the most efficacious antibiotic for oral streptococci. We conclude that this important matter seems to be far from satisfactorily resolved and that further cooperation between the specialties is required to produce guidelines for the safe and effective management of this increasing group of patients.
Full text
PDF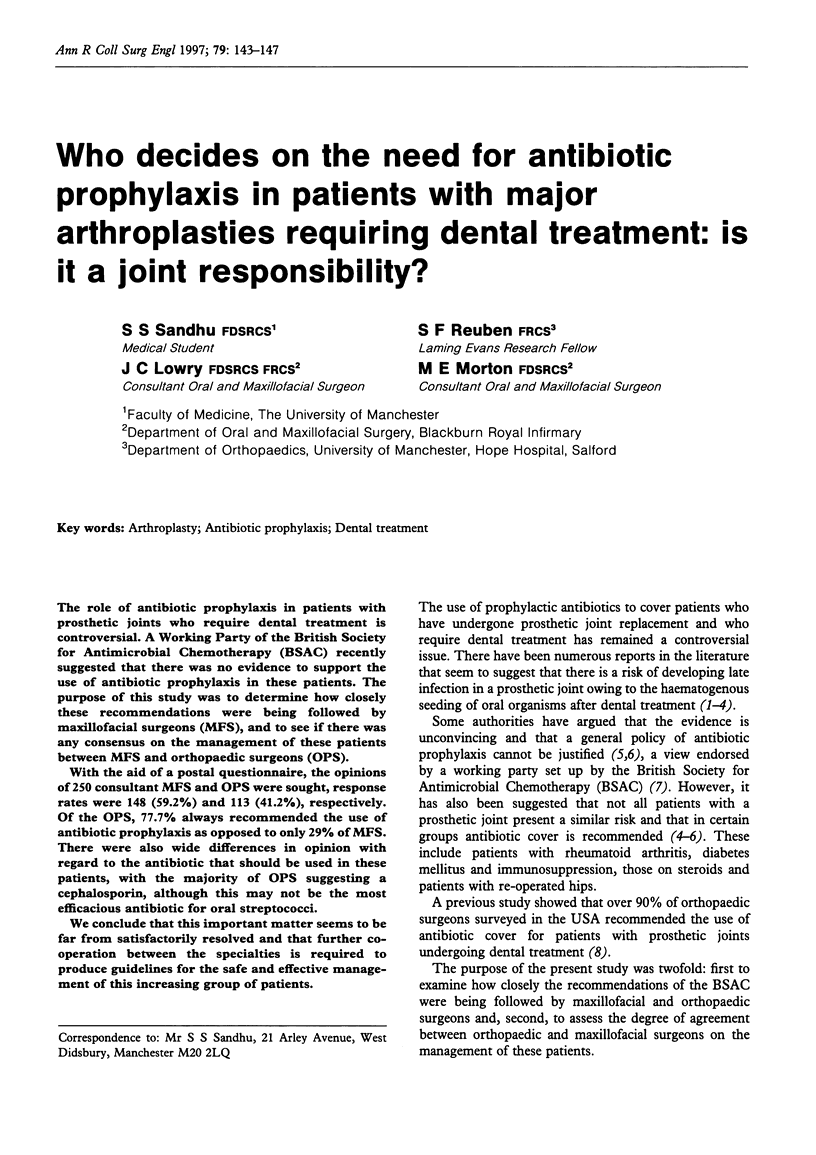

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ahlberg A., Carlsson A. S., Lindberg L. Hematogenous infection in total joint replacement. Clin Orthop Relat Res. 1978 Nov-Dec;(137):69–75. [PubMed] [Google Scholar]
- Bartzokas C. A., Johnson R., Jane M., Martin M. V., Pearce P. K., Saw Y. Relation between mouth and haematogenous infection in total joint replacements. BMJ. 1994 Aug 20;309(6953):506–508. doi: 10.1136/bmj.309.6953.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayliss R., Clarke C., Oakley C. M., Somerville W., Whitfield A. G., Young S. E. The microbiology and pathogenesis of infective endocarditis. Br Heart J. 1983 Dec;50(6):513–519. doi: 10.1136/hrt.50.6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckingham J. K., Gould I. M., Tervitt G., Williams S. Prevention of endocarditis: communication between doctors and dentists. Br Dent J. 1992 Jun 6;172(11):414–415. doi: 10.1038/sj.bdj.4807904. [DOI] [PubMed] [Google Scholar]
- Cruess R. L., Bickel W. S., vonKessler K. L. Infections in total hips secondary to a primary source elsewhere. Clin Orthop Relat Res. 1975 Jan-Feb;(106):99–101. doi: 10.1097/00003086-197501000-00013. [DOI] [PubMed] [Google Scholar]
- Durack D. T., Petersdorf R. G. Chemotherapy of experimental streptococcal endocarditis. I. Comparison of commonly recommended prophylactic regimens. J Clin Invest. 1973 Mar;52(3):592–598. doi: 10.1172/JCI107220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field E. A., Martin M. V. Prophylactic antibiotics for patients with artificial joints undergoing oral and dental surgery: necessary or not? Br J Oral Maxillofac Surg. 1991 Oct;29(5):341–346. doi: 10.1016/0266-4356(91)90124-n. [DOI] [PubMed] [Google Scholar]
- Grant A., Hoddinott C. Joint replacement, dental surgery, and antibiotic prophylaxis. BMJ. 1992 Apr 11;304(6832):959–959. doi: 10.1136/bmj.304.6832.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inman R. D., Gallegos K. V., Brause B. D., Redecha P. B., Christian C. L. Clinical and microbial features of prosthetic joint infection. Am J Med. 1984 Jul;77(1):47–53. doi: 10.1016/0002-9343(84)90434-0. [DOI] [PubMed] [Google Scholar]
- Jacobson J. J., Matthews L. S. Bacteria isolated from late prosthetic joint infections: dental treatment and chemoprophylaxis. Oral Surg Oral Med Oral Pathol. 1987 Jan;63(1):122–126. doi: 10.1016/0030-4220(87)90352-5. [DOI] [PubMed] [Google Scholar]
- Jaspers M. T., Little J. W. Prophylactic antibiotic coverage in patients with total arthroplasty: current practice. J Am Dent Assoc. 1985 Dec;111(6):943–948. doi: 10.14219/jada.archive.1985.0224. [DOI] [PubMed] [Google Scholar]
- Lidwell O. M., Elson R. A., Lowbury E. J., Whyte W., Blowers R., Stanley S. J., Lowe D. Ultraclean air and antibiotics for prevention of postoperative infection. A multicenter study of 8,052 joint replacement operations. Acta Orthop Scand. 1987 Feb;58(1):4–13. doi: 10.3109/17453678709146334. [DOI] [PubMed] [Google Scholar]
- Little J. W. The need for antibiotic coverage for dental treatment of patients with joint replacements. Oral Surg Oral Med Oral Pathol. 1983 Jan;55(1):20–23. doi: 10.1016/0030-4220(83)90300-6. [DOI] [PubMed] [Google Scholar]
- Maderazo E. G., Judson S., Pasternak H. Late infections of total joint prostheses. A review and recommendations for prevention. Clin Orthop Relat Res. 1988 Apr;(229):131–142. [PubMed] [Google Scholar]
- Mason J. C., Dollery C. T., So A., Cohen J., Bloom S. R., Bulpitt C., Russell-Jones R., Oakley C. M. An infected prosthetic hip. Is there a role for prophylactic antibiotics? BMJ. 1992 Aug 1;305(6848):300–302. doi: 10.1136/bmj.305.6848.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M. A., Curzon M. E. The effectiveness of the yellow card warning system for paediatric cardiology patients. Community Dent Health. 1992 Dec;9(4):391–392. [PubMed] [Google Scholar]
- Sullivan P. M., Johnston R. C., Kelley S. S. Late infection after total hip replacement, caused by an oral organism after dental manipulation. A case report. J Bone Joint Surg Am. 1990 Jan;72(1):121–123. [PubMed] [Google Scholar]
- Thyne G. M., Ferguson J. W. Antibiotic prophylaxis during dental treatment in patients with prosthetic joints. J Bone Joint Surg Br. 1991 Mar;73(2):191–194. doi: 10.1302/0301-620X.73B2.2005136. [DOI] [PubMed] [Google Scholar]


