Abstract
External fixation has evolved from being used primarily as a last resort fixation method to becoming a main stream technique used to treat a myriad of bone and soft tissue pathologies. Techniques in limb reconstruction continue to advance largely as a result of the use of these external devices. A thorough understanding of the biomechanical principles of external fixation is useful for all orthopedic surgeons as most will have to occasionally mount a fixator throughout their career. In this review, various types of external fixators and their common clinical applications are described with a focus on unilateral and circular frames. The biomechanical principles that govern bony and fixator stability are reviewed as well as the recommended techniques for applying external fixators to maximize stability. Additionally, we have illustrated methods for managing patients while they are in the external frames to facilitate function and shorten treatment duration.
Key words: Ilizarov reconstruction, external fixation, biomechanics, trauma, deformity, limb lengthening
Introduction
External fixation entails the use of percutaneously placed transosseus pins and/or wires secured to external scaffolding to provide support to a limb. In this way, a bone or joint can be stabilized in the setting of trauma or limb reconstruction. The technique of external fixation was popularized in the mid-20th century when Hoffman introduced a device that used Steinman pins and bars to stabilize long bone fractures. Charnley concomitantly impressed the orthopedic community when he introduced an external fixator for knee arthrodesis. With a simple compression frame, he was able to dramatically increase knee fusion rates and decrease consolidation time. Behrens [1] described three basic concepts that govern the safe and effective application of external frames for bony trauma: The pins and wires should avoid damage to vital structures, allow access to the area of injury, and should meet the mechanical demands of the patient and the injury. While the Western world was using external fixators sparingly, external fixation was becoming a mainstay of orthopedic treatment in Russia and later in Northern Italy. In Kurgan, Siberia, Professor Ilizarov found external frames to be invaluable for a myriad of applications including posttraumatic and congenital limb reconstruction, limb salvage, complex arthrodesis, management of osteomyelitis and bone defects, and deformity correction. Using a circular fixation design with simple and versatile components, he was able to develop a method for osteogenesis that relied on a percutaneous approach with minimal trauma to the limb, closed anatomic fracture reduction, and excellent bony stability that allowed early weight bearing. In today’s fast growing field of limb lengthening and limb reconstruction, external fixators are powerful tools that enable surgeons to carry out the Ilizarov method and provide solutions to many difficult musculoskeletal problems.
The benefits of external fixation are numerous. When compared with internal plates and intramedullary nails, external fixators cause less disruption of the soft tissues, osseus blood supply, and periosteum [2]. This property makes fixators ideal for soft tissue management in the setting of acute trauma with skin contusions and open wounds, in chronic trauma where the extremity is covered in thin skin grafts and muscle flaps, and in patients with poor skin whose healing potential is compromised as in the case of rheumatoid disease, peripheral vascular disease, diabetes mellitus, and Charcot disease (Fig. 1). The temporary nature of the pins and wires makes frames ideal for providing bony stability in the setting of osteomyelitis where the presence of internal implants make eradication of infection more challenging (Fig. 2). The ability to avoid putting fixation into the infected area is equally beneficial. External fixators have been particularly helpful in obtaining solid fusions of large joints with recurrent osteomyelitis [3] (Fig. 3a–c). External fixators are fixed angle devices and as such provide superior fixation in compromised bone (Fig. 4a and b). The ability to use these fixed angle pins in multiple planes offers the versatility needed to optimize stability while minimizing tissue damage. This ability to choose ideal points on the extremity to place wires and half-pins has been particularly helpful in the setting of severe trauma where “good skin” is scarce. Unlike internal plates and intramedullary nails, external fixators provide postoperative adjustability. This allows the extremity to be manipulated in the operating room to gain exposures to fracture fragments for a wash out. In the situation of limb lengthening or deformity correction, gradual manipulation is possible with frame adjustment (Fig. 5a–c). External fixators have been used in pediatric fracture care where open physes preclude intramedullary nailing. Leg length discrepancy can be reliably treated with circular and monolateral design fixators. Many fixators provide excellent stability making early weight bearing and joint motion exercises well tolerated. The purpose of this article is to review the mechanical principles of external fixation that have been identified through biomechanical research and clinical experience. These principles provide a foundation for the proper use of all external frames whose importance in this field continues to grow.
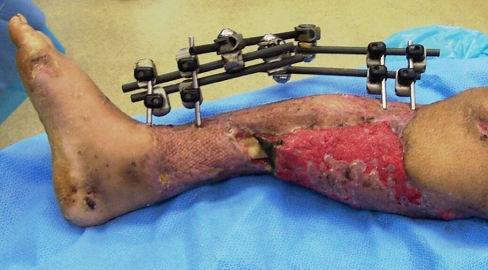
Fig. 1.
In this case of significant lower extremity trauma, the Ilizarov frame provided stability to the fracture, protected the skin grafts, and allowed access to the involved soft tissues. These percutaneous K-wires cause minimal disruption of the blood supply and soft tissues through the zone of injury
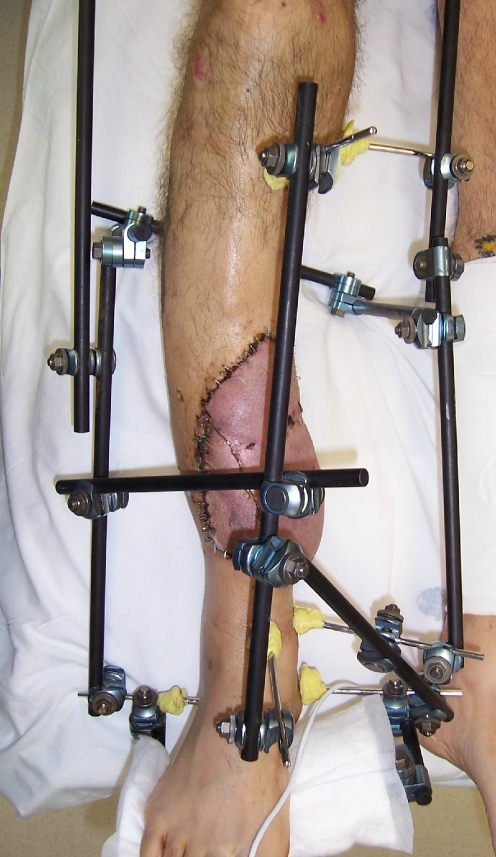
Fig. 2.
Trauma type pin-to-bar fixator used to help eradicate infection in a septic tibial nonunion
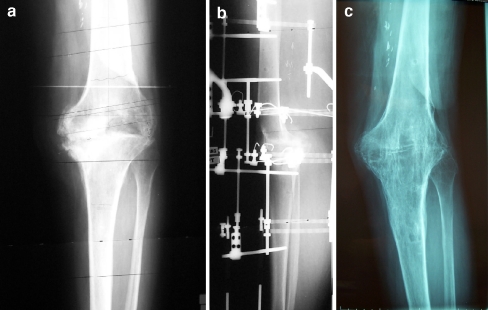
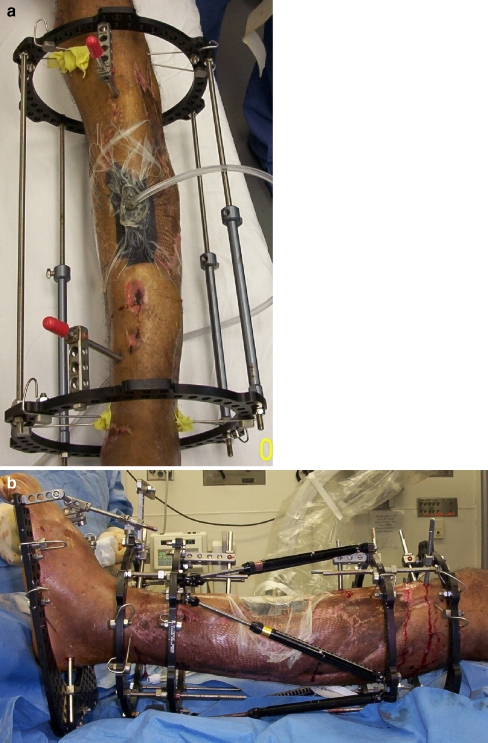
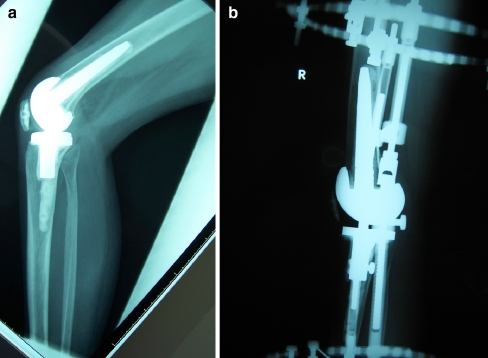
Fig. 3.
(a) This patient failed revision knee replacement surgery for recurrent infection. (b) The Ilizarov fixator was applied for knee fusion.(c) Healed knee fusion
Fig. 4.
(a) This 82 year old woman with diabetes mellitus and advanced peripheral vascular disease had an aseptic tibial nonunion. (b) She was treated with circular fixation and gradual correction of the deformity without open repair of the nonunion. (c) Healed nonunion. The patient was in the frame for 4 months
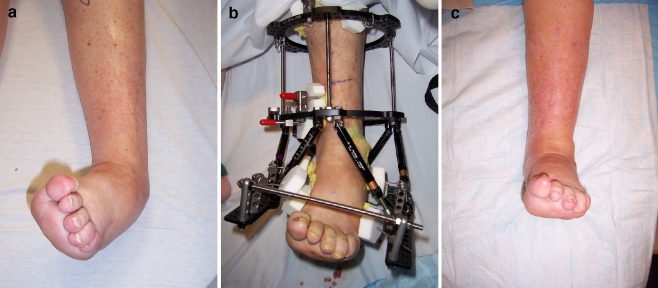
Fig. 5.
(a) This severe varus deformity was corrected through an ankle fusion. (b) A gradual correction approach was taken. (c) Final result after frame removal
The mechanics of unilateral frames
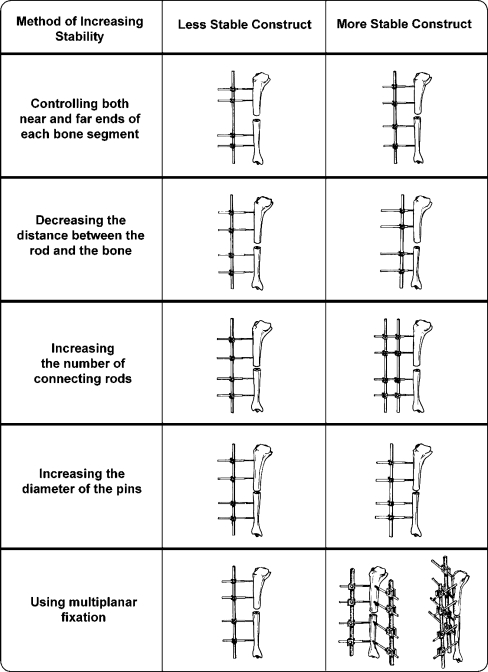
Unilateral frames are distinguished from circular frames in that they are positioned on one side of the limb. Unilateral frames allow the limb to remain functional, avoid complications, and provide bony stability [4]. When we consider unilateral frames, the two most common designs are the bulkier monobody designs (EBI, Parsippany, NJ, USA, and Orthofix, Verona, Italy) and the trauma type pin-to-bar fixators. (A word on hybrid external fixators: Hybrid fixators are unilateral fixators with a ring attached and behave like monobody designs. Hybrid fixation also refers to the substitution of half pins for some wires when using an Ilizarov ringed fixator, a technique developed in Italy. In this report, all references to hybrid fixation refer to the Italian definition.) The stability of all unilateral frames is improved by the use of larger-diameter half pins with more points of fixation, decreasing the distance between the frame and the bone, and placing pins out-of-plane to one another (Fig. 6). The monobody frames have considerable intrinsic stability owing to their heavy and rigid design (Fig. 7). Most pin-to-bar designs use multiple lightweight carbon fiber rods to provide stability. Improved rigidity of these fixators is obtained by adding a second connecting rod to the same pins and by adding a second half-frame in a different plane to the first (Fig. 8). These fixators are versatile enough to allow pins to be placed both near to the fracture and far from the fracture providing excellent control of the bone segment. Behrens et al [5] found that anteriorly placed frames best neutralized the anteroposterior and transverse bending moments in a tibia fracture model. He concluded that an anteriorly placed tibial fixator could control the most significant clinical forces that the leg would experience. Similarly, Gasser et al [6] noted that the bending stiffness of unilateral fixators was dependent on the plane of the half pins and the plane of loading with anteriorly mounted frames providing greater bending stiffness to anteroposterior directed bending forces. In contrast, when these frames were loaded out of plane, with varus–valgus and torsional forces, they had poor control of the bone fragments with significant motion at the fracture site. These results suggest that if one must mount a unilateral tibial fixator in one plane, then it should lie along the anterior tibia, but more stability would be obtained from a multiplanar system. When subjected to axial loading, the unilateral frames demonstrate cantilever bending with asymmetric loading at the fracture site.
Fig. 6.
Unilateral external fixator stability diagram
Fig. 7.
The EBI MAC frame is quite rigid and allows for the correction of multiplanar deformities
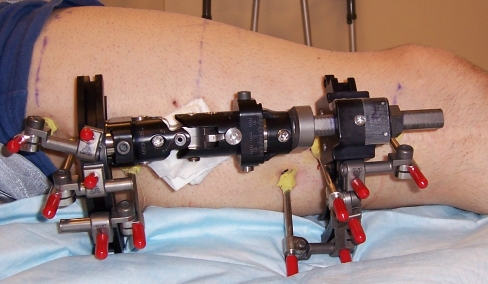
Fig. 8.
This unilateral fixator has gained stability by connecting a second bar to each pair of half pins
The mechanics of circular frames
The classic circular frame is the Ilizarov external fixator that has now been integrated with the newer Taylor Spatial Frame (TSF; Smith and Nephew, Memphis, TN, USA) (Fig. 9). The basic components of this frame are rings, connecting rods, and struts (Fig. 10). Varieties of Ilizarov rings include full (closed) rings, partial (open) rings, or arches. Full rings provide the most stability, and arches the least. However, partial rings and arches are helpful near joints and in areas where a closed ring would prevent normal extremity function or positioning. A partial ring is commonly used around the proximal knee to allow for improved knee flexion (Fig. 11). Open rings and arches are also used around the shoulder and proximal femur where a full ring would not fit comfortably (Fig. 12).
Fig. 9.
This ankle fusion frame combines the classic Ilizarov assembly with the modern aluminum Taylor Spatial rings. This makes the frame more modular as at any time the connecting rods could be exchanged for spatial struts. If a proximal lengthening is planned then existing rings are ready to accept struts as well
Fig. 10.
Taylor spatial rings connected with 10 mm threaded connecting rods
Fig. 11.
The 2/3 ring is used around the knee joint to allow improved joint flexion. Rehabilitation begins during treatment
Fig. 12.
This proximal femoral osteotomy was stabilized with a two Ilizarov arches
Frame stability is greatly impacted by ring properties. Smaller diameter rings are more stable than larger rings of the same thickness [7–9]. In fact, decreasing the ring diameter by 2 cm was found to increase axial frame stiffness by 70% [6]. Mechanically, the smallest diameter ring that will fit the extremity should be used. However, a ring that fits too closely may cause compression and skin ulceration of the extremity that becomes edematous (Fig. 13). A guideline is that one should allow for a minimum of 2 cm of space between the skin and the ring circumferentially. Different diameter rings may be used in the same frame to conform to the limb contours and optimize stability. This is often seen with knee fusion frames where smaller rings are used around the leg and larger rings are needed to accommodate the thigh. Ring widths and heights also vary with the wider and thicker rings being less likely to deflect or bend during loading. The position that the bone occupies in the ring does not appear to affect stability. Although Ilizarov championed centralizing the bone in the ring to enhance stability, others have found that eccentric positioning of the bone in the ring, as occurs around the proximal tibia, had no adverse effect on ring stability and in fact may increase stiffness of the construct [7, 10, 11]. The distance between the rings and the type of ring connectors used will affect stability. Rings that are far apart connected with long rods will experience more motion between them. The use of a “dummy” ring (an empty ring with no fixation to the bone) secured in the mid portion of the long rods will effectively shorten the rods and increase the stability of the frame (Fig. 14). Alternatively, telescopic rods with their greater diameter and superior bending strength can be used to span long distances and preserve frame stability.
Fig. 13.
Despite the use of large rings this patient’s leg swelled to the point of impinging on the middle ring. The skin was observed closely but no intervention was necessary
Fig. 14.

This lengthening frame incorporates a middle ring that has no bony attachment. This “dummy ring” serves to improve fixator stability over long distances
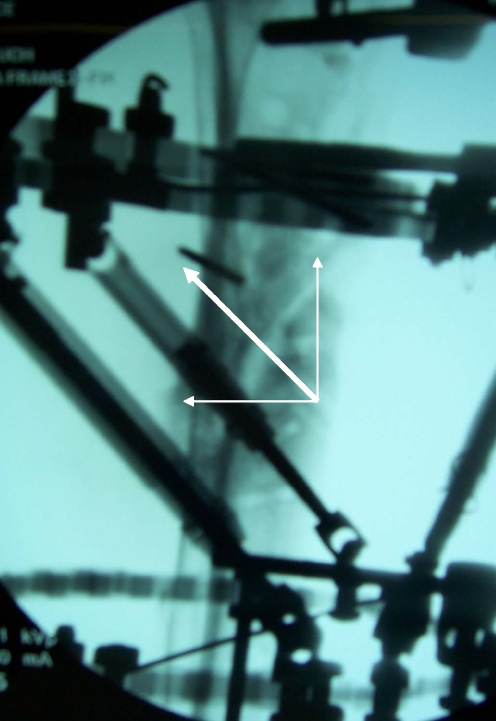
The concept of a ring block is important with respect to frame stability. Simply defined, a ring block is the portion of the frame that is attached to a bone segment. Bones are divided into segments by fractures, defects, or osteotomies. The stability of a ring block will increase with the use of an increasing number of rings, shorter distances between rings, increasing the span of the rings across the bone controlling both near and far ends of each segment, increasing the number of connections between the rings, and increasing number of points of fixation to the bone. Most authors recommend that each bone segment be stabilized by a ring block consisting of two rings with two points of fixation per ring and four connecting rods. The connecting rods in a given ring block should be orthogonal to the mechanical axis of that bone segment (Fig. 15). With the advent of thicker and wider rings and the ability to connect pins away from the ring, ring blocks are more commonly seen to consist of a single ring with 3–4 points of fixation maximally spread across the bone segment. Sarpel et al [12] looked at the stability of single-ring ring blocks as compared with more standard double-ring constructs. He found that two wires and two Shantz screws connected to a single ring provided stability superior to any other single ring construct, but was still inferior to a double-ring ring block at providing bony stability in nearly all modes of loading. Antoci et al [13] showed that the use of a single ring with five wires provided comparable bending stiffness to that of a two-ring construct with four points of fixation. Interestingly, torsional stiffness was higher in the five wire single-level specimens than in any of the double-level models. Following these recommendations will help achieve a stable, well-aligned frame.
Fig. 15.
This severely deformed leg requires the use of two stable ring blocks for correction. In this example each ring block consists of 2 rings with 4 points of fixation. Each ring block is aligned with the axis of its respective bone segment. This crooked frame will be straight when the correction is completed
Comparison of Ilizarov and unilateral fixators
Mechanical aspects
Many studies have been performed that compare the stability of circular and unilateral frames in various modes of loading. As frame stability directly affects osteogenesis, these studies have great clinical relevance. The optimal design for an external fixator is one that is rigid in torsion, bending, and shear but allows for axial movement [14, 15]. Paley et al [16] found the EBI and Orthofix (McKinney, TX, USA) monobody frames to be more rigid than the Ilizarov tibial frame, preventing axial motion at the osteotomy site. This raised concerns from the authors that these unilateral frames may be too stiff, causing stress shielding and delays in healing. With weight bearing monolateral frames experience cantilever bending delivering asymmetric compression to the fracture site. In contrast, the more even loading of the bone ends provided by the Ilizarov frame leads to uniform compression. This was thought to enhance healing and prevent malunion. In studying circular fixators, both Gasser et al [6] and Podolsky and Chao [10] noticed the nonlinearity of the load deformation curve exhibited by the Ilizarov frame in response axial loading that was not seen in the monolateral fixators. The Ilizarov frame demonstrated a load dependence of axial stiffness; when subjected to low loads, the frame had low axial stiffness; at higher loads the stiffness of the wires and frame increased significantly. This nonlinear behavior is reminiscent of the viscoelastic properties of biological materials, such as tendons and ligaments, and may be responsible for the promotion of fracture healing. The low frame rigidity seen at lesser loads allows more axial motion and is presumed to be useful for stimulation of fracture callus formation. The higher frame rigidity seen at increased loads is thought to protect the healing fracture tissues from excessive motion preventing pain and fibrous nonunion. This property may explain how the Ilizarov frame has been able to promote osteogenesis where other frames have failed. One must keep in mind that these studies were performed with the all-wire Ilizarov frame, which is not commonly used in the West, where hybrid fixation constructs are predominant. Some researchers have found that hybrid and all-wire frames exhibit similar properties [11, 17]. Others have reported increased stiffness of the hybrid frames in bending and torsional loading [18].
In our practice, both circular and monobody fixators have provided excellent stability and helped us accomplish fracture union and bone lengthenings very successfully (Fig. 16).
Fig. 16.
Femoral lengthening performed with a unilateral fixator
Clinical aspects
Provisional fracture stabilization
Although all external fixation devices are temporary, certain varieties are designed to be used for short periods of time until a more permanent solution is appropriate. These pin-to-bar constructs have been immensely popular in the United States and Europe (Fig. 17). Their primary role is in providing fast, minimally traumatic stability to a fractured limb. This technique can be limb saving in the setting of high-energy trauma with soft tissue damage in the medically unstable patient and in any circumstance where definitive fracture treatment must be delayed. These frames play a central role in the modern environment of damage control orthopedics. The surgeon can place half pins independently in safe corridors without having to spend time aligning the pins with one another. The connecting bars are then assembled to the pins and one another until all points of fixation are incorporated (Fig. 18). Although circular fixators are commonly perceived as labor-intensive and to be used for definitive treatment only, they can be used in a stripped down version to provide temporary stability with the intention of delayed frame revision (Fig. 19a and b).
Fig. 17.
This open pilon fracture was stabilized with an ankle spanning simple construct
Fig. 18.
This construct emphasizes the freedom that these frames allow for pin placement and incorporation into the frame
Fig. 19.
(a) This temporary two ring frame provides provisional stability and allows access for soft tissue management. (b) Definitive bony treatment follows, in this instance with a more stable bone transport set up
Monobody fixators
The rigid monobody fixators have been very useful for lengthenings and deformity correction procedures of the humerus and femur in particular. These fixators offer a several advantages over circular fixation in these locations. The humerus and femur are surrounded by a bulky soft tissue envelope requiring wires to pass through muscle compartments making them less safe to insert and more uncomfortable. The arm is close to the torso making the use of full rings impractical. The use of arches on the humerus provides improved patient comfort but is mechanically similar to unilateral designs. The thigh does not tolerate full rings well as the opposite thigh impinges. Furthermore, thigh rings are very uncomfortable as the patient cannot sit or lie down easily. Unilateral fixators provide stability and much improved patient comfort. Newer models allow for the simultaneous correction of deformity in multiple planes. (Fig. 7) When compared with ringed fixators, the monobody designs are less awkward. Their reduced bulk facilitates hygiene maintenance and accommodates the use of greater clothing options.
Circular fixators
Until recently circular fixation had not been embraced in the United States, where most surgeons prefer the more familiar unilateral fixators. This is unfortunate because the Ilizarov fixator is quite versatile. It is a completely modular system that can be assembled on the patient in the operating room to provide optimal stability while respecting safe corridors and skin condition. The rings raise the extremity off of the bed both protecting the skin and providing elevation. The rings also provide circumferential access to the limb for placement of wires and half pins making multiplanar fixation simple. The circular nature prevents cantilever bending. Partial rings can be used to accommodate joint motion or wound access for the plastic surgeons. Additional rings can be attached distally or proximally by using smooth wires to provide temporary improved stability with plans for early removal in the office when healing is underway. Gradual corrections of deformity and shortening can be simultaneously addressed [19]. For large bone defects, multilevel osteotomies can be made to reduce bone transport time. When a bone defect is accompanied by overlying soft tissue loss, simultaneous transport of bone and soft tissue has been successfully performed using the Ilizarov method [20]. For large lengthenings, lengthening over a nail or lengthening and then nailing techniques reduce time in the frame dramatically. Major joints can be spanned with hinges to maintain stability and preserve motion. Hinges can also be used to gradually correct joint contractures.
Mechanics of wires and half pins
Wires
The mechanics of transfixion wires, including proper insertion and tensioning techniques, have been elucidated. Wire stability increases with increasing wire diameter and increasing tension placed across the wire. Wire frame stability is enhanced by using more wires per ring, placing wires on opposite sides of the ring, securing wires directly to the ring, and inserting wires in different planes including crossing from the top to the bottom of the ring [10, 17, 21, 22]. Ilizarov [7] taught that increasing the crossing angles of wires approaching 90° provided maximal stability. It was assumed that this was true in all modes of loading. Further testing has demonstrated that a 90° wire crossing angle provides maximal stiffness to axial loading, but a 30° crossing angle for medial-to-lateral wires provides superior resistance to medial bending forces [10, 23].
Two wires that cross at an angle of less than 60° allow for unwanted sliding of the bone segment along the wires. Olive wires can be used to buttress the bone provided that they are inserted from opposite directions. The opposing olive beads will prevent bone sliding despite narrow crossing angles. The addition of half pins has greatly reduced the importance of wire crossing angles and the need for olive wires (Fig. 20).
Fig. 20.
A typical proximal tibial ring block consists of one ring with 4 points of fixation. Although the two wires have a narrow crossing angle (25 degrees), the 2 half pins prevent any sliding of the ring in the coronal plane. These two wires provide excellent resistance to medial–lateral bending forces
A thorough knowledge of the cross-sectional anatomy of the extremity is necessary to avoid neurovascular injury. If under general anesthesia, the patient should not receive paralytic agents as these will mask the important signs of flickering of the distal extremities when a motor nerve is inadvertently irritated by a wire. Spinal or epidural anesthesia will not mask the irritation of a motor nerve. Proper wire insertion demands the use of a low heat technique. It is important to minimize the heat generated during drilling of the wire through the bone in order to prevent bony and soft tissue necrosis, which will typically cause infection and loosening of the wire. To prevent thermal necrosis, the tourniquet should never be inflated prior to drilling as normal blood circulation will help cool passing wires. Saline-soaked sponges can be used to cool and direct the wire during drilling. If the bone is particularly hard, as is the case in diaphyseal wires, then frequent pauses will prevent heat buildup. The all-cortical wires should be avoided as this will generate heat rapidly. When the tip of the wire is through the soft tissue on the opposite side of the extremity, the wire should be pushed the rest of the way using a mallet to avoid winding up of soft tissue.
When inserting a wire near a joint, the joint should be placed in the end range of motion. For example, when placing a wire across the distal tibiofibular joint, and the wire is inserted from posterolateral to anteromedial, the foot should me maximally dorsiflexed prior to piercing the posterolateral skin with this wire and held in that position while drilling through the fibula and tibia to preserve ankle dorsiflexion. The foot should then be positioned in plantarflexion before the wire exits the anteromedial side, insuring uninhibited plantarflexion. Following these recommendations will improve patient comfort and ankle mobility. The same concept is used if passing through fascial compartments, although transcompartmental wires should be avoided as they are uncomfortable and may become infected from movement of the soft tissue at the wire site when activating the muscles [7].
Wire tensioning greatly enhances the rigidity of the wire and the stability of the frame [10]. Wires are typically tensioned to 130 kg or until the ring begins to deflect whichever comes first. If an open ring or an arch is used, then less tension is utilized (70–100 kg). When older tensioners that do not have a load gauge in them are used, it is theoretically possible to cause plastic deformation of the wire. Tension beyond 155 kg will cause this stretching deformation of the K-wire [24].
Half pins (Shantz screws)
The mechanics of these pins follow the same trends as those of transfixion wires. As the core diameter of the pins increases, so does the rigidity. A 90° crossing angle of half pins is desirable for improved control in multiple planes. Knowledge of the anatomic safe zones and respect for the soft tissues apply. The principle of low heat generation during half pins’ insertion is again of paramount importance. All half pins should be bicortical and predrilled using a sharp drill bit with a tissue protection sleeve. In hard bone, frequent pauses are prudent, and the drill flutes may need to be wiped clean before passing through the far cortex to avoid thermal damage. Cannulated drills should be avoided in the diaphysis as they will cause thermal damage to the bone. Pins are inserted by hand.
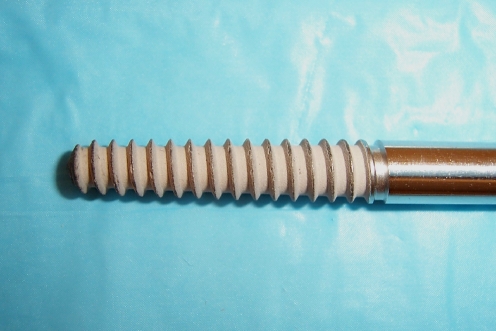
Recently, hydroxyapatite (HA) coated pins have become popular, especially in limb lengthening and deformity surgery where frames stay on for several months. HA coated pins have been shown to have significantly increased extraction torque, lower rates of loosening, decreased infection rates, and even a lower incidence of secondary deformity during lengthening [25–28]. Although both tapered and bicylindrical designs exhibit excellent pin extraction torque and microscopic evidence of direct bone–pin contact [29], we prefer 6-mm tapered, HA-coated pins (Fig. 21). Pins are available in 3.5-, 4.5-, and 6-mm-diameter sizes. When selecting a pin, keep in mind that the diameter of the half pin should be less than one-third of the bone diameter to minimize the risk of fracture at the pins’ site. Unicortical half pins also increase the risk of fracture.
Fig. 21.
Typical hydroxyapatite (HA) coated, 5–to–6 mm tapered half pin. This would be used in the adult tibia, femur and humerus
Wires versus half pins
Whether to use a wire or a half pin has become a subject of debate between classic and modern Ilizarov surgeons. Decisions will be made based on surgeon preference, anatomic constraints, and mechanical principles. While all wire or all half pin frames can be correct if applied with sound mechanical principles, we prefer hybrid frames in which wires and half pins are used optimally. Transverse wires are useful in the metaphysis where they avoid muscle compartments and help establish proper ring orientation (reference wire). The reference wire helps with the application of a reference ring to a given bony segment. Wires are useful for tibia and fibula fixation in both the proximal and distal leg—a necessary part of any lengthening procedure. Stable fixation of small bone segments is made possible by using multiple wires. This is especially true in pediatric fractures with narrow metaphyseal segments between the fracture and the growth plate. This is also the case when fixing a short, periarticular bone segment. Multiple wires provide improved fixation in osteoporotic bone. Wires allow for axial motion at the fracture/osteotomy site producing a “trampoline effect” with weight bearing, which is thought to encourage osteogenesis. Because wires can be easily removed in the clinic, they can be used when only temporary fixation is needed. (For example, foot wires and a foot ring are used to temporarily span the ankle joint. The wires and ring can then be removed in the office with minimal discomfort.)
The use of half pins in lieu of some wires gained popularity in the West. Most external fixators used in the United States rely on half pins to provide bony fixation. Advantages of half pin fixation include familiarity in application, patient comfort, rigid fixation, and a low infection rate. Half pins are particularly useful in the diaphysis where large crossing angles can be achieved without invading the muscle compartments of the leg. In the metaphysis of the tibia, half pins can be inserted in a greater anterior to posterior orientation than could be achieved with wires. Half pins are very useful in the femur and humerus for anatomic reasons.
When deciding whether to use half pins or wires for fixation, the clinical scenario may call for one over the other. We have concerns about the use of half pins in patients with neuropathy as the pins have tendency to become loose and infected, or fatigued and break at the level of the cortex. On radiographs, we have observed large areas of bone resorption around the half pins, which are likely the result of uncontrolled weight bearing in patients who lack the protection of pain feedback. (Minimal weight bearing is recommended to these patients). In children we tend to use more wires close to the growth plate. In children with congenital pseudarthrosis of the tibia, we avoid half-pins because of their poor potential for remodeling larger holes from half-pins.
Frame stability and weight bearing
A key component for successful bone healing is early weight bearing and functional activity. Weight bearing provides axial loading to the fracture, nonunion, or osteotomy site that stimulates osteogenesis. Sarmiento et al’s [30] classic experiment in rat femur fractures treated with either early weight bearing or nonweight bearing showed that functional weight bearing accelerated fracture healing and significantly improved the strength of the fracture callus. Klein et al [31] found that early weight bearing in combination with an appropriate amount of motion at the fracture site results in accelerated healing rate with increased stiffness of fracture callus. Kenwright et al [15] found that in tibia fractures treated with a dynamic unilateral fixator, both clinical and mechanical healing were enhanced by the addition of axial micromotion at the fracture site. He added that although rigidly locked frames did allow for earlier full weight bearing, they also prevented axial interfragmentary motion and resulted in delayed healing. Ilizarov [7] reported that a lack of axial loading in the presence of normal blood supply and adequate bony stability will cause resorption at the bone gap site. He added that weight bearing alone without a sufficient blood supply will inhibit osteogenesis, and weight bearing with poor fixation will lead to resorption of the bone ends. Only the combination of a sufficient blood supply, bony stability, and axial loading will provide the necessary environment for osteogenesis.
The stability of the bone fragments and the rigidity and design of the fixator will determine how much weight bearing is possible. A stable frame will control the bone ends and make ambulation comfortable, which is the first step in getting the patient to walk. The geometry of the fracture or osteotomy gap will affect stability. Good bony contact at the gap site dramatically augments frame stability and the ability to bear weight [7, 10]. Likewise, in a lengthening model, the volume of regenerate will affect frame stability. A shorter and wider regenerate, such as occurs in a metaphyseal osteoplasty location, provides greater stability then a long diaphyseal regenerate. As the regenerate ossifies and unloads the pins, the patient will walk more comfortably.
In general, frames should initially be very stable. This will help with early fracture healing or deformity correction and allow early weight bearing. As healing progresses, the bone bears greater load and less stability is needed for comfort or bony healing. Frames can be gradually dynamized or minimized in the office by removing wires and rings.
A loss of bony contact will adversely affect frame stability. If a patient with a bone defect has a stable frame that allows ambulation, full weightbearing is not recommended as the bone is stress-shielded. The lack of bone contact transfers the full axial load through the pins and wires, causing increased relative motion at the skin interface. Motion often leads to pin loosening and infection. Frame instability significantly affects the ability to weight bear. Many of the unilateral trauma fixators were designed to provide portable traction to the injured limb and are not suitable for full ambulation (Fig. 22).
Fig. 22.
This knee spanning design provides suboptimal stability for ambulation as a minimal number of pins were used, the pins are clustered close together, and there is poor control over sagittal motion
Compression and distraction forces
The effect of compression or distraction of the frame across a fracture or osteotomy site is an increase in frame stability. The mechanics of this increase in frame stability is attributable to the effect of compression and distraction on the wires and soft tissues. Compression of the bone ends causes an increase in wire tension and wire rigidity that improves the stiffness of the entire frame. Good bony contact under compression also increases the intrinsic bony stability [10]. Distraction of the bone ends generates significant resistance in the surrounding soft tissue envelope that imparts great tension onto the frame, dramatically increasing stability despite the presence of a bone gap [7].
Articulated external fixation
Many fixators have been designed to cross major joints in an effort to both stabilize the joint while affording some joint motion or to correct large joint contractures. The Ilizarov external fixator, in particular, has found great utility in this regard. Its modular nature allows for the recreation of both a simple joint hinge, as occurs about the elbow, and an oblique axis hinge, as occurs about the ankle. Knee flexion and extension contractures as well as ankle equines contractures have been successfully corrected with a gradual technique using a simple hinge construct [32, 33] (Fig. 23a and b). Central to the success of this method is proper identification and re-creation of the true flexion and extension axis of the joint with the hinges. Inaccurate positioning of the hinge may lead to inadvertent joint compression, distraction, or subluxation. Risk of recurrence remains a problem [34].
Fig. 23.
(a) Persistent knee flexion contracture after total knee replacement surgery was treated with Ilizarov method using hinges. (b) Full knee extension was accomplished safely using this method
Fracture reduction techniques
The traditional approach to fracture management with external fixation involves placing longitudinal traction across the limb to obtain a closed reduction and mounting the fixator while maintaining the reduction. An alternative technique is to mount the frame and then use it to reduce the fracture fragments. In the latter case, fixation is applied to the principal bone segments where they lie using the safe corridors. Separate rings or connecting bars are connected to the wires and half pins of each segment independently. The bone segments are manipulated to reduce the fracture, and the rings and bars are connected to maintain the reduction. The introduction of the Ilizarov/TSF has further advanced this technique for fracture reduction. After applying free rings to each segment, struts are used to connect the rings. The fracture is closed reduced and the struts are locked to hold this position. If the reduction is not anatomic, then the TSF web-based program can be used to acutely or gradually fine-tune the movement of the rings yielding an anatomic reduction. This versatile frame is also capable of providing oblique compression vectors. This prevents sliding of oblique fractures that would occur under traditional axial compression (Fig. 24).
Fig. 24.
The Taylor Spatial Frame has the unique ability to apply compression to a fracture in an oblique plane. By telling the computer to “shorten” (axially compress) and “posteriorly translate” the distal fragment, a net vector of compression is created in an oblique plane perpendicular to the fracture plane
Removal of external fixator
Dynamization
The first step of frame removal is preparing the bone for upcoming loss of external support. An important part of the bone healing process is the gradual addition of increasing load across the site of osteogenesis as the callus gains stability. This process of dynamization prevents stress shielding by the external fixator and results in greater callus formation. Dynamization is accomplished by destabilizing the frame. Unilateral fixators can be made more unstable by removing bars, sliding the bars further away from the bone, removing half pins, and releasing tension or compression from the system. Circular frames can be dynamized by removing wires, releasing tension from the wires, removing connecting rods between rings, removing whole rings from a ring block, releasing all tension or compression from the system. The main drawback of dynamization is early loss of frame stability leading to delayed union, refracture, or development of secondary deformity.
Timing of removal
Making the decision of when a fixator is ready to be removed is as much an art as a science. General convention is when three of four cortices demonstrate radiographic healing, the bone has enough intrinsic stability to remove the fixator. A more objective method to measure the bone’s ability to tolerate full, unsupported weight has been suggested. While patients were still in the frame, the load passing through the fixator was compared to the load through the extremity at multiple intervals in patients during the consolidation phase of Ilizarov distraction osteogenesis. A load/share ratio was created to calculate the percentage of the weight-bearing load that was being carried by the fixator. As healing progressed, the amount of load that the bone supported increased and the ratio decreased. The group found that when 10% of load passed through the fixator, the frame was ready to be removed [35]. This study shows that more accurate methods are being developed to determine ideal timing for frame removal to reduce time in the frame while avoiding complications of premature removal. Some surgeons are so concerned about these complications that they will remove the fixator and retain the pins for an additional week. If there are signs of bony instability upon the return visit, the frame will be reapplied.
Complications
Pin site infection is a common complication of external fixation. In our practice, most infections respond well to aggressive local pin care and empiric oral antibiotics. If the infection does not resolve quickly, then culture-specific antibiotics are used. More advanced infections are aggressively treated with removal of the pin or wire. Cellulitis is treated with intravenous antibiotics. Rarely, operative intervention is needed for pin infections to replace an important pin or debride osteomyelitic bone. Historically, malunion has been a commonly reported complication for fracture treatment with fixators, but this has not been the case in our practice. Septic arthritis may complicate any patient being treated with fixators. Avoidance of intracapsular wires is important. A high index of suspicion should be maintained when using fixation around periarticular fractures, where intraarticular communication with the fracture site is present.
While malunion is a known complication of fracture treatment by external fixation, modern fracture management approaches have minimized this problem. When external fixators are used as a means of obtaining temporary bony stability, obtaining anatomic alignment is not of primary importance. When delayed definitive fixation is performed, typically with an internal implant, the alignment is addressed and malunion is uncommon. Definitive treatment with an external fixator typically involves the use of the newer generation reconstruction frames including the Ilizarov/TSF or a solid, adjustable monobody design. These frames provide the stability needed to prevent fracture fragment shifting and malunion. More importantly, these fixators provide postoperative adjustability. An impending malunion can be realigned postoperatively by using the fixator to correct deformity. This does not typically require additional surgery. By correcting all deformity before the bone heals, a malunion is avoided.
Deep vein thrombosis is a complication that accompanies any lower extremity surgery. Treatment is geared toward prevention. The mobility afforded to patients by external fixation helps with early rehabilitation and prevention of venous stasis decreasing the incidence of this complication. Anticoagulation is often a part of the postoperative protocol.
Although the fixator protects the bone that it spans, it creates a stress riser in the adjacent bone that is not within the frame. This situation can lead to fractures around the frame. Often, this occurs through the most proximal or most distal screw hole. Once the frame has been removed, stress fractures may occur through any of the screw holes before they have had a chance to remodel.
Stiffness of adjacent joints occurs if the joint has been spanned for some time and during lengthening procedures. The ankle joint tolerates this immobility far better than the knee joint. When trauma fixators are used to stabilize tibia fractures, strong consideration should be given to initially including the foot (spanning the ankle joint) to prevent the development of an early equinus contracture. Once the patient is more mobile and pain-free, the foot ring is removed, allowing for ankle motion and easier weight bearing.
Future directions
The Ilizarov method has greatly contributed to the fields of trauma, limb lengthening, limb reconstruction, and deformity correction. Central to the success of this method is the Ilizarov circular frame both in its traditional and hybrid forms, whose mechanical properties have been demonstrated. Over the last decade the Taylor Spatial Frame has been introduced and embraced by the Trauma and Limb Lengthening communities. This frame has been used with great success for multiplanar deformity corrections, distraction osteogenesis, nonunion management, and fracture care. Although the TSF allows for increased motion while in its neutral mode (due to the universal joint struts-to-ring connections), when under tension or compression the frame clinically provides the stability needed for osteogenesis. Further biomechanical testing and clinical studies need to be carried out with the TSF looking at frame stability compared with the Ilizarov system.
References
- 1.Behrens F (1989) General theories and principles of external fixation. Clin Orthop 241:15–23 [PubMed]
- 2.Claes L, Heitemeyer U, Krischak G, et al. (1999) Fixation technique influences osteogenesis of comminuted fractures. Clin Orthop 365:221–229 [DOI] [PubMed]
- 3.Rozbruch SR, Ilizarov S, Blyakher A (2005) Knee arthrodesis with simultaneous lengthening using the Ilizarov method. J Orthop Trauma 19:171–179 [DOI] [PubMed]
- 4.Behrens F, Searls K (1986) External fixation of the tibia. Basic concepts and prospective evaluation. J Bone Joint Surg Br 62:246–254 [DOI] [PubMed]
- 5.Behrens F, Johnson WD, Koch TW, Kovacevic N (1983) Bending stiffness of unilateral and bilateral fixation frames. Clin Orthop 178:103–110 [PubMed]
- 6.Gasser B, Boman B, Wyder D, et al (1990) Stiffness characteristics of the circular Ilizarov device as opposed to conventional external fixators. J Biomech Eng 112:15–21 [DOI] [PubMed]
- 7.Ilizarov GA (1992) The Apparatus: components and biomechanical principles of application. In: Green S (Ed) Transosseus osteosynthesis. Theoretical and clinical aspects of the regeneration and growth of tissue. Springer-Verlag Berlin, pp 63–136
- 8.Duda GN, Kassi JP, Hoffman JE, et al (2000) Mechanical behavior of Ilizarov ring fixators. Effect of frame parameters on stiffness and consequences for clinical use. Unfallchirurgie 103:839–845 [DOI] [PubMed]
- 9.Cross AR, Lewis DD, Murphy ST, et al (2001) Effects of ring diameter and wire tension on the axial biomechanics of four-ring circular external fixator constructs. Am J Vet Res 62:1025–1030 [DOI] [PubMed]
- 10.Podolsky A, Chao EY (1993) Mechanical performance of Ilizarov circular external fixators in comparison with other external fixators. Clin Orthop 293:61–70 [PubMed]
- 11.Flemming B, Paley D, Kristiansen T, et al (1989) A biomechanical analysis of the Ilizarov external fixator. Clin Orthop 241:95–105 [PubMed]
- 12.Sarpel Y, Gulsen M, Togrul E, et al (2005) Comparison of mechanical performance among different frame configurations of the Ilizarov external fixator: experimental study. J Trauma 58:546–552 [DOI] [PubMed]
- 13.Antoci V, Roberts CS, Antoci V Jr, et al (2005) The effect of transfixion wire number and spacing between two levels of fixation on the stiffness of proximal tibial external fixation. J Orthop Trauma 19:180–186 [DOI] [PubMed]
- 14.Goodship AE, Watkins PE, Rigby HS, et al (1993) The role of rigid frame stiffness in the control of fracture healing. An experimental study. J Biomech 26:1027–1035 [DOI] [PubMed]
- 15.Kenwright J, Richardson JB, Cunningham JL, et al (1991) Axial movement and tibial fractures. A controlled randomized trial of treatment. J Bone Joint Surg Br 73:654–659 [DOI] [PubMed]
- 16.Paley D, Fleming B, Catagni M, et al (1990) Mechanical evaluation of external fixators used in limb lengthening. Clin Orthop 250:50–57 [PubMed]
- 17.Yang L, Nayagam S, Saleh M (2003) Stiffness characteristics and inter-fragmentary displacements with different hybrid external fixators. Clin Biomech 18:166–172 [DOI] [PubMed]
- 18.Calhoun JH, Li F, Bauford WL, et al (1992) Rigidity of half pins for the Ilizarov external fixator. Bull Hosp Jt Dis 52:21–26 [PubMed]
- 19.Rozbruch SR, Helfet DL, Blyakher A (2002) Distraction of hypertrophic nonunion of tibia with deformity using Ilizarov/Taylor spatial frame. Arch Orthop Trauma Surg 122:295–298 [DOI] [PubMed]
- 20.Rozbruch SR, Weitzman AM, Watson JT, et al (2006) Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 20(3):194–202 [DOI] [PubMed]
- 21.Orbay GL, Frankel VH, Kummer FJ (1992) The effect of wire configuration on the stability of the Ilizarov external fixator. Clin Orthop 279:299–302 [PubMed]
- 22.Calhoun JH, Ledbetter BR, Gill CA (1992) Biomechanics of the Ilizarov fixator for fracture fixation. Clin Orthop 280:15–22 [PubMed]
- 23.Roberts CS, Antoci V, Antoci V Jr, et al (2005) The effect of transfixion wire crossing angle on the stiffness of fine wire external fixation: a biomechanical study. Injury 36(9):1107–1112 [DOI] [PubMed]
- 24.Ilizarov GA, Emilyanova HS, Lebedev BE, et al (1772) Some experimental studies. Mechanical characteristics of Kirsherner wires. In: Perosseus compression and distraction osteosynthesis in traumatology and orthopedics. Kurgan, pp 34–47
- 25.Caja VL, Piza G, Navarro A (2003) Hydroxyapatite coating of external fixation pins decrease axial deformity during tibial lengthening for short stature. J Bone Jt Surg Am 85:1527–1531 [DOI] [PubMed]
- 26.Moroni A, Vannini F, Mosca M, et al (2002) State of the art review: techniques to avoid pin loosening and infection in external fixation. J Orthop Trauma 16:189–195 [DOI] [PubMed]
- 27.Piza G, Caja VL, Gonzalez-Viejo MA, et al (2004) Hydroxyapatite-coated external-fixation pins. The effect on pin loosening and pin-tract infection in lengthening for short stature. J Bone Jt Surg Br 86:892–897 [DOI] [PubMed]
- 28.Pommer A, Muhr G, David A (2002) Hydroxyapatite-coated Schantz pins in external fixators for distraction osteogenesis: a randomized, controlled trial. J Bone Jt Surg Am 84:1162–1166 [DOI] [PubMed]
- 29.Moroni A, Faldini C, Pegreffi F, et al (2002) Fixation strength of tapered versus bicylindrical hydroxyapatite-coated external fixation pins: an animal study. J Biomed Mater Res 63:61–64 [DOI] [PubMed]
- 30.Sarmiento A, Schaeffer JF, Beckerman L, et al (1977) Fracture healing in rat femora as affected by functional weight-bearing. J Bone Jt Surg Am 59:369–375 [PubMed]
- 31.Klein P, Schell H, Streitparth F, et al (2003) The initial phase of fracture healing is specifically sensitive to mechanical conditions. J Orthop Res 21:662–669 [DOI] [PubMed]
- 32.Herzenberg JE, Davis JR, Paley D, et al (1994) Mechanical distraction for treatment of severe knee flexion contractures. Clin Orthop Relat Res 301:80–88 [PubMed]
- 33.Huang SC (1996) Soft tissue contractures of the knee or ankle treated by the Ilizarov technique. High recurrence rate in 26 patients followed for 3–6 years. Acta Orthop Scand 67(5):443–449 [DOI] [PubMed]
- 34.Carmichael KD, Maxwell SC, Calhoun JH (2005) Recurrence rates of burn contracture ankle equines and other foot deformities in children treated with Ilizarov fixation. J Pediatric Orthop 25(4):523–528 [DOI] [PubMed]
- 35.Aarnes GT, Steen H, Ludvigsen P, et al (2005) In vivo assessment of regenerate axial stiffness in distraction osteogenesis. J Orthop Res 23:494–498 [DOI] [PubMed]