Abstract
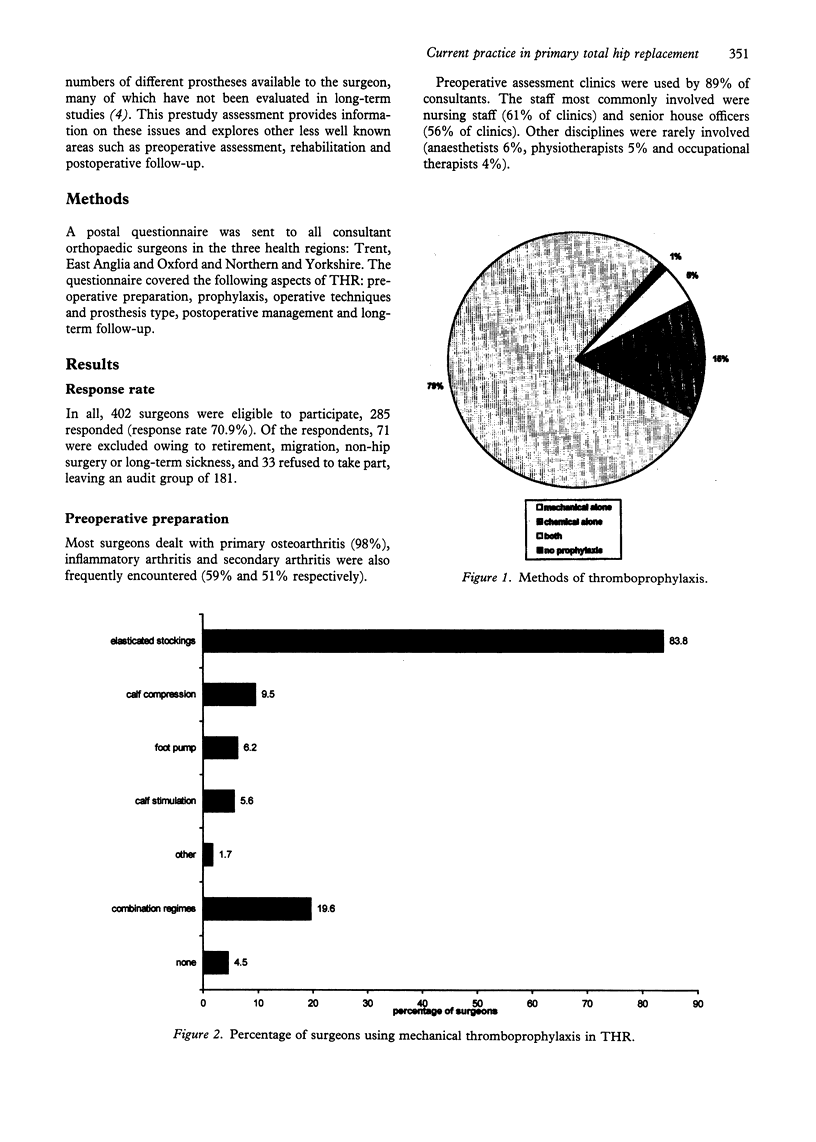
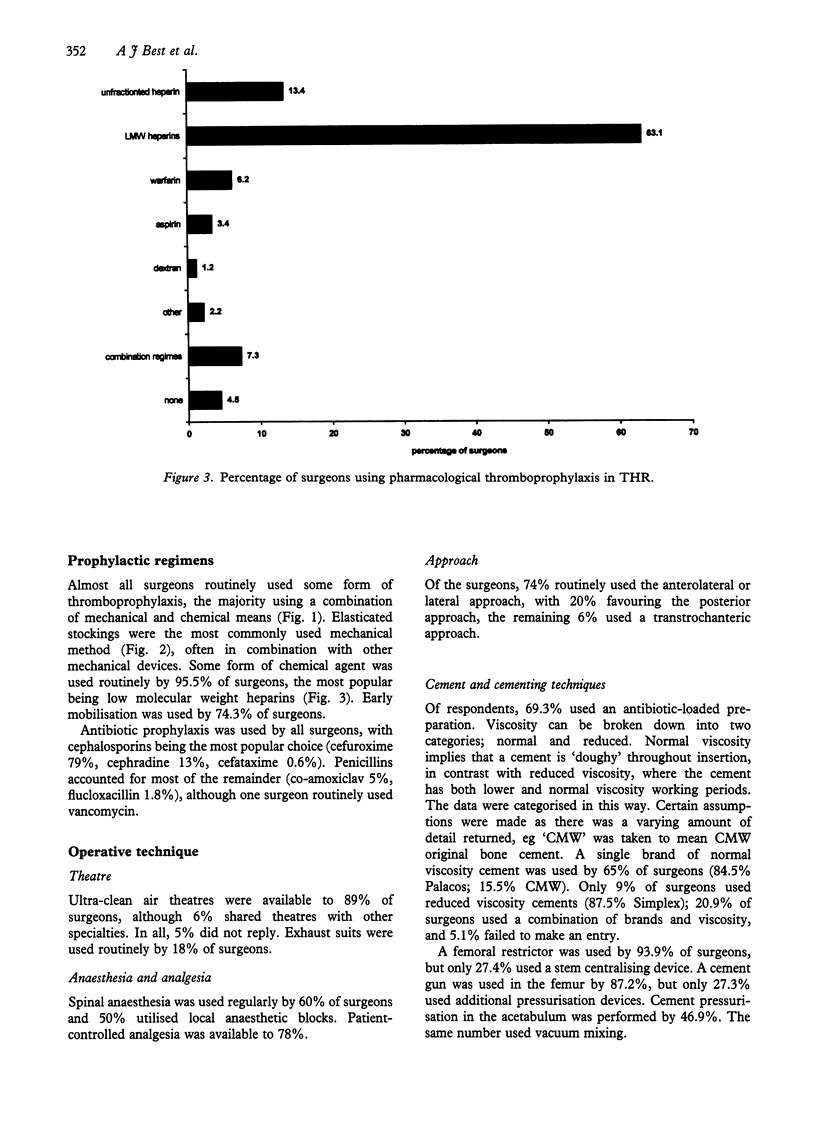
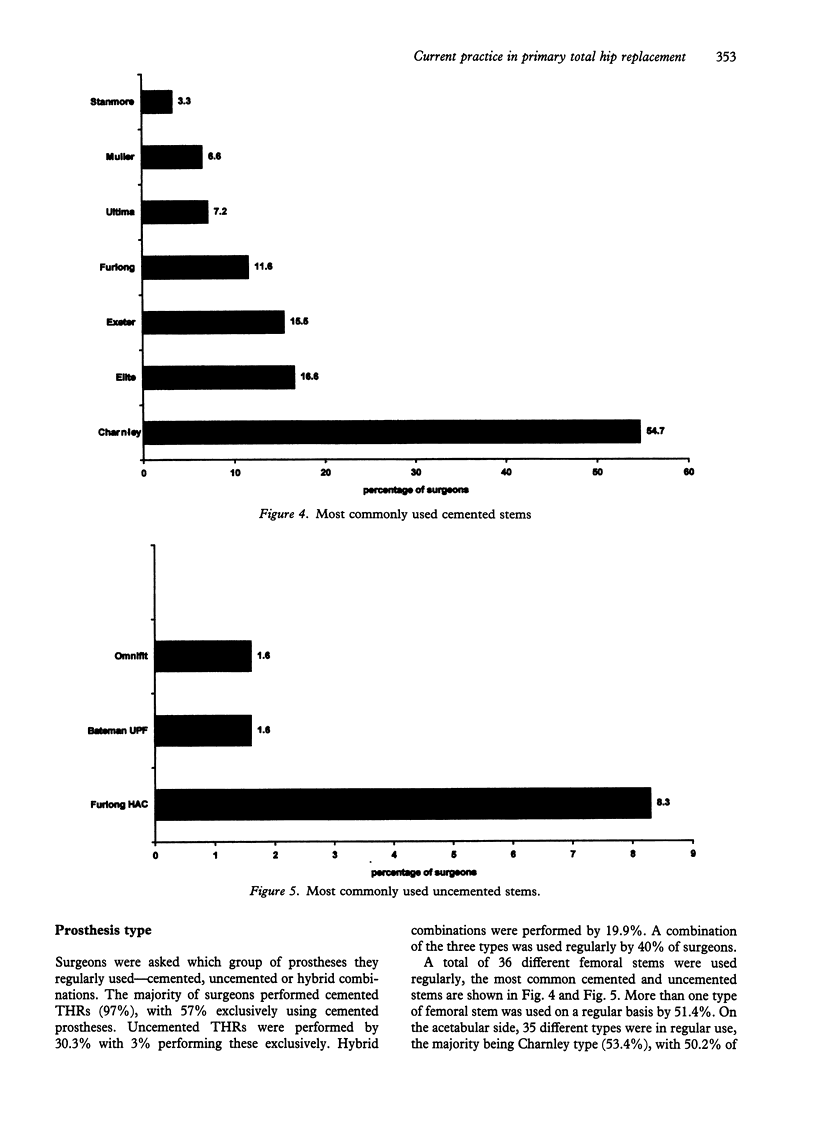
As part of the National Study of Primary Hip Replacement Outcome, 402 consultant orthopaedic surgeons from three regions were contacted by postal questionnaire which covered all aspects of total hip replacement (THR). There was a 70% response rate of which 71 did not perform hip surgery, a further 33 refused to take part, leaving 181 valid responses. Preoperative assessment clinics were used by 89% of surgeons, but anaesthetists and rehabilitation services were rarely involved at this stage. Of respondents, 99% used routine thromboprophylaxis, with 79% using a combination of mechanical and chemical methods. Of surgeons, 84% routinely used stockings, whereas 95.5% used chemical prophylaxis, 63% employed low molecular weight heparins. Theatre facilities were shared with other surgical specialties by 6% of surgeons and 18% regularly used body exhaust suits for THR. Antibiotic loaded cement was used by 69% of surgeons, the majority (65%) used a single brand of normal viscosity cement with 9% using reduced viscosity formulations. Modern cementing techniques were commonly used at least in part, 87% used a cement gun and 94% a cement restrictor for femoral cementing. On the acetabulum, 47% pressurised the cement. In all, 36 different femoral stems and 35 acetabular cups were in routine use, but the majority of surgeons (55%) used Charnley type prostheses. Of the surgeons, 57% performed only cemented THR, while 3% exclusively used uncemented THR. Of consultants, 21% followed up their patients to 5 years, the majority discharge patients within the first year. Of concern is a large proportion of surgeons using low molecular weight heparins despite a lack of evidence with regard to reducing fatal pulmonary embolism, and also the small number of surgeons using prostheses of unproven value. Third generation cementing techniques have yet to be fully adopted. The introduction of a national hip register could help to resolve some of these issues.
Full text
PDF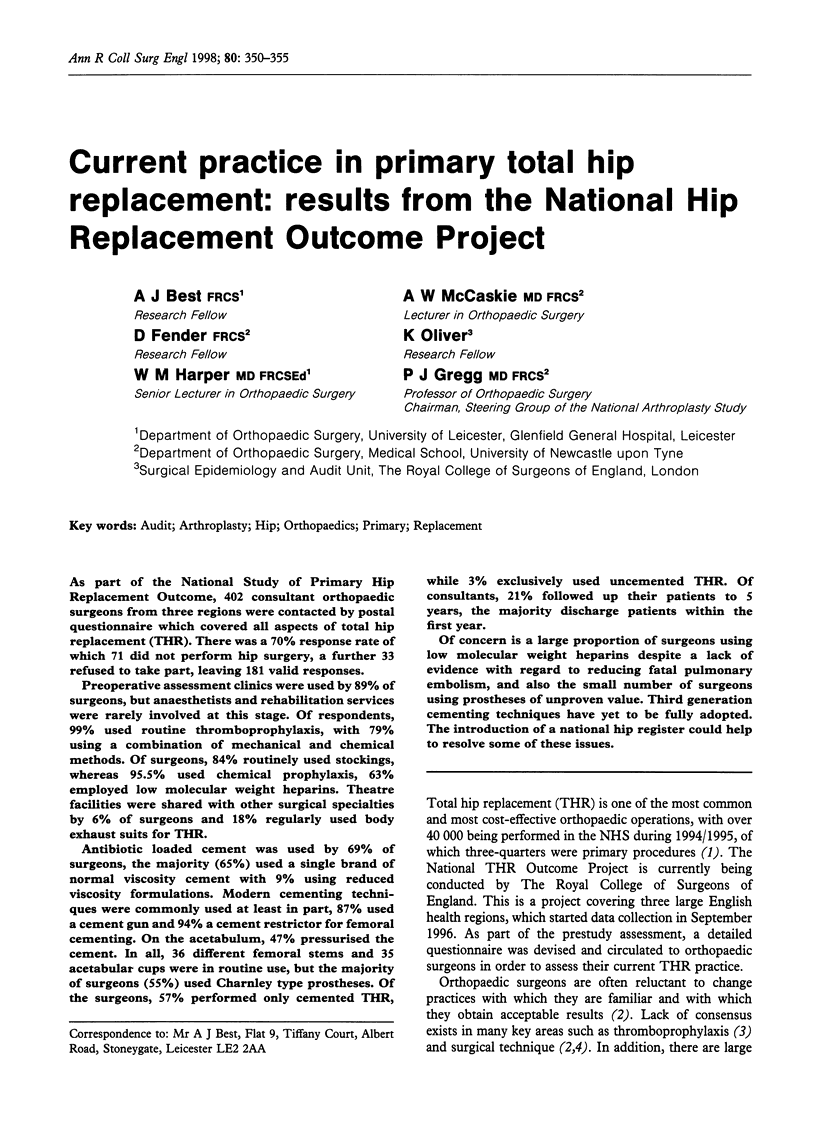
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Brenkel I. J., Clancy M. J. Total hip replacement and antithrombotic prophylaxis. Br J Hosp Med. 1989 Oct;42(4):282–284. [PubMed] [Google Scholar]
- Bulstrode C. J., Murray D. W., Carr A. J., Pynsent P. B., Carter S. R. Designer hips. BMJ. 1993 Mar 20;306(6880):732–733. doi: 10.1136/bmj.306.6880.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collis D. K., Steinhaus K. Total hip replacement without deep infection in a standard operating room. J Bone Joint Surg Am. 1976 Jun;58(4):446–450. [PubMed] [Google Scholar]
- Hashemi-Nejad A., Birch N. C., Goddard N. J. Current attitudes to cementing techniques in British hip surgery. Ann R Coll Surg Engl. 1994 Nov;76(6):396–400. [PMC free article] [PubMed] [Google Scholar]
- Hui A. C., Heras-Palou C., Dunn I., Triffitt P. D., Crozier A., Imeson J., Gregg P. J. Graded compression stockings for prevention of deep-vein thrombosis after hip and knee replacement. J Bone Joint Surg Br. 1996 Jul;78(4):550–554. [PubMed] [Google Scholar]
- Jeffery P. C., Nicolaides A. N. Graduated compression stockings in the prevention of postoperative deep vein thrombosis. Br J Surg. 1990 Apr;77(4):380–383. doi: 10.1002/bjs.1800770407. [DOI] [PubMed] [Google Scholar]
- Laverick M. D., Croal S. A., Mollan R. A. Orthopaedic surgeons and thromboprophylaxis. BMJ. 1991 Sep 7;303(6802):549–550. doi: 10.1136/bmj.303.6802.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leach W. J., Wilson N. I. Trends in infection prophylaxis in orthopaedics. J R Coll Surg Edinb. 1992 Aug;37(4):265–266. [PubMed] [Google Scholar]
- Learmonth I. D. Prevention of infection in the 1990s. Orthop Clin North Am. 1993 Oct;24(4):735–741. [PubMed] [Google Scholar]
- Lidwell O. M., Lowbury E. J., Whyte W., Blowers R., Stanley S. J., Lowe D. Infection and sepsis after operations for total hip or knee-joint replacement: influence of ultraclean air, prophylactic antibiotics and other factors. J Hyg (Lond) 1984 Dec;93(3):505–529. doi: 10.1017/s0022172400065098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaskie A. W., Gregg P. J. Femoral cementing technique: current trends and future developments. J Bone Joint Surg Br. 1994 Mar;76(2):176–177. [PubMed] [Google Scholar]
- Murray D. W., Carr A. J., Bulstrode C. J. Which primary total hip replacement? J Bone Joint Surg Br. 1995 Jul;77(4):520–527. [PubMed] [Google Scholar]
- Nasser S. Prevention and treatment of sepsis in total hip replacement surgery. Orthop Clin North Am. 1992 Apr;23(2):265–277. [PubMed] [Google Scholar]
- Newman K. J. Total hip and knee replacements: a survey of 261 hospitals in England. J R Soc Med. 1993 Sep;86(9):527–529. [PMC free article] [PubMed] [Google Scholar]
- Owen T. D., Coorsh J. The use of thromboprophylaxis in total hip replacement surgery: are the attitudes of orthopaedic surgeons changing? J R Soc Med. 1992 Nov;85(11):679–681. doi: 10.1177/014107689208501108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker-Williams J., Vickers R. Major orthopaedic surgery on the leg and thromboembolism. BMJ. 1991 Sep 7;303(6802):531–532. doi: 10.1136/bmj.303.6802.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unwin A. J., Jones J. R., Harries W. J. Current UK opinion on thromboprophylaxis in orthopaedic surgery: its use in routine total hip and knee arthroplasty. Ann R Coll Surg Engl. 1995 Sep;77(5):351–354. [PMC free article] [PubMed] [Google Scholar]
- Warwick D., Williams M. H., Bannister G. C. Death and thromboembolic disease after total hip replacement. A series of 1162 cases with no routine chemical prophylaxis. J Bone Joint Surg Br. 1995 Jan;77(1):6–10. [PubMed] [Google Scholar]


