Abstract
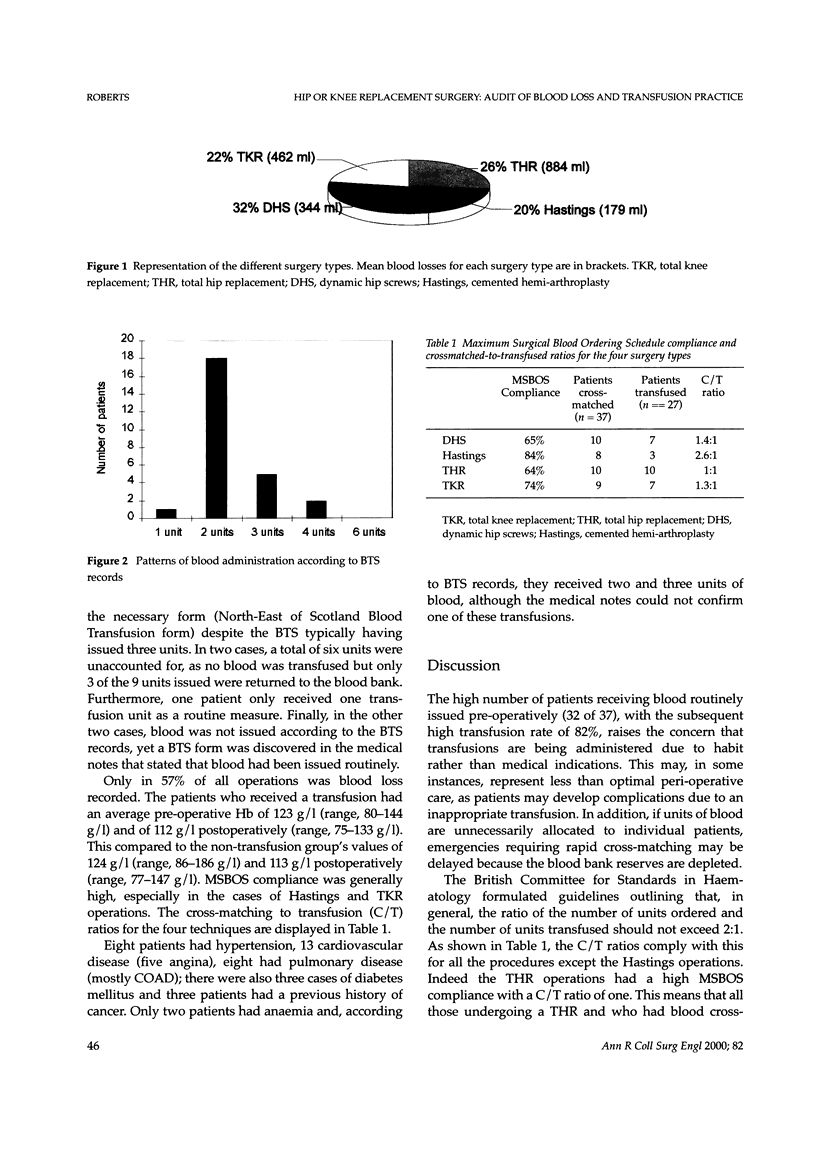
We prospectively audited peri-operative blood loss and blood transfusion practice in 42 elderly patients (mean age, 71.8 years, 68% female) undergoing hip or knee surgery in an orthopaedic unit. Only in 57% of all operations was blood loss recorded. Compliance with the Maximum Surgical Blood Ordering Schedule (MSBOS) was variable, and Cross-matching to Transfusion (C/T) ratios were low. In 86% of operations, blood had been issued pre-operatively (average three units, range = 1-61 units). Of these patients, 75% subsequently received a transfusion. In 26% of all the operations, the transfusion, although confirmed by the blood transfusion laboratory records, had not been recorded in the medical or nursing notes. The average pre-operative Hb in the transfusion group was 123 g/l (range, 80-144 g/l) and 112 g/l postoperatively and after a transfusion (range, 75-133 g/l). This compared to the non-transfusion group's value of 124 g/l (range, 86-186 g/l) and 113 g/l (range, 77-147 g/l) postoperatively. The high blood issuing and transfusion rates raise the concern that transfusions are being given in response to habit or blood availability, and not medical indications. This would imply that some patients are exposed to unnecessary risks. Furthermore, inadequate documentation of the transfusion process opens the medical profession to criticism and medical, legal and ethical complications regarding patient care. Positive improvements suggested by regular medical audit may help address these problems.
Full text
PDF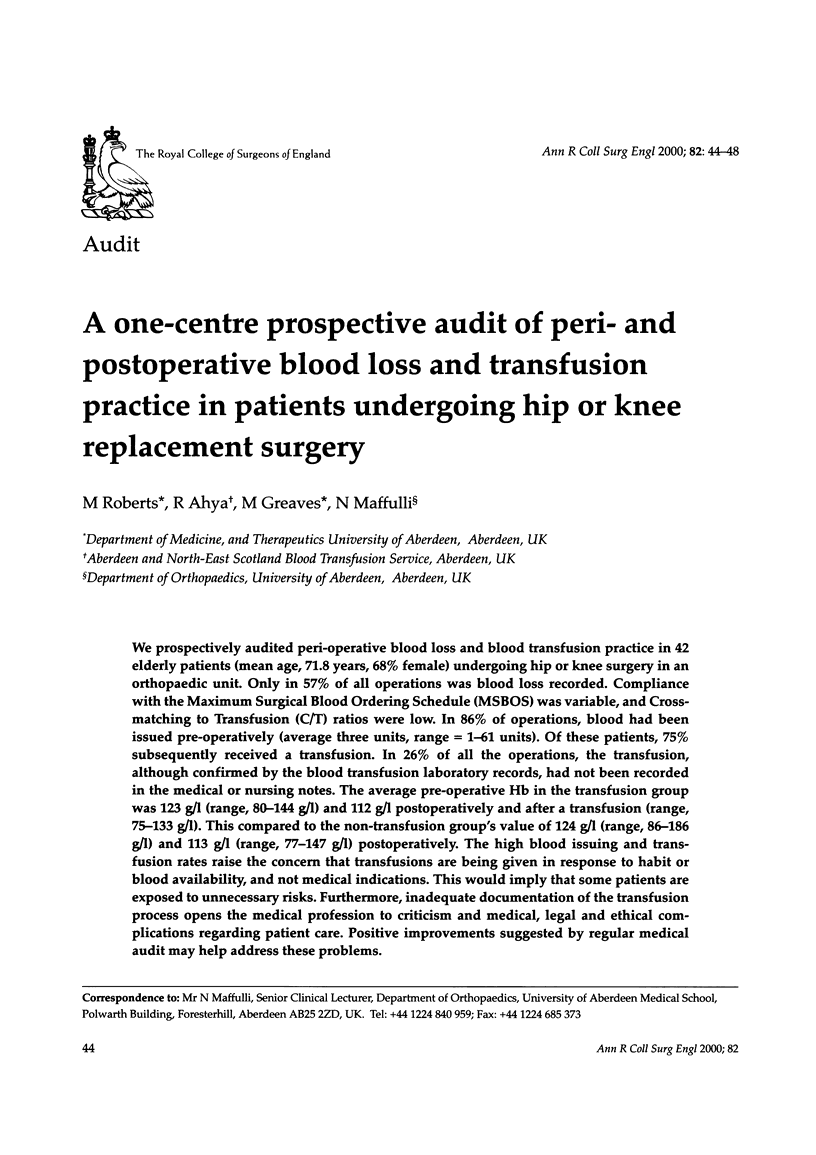



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Carson J. L., Duff A., Berlin J. A., Lawrence V. A., Poses R. M., Huber E. C., O'Hara D. A., Noveck H., Strom B. L. Perioperative blood transfusion and postoperative mortality. JAMA. 1998 Jan 21;279(3):199–205. doi: 10.1001/jama.279.3.199. [DOI] [PubMed] [Google Scholar]
- Hartigan G. National audit of the quality of the clinical blood transfusion process. New audit measures for good practice in blood transfusion medicine. J R Coll Physicians Lond. 1996 Jan-Feb;30(1):36–36. [PMC free article] [PubMed] [Google Scholar]
- Metz J., McGrath K. M., Copperchini M. L., Haeusler M., Haysom H. E., Gibson P. R., Millar R. J., Babarczy A., Ferris L., Grigg A. P. Appropriateness of transfusions of red cells, platelets and fresh frozen plasma. An audit in a tertiary care teaching hospital. Med J Aust. 1995 Jun 5;162(11):572-3, 576-7. [PubMed] [Google Scholar]
- Mintz P. D. Quality assessment and improvement of transfusion practices. Hematol Oncol Clin North Am. 1995 Feb;9(1):219–232. [PubMed] [Google Scholar]
- Nicholls M. D. How safe is blood? Anaesth Intensive Care. 1993 Feb;21(1):13–14. doi: 10.1177/0310057X9302100106. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., Salem-Schatz S., Avorn J., Casteris C. S., Ross-Degnan D., Popovsky M. A. A controlled trial of educational outreach to improve blood transfusion practice. JAMA. 1993 Aug 25;270(8):961–966. [PubMed] [Google Scholar]
- Sudhindran S. Perioperative blood transfusion: a plea for guidelines. Ann R Coll Surg Engl. 1997 Jul;79(4):299–302. [PMC free article] [PubMed] [Google Scholar]
- Toy P. T. Effectiveness of transfusion audits and practice guidelines. Arch Pathol Lab Med. 1994 Apr;118(4):435–437. [PubMed] [Google Scholar]
- Weiskopf R. B., Viele M. K., Feiner J., Kelley S., Lieberman J., Noorani M., Leung J. M., Fisher D. M., Murray W. R., Toy P. Human cardiovascular and metabolic response to acute, severe isovolemic anemia. JAMA. 1998 Jan 21;279(3):217–221. doi: 10.1001/jama.279.3.217. [DOI] [PubMed] [Google Scholar]


