Abstract
Adult traumatic brachial plexus injuries can have devastating effects on upper extremity function. Although neurolysis, nerve repair, and nerve grafting have been used to treat injuries to the plexus, nerve transfer makes use of an undamaged nerve to supply motor input over a relatively short distance to reinnervate a denervated muscle. A review of several recent innovations in nerve transfer surgery for brachial plexus injuries is illustrated with surgical cases performed at this institution.
Key words: adult, brachial plexus, nerve transfer, microsurgery, nerve repair
Introduction
Over the past century, our understanding of nerve injury, regeneration, and repair techniques has evolved. Historical options for treatment of adult traumatic brachial plexus palsy have included neurolysis, nerve repair, or nerve grafting. However, because of the frequency of avulsion-type injuries, the lack of available nerve roots for grafting, and the extensive scarring at the injury site, these treatment options are frequently inadequate to restore function in the severely affected patient.
Isolated neurolysis has been shown to be effective only if scar tissue within the epineurium or surrounding the nerve is the demonstrable barrier to recovery or alleviation of pain [1]. Nerve repair, although an excellent option for treating sharply transected peripheral nerves [2], is usually not possible in nonpenetrating traumatic brachial plexus injuries [3]. Traumatic brachial plexus palsy is usually caused by traction across long segments of the trunks, divisions or cords, and may be segmental in nature. Grafting of small segments of ruptured nerves can be performed using donor peripheral nerves, but brachial plexus lesions often necessitate long graft lengths and most studies indicate that shorter grafts (<10 cm) result in more successful outcomes [4–7]. Nerve transfer (neurotization) employs redirection of an intact motor nerve from one muscle to the distal undamaged portion of a nerve from another, effectively bypassing the injured segment of nerve. Several recently described nerve transfers have been effectively employed and preliminary outcomes reported.
Spinal accessory nerve transfer
The spinal accessory nerve is a pure motor nerve, which innervates the sternocleidomastoid and trapezius muscles. It is essential to protect branches to the upper and middle trapezius to preserve function when this nerve is used as a donor. Proximity of the spinal accessory nerve to the suprascapular nerve allows direct microapproximation without graft. Although transfers to the more distal musculocutaneous nerve and axillary nerves have been described, both require use of an interpositional nerve graft [8]. Nerve transfers to the shoulder and elbow have been shown to be significantly more effective when performed without an intercalated nerve graft [9].
Technique Supraclavicular exposure is performed using a 15-cm necklace incision [10, 11] situated 1 cm above and parallel to the clavicle. Division of the platysma allows supraclavicular nerve identification and preservation. The spino-accessory nerve is identified just deep to the supero-lateral margin of the trapezius near the clavicle and traced distally to its bifurcation. Nerve stimulation and contractility of the trapezius confirms viability of the spinal accessory nerve. The distal portion of the spinal accessory nerve is divided sharply and the end coapted to that of the recipient suprascapular nerve using 8-0 or 9-0 nylon sutures and microscopic magnification.
Intercostal nerve transfer
In 1988, Narakas described his extensive experience using intercostal nerves as donor nerves for brachial plexus neurotization [12]. Intercostal nerves are satisfactory donors for a variety of transfers; they are harvested via a thoracic exposure and subperiosteal dissection along the inferior surface of the ribs. However, their precarious location, especially in the setting of high-energy trauma, can preclude availability; they are often injured by placement of chest tubes or by rib fractures and associated callus. Further, the intercostal nerves are a mixed motor and sensory nerve with a finite number of available axons, necessitating transfer of multiple nerves to any particular recipient nerve. Because of improved results with interplexal nerve transfers such as those that employ a fascicle of the pectoral, ulnar, or median nerves, transfer of intercostal nerves for elbow or shoulder reinnervation is now reserved for use when other available donor nerves are unavailable or injured.
Technique A long incision beginning high in the axilla and running inferiorly along the midthoracic line is curved beneath the ipsilateral nipple, corresponding to the inferior margin of the fifth rib. The pectoralis major muscle is reflected medially and superiorly, and slips of the serratus are bluntly divided to expose each rib. Electrocautery is used to open the periosteal sleeve, and a curved Adson elevator used to dissect the periosteum from the internal surface of the rib. Sharp dissection through the periosteum identifies the intercostal nerve and intimately associated artery; extreme care should be used so as not to perforate the pleura, which lies immediately deep to the nerves. Exposure can be improved by the use of a Kerrison rongeur to remove the inferior margin of the rib, particularly in the more superior ribs, which are broader and beneath which the nerves tend to run more superiorly. The nerves are stimulated to identify the motor branch and traced to the anterior nipple line. Both motor and sensory portions are tagged for later direct approximation to motor and sensory (usually median) nerve recipients.
Triceps nerve branch to axillary nerve
Functional restoration of shoulder abduction can be achieved by transferring a nerve branch of the long head, lateral head [13], or medial head (MacKinnon SE and Oberlin C, personal communication) of the triceps muscle to the distal deltoid motor branch of the damaged axillary nerve; the anatomic and clinical feasibility of this was described in 2003 [14]. Use of a single branch does not sacrifice elbow extension as evidenced by its recognized use in muscle flaps [15, 16].
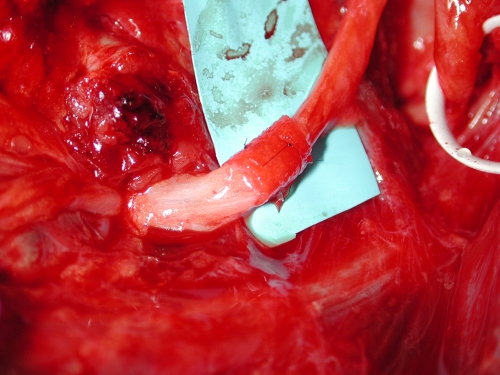
Technique A posterior incision 15 cm long over the sulcus between the lateral and long heads of the triceps is made, and the radial nerve is identified deep between the long head and the lateral head of the triceps. Branches are elevated and stimulated to confirm branching to medial, long, and lateral heads. The teres major fascia is divided to allow for more proximal dissection. The axillary nerve is located in the quadrangular space and traced to identify the branch of the teres minor, posterior deltoid, anterior branch to the skin, and the branch to the anterior and middle deltoid. A suitable branch to one head of the triceps is divided distally and reflected to directly approximate the motor branch of the axillary nerve. Recent work suggests that the deep (medial) head branch is longer and a more robust axonal contribution for axillary reinnervation (MacKinnon SE, Oberlin C, personal communication). If a size discrepancy exists, a nerve conduit can be used for better approximation and grouping of the fascicles (Fig. 1).
Fig. 1.
A radial nerve branch to the long head of triceps was transferred to the axillary nerve using nerve conduit
Ulnar nerve to musculocutaneous nerve transfer
Christophe Oberlin described transfer of one or more ulnar nerve fascicles to the motor branch(es) of the biceps muscle [17]. This is performed to restore elbow flexion in patients who have an irreparable upper trunk injury or avulsion, and an intact lower trunk [18]. Careful selection of ulnar nerve fascicles using intraoperative nerve stimulation enables one to perform this transfer without a donor motor or sensory deficit.
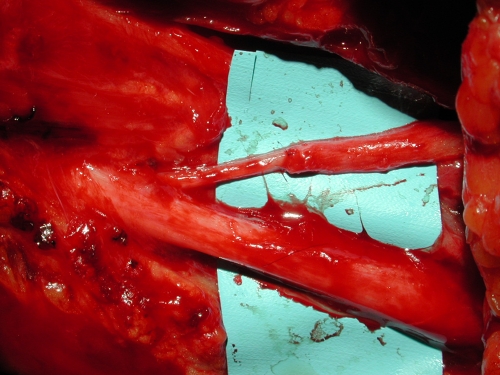
Technique A 15-cm incision is made along the medial arm beginning at the pectoralis and coursing distally along the neurovascular bundle. The biceps fascia is opened and the musculocutaneous nerve identified. The motor branches to both heads of the biceps are identified approximately 12 cm distal to the acromion and stimulated to ensure complete denervation; the branches are traced proximally where they usually coalesce into a single motor branch from the parent musculocutaneous nerve, and then divided sharply for transfer to the ulnar nerve. The ulnar nerve is identified by external neurolysis, and the epineurium is opened. Several fascicles of the ulnar nerve are chosen 3–4 cm distal to the level of the MC branch to the biceps and stimulated with a portable nerve stimulation unit. A single large fascicle can usually be identified to produce maximal contraction of the flexor carpi ulnaris without significant contraction of the ulnar intrinsic muscles. This fascicle (or fascicles) are divided far enough distally to transfer directly to the motor branch(es) of the musculocutaneous nerve (Fig. 2).
Fig. 2.
Ulnar nerve fascicle was transferred to the musculocutaneous nerve (Oberlin transfer) to achieve biceps function
Double fascicular transfer for elbow flexion
Mackinnon reported on six patients who had direct transfer of motor fascicles from both the ulnar and median nerves to the biceps and brachialis branches of the musculocutaneous nerve, respectively [19]. Reinnervation was noted at 5.5 months, and mean elbow flexion recovery was 4+. No motor or sensory morbidity was noted postoperatively in any of the patients. The authors have observed that double nerve transfer increases the rate and success of recovery of elbow flexion over single nerve transfer.
Medial pectoral nerve transfer for elbow flexion
Transfer of the medial pectoral nerve to the musculocutaneous nerve innervating the biceps was described anatomically and clinically by Brandt and MacKinnon [20, 21]. The proximity of the normal medial pectoral motor nerve to the musculocutaneous recipient provides a theoretical advantage toward early recovery; Brandt confirmed that biceps reinnervation occurred between 6 and 8 months postoperatively.
Case reports
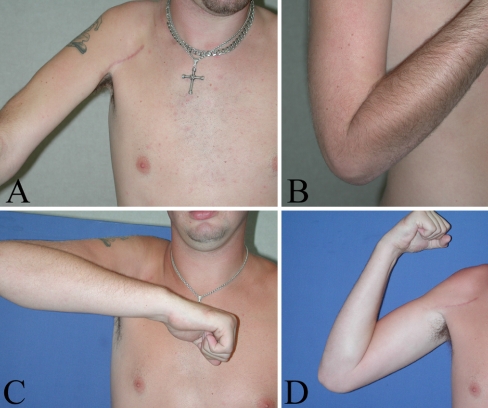
Case 1 The patient is a 20-year-old right-hand-dominant male who sustained an injury to the upper trunk of his right brachial plexus. Five months postinjury, intraoperative nerve stimulation revealed normal conduction of the ulnar, median, radial, medial pectoral, and spinal accessory nerves, but no conduction of the suprascapular, axillary, and musculocutaneous nerves. Transfer of a branch of the ulnar nerve to the motor branch of the biceps for elbow flexion, transfer of a branch of the medial pectoral to the axillary nerve for deltoid and teres function, transfer of a spinal accessory nerve branch to the suprascapular nerve for dual innervation of the shoulder [9], and transfer of the second intercostal nerve to the distal end of the long thoracic nerve for serratus anterior function were performed. He began therapy within 4 weeks of surgery to maintain passive mobility of all the reinnervated articulations. When active contractions were detected, he began a strengthening program for the serratus anterior, deltoid, biceps, triceps, supraspinatus, and infraspinatus.By 6 months postoperatively, he reported very little pain and resolution of hand dysesthesias. He had returned to work at 4 months postoperatively. Examination revealed a visible and palpable contraction of his biceps with hand grasp, but no elbow flexion. The deltoid visibly twitched with pectoralis firing. Twelve months after surgery, scapular winging had resolved, and he had achieved 135° of elbow flexion, shoulder abduction to 40° and shoulder forward flexion to 60°. Deltoid contraction power was 2/5, suprascapular 3/5, and biceps 5-/5. At 18 months, he demonstrated full elbow flexion and extension with 5-/5 strength, shoulder abduction to 90° with 4-/5 strength, shoulder external rotation to 80° with 4-/5 strength, and serratus anterior strength of 4/5. He continues running his own patio construction company (Fig. 3).
Fig. 3.
Shoulder abduction and elbow flexion 1 year (A and B, respectively) and 2 years (C and D, respectively) postoperatively demonstrate improvement over time
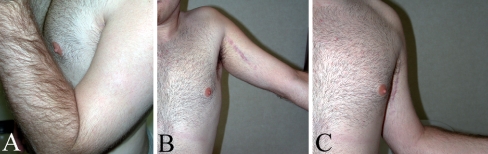
Case 2 The patient is a 21-year-old right-hand-dominant male who sustained a left brachial plexus injury. He presented for treatment 4 months postinjury, with marked atrophy about the supra- and infraspinatus, mild to moderate subacromial subluxation, substantial atrophy of the left biceps, but no appreciable atrophy of the forearm or hand. Motor testing revealed absent (0/5) function of deltoids, supraspinatus, infraspinatus, brachioradialis, and biceps (Table 1), but normal spinal accessory nerve function was demonstrated. Intraoperative nerve stimulation 5 months postinjury indicated no function of the suprascapular, axillary nerves, and musculocutaneous nerves. He underwent exploration and neurolysis of the brachial plexus, transfer of the terminal branches of the spinal accessory to the suprascapular nerve, transfer of an ulnar nerve fascicle to the biceps motor branch, transfer of a median nerve fascicle to the brachialis motor branch, and a transfer of the triceps long head branch to the deltoid motor branch. By 5 months postoperatively, he generated 20° of abduction through an early functioning deltoid. Brachialis was palpable and functional, as flexion past 90° and supination in both extended and flexed positions was achieved. By 9 months, he demonstrated elbow flexion to 135°, shoulder external rotation to 80°, and shoulder abduction to 30° (Fig. 4). He continues a home therapy program.
Table 1.
Initial (preoperative) motor examination of patient in case 2
| Muscle | Strength |
|---|---|
| Trapezius | 5/5 |
| Serratus | 5/5 |
| Rhomboids | 5/5 |
| Latissimus | 5/5 |
| Deltoids | 0/5 |
| Supraspinatus | 0/5 |
| Infraspinatus | 0/5 |
| Pectoralis | 5/5 |
| Biceps | 0/5 |
| Triceps | 5/5 |
| Brachioradialis | 0/5 |
| Pronator | 5/5 |
| Flexor carpi radialis | 5/5 |
| Flexor sublimes | 5/5 |
| Flexor profundus | 5/5 |
| Flexor pollicis | 5/5 |
| Extensor digitorum communis | 5/5 |
| Extensor carpi radialis longus | 5/5 |
| Extensor carpi ulnaris | 5/5 |
| Extensor pollicis longus | 5/5 |
| Intrinsics | 5/5 |
Fig. 4.
Elbow flexion (A), shoulder abduction (B), and shoulder external rotation (C) are noted at 9 months postoperatively
Discussion
Prioritization of reconstruction varies by surgeon preference; in general, the primary functional priority is restoration of elbow flexion, followed by shoulder abduction, then hand sensibility and prehension [8].
Early results of elbow flexion restoration using intercostal transfer to the musculocutaneous nerve demonstrated 66% success [22]; this was confirmed with a metaanalysis of 1,088 nerve transfers conducted by the senior author in 2001 [9], which showed 72% of intercostal to musculocutaneous nerve transfers exhibiting M ≥ 3 and 37% M ≥ 4 bicep function. More recently, an average of 80% success (M ≥ 3) was reported [23]. Milestone physical findings include the elicitation of chest pain by squeezing of the biceps muscle at approximately 3 months postoperatively, visible biceps contraction (M1) during deep inspiration at 6 months, and antigravity elbow flexion within 18 months of surgery [23]. Some series have reported up to 65% antigravity elbow flexion within 12 months, and that voluntary biceps control was no longer dependent on the respiratory cycle by 3 years after surgery. [8]
Despite the encouraging results with intercostal nerve transfer, greater functional success has been achieved more recently by transferring intact branches of the ulnar or median nerves directly to the motor branches of the biceps and/or brachialis. Early results demonstrated 75 to 100% of patients achieved antigravity (M3) biceps strength or better, and recent results show between 75 and 94% M4 strength [17,24–26]. In 2005, Mackinnon reported M4 or better strength of elbow flexion in six patients in her series with dual transfers for elbow flexion, with clinical reinnervation noted at a mean of 5.5 months [19].
Shoulder abduction generally is accomplished by dual nerve transfers to restore strength of supraspinatus, infraspinatus, and deltoid muscles [9,10]. Results of a metaanalysis by Merrell et al. showed that dual transfers to restore shoulder function (to suprascapular and axillary nerves) yielded significantly improved results when compared with single nerve transfer [9]. In that study, successful transfers to the suprascapular nerve (92%) outnumber those to the axillary nerve (69%) [9]. Chuang recently reported 60° of abduction in patients with root avulsions and 90° or more in patients with upper root avulsions using a combination of nerve transfers for shoulder abduction [23]. In a series of 577 spinal accessory nerve transfers, Songcharoen described 80% motor recovery (M ≥ 3) with transfer to suprascapular nerve, obtaining 60° of shoulder abduction and 45° shoulder flexion. In the same series, spinal accessory transfer to axillary only achieved 60% success; the poorer results may be attributed to the longer reinnervation distance and the requisite need for interpositional nerve grafts [8]. The phrenic nerve has been transferred to the suprascapular nerve without grafting, achieving grade 3 muscle recovery within 8 months [8]; however, phrenic nerve harvest has the potential to compromise diaphragmatic and pulmonary function, and is often contraindicated in patients who have had chest trauma. The most recent nerve transfer innovation for shoulder abduction involves the use of a single triceps branch of the radial nerve, transferred directly to the motor branch of the axillary. Leechavengvongs reported excellent results in five of seven cases using the long head branch of the radial nerve branch to axillary nerve, with a mean shoulder abduction of 124° by 28 months [27]. Most authors today would agree that a powerful combination of transfers for shoulder abduction includes the spino-accessory to suprascapular nerve and a triceps branch to axillary nerve.
Restoration of function below the elbow remains a challenge. Intrinsic muscle function and wrist or digital flexion cannot readily be restored by nerve transfers. Neurotization of the median nerve to obtain sensation and finger flexion is a potential surgical alternative, as is staged double-functioning free-muscle transplantation. [23,28,29]. All or a portion of the contralateral C7 nerve root can be transferred to the median nerve; a series of 111 such transfers yielded 30% M3 and 20% M2 function. Despite the discouraging motor results, 83% obtained protective sensory recovery (50% S3 and 33% S2) after this procedure [8].
Conclusions
Treatment of adult traumatic brachial plexus injuries remains a difficult problem. Early intervention can enable functional recovery of shoulder and elbow function in the majority of patients. Nerve transfer techniques to restore shoulder and elbow function has revolutionized the care of these challenging injuries, and has yielded superior results to historical reports for nerve grafting of plexus injuries. A patient registry is currently in use to track patients and their outcomes in an effort to improve management of these devastating injuries.
Footnotes
Approval obtained from Hospital for Special Surgery Institutional Review Board
Level IV: series with no or a historical control group.
References
- 1.Narakas A (1981) Brachial plexus surgery. Orthop Clin North Am 12(2):303–323 [PubMed]
- 2.Kline DG, Tiel RL (2005) Direct plexus repair by grafts supplemented by nerve transfers. Hand Clin 21:55–69 [DOI] [PubMed]
- 3.Brophy RH, Wolfe SW (2005) Planning brachial plexus surgery: treatment options and priorities. Hand Clin 21(1):47–54 [DOI] [PubMed]
- 4.Bentolila V, Nizard R, Bizot P, et al. (1999) Complete traumatic brachial plexus palsy: Treatment and outcome after repair. J Bone Jt Surg 81-A(1):20–28 [DOI] [PubMed]
- 5.Samii M, Carvalho GA, Nikkhah G, et al. (1997) Surgical reconstruction of the musculocutaneous nerve in traumatic brachial plexus injuries. J Neurosurg 87(6):881–886 [DOI] [PubMed]
- 6.Chuang DC, Epstein MD, Yeh MC, et al. (1993) Functional restoration of elbow flexion in brachial plexus injuries: Results in 167 patients (excluding obstetric brachial plexus injury). J Hand Surg 18A(2):285–291 [DOI] [PubMed]
- 7.Hentz VR, Narakas A (1988) The results of microneurosurgical reconstruction in complete brachial plexus palsy: Assessing outcome and predicting results. Orthop Clin North Am 19(1):107–114 [PubMed]
- 8.Songcharoen P, Wongtrakul S, Spinner RJ (2005) Brachial plexus injuries in the adult. Nerve transfers: The Siriraj Hospital experience. Hand Clin 21:83–89 [DOI] [PubMed]
- 9.Merrell GA, Barrie KA, Katz DL, et al. (2001) Results of nerve transfer techniques for restoration of shoulder and elbow function in the context of a meta-analysis of the English literature. J Hand Surg 26A:303–314 [DOI] [PubMed]
- 10.Merrell GA, Wolfe SW (2002) Adult brachial plexus and thoracic outlet surgery. Tech Should Elb Surg 3(4):271–281 [DOI]
- 11.Birch R, Bonney G, Wynn Parry CB (1998) Traumatic lesions of the brachial plexus. In: Surgical disorders of the peripheral nerves. Churchill Livingstone, Hong Kong, pp 175–177
- 12.Narakas AO, Hentz VR (1988) Neurotization in brachial plexus injuries: Indications and results. Clin Orthop Relat Res 237:43–56 [PubMed]
- 13.Bertelli JA, Ghizoni MF (2004) Reconstruction of C5 and C6 brachial plexus avulsion injury by multiple nerve transfers: Spinal accessory to suprascapular, ulnar fascicles to biceps branch, and triceps long or lateral head branch to axillary nerve. J Hand Surg [Am] 29(1):131–139 [DOI] [PubMed]
- 14.Witoonchart K, Leechavengvongs S, Uerpairojkit C, et al. (2003) Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part I: An anatomic feasibility study. J Hand Surg 28A:628–632 [DOI] [PubMed]
- 15.Hallock GG (1993) The triceps muscle flap for axillary contracture release. Ann Plast Surg 30:359–362 [DOI] [PubMed]
- 16.Lim AYT, Pereira BP, Kumar, VP (2001) The long head of the triceps brachhii as a free functioning muscle transfer. Plast Reconstr Surg 107:1746–1752 [DOI] [PubMed]
- 17.OberlinC, Beal D, Leechavengvongs S, et al. (1994) Nerve transfer to biceps muscle using a part of ulnar nerve for C5-C6 avulsion of the brachial plexus: Anatomical study and report of four cases. J Hand Surg 19A(2):232–237 [DOI] [PubMed]
- 18.Nagano A, Tsuyama N, Ochiai N, et al. (1989) Direct nerve crossing with the intercostals nerve to treat avulsion injuries of the brachial plexus. J Hand Surg 14A(6):980–985 [DOI] [PubMed]
- 19.Mackinnon SE, Novak CB, Myckatyn TM, et al. (2005) Results of reinnervation of the biceps and brachialis muscles with a double fascicular transfer for elbow flexion. J Hand Surg [Am] 30(5):978–985 [DOI] [PubMed]
- 20.Brandt KE, Mackinnon SE (1993) A technique for maximizing biceps recovery in brachial plexus reconstruction. J Hand Surg 18A:726–733 [DOI] [PubMed]
- 21.Mackinnon SE, Dellon AL (1991) Surgery of the peripheral nerve. Thieme Medical Publishers, New York, pp 423–454
- 22.Chuang DCC, Yeh MC, Wei FC (1992) Intercostal nerve transfer of the musculocutaneous nerve in avulsed brachial plexus injuries—evaluation of 66 patients. J Hand Surg 17A:822–828 [DOI] [PubMed]
- 23.Chuang DC (2005) Nerve transfers in adult brachial plexus injuries: My methods. Hand Clin 21:71–82 [DOI] [PubMed]
- 24.Leechavengvongs S, Witoonchart K, Uerpairojkit C, et al. (1998) Nerve transfer to biceps muscle using a part of the ulnar nerve in brachial plexus injury (upper arm type): A report of 32 cases. J Hand Surg 23A(4):711–716 [DOI] [PubMed]
- 25.Teboul F, Kakkar R, Ameur N, et al. (2004) Transfer of fascicles from the ulnar nerve to the nerve to the biceps in the treatment of upper brachial plexus palsy. J Bone Jt Surg 86-A(7):1485–1490 [DOI] [PubMed]
- 26.Sungpet A, Suphachatwong C, Kawinwonggowit V, et al. (2000) Transfer of a single fascicle from the ulnar nerve to the biceps muscle after avulsions of upper roots of the brachial plexus. J Hand Surg 25B(4):325–328 [DOI] [PubMed]
- 27.Leechavengvongs S, Witoonchart K, Uerpairojkit C, et al. (2003) Nerve transfer to deltoid muscle using the nerve to the long head of the triceps, part II: A report of 7 cases. J Hand Surg 28A:633–638 [DOI] [PubMed]
- 28.Doi K, Sakai K, Kuwata N, et al. (1995) Double-muscle technique for reconstruction of prehension after complete avulsion of brachial plexus. J Hand Surg [Am] 20:408 [DOI] [PubMed]
- 29.Barrie KA, Steinmann SP, Shin AY, et al. (2004) Gracilis free muscle transfer for restoration of function after complete brachial plexus avulsion. Neurosurg Focus 16(5):E8 [DOI] [PubMed]