Abstract
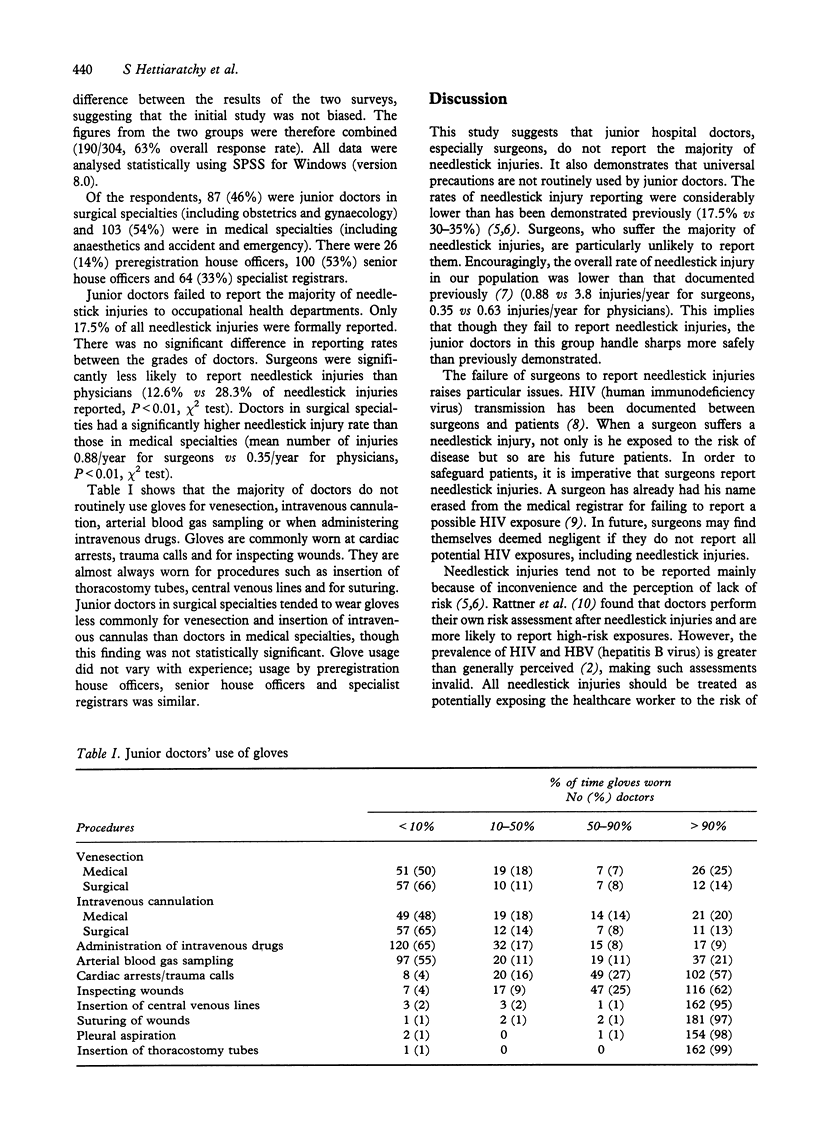
The use of gloves when conducting invasive procedures and the reporting of needlestick injuries have been strongly encouraged. Despite this, neither practice appears to be universal. In order to determine the rates of glove usage and needlestick injury reporting, we conducted a survey of junior doctors in three hospitals in the UK. Of the 190 respondents, the majority rarely wore gloves for venesection, insertion of intravenous cannulas or arterial blood gas sampling. For more major procedures (insertion of central venous lines, insertion of thoracostomy tubes, suturing) gloves were invariably worn. Only 17.5% of needlestick injuries were reported. The rates of glove usage and needlestick injury reporting were lower than previous studies have demonstrated in North America. Surgeons suffered the most needlestick injuries and were the least likely to report them. The low reporting rate may have serious implications, particularly in view of the new Government guidelines on needlestick injuries which involve HIV-infected blood. By failing to use gloves and report needlestick injuries, junior doctors, in particular surgeons, are placing themselves and patients at increased risk of blood-borne transmissible diseases.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Birnbaum D. Meaningful measurement of compliance. Infect Control Hosp Epidemiol. 1995 Jan;16(1):3–3. doi: 10.1086/646992. [DOI] [PubMed] [Google Scholar]
- Heald A. E., Ransohoff D. F. Needlestick injuries among resident physicians. J Gen Intern Med. 1990 Sep-Oct;5(5):389–393. doi: 10.1007/BF02599422. [DOI] [PubMed] [Google Scholar]
- Kaczmarek R. G., Moore R. M., Jr, McCrohan J., Arrowsmith-Lowe J. T., Caquelin C., Reynolds C., Israel E. Glove use by health care workers: results of a tristate investigation. Am J Infect Control. 1991 Oct;19(5):228–232. doi: 10.1016/s0196-6553(05)80253-6. [DOI] [PubMed] [Google Scholar]
- Marcus R., Culver D. H., Bell D. M., Srivastava P. U., Mendelson M. H., Zalenski R. J., Farber B., Fligner D., Hassett J., Quinn T. C. Risk of human immunodeficiency virus infection among emergency department workers. Am J Med. 1993 Apr;94(4):363–370. doi: 10.1016/0002-9343(93)90146-g. [DOI] [PubMed] [Google Scholar]
- Mast S. T., Woolwine J. D., Gerberding J. L. Efficacy of gloves in reducing blood volumes transferred during simulated needlestick injury. J Infect Dis. 1993 Dec;168(6):1589–1592. doi: 10.1093/infdis/168.6.1589. [DOI] [PubMed] [Google Scholar]
- Paice E., West G., Cooper R., Orton V., Scotland A. Senior house officer training: is it getting better? A questionnaire survey. BMJ. 1997 Mar 8;314(7082):719–720. doi: 10.1136/bmj.314.7082.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rattner S. L., Norman S. A., Berlin J. A. Percutaneous injuries on the "front line": a survey of housestaff and nurses. Am J Prev Med. 1994 Nov-Dec;10(6):372–377. [PubMed] [Google Scholar]
- Schinstock B., Schaffer B. Occupational exposure to HIV. Am J Med. 1992 Jan;92(1):115–116. doi: 10.1016/0002-9343(92)90033-8. [DOI] [PubMed] [Google Scholar]
- Tandberg D., Stewart K. K., Doezema D. Under-reporting of contaminated needlestick injuries in emergency health care workers. Ann Emerg Med. 1991 Jan;20(1):66–70. doi: 10.1016/s0196-0644(05)81122-9. [DOI] [PubMed] [Google Scholar]


