Abstract
Objective
To explore and evaluate the most common factors causing therapeutic non-compliance.
Methods
A qualitative review was undertaken by a literature search of the Medline database from 1970 to 2005 to identify studies evaluating the factors contributing to therapeutic non-compliance.
Results
A total of 102 articles was retrieved and used in the review from the 2095 articles identified by the literature review process. From the literature review, it would appear that the definition of therapeutic compliance is adequately resolved. The preliminary evaluation revealed a number of factors that contributed to therapeutic non-compliance. These factors could be categorized to patient-centered factors, therapy-related factors, social and economic factors, healthcare system factors, and disease factors. For some of these factors, the impact on compliance was not unequivocal, but for other factors, the impact was inconsistent and contradictory.
Conclusion
There are numerous studies on therapeutic noncompliance over the years. The factors related to compliance may be better categorized as “soft” and “hard” factors as the approach in countering their effects may differ. The review also highlights that the interaction of the various factors has not been studied systematically. Future studies need to address this interaction issue, as this may be crucial to reducing the level of non-compliance in general, and to enhancing the possibility of achieving the desired healthcare outcomes.
Keywords: patient compliance, adherence, factors
Introduction
The ultimate aim of any prescribed medical therapy is to achieve certain desired outcomes in the patients concerned. These desired outcomes are part and parcel of the objectives in the management of the diseases or conditions. However, despite all the best intention and efforts on the part of the healthcare professionals, those outcomes might not be achievable if the patients are non-compliant. This shortfall may also have serious and detrimental effects from the perspective of disease management. Hence, therapeutic compliance has been a topic of clinical concern since the 1970s due to the widespread nature of non-compliance with therapy. Therapeutic compliance not only includes patient compliance with medication but also with diet, exercise, or life style changes. In order to evaluate the possible impact of therapeutic non-compliance on clinical outcomes, numerous studies using various methods have been conducted in the United States (USA), United Kingdom (UK), Australia, Canada and other countries to evaluate the rate of therapeutic compliance in different diseases and different patient populations. Generally speaking, it was estimated that the compliance rate of long-term medication therapies was between 40% and 50%. The rate of compliance for short-term therapy was much higher at between 70% and 80%, while the compliance with lifestyle changes was the lowest at 20%–30% (DiMatteo 1995). Furthermore, the rates of non-compliance with different types of treatment also differ greatly. Estimates showed that almost 50% of the prescription drugs for the prevention of bronchial asthma were not taken as prescribed (Sabaté 2003). Patients’ compliance with medication therapy for hypertension was reported to vary between 50% and 70% (Sabaté 2003). In one US study, Monane et al found that antihypertensive compliance averaged 49%, and only 23% of the patients had good compliance levels of 80% or higher (Monane et al 1996). Among adolescent outpatients with cancer, the rate of compliance with medication was reported to be 41%, while among teenagers with cancer it was higher at between 41% and 53% (Tebbi et al 1986). For the management of diabetes, the rate of compliance among patients to diet varied from 25% to 65%, and for insulin administration was about 20% (Cerkoney and Hart 1980). More than 20 studies published in the past few years found that compliance with oral medication for type 2 diabetes mellitus ranged from 65% to 85% (Rubin 2005). As previously mentioned, if the patients do not follow or adhere to the treatment plan faithfully, the intended beneficial effects of even the most carefully and scientifically-based treatment plan will not be realized. The above examples illustrate the extent of the problem of therapeutic non-compliance and why it should be a concern to all healthcare providers.
Definition of compliance
To address the issue of therapeutic non-compliance, it is of first and foremost importance to have a clear and acceptable definition of compliance. In the Oxford dictionary, compliance is defined as the practice of obeying rules or requests made by people in authority (Oxford Advanced Learner’s Dictionary of Current English). In healthcare, the most commonly used definition of compliance is “patient’s behaviors (in terms of taking medication, following diets, or executing life style changes) coincide with healthcare providers’ recommendations for health and medical advice” (Sackett 1976). Thus, therapeutic non-compliance occurs when an individual’s health-seeking or maintenance behavior lacks congruence with the recommendations as prescribed by a healthcare provider. Other similar terms have been used instead of compliance, and the meaning is more or less identical. For example, the term adherence is often used interchangeably with compliance. Adherence is defined as the ability and willingness to abide by a prescribed therapeutic regimen (Inkster 2006). Recently, the term “concordance” is also suggested to be used. Compared with “compliance”, the term concordance makes the patient the decision-maker in the process and denotes patients-prescribers agreement and harmony (Vermeire et al 2001). Although there are slight and subtle differences between these terms, in clinical practice, these terms are used interchangeably (albeit may not be totally correctly). Therefore, the more commonly used term of compliance will be used throughout this article.
Types of non-compliance
After defining what is meant by compliance, the next question that comes to mind to the healthcare providers would be: “What are the common types of non-compliance encountered in clinical medicine?” A knowledge and understanding of the various types of non-compliance commonly encountered in clinical practice would allow the formulation of strategies to tackle them effectively. A review of the literature reveals several types of commonly reported or detected non-compliance. (Table 1) Besides the types of non-compliance encountered, another logical question to ask in trying to complete the jigsaw puzzle of therapeutic non-compliance would be: “In clinical medicine, what is considered to be good or acceptable compliance?” Although it must be acknowledged that this is still controversial, in relation to good medication compliance, it has commonly been defined as taking 80 to 120% of the medication prescribed (Sackett et al 1975; Monane et al 1996; Avorn et al 1998; Hope et al 2004). For compliance with other treatment such as exercise or diet, the definition of acceptable compliance varied among different studies and there does not seem to be any commonly accepted criterion to define good or acceptable compliance.
Table 1.
Type of reported non-compliance
| Type of non-compliance | Reference |
|---|---|
| Receiving a prescription but not filling it | Donovan and Blake 1992 |
| Taking an incorrect dose | |
| Taking medication at the wrong times | |
| Increasing or decreasing the frequency of doses | |
| Stopping the treatment too soon | |
| Delaying in seeking healthcare | Vermeire et al 2001 |
| Non-participation in clinic visits | |
| Failure to follow doctor’s instructions | Gordis 1979 |
| “Drug holidays”, which means the patient stops the therapy for a while and then restarts the therapy | Cummings et al 1982;Vermeire 2001 |
| “White-coat compliance”, which means patients are compliant to the medication regimen around the time of clinic appointments | Cramer et al 1990; Feinstein 1990; Vermeire 2001; Burnier et al 2003 |
Problems with therapeutic non-compliance
Before we can formulate strategies to tackle the issue of therapeutic non-compliance, we need to assess the clinical and other implications of therapeutic non-compliance.
From the perspective of healthcare providers, therapeutic compliance is a major clinical issue for two reasons. Firstly, non-compliance could have a major effect on treatment outcomes and direct clinical consequences. Non-compliance is directly associated with poor treatment outcomes in patients with diabetes, epilepsy, AIDS (acquired immunodeficiency syndrome), asthma, tuberculosis, hypertension, and organ transplants (Sabaté 2003). In hypertensive patients, poor compliance with therapy is the most important reason for poorly controlled blood pressure, thus increasing the risk of stroke, myocardial infarction, and renal impairment markedly. Data from the third NHANES (the National Health and Nutrition Examination Survey), which provides periodic information on the health of the US population, showed that blood pressure was controlled in only 31% of the hypertension patients between 1999 and 2000 (Hajjar and Kotchen 2003). It is likely that non-compliance with treatment contributed to this lack of blood pressure control among the general population. For therapeutic non-compliance in infectious diseases, the consequences can include not only the direct impact such as treatment failures, but also indirect impact or negative externalities as well via the development of resistant microorganisms (Sanson-Fisher et al 1992). In addition, it has been shown that almost all patients who had poor compliance with drugs eventually dropped out of treatments completely, and therefore did not benefit at all from the treatment effects (Lim and Ngah 1991).
Besides undesirable impact on clinical outcomes, non-compliance would also cause an increased financial burden for society. For example, therapeutic non-compliance has been associated with excess urgent care visits, hospitalizations and higher treatment costs (Bond and Hussar 1991, Svarstad et al 2001). It has been estimated that 25% of hospital admissions in Australia, and 33%–69% of medication-related hospital admissions in the USA were due to non-compliance with treatment regimens (Sanson-Fisher et al 1992; Osterberg and Blaschke 2005). Additionally, besides direct financial impact, therapeutic non-compliance would have indirect cost implications due to the loss of productivity, without even mentioning the substantial negative effect on patient’s quality of life.
Furthermore, as a result of undetected or unreported therapeutic non-compliance, physicians may change the regimen, which may increase the cost or complexity of the treatment, thus further increasing the burden on the healthcare system. The cost burden has been estimated at US$100 billion each year in the USA alone (Vermeire et al 2001). Prescription drug cost is the fastest growing component of healthcare costs in the USA. National outpatient drug spending has increased by 13 to 16% per year during the past few years, and it is expected to continue to grow by 9%–13% per year during the coming decade (Sokol et al 2005). In the era where cost-effectiveness is a buzz word in healthcare delivery, any factors that could contribute to increased drug use should be a concern for the healthcare providers.
Hence, from both the perspective of achieving desirable clinical and economic outcomes, the negative effect of therapeutic non-compliance needs to be minimized. However, in order to formulate effective strategies to contain the problem of non-compliance, there is a need to systematically review the factors that contribute to non-compliance. An understanding of the predictive value of these factors on non-compliance would also contribute positively to the overall planning of any disease management program.
Objectives
To conduct a systematic qualitative review to identify the most common factors causing therapeutic non-compliance from the patient’s perspective.
Methods
Literature searches were undertaken through the Medline database from 1970 to 2005. The following MeSH (medical subject heading) terms were used: treatment refusal, patient compliance, and patient dropouts. MeSH terms provide a consistent way to retrieve information that may use different terminology for the same concepts. Besides MeSH terms, the following key words were also searched in the title or abstract: factors, predictors and determinants.
Only English-language journal articles with abstracts were included. The populations were adolescents aged 13–18 years and adults aged 19 years or older. Clinical trials were excluded since they were carried out under close monitoring and therefore the compliance rates reported would not be generalizable. Articles which were categorized by Medline in subsets on AIDS, bioethics, history of medicine, space life sciences and toxicology were not included as well.
Abstracts of identified articles were retrieved manually to select original studies and reviews which mainly focused on the topics of interest. The topics of interest in the field of patient compliance were: factors that influence therapeutic non-compliance and the extent of non-compliance with treatment. Only non-compliance studies from the patient’s perspective were selected. Original studies that included fewer than 50 patients were eliminated because of inadequate sample size. If the sample population of studies was very specific, such as involving only males or females, or recruiting patients from one specific class (homeless, prisoners or workers from one employer, etc), they were eliminated as well because results from these studies might not be generalizable to the general population. In addition, a number of articles were excluded if they mainly focused on strategies to enhance patient’s compliance, methods to measure compliance, validating instruments to identify factors influencing non-compliance and the effect of non-compliance. When the abstracts were not clear enough to decide whether articles met the inclusion criteria, full articles were read to make the decision.
Results
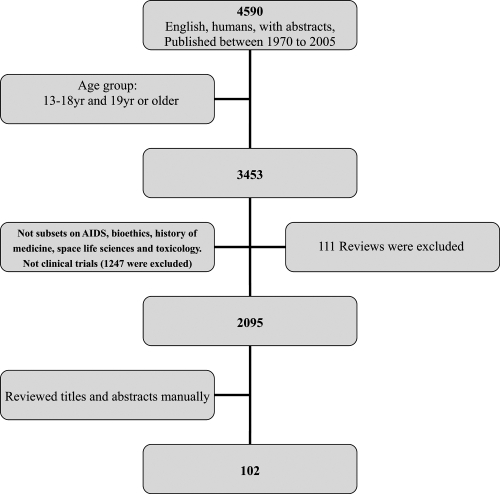
A total of 2095 articles were retrieved in this process, and after the culling process, 102 articles met the inclusion criteria. The rest were excluded for the reasons such as small sample size, not focused on factors affecting compliance, not from patients’ perspective, etc (Figure 1). The impact of these factors on therapeutic non-compliance would be discussed in details in the subsequent sections.
Figure 1.
Retrieval and culling process of the articles in literature review process.
Factors identified
The factors identified from the studies and reviews may be grouped into several categories, namely, patient-centered factors, therapy-related factors, healthcare system factors, social and economic factors, and disease factors (Table 2).
Table 2.
Categories of factors identified from the literature review
| Category | Factors |
|---|---|
| Patient-centered factors | Demographic Factors: Age, Ethnicity, Gender, Education, Marriage Status |
| Psychosocial factors: Beliefs, Motivation,Attitude | |
| Patient-prescriber relationship | |
| Health literacy | |
| Patient knowledge | |
| Physical difficulties | |
| Tobacco Smoking or alcohol intake | |
| Forgetfulness | |
| History of good compliance | |
| Therapy-related factors | Route of administration |
| Treatment complexity | |
| Duration of the treatment period | |
| Medication side effects | |
| Degree of behavioral change required | |
| Taste of the medication | |
| Requirements for drug storage | |
| Healthcare system factors | Lack of accessibility |
| Long waiting time | |
| Difficulty in getting prescriptions filled | |
| Unhappy clinic visits | |
| Social and economic factors | Inability to take time off work |
| Cost and Income | |
| Social support | |
| Disease factors | Disease symptoms |
| Severity of the disease |
Patient-centered factors
Demographic factors
Factors identified to be in this group include patient’s age, ethnicity, gender, education, and marital status. A summary of the impact of these factors on therapeutic compliance is presented (Table 3).
Table 3.
The effect of demographic factors on compliance
Age
More than thirty retrieved articles were related to this factor. The majority of the studies showed that age was related to compliance, although a few researchers found age not to be a factor causing non-compliance (Lorenc and Branthwaite 1993; Menzies et al 1993; Wild et al 2004; Wai et al 2005). From a review of the articles showing a correlation between age and non-compliance, it would appear that the effect of age could be divided into 3 major groups: the elderly group (over 55 years old), the middle-age group (40 to 54 years old) and the young group (under 40 years old).
For elderly people, the results from the various studies are not unidirectional. A large proportion of retrieved studies suggested that they might have higher compliance (Norman et al 1985; Didlake et al 1988; Schweizer et al 1990; Shea et al 1992; Frazier et al 1994; McLane et al 1995; Shaw et al 1995; Monane et al 1996; Buck et al 1997; Viller et al 1999; Sirey et al 2001; Kim et al 2002; Senior et al 2004; Hertz et al 2005). In a study carried out in UK, patients over 60 years old were more likely to be always compliant with their antiepileptic tablets than patients under 60 years old (86% vs 66%, respectively) (Buck et al 1997). It was also suggested that patients’ antidepressant drug compliance was positively related to age over 60 years (Sirey et al 2001). These results are consistent with the conclusion from another published review (Krousel-Wood et al 2004). In addition, four studies focusing on younger people (mean age 46–50 yr) indicated the same trend that compliance increased with the increasing age (Degoulet et al 1983; Christensen and Smith 1995; Caspard et al 2005; Lacasse et al 2005).
However, some studies found that advancing age affected compliance among elderly people in the opposite direction (Okuno et al 1999; Benner et al 2002; Balbay et al 2005). Nevertheless, there were confounding factors in these studies. The study by Balbay et al was carried out in a rural area of Turkey among patients with tuberculosis and found that younger patients were more compliant to treatment than older patients (mean age 42 yr vs 50 yr) (Balbay et al 2005). The researchers stated that this might be due to the low education level of older patients. Similarly, the study by Okuno et al suggested that home-care patients aged 80 and over were less likely to be compliant with their prescribed medication, but the participants in that particular study had physical disabilities which limit its generalizability (Okuno et al 1999).
Several studies also attempted to venture plausible reasons for poorer compliance among elderly patients. Elderly patients may have problems in vision, hearing and memory. In addition, they may have more difficulties in following therapy instructions due to cognitive impairment or other physical difficulties, such as having problems in swallowing tablets, opening drug containers, handling small tablets, distinguishing colors or identifying markings on drugs. (Murray et al 1986; Stewart and Caranasos 1989; Chizzola et al 1996; Nikolaus et al 1996; Okuno et al 2001; Benner et al 2002; Jeste et al 2003; Cooper et al 2005). On the contrary, older people might also have more concern about their health than younger patients, so that older patients’ non-compliance is non-intentional in most cases. As a result, if they can get the necessary help from healthcare providers or family members, they may be more likely to be compliant with therapies.
In comparison, the impact of younger age on compliance is much more congruent among the studies. Middle-aged patients were less likely to be compliant to therapy. In Japan, patients in the prime of their life (40–59 years) were found less likely to be compliant to the medication (Iihara et al 2004). Similarly, young patients under 40 years also have a low compliance rate (Neeleman and Mikhail 1997; Leggat et al 1998; Loong 1999; Siegal and Greenstein 1999). In Singapore, patients less than 30 years old were found to be less likely to collect the medication prescribed at a polyclinic (Loong 1999). In a study about patients’ compliance with hemodialysis, patients aged 20 to 39 years were poorly compliant (Leggat et al 1998). Patients in these two age ranges (middle-aged patients and young patients under 40 years old) always have other priorities in their daily life. Due to their work and other commitments, they may not be able to attend to treatment or spend a long time waiting for clinic appointments.
Likewise, low compliance also occurs in adolescents and children with chronic disease (Buck et al 1997; Kyngas 1999). Very young children need more help from their parents or guardians to implement treatment. Therefore, their poorer compliance may be due to a lack of understanding or other factors relating to their parents or guardians. For adolescents, this period is often marked by rebellious behavior and disagreement with parents and authorities (Tebbi 1993). They usually would prefer to live a normal life like their friends. This priority could therefore influence their compliance.
Ethnicity
Race as a factor causing non-compliance has been studied fairly widely in the USA and European countries and sixteen studies on this factor were retrieved. Caucasians are believed to have good compliance according to some studies (Didlake et al 1988; Sharkness and Snow 1992; Turner et al 1995; Raiz et al 1999; Thomas et al 2001; Yu et al 2005), while African-Americans, Hispanics and other minorities were found to have comparatively poor compliance (Schweizer et al 1990; Monane et al 1996; Leggat et al 1998; Benner et al 2002; Apter et al 2003; Opolka et al 2003; Spikmans et al 2003; Butterworth et al 2004; Kaplan et al 2004; Dominick et al 2005). However, a plausible explanation for this may be due to patient’s lower socio-economic status and language barriers of the minority races in the study countries. Hence, due to these confounding variables, ethnicity may not be a true predictive factor of poorer compliance.
Gender
In the twenty-two studies retrieved related to this factor, the results are contradictory. Female patients were found by some researchers to have better compliance (Degoulet et al 1983; Chuah 1991; Shea et al 1992; Kyngas and Lahdenpera 1999; Viller et al 1999; Kiortsis et al 2000; Lindberg et al 2001; Balbay et al 2005; Choi-Kwon 2005; Fodor et al 2005; Lertmaharit et al 2005), while some studies suggested otherwise (Frazier et al 1994; Sung et al 1998; Caspard et al 2005; Hertz et al 2005). In addition, some studies could not find a relationship between gender and compliance (Menzies et al 1993; Buck et al 1997; Horne and Weinman 1999; Ghods and Nasrollahzadeh 2003; Spikmans et al 2003; Senior et al 2004). This is consistent with another literature review on compliance in seniors that concluded that gender has not been found to influence compliance (Vic et al 2004). Gender may not be a good predictor of non-compliance because of the inconsistent conclusions.
Educational level
The effect of educational level on non-compliance was equivocal after reviewing thirteen articles which focused on the impact of educational level as they used different criteria for “higher” and “lower” education. Several studies found that patients with higher educational level might have higher compliance (Apter et al 1998; Okuno et al 2001; Ghods and Nasrollahzadeh 2003; Yavuz et al 2004), while some studies found no association (Norman et al 1985; Horne and Weinman 1999; Spikmans et al 2003; Kaona et al 2004; Stilley et al 2004; Wai et al 2005). Intuitively, it may be expected that patients with higher educational level should have better knowledge about the disease and therapy and therefore be more compliant. However, DiMatteo found that even highly educated patients may not understand their conditions or believe in the benefits of being compliant to their medication regimen (DiMatteo 1995). Other researchers showed that patients with lower education level have better compliance (Kyngas and Lahdenpera 1999; Senior et al 2004). A UK study group found that patients without formal educational qualifications had better compliance with cholesterol-lowering medication (Senior et al 2004). Patients with lower educational level might have more trust in physicians’ advice. From these results, it seems that educational level may not be a good predictor of therapeutic compliance.
Marital status
Marital status might influence patients’ compliance with medication positively (Swett and Noones 1989; Frazier et al 1994; De Geest et al 1995; Turner et al 1995; Cooper et al 2005). The help and support from a spouse could be the reason why married patients were more compliant to medication than single patients. However, marital status was not found to be related to patient’s compliance in five recent studies (Ghods and Nasrollahzadeh 2003; Spikmans et al 2003; Kaona et al 2004; Wild et al 2004; Yavuz et al 2004). This disparity might be due to the fact that the recent studies investigated the effect of marital status in disease conditions which were different from those evaluated in the older studies, with the impact being masked by the disease factor.
Psychological factors
Patient’s beliefs, motivation and negative attitude towards therapy were identified as factors to be included in this category.
Patients’ beliefs and motivation about the therapy
Twenty-three articles were identified for this factor in the review process. From the results, patients’ beliefs about the causes and meaning of illness, and motivation to follow the therapy were strongly related to their compliance with healthcare (Lim and Ngah 1991; Buck et al 1997; Cochrane et al 1999; Kyngas 1999; Kyngas 2001; Kyngas and Rissanen 2001; Vincze et al 2004).
In summarizing the findings from the various studies, it would appear that compliance was better when the patient had the following beliefs:
The patient feels susceptible to the illness or its complication (Haynes et al 1980; Abbott et al 1996; Spikmans et al 2003).
The patient believes that the illness or its complications could pose severe consequences for his health (McLane et al 1995; Sirey et al 2001; Loffler et al 2003).
The patient believes that the therapy will be effective or perceives benefits from the therapy (Lorenc and Branthwaite 1993; De Geest et al 1995; Cochrane et al 1999; Horne and Weinman 1999; Apter et al 2003; Spikmans et al 2003; Krousel-Wood et al 2004; Wild et al 2004; Gonzalez et al 2005; Seo and Min 2005).
On the contrary, misconceptions or erroneous beliefs held by patients would contribute to poor compliance. Patient’s worries about the treatment, believing that the disease is uncontrollable and religious belief might add to the likelihood that they are not compliant to therapy. In a review to identify patient’s barriers to asthma treatment compliance, it was suggested that if the patients were worried about diminishing effectiveness of medication over time, they were likely to have poor compliance with the therapy (Bender and Bender 2005). In patients with chronic disease, the fear of dependence on the long-term medication might be a negative contributing factor to compliance (Apter et al 2003; Bender and Bender 2005). This is sometimes augmented further by cultural beliefs. For example, in Malaysia, some hypertension patients believed long-term use of “Western” medication was “harmful”, and they were more confident in herbal or natural remedies (Lim and Ngah 1991). In a New Zealand study, Tongan patients may think disease is God’s will and uncontrollable; and as a consequence, they perceived less need for medication (Barnes et al 2004). Similarly, in Pakistan, inbred fears and supernatural beliefs were reported to be two major factors affecting patients’ compliance with treatment (Sloan and Sloan 1981).
Patients who had low motivation to change behaviors or take medication are believed to have poor compliance (Lim and Ngah 1991; Hernandez-Ronquillo et al 2003; Spikmans et al 2003). In a study done in Malaysia, 85% of hypertension patients cited lack of motivation as the reason for dropping out of treatment (Lim and Ngah 1991).
Negative attitude towards therapy
Fifteen studies showed an association between patients’ negative attitude towards therapy (eg, depression, anxiety, fears or anger about the illness) and their compliance (Lorenc and Branthwaite 1993; Bosley et al 1995; Carney et al 1995; Milas et al 1995; Jette et al 1998; Clark et al 1999; Raiz et al 1999; Sirey et al 2001; Barnes et al 2004; Gascon et al 2004; Iihara et al 2004; Kaplan et al 2004; Stilley et al 2004; Kilbourne et al 2005; Yu et al 2005). In one study conducted in patients older than 65 years with coronary artery disease, depression affected compliance markedly (Carney et al 1995). There were other studies reporting that for children or adolescents, treatment may make them feel stigmatized (Bender and Bender 2005), or feel pressure because they are not as normal as their friends or classmates (Kyngas 1999). Therefore, negative attitude towards therapy should be viewed as a strong predictor of poor compliance.
Patient-prescriber relationship
Seventeen articles evaluated the effect of the patient-prescriber relationship to patient’s compliance. From these articles it could be concluded that patient-prescriber relationship is another strong factor which affects patients’ compliance (Buck et al 1997; Roter and Hall 1998; Stromberg et al 1999; Kiortsis et al 2000; Okuno et al 2001; Kim et al 2002; Loffler et al 2003; Moore et al 2004; Gonzalez et al 2005). A healthy relationship is based on patients’ trust in prescribers and empathy from the prescribers. Studies have found that compliance is good when doctors are emotionally supportive, giving reassurance or respect, and treating patients as an equal partner (Moore et al 2004; Lawson et al 2005). Rubin mentioned some situations that may influence patients’ trust in physicians (Rubin 2005). For example, physicians who asked few questions and seldom made eye contact with patients, and patients who found it difficult to understand the physician’s language or writing. More importantly, too little time spent with patients was also likely to threaten patient’s motivation for maintaining therapy (Lim and Ngah 1991; Gascon et al 2004; Moore et al 2004; Lawson et al 2005).
Poor communication with healthcare providers was also likely to cause a negative effect on patient’s compliance (Bartlett et al 1984; Apter et al 1998). Lim and Ngah showed in their study that non-compliant hypertension patients felt the doctors were lacking concern for their problems (Lim and Ngah 1991). In addition, multiple physicians or healthcare providers prescribing medications might decrease patients’ confidence in the prescribed treatment (Vlasnik et al 2005).
These findings demonstrate the need for cooperation between patients and healthcare providers and the importance of good communication. To build a good and healthy relationship between patients and providers, providers should have patients involved in designing their treatment plan (Gonzalez et al 2005; Vlasnik et al 2005), and give patients a detailed explanation about the disease and treatment (Butterworth et al 2004; Gascon et al 2004). Good communication is also very important to help patients understand their condition and therapy (Lorenc and Branthwaite 1993).
Health literacy
Health literacy means patients are able to read, understand, remember medication instructions, and act on health information (Vlasnik et al 2005). Patients with low health literacy were reported to be less compliant with their therapy (Nichols-English and Poirier 2000). On the contrary, patients who can read and understand drug labels were found to be more likely to have good compliance (Murray et al 1986; Lorenc and Branthwaite 1993; Butterworth et al 2004). Thus, using written instructions and pictograms on medicine labels has proven to be effective in improving patient’s compliance (Dowse and Ehlers 2005; Segador et al 2005).
Patient knowledge
Patient’s knowledge about their disease and treatment is not always adequate. Some patients lack understanding of the role their therapies play in the treatment (Ponnusankar et al 2004); others lack knowledge about the disease and consequences of poor compliance (Alm-Roijer et al 2004; Gascon et al 2004); or lack understanding of the value of clinic visits (Lawson et al 2005). Some patients thought the need for medication was intermittent, so they stopped the drug to see whether medication was still needed (Vic et al 2004; Bender and Bender 2005). For these reasons, patient education is very important to enhance compliance. Counseling about medications is very useful in improving patient’s compliance (Ponnusankar et al 2004). Healthcare providers should give patients enough education about the treatment and disease (Haynes et al 1980; Norman et al 1985; Stanton 1987; Olubodun et al 1990; Lorenc and Branthwaite 1993; Menzies et al 1993; Milas et al 1995; Chizzola et al 1996; Hungin 1999; Liam et al 1999; Okuno et al 1999; Viller et al 1999; Lindberg et al 2001; Thomas et al 2001; Gascon et al 2004; Iihara et al 2004; Kaona et al 2004; Ponnusankar et al 2004; Seo and Min 2005).
However, education is not always “the more the better”. An “inverted U” relationship between knowledge and compliance existed in adolescents. Adolescent patients who knew very little about their therapies and illness were poor compliers, while patients who were adequately educated about their disease and drug regimens were good compliers; but patients who knew the life-long consequences might show poor compliance (Hamburg and Inoff 1982). Nevertheless, there is no report of similar observations in other age groups. In addition, patients’ detailed knowledge of the disease was not always effective. In Hong Kong, researchers could not find any association between diabetes knowledge and compliance. They suggested that there was a gap between what the patients were taught and what they were actually doing (Chan and Molassiotis 1999).
In addition, the content of education is crucial. Rubin found that educating the patients about their disease state and general comprehension of medications would increase their active participation in treatment (Rubin 2005). Making sure patients understand the drug dosing regimen could also improve compliance (Olubodun et al 1990). To make sure patients remember what was taught, written instructions work better than verbal ones, as patients often forget physician’s advice and statements easily (Tebbi 1993).
Other factors
Smoking or alcohol intake
Several studies about compliance among asthma, hypertension and renal transplantation patients found that patients who smoked or drank alcohol were more likely to be non-compliant (Degoulet et al 1983; Shea et al 1992; Turner et al 1995; Leggat et al 1998; Kyngas 1999; Kyngas and Lahdenpera 1999; Kiortsis et al 2000; Kim et al 2002; Ghods and Nasrollahzadeh 2003; Yavuz et al 2004; Balbay et al 2005; Cooper et al 2005; Fodor et al 2005). In a study conducted in Finland in hypertension patients, non-smokers were more compliant to the diet restrictions (Kyngas and Lahdenpera 1999). Likewise, another study in renal transplantation patients in Turkey found that patients who were smoking or drinking were unlikely to be compliant to the therapy (Yavuz et al 2004). Only one single study about obstructive sleep apnoea/hypopnoea syndrome (OSAHS) found no relationship between smoking or alcohol intake and patient’s compliance with continuous positive airway pressure treatment (Wild et al 2004).
Forgetfulness
Forgetfulness is a widely reported factor that causes non-compliance with medication or clinic appointments (Cummings et al 1982; Kelloway et al 1994; Okuno et al 2001; Hernandez-Ronquillo et al 2003; Ponnusankar et al 2004; Wai et al 2005). A Japanese study in elderly home-care recipients found an interesting association between meal frequency and compliance. Patients having less than 3 meals per day were less compliant than patients having 3 meals a day. It suggested that meal frequency was an effective tool to remind the patient to take drugs (Okuno et al 1999). As mentioned in a previous section, written instructions are better than oral advice for reminding patients to take medication.
Therapy-related factors
Therapy-related factors identified include: route of administration, treatment complexity, duration of treatment period, medication side effects, degree of behavioral change required, taste of medication and requirement for drug storage (Table 4).
Table 4.
The effect of therapy-related factors on compliance
Route of administration
Medications with a convenient way of administration (eg, oral medication) are likely to make patients compliant. Studies in asthma patients compared compliance between oral and inhaled asthma medications, and found patients had better compliance with oral medication (Kelloway et al 1994; Nichols-English and Poirier 2000). Likewise, difficulty in using inhalers contributes to non-compliance in patients with asthma (Bender and Bender 2005).
Treatment complexity
Complex treatment is believed to threaten the patient’s compliance. However, compliance does not seem to correlate with the number of drugs prescribed (Horne and Weinman 1999; Patal and Taylor 2002; Grant et al 2003; Iihara et al 2004), but the number of dosing times every day of all prescribed medications (Kass et al 1986; Cockburn et al 1987; Cramer et al 1989; Eisen et al 1990; Cramer 1998; Sung et al 1998; Claxton et al 2001; Iskedjian et al 2002). The rate of compliance decreased as the number of daily doses increased. This is illustrated by one study where compliance was assessed by pill counts and self-reports that showed that non-compliance increased with an increase in the frequency of prescribed dosing: 20% for once daily; 30% for twice daily; 60% for three times a day; and 70% for four times daily (Cramer et al 1989). Similarly, a meta-analysis found that there was a significant difference in compliance rate between patients taking antihypertensive medication once daily and twice daily (92.1% and 88.9%, respectively) (Iskedjian et al 2002). Thus, simplifying the medication dosing frequency could improve compliance markedly.
Duration of the treatment period
Acute illnesses are associated with higher compliance than chronic illnesses (Gascon et al 2004). In addition, longer duration of the disease may adversely affect compliance (Farmer et al 1994; Frazier et al 1994). Similarly, a longer duration of treatment period might also compromise patient’s compliance (Menzies et al 1993; Ghods and Nasrollahzadeh 2003; Dhanireddy et al 2005). In one trial that compared 6-month and 9-month treatment of tuberculosis, compliance rates were 60% and 50% for the two regimens, respectively (Combs et al 1987). In another study comparing preventive regimens of 3, 6 and 12 months, compliance rates were 87%, 78% and 68% for the three regimens, respectively (International Union Against Tuberculosis 1982).
However, some studies about chronic diseases found that longer duration of the disease resulted in good compliance (Sharkness and Snow 1992; Garay-Sevilla et al 1995), and newly diagnosed patients had poor compliance (Caro et al 1999). This may indicate that compliance is improved because patient’s attitude of denying the disease is reduced and they accepted treatment after years of suffering from the disease.
Medication side effects
All of the seventeen studies on side effects factor found that side effects threaten patient’s compliance (Spagnoli et al 1989; Shaw et al 1995; Buck et al 1997; Dusing et al 1998; Hungin 1999; Kiortsis et al 2000; Linden et al 2000; Kim et al 2002; Dietrich et al 2003; Grant et al 2003; Loffler et al 2003; Sleath et al 2003; Iihara et al 2004; Kaplan et al 2004; Ponnusankar et al 2004; O’Donoghue 2004). In a German study, the second most common reason for non-compliance with antihypertensive therapy was adverse effects (Dusing et al 1998). The effect of side effects on compliance may be explained in terms of physical discomfort, skepticism about the efficacy of the medication, and decreasing the trust in physicians (Christensen 1978).
Degree of behavioral change required
The degree of required behavioral change is related to patients’ motivation to be compliant with the therapy (Milas et al 1995; Hernandez-Ronquillo et al 2003; Vincze et al 2004). A study done in Mexico demonstrated that patients with type 2 diabetes could not follow the diet because of the difficulty of changing their dietary habits (Hernandez-Ronquillo et al 2003).
Social and economic factors
Social and economic factors include: time commitment, cost of therapy, income and social support.
Time commitment
Patients may not be able to take time off work for treatment; as a result, their rate of compliance could be threatened (Shaw et al 1995; Siegal and Greenstein 1999; Hernandez-Ronquillo et al 2003; Lawson et al 2005; Neal et al 2005). Therefore, a shorter traveling time between residence and healthcare facilities could enhance patient’s compliance (Gonzalez et al 2005). A study suggested that white collar patients have poor compliance because they have other priorities (Siegal and Greenstein 1999). Housewives with tuberculosis were more compliant to therapy in an observational study in Malaysia (Chuah 1991). This may be because housewives can adapt well to clinic appointment times and treatment.
Cost of therapy and income
Cost is a crucial issue in patient’s compliance especially for patients with chronic disease as the treatment period could be life-long (Connelly 1984; Shaw et al 1995; Ellis et al 2004; Ponnusankar et al 2004). Healthcare expenditure could be a large portion of living expenses for patients suffering from chronic disease. Cost and income are two interrelated factors. Healthcare cost should not be a big burden if the patient has a relatively high income or health insurance. A number of studies found that patients who had no insurance cover (Swett and Noones 1989; Kaplan et al 2004; Choi-Kwon 2005), or who had low income (Degoulet et al 1983; Cockburn et al 1987; Shea et al 1992; Frazier et al 1994; Apter et al 1998; Berghofer et al 2002; Benner et al 2002; Ghods and Nasrollahzadeh 2003; Hernandez-Ronquillo et al 2003; Mishra et al 2005) were more likely to be non-compliant to treatment. However, even for patients with health insurance, health expenses could still be a problem. More than one in ten seniors in the USA reported using less of their required medications because of cost (Congressional Budget Office 2003). Nevertheless, in other cases, income was not related to compliance level (Norman et al 1985; Lim and Ngah 1991; Patal and Taylor 2002; Stilley et al 2004; Wai et al 2005). In Singapore, a study on chronic hepatitis B surveillance found that monthly income was not related to patient’s compliance with regular surveillance (Wai et al 2005). This discrepancy might due to different healthcare systems in different countries. Healthcare personnel should be aware of patient’s economic situation and help them use medication more cost-effectively.
Social support
The general findings from these articles showed that patients who had emotional support and help from family members, friends or healthcare providers were more likely to be compliant to the treatment (Stanton 1987; Lorenc and Branthwaite 1993; Garay-Sevilla et al 1995; Milas et al 1995; Kyngas 1999; Okuno et al 1999; Stromberg et al 1999; Kyngas 2001; Kyngas and Rissanen 2001; Thomas et al 2001; Loffler et al 2003; DiMatteo 2004; Feinstein et al 2005; Seo and Min 2005; Voils et al 2005). The social support helps patients in reducing negative attitudes to treatment, having motivation and remembering to implement the treatment as well.
Healthcare system factors
The main factor identified relating to healthcare systems include availability and accessibility. Lack of accessibility to healthcare (Ponnusankar et al 2004), long waiting time for clinic visits (Grunebaum et al 1996; Balkrishnan et al 2003; Moore et al 2004; Lawson et al 2005; Wai et al 2005), difficulty in getting prescriptions filled (Cummings et al 1982; Vlasnik et al 2005), and unhappy or unsatisfied clinic visits (Spikmans et al 2003; Gascon et al 2004; Lawson et al 2005) all contributed to poor compliance. The above observation is further supported by another study that showed patient’s satisfaction with clinic visits is most likely to improve their compliance with the treatment (Haynes et al 1980).
Disease factor
Patients who are suffering from diseases with fluctuation or absence of symptoms (at least at the initial phase), such as asthma and hypertension, might have a poor compliance (Hungin 1999; Kyngas and Lahdenpera 1999; Vlasnik et al 2005). Kyngas and Lahdenpera demonstrated that there was a significant relationship between the presence of hypertension symptoms and reduction in the sodium consumption. Seventy-one percent of the patients who had symptoms reduced the use of sodium, as compared to only 7% of the patients who did not suffer from symptoms (Kyngas and Lahdenpera 1999). Patients who had marked improvement in symptoms with the help of treatment normally had better compliance (Lim et al 1992; Viller et al 1999; Grant et al 2003).
In addition, no consistent evidence shows that subjects with greater disease severity based on clinical evaluation comply better with medications than healthier ones (Matthews and Hingson 1977; Kyngas 1999; Wild et al 2004; Seo and Min 2005). A study in patients with OSAHS found that greater disease severity based on clinical variables predicted better compliance (Wild et al 2004). However, a study on compliance in adolescents with asthma showed that only patients with mild severity had good compliance (Kyngas 1999). Similarly, Matthews et al suggested that the actual severity of the illness (based on the physician’s clinical evaluation) was not related to compliance (Matthews and Hingson 1977). Instead of actual disease severity, perceived health status may have more significant influence on compliance. Patients expecting poor health status are more motivated to be compliant with treatment if they consider the medication to be effective (Rosenstock et al 1988). In a study conducted in the USA in patients on antihyperlipidemic medications, patients with a perception of poor health status were more compliant with treatment (Sung et al 1998). This supports the suggestion that how patients feel plays a crucial role in predicting compliance.
Discussion
From the literature review, it can be concluded that although several terms have been used, the terms are used more or less interchangeably in clinical practice and therefore, the definition of compliance is adequately defined in the practical context. However, one alarming observation is that non-compliance remains a major issue in enhancing healthcare outcomes in spite of the many studies highlighting the problem over the years.
In this review we attempted to identify factors related to compliance which would have wide generalizability, and we retrieved original studies investigating non-compliance from different diseases, population settings and different countries. In the process, we identified a wide array of influencing factors. Although some factors’ effect on compliance is complex and not unequivocal, several factors with consistent impact on compliance have been identified through the review process.
Firstly, addressing therapy-related factors should contribute positively in improving patient’s compliance. Prescribing medication with non-invasive route of administration (eg, oral medication) and simple dosing regimens might motivate patients to be compliant. Long duration of treatment period and medication side effects might compromise patient’s beliefs about medication effectiveness. Therefore, healthcare providers should consider therapy-related problems when designing the therapy plan and involve the patients in the process to minimize the possible therapeutic barriers.
Besides therapy-related factors, healthcare system problems were found to be significantly related to compliance. Accessibility and satisfaction with the healthcare facilities are important contributors to compliance because patient’s satisfaction with healthcare is crucial for their compliance. Long waiting time for clinic visits and unhappy experience during clinic visits was indicated by many studies. A healthcare system designed with convenient accessibility and patient satisfaction in mind would be a great help for compliance issue.
Thirdly, compliance is also related with disease characteristics. Non-compliance is usually not a prevalent issue in acute illness or illness of short duration. In contrast, patients who are suffering from chronic diseases, in particular those with fluctuation or absence of symptoms (eg, asthma and hypertension) are likely to be non-compliant. Special efforts and attention should be paid to address the issue of non-compliance in chronic disease patients.
Lastly, healthcare expenditure is a very important factor for patients with chronic diseases because the treatment could be life-long so the cost of therapy would constitute a large portion of their disposable income. If the patient feels that the cost of therapy is a financial burden, the compliance with therapy will definitely be threatened. Healthcare personnel should be aware of patient’s economic situation during the planning of a treatment regimen, and a healthcare finance system that provides at least some financial assistance to low income patients would be helpful to boost compliance.
These factors discussed so far are directly and clearly related to patient’s compliance. We can call them the “hard” factors. We are using this term as the impact of factors identified is more quantifiable. By and large, these “hard” factors are amendable to a certain extent by counseling and communication by healthcare providers. In additional, the society could also participate in minimizing the barriers for patients to follow the therapy.
In contrast with “hard” factors, some other factors might be classified as “soft” factors because their effects are much more difficult to measure and counter. In fact, a failure to address the “soft” factors may negate all efforts spent in countering the effects of the “hard” factors.
Psycho-social factors such as patient’s beliefs, attitude towards therapy and their motivation to the therapy could be classified as “soft” factors. Since the 1990’s, research has focused more on the patient-provider relationship and patients’ beliefs about the therapies. For patients with chronic diseases, they would do their own cost-benefit analysis of therapy, either consciously or subconsciously. It means they weigh the benefits from compliance with therapy (ie, controlling symptoms and preventing medical complications) against constraints on their daily lives and perceived risks of therapy such as side effects, time and effort involved (Donovan and Blake 1992). Sometimes, they may have the wrong beliefs based on inadequate health knowledge or a negative relationship with the healthcare provider. Hence, patients should be given adequate knowledge about the purpose of the therapy and consequences of non-compliance. In addition, a healthy relationship and effective communication between the patient and healthcare provider would enhance patient’s compliance. In fact, the effects of patient’s beliefs, health knowledge and relationship with the healthcare provider are very complex because these “soft” factors are inter-related with each other. The interaction is a bit like antibiotic combinations. Sometimes the effect would be additive or synergistic, while other times the effect would be antagonistic. However, due to the design of the studies performed so far, it is difficult, if not impossible, to differentiate precisely whether the interaction between these factors would be additive, synergistic or antagonistic. More robust and better designed studies would be needed in future to elucidate this effect.
Similar to the “soft” factors, the effect of demographic factors (eg, age, gender, ethnicity, educational level and marital status) on compliance is also rather complicated, because they may not be truly independent factors influencing compliance. Actually, demographic factors are related to patient’s various cultural, socioeconomic and psychological backgrounds. Thus, future studies on compliance should not focus on demographic factors alone.
Definitely, there are some limitations in the current review. Firstly, only one electronic database, PubMed, was searched and only English articles were included. It might be possible that some informative studies in other literature databases or in other languages were omitted. Secondly, there is a shortcoming in the search strategy in that only articles with abstracts were retrieved. There are quite a number of studies published in 1970s and early 1980s without abstracts that were not screened. However, we do believe that the review so far has captured most of the key factors with potential influence on therapeutic compliance from the patient’s perspective.
In conclusion, from the review of the literature starting from the 1970s to identify relevant factors relating to therapeutic compliance, the evidence indicates that non-compliance is still commonplace in healthcare and no substantial change occurred despite the large number of studies attempting to address and highlight the problem. In addition, too few studies are being done systematically to quantify the impact of non-compliance on health and financial outcomes. The magnitude of the impact of non-compliance needs to be studied in future compliance research due to the potential tremendous implication of poor compliance on clinical and economic outcomes. Finally, few studies on compliance have been performed in Asian and developing countries where most of the world’s population resides. More studies on factors influencing compliance in these countries or regions would be helpful to fill in the knowledge gap and contribute to formulating international strategies for countering non-compliance.
References
- Abbott J, Dodd M, Webb AK. Health perceptions and treatment adherence in adults with cystic fibrosis. Thorax. 1996;51:1233–8. doi: 10.1136/thx.51.12.1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alm-Roijer C, Stagmo M, Uden G, et al. Better knowledge improves adherence to lifestyle changes and medication in patients with coronary heart disease. Eur J Cardiovasc Nurs. 2004;3:321–30. doi: 10.1016/j.ejcnurse.2004.05.002. [DOI] [PubMed] [Google Scholar]
- Apter AJ, Reisine ST, Affleck G, et al. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157:1810–7. doi: 10.1164/ajrccm.157.6.9712007. [DOI] [PubMed] [Google Scholar]
- Apter AJ, Boston RC, George M. Modifiable barriers to adherence to inhaled steroids among adults with asthma: it’s not just black and white. J Allergy Clin Immunol. 2003;111:1219–26. doi: 10.1067/mai.2003.1479. [DOI] [PubMed] [Google Scholar]
- Avorn J, Monette J, Lacour A, et al. Persistence of use of lipid-lowering medications: a cross national study. JAMA. 1998;279:1458–62. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- Balbay O, Annakkaya AN, Arbak P, et al. Which patients are able to adhere to tuberculosis treatment? A study in a rural area in the northwest part of Turkey. Jpn J Infect Dis. 2005;58:152–8. [PubMed] [Google Scholar]
- Balkrishnan R, Rajagopalan R, Camacho FT, et al. Predictors of medication adherence and associated health care costs in an older population with type 2 diabetes mellitus: a longitudinal cohort study. Clin Ther. 2003;25:2958–71. doi: 10.1016/s0149-2918(03)80347-8. [DOI] [PubMed] [Google Scholar]
- Barnes L, Moss-Morris R, Kaufusi M. Illness beliefs and adherence in diabetes mellitus: a comparison between Tongan and European patients. N Z Med J. 2004;117:U743. [PubMed] [Google Scholar]
- Bartlett EE, Grayson M, Barker R, et al. The effects of physician communications skills on patient satisfaction; recall, and adherence. J Chronic Dis. 1984;37:755–64. doi: 10.1016/0021-9681(84)90044-4. [DOI] [PubMed] [Google Scholar]
- Bender BG, Bender SE. Patient-identified barriers to asthma treatment adherence: responses to interviews, focus groups, and questionnaires. Immunol Allergy Clin N Am. 2005;25:107–30. doi: 10.1016/j.iac.2004.09.005. [DOI] [PubMed] [Google Scholar]
- Benner JS, Glynn RJ, Mogun H, et al. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–61. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- Berghofer G, Schmidl F, Rudas S, et al. Predictors of treatment discontinuity in outpatient mental health care. Soc Psychiatry Psychiatr Epidemiol. 2002;37:276–82. doi: 10.1007/s001270200020. [DOI] [PubMed] [Google Scholar]
- Bond WS, Hussar DA. Detection methods and strategies for improving medication compliance. Am J Hosp Pharm. 1991;48:1978–88. [PubMed] [Google Scholar]
- Bosley CM, Fosbury JA, Cochrane GM. The psychological factors associated with poor compliance with treatment in asthma. Eur Respir J. 1995;8:899–904. [PubMed] [Google Scholar]
- Buck D, Jacoby A, Baker GA, et al. Factors influencing compliance with antiepileptic drug regimes. Seizure. 1997;6:87–93. doi: 10.1016/s1059-1311(97)80060-x. [DOI] [PubMed] [Google Scholar]
- Burnier M, Santschi V, Favrat B, et al. Monitoring compliance in resistant hypertension: an important step in patient management. J Hypertens Suppl. 2003;21:S37–42. doi: 10.1097/00004872-200305002-00007. [DOI] [PubMed] [Google Scholar]
- Butterworth JR, Banfield LM, Iqbal TH, et al. Factors relating to compliance with a gluten-free diet in patients with coeliac disease: comparison of white Caucasian and South Asian patients. Clin Nutr. 2004;23:1127–34. doi: 10.1016/j.clnu.2004.02.009. [DOI] [PubMed] [Google Scholar]
- Carney RM, Freedland KE, Eisen SA, et al. Major depression and medication adherence in elderly patients with coronary artery disease. Health Psychol. 1995;14:88–90. doi: 10.1037//0278-6133.14.1.88. [DOI] [PubMed] [Google Scholar]
- Caro JJ, Salas M, Speckman JL, et al. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160:31–7. [PMC free article] [PubMed] [Google Scholar]
- Caspard H, Chan AK, Walker AM. Compliance with a statin treatment in a usual-care setting: retrospective database analysis over 3 years after treatment initiation in health maintenance organization enrollees with dyslipidemia. Clin Ther. 2005;27:1639–46. doi: 10.1016/j.clinthera.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Cerkoney KA, Hart LK. The relationship between the health belief model and compliance of persons with diabetes mellitus. Diabetes Care. 1980;3:594–8. doi: 10.2337/diacare.3.5.594. [DOI] [PubMed] [Google Scholar]
- Chan YM, Molassiotis A. The relationship between diabetes knowledge and compliance among Chinese with non-insulin dependent diabetes mellitus in Hong Kong. J Adv Nurs. 1999;30:431–8. doi: 10.1046/j.1365-2648.1999.01098.x. [DOI] [PubMed] [Google Scholar]
- Chizzola PR, Mansur AJ, da Luz PL, et al. Compliance with pharmacological treatment in outpatients from a Brazilian cardiology referral center. Sao Paulo Med J. 1996;114:1259–64. doi: 10.1590/s1516-31801996000500004. [DOI] [PubMed] [Google Scholar]
- Choi-Kwon S, Kwon SU, Kim JS. Compliance with risk factor modification: early-onset versus late-onset stroke patients. Eur Neurol. 2005;54:204–11. doi: 10.1159/000090710. [DOI] [PubMed] [Google Scholar]
- Christensen AJ, Smith TW. Personality and patient adherence: correlates of the five-factor model in renal dialysis. J Behav Med. 1995;18:305–13. doi: 10.1007/BF01857875. [DOI] [PubMed] [Google Scholar]
- Christensen DB. Drug-taking compliance: a review and synthesis. Health Serv Res. 1978;13:171–87. [PMC free article] [PubMed] [Google Scholar]
- Chuah SY. Factors associated with poor patient compliance with antituberculosis therapy in Northwest Perak, Malaysia. Tubercle. 1991;72:261–4. doi: 10.1016/0041-3879(91)90051-s. [DOI] [PubMed] [Google Scholar]
- Clark N, Jones P, Keller S, et al. Patient factors and compliance with asthma therapy. Respir Med. 1999;93:856–62. doi: 10.1016/s0954-6111(99)90050-1. [DOI] [PubMed] [Google Scholar]
- Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther. 2001;23:1296–310. doi: 10.1016/s0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- Cramer JA, Mattson RH, Prevey ML, et al. How often is medication taken as prescribed? A novel assessment technique. JAMA. 1989;261:3273–7. [PubMed] [Google Scholar]
- Cramer JA, Scheyer RD, Mattson RH. Compliance declines between clinic visits. Arch Intern Med. 1990;150:1509–10. [PubMed] [Google Scholar]
- Cramer JA. Enhancing patient compliance in the elderly. Role of packaging aids and monitoring. Drugs Aging. 1998;12:7–15. doi: 10.2165/00002512-199812010-00002. [DOI] [PubMed] [Google Scholar]
- Cochrane GM, Horne R, Chanez P. Compliance in asthma. Respir Med. 1999;93:763–9. doi: 10.1016/s0954-6111(99)90260-3. [DOI] [PubMed] [Google Scholar]
- Cockburn J, Gibberd RW, Reid AL, et al. Determinants of non-compliance with short term antibiotic regimens. Br Med J (Clin Res Ed) 1987;295:814–8. doi: 10.1136/bmj.295.6602.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Combs DL, O’Brien RJ, Geiter LJ, et al. Compliance with tuberculosis regimes: results from USPHS therapy trial 21. Am Rev Respir Dis. 1987;135:A138. [Google Scholar]
- Congressional Budget Office. Prescription drug coverage and Medicare’s fiscal challenges. 2003 [online] Accessed on 1 March 2007.URL: http://www.cbo.gov/showdoc.cfm?index=4159&sequence=0.
- Connelly CE. Compliance with outpatient lithium therapy. Perspect Psychiatr Care. 1984;22:44–50. doi: 10.1111/j.1744-6163.1984.tb00203.x. [DOI] [PubMed] [Google Scholar]
- Cooper C, Carpenter I, Katona C, et al. The AdHOC study of older adults’ adherence to medication in 11 countries. Am J Geriatr Psychiatry. 2005;13:1067–76. doi: 10.1176/appi.ajgp.13.12.1067. [DOI] [PubMed] [Google Scholar]
- Cummings KM, Kirscht JP, Binder LR, et al. Determinants of drug treatment maintenance among hypertensive persons in inner city Detroit. Public Health Rep. 1982;97:99–106. [PMC free article] [PubMed] [Google Scholar]
- De Geest S, Borgermans L, Gemoets H, et al. Incidence, determinants, and consequences of subclinical noncompliance with immunosuppressive therapy in renal transplant recipients. Transplantation. 1995;59:340–7. [PubMed] [Google Scholar]
- Degoulet P, Menard J, Vu HA, et al. Factors predictive of attendance at clinic and blood pressure control in hypertensive patients. Br Med J (Clin Res Ed) 1983;287:88–93. doi: 10.1136/bmj.287.6385.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhanireddy KK, Maniscalco J, Kirk AD. Is tolerance induction the answer to adolescent non-adherence? Pediatr Transplant. 2005;9:357–63. doi: 10.1111/j.1399-3046.2005.00285.x. [DOI] [PubMed] [Google Scholar]
- Didlake RH, Dreyfus K, Kerman RH, et al. Patient noncompliance: a major cause of late graft failure in cyclosporine-treated renal transplants. Transplant Proc. 1988;20:63–9. [PubMed] [Google Scholar]
- Dietrich AJ, Oxman TE, Burns MR, et al. Application of a depression management office system in community practice: a demonstration. J Am Board Fam Pract. 2003;16:107–14. doi: 10.3122/jabfm.16.2.107. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR. Patient adherence to pharmacotherapy: the importance of effective communication. Formulary. 1995;30:596–8. 601–2, 605. [PubMed] [Google Scholar]
- DiMatteo MR. Social support and patient adherence to medical treatment: a meta-analysis. Health Psychol. 2004;23:207–18. doi: 10.1037/0278-6133.23.2.207. [DOI] [PubMed] [Google Scholar]
- Dominick KL, Golightly YM, Bosworth HB. Racial differences in analgesic/anti-inflammatory medication adherence among patients with osteoarthritis. Ethn Dis. 2005;15:116–22. [PubMed] [Google Scholar]
- Donovan JL, Blake DR. Patient non-compliance: deviance or reasoned decision-making? Soc Sci Med. 1992;34:507–13. doi: 10.1016/0277-9536(92)90206-6. [DOI] [PubMed] [Google Scholar]
- Dowse R, Ehlers M. Medicine labels incorporating pictograms: do they influence understanding and adherence? Patient Educ Couns. 2005;58:63–70. doi: 10.1016/j.pec.2004.06.012. [DOI] [PubMed] [Google Scholar]
- Dusing R, Weisser B, Mengden T, et al. Changes in antihypertensive therapy-the role of adverse effects and compliance. Blood Press. 1998;7:313–5. doi: 10.1080/080370598437187. [DOI] [PubMed] [Google Scholar]
- Eisen SA, Miller DK, Woodward RS, et al. The effect of prescribed daily dose frequency on patient medication compliance. Arch Intern Med. 1990;150:1881–4. [PubMed] [Google Scholar]
- Ellis JJ, Erickson SR, Stevenson JG, et al. Suboptimal statin adherence and discontinuation in primary and secondary prevention populations. J Gen Intern Med. 2004;19:638–45. doi: 10.1111/j.1525-1497.2004.30516.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer KC, Jacobs EW, Phillips CR. Long-term patient compliance with prescribed regimens of calcium channel blockers. Clin Ther. 1994;16:316–26. [PubMed] [Google Scholar]
- Feinstein AR. On white-coat effects and the electronic monitoring of compliance. Arch Intern Med. 1990;150:1377–8. [PubMed] [Google Scholar]
- Feinstein S, Keich R, Becker-Cohen R, et al. Is noncompliance among adolescent renal transplant recipients inevitable? Pediatrics. 2005;115:969–73. doi: 10.1542/peds.2004-0211. [DOI] [PubMed] [Google Scholar]
- Fodor GJ, Kotrec M, Bacskai K, et al. Is interview a reliable method to verify the compliance with antihypertensive therapy? An international central-European study. J Hypertens. 2005;23:1261–6. doi: 10.1097/01.hjh.0000170390.07321.ca. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Davis-Ali SH, Dahl KE. Correlates of noncompliance among renal transplant recipients. Clin Transplant. 1994;8:550–7. [PubMed] [Google Scholar]
- Garay-Sevilla ME, Nava LE, Malacara JM, et al. Adherence to treatment and social support in patients with non-insulin dependent diabetes mellitus. J Diabetes Complications. 1995;9:81–6. doi: 10.1016/1056-8727(94)00021-f. [DOI] [PubMed] [Google Scholar]
- Gascon JJ, Sanchez-Ortuno M, Llor B, et al. Treatment Compliance in Hypertension Study Group. Why hypertensive patients do not comply with the treatment: results from a qualitative study. Fam Pract. 2004;21:125–30. doi: 10.1093/fampra/cmh202. [DOI] [PubMed] [Google Scholar]
- Ghods AJ, Nasrollahzadeh D. Noncompliance with immunnosuppressive medications after renal transplantation. Exp Clin Transplant. 2003;1:39–47. [PubMed] [Google Scholar]
- Gonzalez J, Williams JW, Jr, Noel PH, et al. Adherence to mental health treatment in a primary care clinic. J Am Board Fam Pract. 2005;18:87–96. doi: 10.3122/jabfm.18.2.87. [DOI] [PubMed] [Google Scholar]
- Gordis L. Conceptual and methodologic problem in measuring patient compliance. In: Haynes B, Taylor DW, Sackett DL, editors. Compliance in health care. Baltimore: The John Hopkins University Press; 1979. pp. 23–45. [Google Scholar]
- Grant RW, Devita NG, Singer DE, et al. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care. 2003;26:1408–12. doi: 10.2337/diacare.26.5.1408. [DOI] [PubMed] [Google Scholar]
- Grunebaum M, Luber P, Callahan M, et al. Predictors of missed appointments for psychiatric consultations in a primary care clinic. Psychiatr Serv. 1996;47:848–52. doi: 10.1176/ps.47.8.848. [DOI] [PubMed] [Google Scholar]
- Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment and control of hypertension in the United States, 1988-2000. JAMA. 2003;290:199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- Hamburg BA, Inoff GE. Relationships between behavioral factors and diabetic control in children and adolescents: a camp study. Psychosom Med. 1982;44:321–39. doi: 10.1097/00006842-198209000-00002. [DOI] [PubMed] [Google Scholar]
- Haynes RB, Taylor DW, Sackett DL, et al. Can simple clinical measurements detect patient noncompliance? Hypertension. 1980;2:757–64. doi: 10.1161/01.hyp.2.6.757. [DOI] [PubMed] [Google Scholar]
- Hernandez-Ronquillo L, Tellez-Zenteno JF, Garduno-Espinosa J, et al. Factors associated with therapy noncompliance in type-2 diabetes patients. Salud Publica Mex. 2003;45:191–7. doi: 10.1590/s0036-36342003000300008. [DOI] [PubMed] [Google Scholar]
- Hertz RP, Unger AN, Lustik MB. Adherence with pharmacotherapy for type 2 diabetes: a retrospective cohort study of adults with employer-sponsored health insurance. Clin Ther. 2005;27:1064–73. doi: 10.1016/j.clinthera.2005.07.009. [DOI] [PubMed] [Google Scholar]
- Hope CJ, Wu J, Tu W, et al. Association of medication adherence, knowledge, and skills with emergency department visits by adults 50 years or older with congestive heart failure. Am J Health Syst Pharm. 2004;61:2043–9. doi: 10.1093/ajhp/61.19.2043. [DOI] [PubMed] [Google Scholar]
- Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Hungin AP, Rubin G, O’Flanagan H. Factors influencing compliance in long-term proton pump inhibitor therapy in general practice. Br J Gen Pract. 1999;49:463–4. [PMC free article] [PubMed] [Google Scholar]
- Iihara N, Tsukamoto T, Morita S, et al. Beliefs of chronically ill Japanese patients that lead to intentional non-adherence to medication. J Clin Pharm Ther. 2004;29:417–24. doi: 10.1111/j.1365-2710.2004.00580.x. [DOI] [PubMed] [Google Scholar]
- Inkster ME, Donnan PT, MacDonald TM, et al. Adherence to antihypertensive medication and association with patient and practice factors. J Hum Hypertens. 2006;20:295–7. doi: 10.1038/sj.jhh.1001981. [DOI] [PubMed] [Google Scholar]
- International Union Against Tuberculosis Committee on Prophylaxis. Efficacy of various durations of isoniazid preventive therapy for tuberculosis: five years of follow-up in the IUAT trial. Bull World Health Organ. 1982;60:556–64. [PMC free article] [PubMed] [Google Scholar]
- Iskedjian M, Einarson TR, MacKeigan LD, et al. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther. 2002;24:302–16. doi: 10.1016/s0149-2918(02)85026-3. [DOI] [PubMed] [Google Scholar]
- Jeste SD, Patterson TL, Palmer BW, et al. Cognitive predictors of medication adherence among middle-aged and older outpatients with schizophrenia. Schizophr Res. 2003;63:49–58. doi: 10.1016/s0920-9964(02)00314-6. [DOI] [PubMed] [Google Scholar]
- Jette AM, Rooks D, Lachman M, et al. Home-based resistance training: predictors of participation and adherence. Gerontologist. 1998;38:412–21. doi: 10.1093/geront/38.4.412. [DOI] [PubMed] [Google Scholar]
- Kaona FA, Tuba M, Siziya S, et al. An assessment of factors contributing to treatment adherence and knowledge of TB transmission among patients on TB treatment. BMC Public Health. 2004;29:68. doi: 10.1186/1471-2458-4-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplan RC, Bhalodkar NC, Brown EJ, Jr, et al. Race, ethnicity, and sociocultural characteristics predict noncompliance with lipid-lowering medications. Prev Med. 2004;39:1249–55. doi: 10.1016/j.ypmed.2004.04.041. [DOI] [PubMed] [Google Scholar]
- Kass MA, Meltzer DW, Gordon M, et al. Compliance with topical pilocarpine treatment. Am J Ophthalmol. 1986;101:515–23. doi: 10.1016/0002-9394(86)90939-6. [DOI] [PubMed] [Google Scholar]
- Kelloway JS, Wyatt RA, Adlis SA. Comparison of patients’ compliance with prescribed oral and inhaled asthma medications. Arch Intern Med. 1994;154:1349–52. [PubMed] [Google Scholar]
- Kilbourne AM, Reynolds CF, 3, Good CB, et al. How does depression influence diabetes medication adherence in older patients? Am J Geriatr Psychiatry. 2005;13:202–10. doi: 10.1176/appi.ajgp.13.3.202. [DOI] [PubMed] [Google Scholar]
- Kim YS, Sunwoo S, Lee HR, et al. Determinants of non-compliance with lipid-lowering therapy in hyperlipidemic patients. Pharmacoepidemiol Drug Saf. 2002;11:593–600. doi: 10.1002/pds.730. [DOI] [PubMed] [Google Scholar]
- Kiortsis DN, Giral P, Bruckert E, et al. Factors associated with low compliance with lipid-lowering drugs in hyperlipidemic patients. J Clin Pharm Ther. 2000;25:445–51. doi: 10.1046/j.1365-2710.2000.00315.x. [DOI] [PubMed] [Google Scholar]
- Krousel-Wood MA, Thomas S, Muntner P, et al. Medication adherence: a key factor in achieving blood pressure control and good clinical outcomes in hypertensive patients. Curr Opin Cardiol. 2004;19:357–62. doi: 10.1097/01.hco.0000126978.03828.9e. [DOI] [PubMed] [Google Scholar]
- Kyngas HA. Compliance of adolescents with asthma. Nurs Health Sci. 1999;1:195–202. doi: 10.1046/j.1442-2018.1999.00025.x. [DOI] [PubMed] [Google Scholar]
- Kyngas H, Lahdenpera T. Compliance of patients with hypertension and associated factors. J Ad Nurs. 1999;29:832–9. doi: 10.1046/j.1365-2648.1999.00962.x. [DOI] [PubMed] [Google Scholar]
- Kyngas H. Predictors of good compliance in adolescents with epilepsy. Seizure. 2001;10:549–53. doi: 10.1053/seiz.2001.0557. [DOI] [PubMed] [Google Scholar]
- Kyngas H, Rissanen M. Support as a crucial predictor of good compliance of adolescents with a chronic disease. J Clin Nurs. 2001;10:767–74. doi: 10.1046/j.1365-2702.2001.00538.x. [DOI] [PubMed] [Google Scholar]
- Lacasse Y, Archibald H, Ernst P, et al. Patterns and determinants of compliance with inhaled steroids in adults with asthma. Can Respir J. 2005;12:211–7. doi: 10.1155/2005/375454. [DOI] [PubMed] [Google Scholar]
- Lawson VL, Lyne PA, Harvey JN, et al. Understanding why people with type 1 diabetes do not attend for specialist advice: a qualitative analysis of the views of people with insulin-dependent diabetes who do not attend diabetes clinic. J Health Psychol. 2005;10:409–23. doi: 10.1177/1359105305051426. [DOI] [PubMed] [Google Scholar]
- Leggat JE, Jr, Orzol SM, Hulbert-Shearon TE, et al. Noncompliance in hemodialysis: predictors and survival analysis. Am J Kidney Dis. 1998;32:139–45. doi: 10.1053/ajkd.1998.v32.pm9669435. [DOI] [PubMed] [Google Scholar]
- Lertmaharit S, Kamol-Ratankul P, Sawert H, et al. Factors associated with compliance among tuberculosis patients in Thailand. J Med Assoc Thai. 2005;88(Suppl 4):S149–56. [PubMed] [Google Scholar]
- Liam CK, Lim KH, Wong CM, et al. Attitudes and knowledge of newly diagnosed tuberculosis patients regarding the disease, and factors affecting treatment compliance. Int J Tuberc Lung Dis. 1999;3:300–9. [PubMed] [Google Scholar]
- Lim TO, Ngah BA. The Mentakab hypertension study project. Part II – why do hypertensives drop out of treatment? Singapore Med J. 1991;32:249–51. [PubMed] [Google Scholar]
- Lim TO, Ngah BA, Rahman RA, et al. The Mentakab hypertension study project Part V – Drug compliance in hypertensive patients. Singapore Med J. 1992;33:63–6. [PubMed] [Google Scholar]
- Lindberg M, Ekstrom T, Moller M, et al. Asthma care and factors affecting medication compliance: the patient’s point of view. Int J Qual Health Care. 2001;13:375–83. doi: 10.1093/intqhc/13.5.375. [DOI] [PubMed] [Google Scholar]
- Linden M, Gothe H, Dittmann RW, et al. Early termination of antidepressant drug treatment. J Clin Psychopharmacol. 2000;20:523–30. doi: 10.1097/00004714-200010000-00005. [DOI] [PubMed] [Google Scholar]
- Loffler W, Kilian R, Toumi M, et al. Schizophrenic patients’ subjective reasons for compliance and noncompliance with neuroleptic treatment. Pharmacopsychiatry. 2003;36:105–12. doi: 10.1055/s-2003-39985. [DOI] [PubMed] [Google Scholar]
- Loong TW. Primary non-compliance in a Singapore polyclinic. Singapore Med J. 1999;40:691–3. [PubMed] [Google Scholar]
- Lorenc L, Branthwaite A. Are older adults less compliant with prescribed medication than younger adults? Br J Clin Psychol. 1993;32:485–92. doi: 10.1111/j.2044-8260.1993.tb01084.x. [DOI] [PubMed] [Google Scholar]
- Matthews D, Hingson R. Improving patient compliance: a guide for physicians. Med Clin North Am. 1977;61:879–89. doi: 10.1016/s0025-7125(16)31304-9. [DOI] [PubMed] [Google Scholar]
- McLane CG, Zyzanski SJ, Flocke SA. Factors associated with medication noncompliance in rural elderly hypertensive patients. Am J Hypertens. 1995;8:206–9. doi: 10.1016/0895-7061(94)00194-G. [DOI] [PubMed] [Google Scholar]
- Menzies R, Rocher I, Vissandjee B. Factors associated with compliance in treatment of tuberculosis. Tuber Lung Dis. 1993;74:32–7. doi: 10.1016/0962-8479(93)90066-7. [DOI] [PubMed] [Google Scholar]
- Milas NC, Nowalk MP, Akpele L, et al. Factors associated with adherence to the dietary protein intervention in the Modification of Diet in Renal Disease Study. J Am Diet Assoc. 1995;95:1295–300. doi: 10.1016/s0002-8223(95)00340-1. [DOI] [PubMed] [Google Scholar]
- Mishra P, Hansen EH, Sabroe S, et al. Socio-economic status and adherence to tuberculosis treatment: a case-control study in a district of Nepal. Int J Tuberc Lung Dis. 2005;9:1134–9. [PubMed] [Google Scholar]
- Monane M, Bohn RL, Gurwitz JH, et al. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86:1805–8. doi: 10.2105/ajph.86.12.1805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore PJ, Sickel AE, Malat J, et al. Psychosocial factors in medical and psychological treatment avoidance: the role of the doctor-patient relationship. J Health Psychol. 2004;9:421–33. doi: 10.1177/1359105304042351. [DOI] [PubMed] [Google Scholar]
- Murray MD, Darnell J, Weinberger M, et al. Factors contributing to medication noncompliance in elderly public housing tenants. Drug Intell Clin Pharm. 1986;20:146–52. doi: 10.1177/106002808602000210. [DOI] [PubMed] [Google Scholar]
- Neal RD, Hussain-Gambles M, Allgar VL, et al. Reasons for and consequences of missed appointments in general practice in the UK: questionnaire survey and prospective review of medical records. BMC Fam Pract. 2005;6:47. doi: 10.1186/1471-2296-6-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neeleman J, Mikhail WI. A case control study of GP and patient-related variables associated with nonattendance at new psychiatric outpatient appointments. J Mental Health. 1997;6:301–6. [Google Scholar]
- Nichols-English G, Poirier S. Optimizing adherence to pharmaceutical care plans. J Am Pharm Assoc. 2000;40:475–85. [PubMed] [Google Scholar]
- Nikolaus T, Kruse W, Bach M, et al. Elderly patients’ problems with medication. An in-hospital and follow-up study. Eur J Clin Pharmacol. 1996;49:255–9. doi: 10.1007/BF00226324. [DOI] [PubMed] [Google Scholar]
- Norman SA, Marconi KM, Schezel GW, et al. Beliefs, social normative influences, and compliance with antihypertensive medication. Am J Prev Med. 1985;1:10–7. [PubMed] [Google Scholar]
- O’Donoghue MN. Compliance with antibiotics. Cutis. 2004;73(Suppl 5):30–2. [PubMed] [Google Scholar]
- Okuno J, Yanagi H, Tomura S, et al. Compliance and medication knowledge among elderly Japanese home-care recipients. Eur J Clin Pharmacol. 1999;55:145–9. doi: 10.1007/s002280050609. [DOI] [PubMed] [Google Scholar]
- Okuno J, Yanagi H, Tomura S. Is cognitive impairment a risk factor for poor compliance among Japanese elderly in the community? Eur J Clin Pharmacol. 2001;57:589–94. doi: 10.1007/s002280100347. [DOI] [PubMed] [Google Scholar]
- Olubodun JOB, Falase AO, Cole TO. Drug compliance in hypertensive Nigerians with and without heart failure. Int J Cardiol. 1990;27:229–34. doi: 10.1016/0167-5273(90)90164-z. [DOI] [PubMed] [Google Scholar]
- Opolka JL, Rascati KL, Brown CM, et al. Role of ethnicity in predicting antipsychotic medication adherence. Ann Pharmacother. 2003;37:625–30. doi: 10.1345/aph.1C321. [DOI] [PubMed] [Google Scholar]
- Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- Oxford advanced learner’s dictionary of current English. 7. Oxford: Oxford University Press; 2005. p. 296. compliance. [Google Scholar]
- Patal RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother. 2002;36:40–5. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- Ponnusankar S, Surulivelrajan M, Anandamoorthy N, et al. Assessment of impact of medication counseling on patients’ medication knowledge and compliance in an outpatient clinic in South India. Patient Educ Couns. 2004;54:55–60. doi: 10.1016/S0738-3991(03)00193-9. [DOI] [PubMed] [Google Scholar]
- Raiz LR, Kilty KM, Henry ML. Medication compliance following renal transplantation. Transplantation. 1999;68:51–5. doi: 10.1097/00007890-199907150-00010. [DOI] [PubMed] [Google Scholar]
- Rubin RR. Adherence to pharmacologic therapy in patients with type 2 diabetes mellitus. Am J Med. 2005;118:27s–34s. doi: 10.1016/j.amjmed.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the Health Belief Model. Health Educ Q. 1988;15:175–83. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Roter DL, Hall JA. Why physician gender matters in shaping the physician-patient relationship. J Womens Health. 1998;7:1093–7. doi: 10.1089/jwh.1998.7.1093. [DOI] [PubMed] [Google Scholar]
- Sabaté E, editor. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization; 2003. [Google Scholar]
- Sackett DL. Introduction. In: Sackett DL, Haynes RB, editors. Compliance with therapeutic regimens. Baltimore: Johns Hopkins University Press; 1976. pp. 1–6. [Google Scholar]
- Sackett DL, Haynes RB, Gibson ES, et al. Randomised clinical trial of strategies for improving medication compliance in primary hypertension. Lancet. 1975;1:1205–7. doi: 10.1016/s0140-6736(75)92192-3. [DOI] [PubMed] [Google Scholar]
- Sanson-Fisher R, Bowman J, Armstrong S. Factors affecting nonadherence with antibiotics. Diagn Microbiol Infect Dis. 1992;15:103S–109S. doi: 10.1016/0732-8893(92)90136-h. [DOI] [PubMed] [Google Scholar]
- Schweizer RT, Rovelli M, Palmeri D, et al. Noncompliance in organ transplant recipients. Transplantation. 1990;49:374–7. doi: 10.1097/00007890-199002000-00029. [DOI] [PubMed] [Google Scholar]
- Segador J, Gil-Guillen VF, Orozco D, et al. The effect of written information on adherence to antibiotic treatment in acute sore throat. Int J Antimicrob Agents. 2005;26:56–61. doi: 10.1016/j.ijantimicag.2005.03.009. [DOI] [PubMed] [Google Scholar]
- Senior V, Marteau TM, Weinman J. Self-reported adherence to cholesterol-lowering medication in patients with familial hypercholesterolaemia: the role of illness perceptions. Cardiovasc Drugs Ther. 2004;18:475–81. doi: 10.1007/s10557-004-6225-z. [DOI] [PubMed] [Google Scholar]
- Seo MA, Min SK. Development of a structural model explaining medication compliance of persons with schizophrenia. Yonsei Med J. 2005;46:331–40. doi: 10.3349/ymj.2005.46.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw E, Anderson JG, Maloney M, et al. Factors associated with noncompliance of patients taking antihypertensive medications. Hosp Pharm. 1995;30:201–3. 206–7. [PubMed] [Google Scholar]
- Sharkness CM, Snow DA. The patient’s view of hypertension and compliance. Am J Prev Med. 1992;8:141–6. [PubMed] [Google Scholar]
- Shea S, Misra D, Ehrlich MH, et al. Correlates of nonadherence to hypertension treatment in an inner-city minority population. Am J Public Health. 1992;82:1607–12. doi: 10.2105/ajph.82.12.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegal B, Greenstein SJ. Compliance and noncompliance in kidney transplant patients: cues for transplant coordinators. Transpl Coord. 1999;9:104–8. doi: 10.7182/prtr.1.9.2.a67514546814h767. [DOI] [PubMed] [Google Scholar]
- Sirey JA, Bruce ML, Alexopoulos GS, et al. Stigma as a barrier to recovery: Perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52:1615–20. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- Sleath B, Wurst K, Lowery T. Drug information sources and antidepressant adherence. Community Ment Health J. 2003;39:359–68. doi: 10.1023/a:1024080410284. [DOI] [PubMed] [Google Scholar]
- Sloan JP, Sloan MC. An assessment of default and non-compliance in tuberculosis control in Pakistan. Trans R Soc Trop Med Hyg. 1981;75:717–8. doi: 10.1016/0035-9203(81)90161-9. [DOI] [PubMed] [Google Scholar]
- Sokol MC, McGuigan KA, Verbrugge RR, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- Spagnoli A, Ostino G, Borga AD, et al. Drug compliance and unreported drugs in the elderly. J Am Geriatr Soc. 1989;37:619–24. doi: 10.1111/j.1532-5415.1989.tb01252.x. [DOI] [PubMed] [Google Scholar]
- Spikmans FJ, Brug J, Doven MM, et al. Why do diabetic patients not attend appointments with their dietitian? J Hum Nutr Diet. 2003;16:151–8. doi: 10.1046/j.1365-277x.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- Stanton AL. Determinants of adherence to medical regimens by hypertensive patients. J Behav Med. 1987;10:377–94. doi: 10.1007/BF00846477. [DOI] [PubMed] [Google Scholar]
- Stewart RB, Caranasos GJ. Medication compliance in the elderly. Med Clin North Am. 1989;73:1551–63. doi: 10.1016/s0025-7125(16)30616-2. [DOI] [PubMed] [Google Scholar]
- Stilley CS, Sereika S, Muldoon MF, et al. Psychological and cognitive function: predictors of adherence with cholesterol lowering treatment. Ann Behav Med. 2004;27:117–24. doi: 10.1207/s15324796abm2702_6. [DOI] [PubMed] [Google Scholar]
- Stromberg A, Brostrom A, Dahlstrom U, et al. Factors influencing patient compliance with therapeutic regimens in chronic heart failure: A critical incident technique analysis. Heart Lung. 1999;28:334–41. doi: 10.1053/hl.1999.v28.a99538. [DOI] [PubMed] [Google Scholar]
- Sung JC, Nichol MB, Venturini F, et al. Factors affecting patient compliance with antihyperlipidemic medications in an HMO population. Am J Manag Care. 1998;4:1421–30. [PubMed] [Google Scholar]
- Svarstad BL, Shireman TI, Sweeney JK. Using drug claims data to assess the relationship of medication adherence with hospitalization and costs. Psychiatr Serv. 2001;52:805–11. doi: 10.1176/appi.ps.52.6.805. [DOI] [PubMed] [Google Scholar]
- Swett C, Jr, Noones J. Factors associated with premature termination from outpatient treatment. Hosp Community Psychiatry. 1989;40:947–51. doi: 10.1176/ps.40.9.947. [DOI] [PubMed] [Google Scholar]
- Tebbi CK, Cummings KM, Zevon MA, et al. Compliance of pediatric and adolescent cancer patients. Cancer. 1986;58:1179–84. doi: 10.1002/1097-0142(19860901)58:5<1179::aid-cncr2820580534>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- Tebbi CK. Treatment compliance in childhood and adolescence. Cancer. 1993;71:3441–9. doi: 10.1002/1097-0142(19930515)71:10+<3441::aid-cncr2820711751>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Thomas LK, Sargent RG, Michels PC, et al. Identification of the factors associated with compliance to therapeutic diets in older adults with end stage renal disease. J Ren Nutr. 2001;11:80–9. doi: 10.1016/s1051-2276(01)98615-7. [DOI] [PubMed] [Google Scholar]
- Turner J, Wright E, Mendella L, et al. Predictors of patient adherence to long-term home nebulizer therapy for COPD. Chest. 1995;108:394–400. doi: 10.1378/chest.108.2.394. [DOI] [PubMed] [Google Scholar]
- Vermeire E, Hearnshaw H, Van Royen P, et al. Patient adherence to treatment: three decades of research A comprehensive review. J Clin Pharm Therap. 2001;26:331–42. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- Vic SA, Maxwell CJ, Hogan DB. Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother. 2004;38:303–12. doi: 10.1345/aph.1D252. [DOI] [PubMed] [Google Scholar]
- Viller F, Guillemin F, Briancon S, et al. Compliance to drug treatment of patients with rheumatoid arthritis: a 3 year longitudinal study. J Rheumatol. 1999;26:2114–22. [PubMed] [Google Scholar]
- Vincze G, Barner JC, Lopez D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ. 2004;30:112–25. doi: 10.1177/014572170403000119. [DOI] [PubMed] [Google Scholar]
- Vlasnik JJ, Aliotta SL, DeLor B. Medication adherence: factors influencing compliance with prescribed medication plans. Case Manager. 2005;16:47–51. doi: 10.1016/j.casemgr.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Voils CI, Steffens DC, Flint EP, et al. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. Am J Geriatr Psychiatry. 2005;13:157–65. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- Wai CT, Wong ML, Ng S, et al. Utility of the Health Belief Model in predicting compliance of screening in patients with chronic hepatitis B. Aliment Pharmacol Ther. 2005;21:1255–62. doi: 10.1111/j.1365-2036.2005.02497.x. [DOI] [PubMed] [Google Scholar]
- Wild MR, Engleman HM, Douglas NJ, et al. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24:461–5. doi: 10.1183/09031936.04.00114603. [DOI] [PubMed] [Google Scholar]
- Yavuz A, Tuncer M, Erdogan O, et al. Is there any effect of compliance on clinical parameters of renal transplant recipients? Transplant Proc. 2004;36:120–1. doi: 10.1016/j.transproceed.2003.11.052. [DOI] [PubMed] [Google Scholar]
- Yu YF, Nichol MB, Yu AP, et al. Persistence and adherence of medications for chronic overactive bladder/urinary incontinence in the California medicaid program. Value Health. 2005;8:495–505. doi: 10.1111/j.1524-4733.2005.00041.x. [DOI] [PubMed] [Google Scholar]