Abstract
Background
The risk of radiographic knee degeneration after partial or total meniscectomy is well documented, but no prior study has employed cartilage-sensitive MRI technology to assess degenerative changes after meniscectomy.
Hypothesis
Arthroscopic partial meniscectomy results in early articular cartilage wear and subchondral bony degeneration, even in the absence of clinical symptoms, and these findings can be evaluated with cartilage-sensitive MRI.
Study design
Retrospective cohort.
Methods
Twenty-nine patients (ages: 15–40) who had undergone isolated arthroscopic partial medial or lateral meniscectomy with at least 5-year follow-up were evaluated. All patients had arthroscopically normal articular cartilage at the time of initial meniscectomy. Seventeen patients (18 knees) underwent partial medial meniscectomy (MM) and 12 patients underwent partial lateral meniscectomy (LM) with mean follow-up of 8.4 and 7.1 years, respectively. Follow-up evaluation included physical examination, outcome questionnaires, and cartilage-sensitive MRI examination with modified Outerbridge grading of articular surfaces.
Results
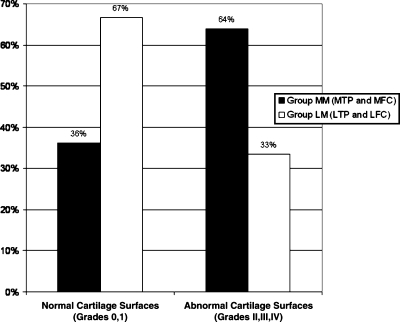
Outerbridge grades II–IV were noted in 64% of medial compartment joint surfaces in group MM knees versus 33% of lateral compartment joint surfaces in group LM knees. Abnormal cartilage surfaces (grades II–IV), subchondral sclerosis, and condylar squaring were all significantly more frequent after medial meniscectomy (p < 0.05). Groups MM and LM had no significant differences among outcome scores, which remained excellent in both groups. A significant negative correlation was found between the severity of cartilage wear and functional scoring in the MM group, suggesting that functional disability lags behind early MRI evidence of degeneration.
Conclusions
Despite optimal preoperative prognostic factors and excellent functional outcomes, MRI evidence of early articular cartilage degeneration was present in both partial medial and lateral meniscectomy patients at a minimum 5-year follow-up. Results support the use of cartilage-sensitive MRI as a noninvasive screening technique to evaluate cartilage changes after arthroscopic partial meniscectomy and may help to counsel the high-risk patient in regard to postoperative activity.
Key words: cartilage, meniscus, MRI, Knee
Introduction
Meniscal tears are common knee injuries with the incidence of acute tears approaching 60 in 100,000 [31]. The principal functions of the meniscus include load transmission, shock absorption, and passive stabilization of the tibio-femoral joint. The menisci transmit 50–90% of the weight-bearing load of the knee. Mechanical studies have demonstrated that after partial meniscectomy, an acute increase in knee joint contact pressures occurs; this phenomenon results in the remodeling of subchondral bone and the surrounding soft tissue [1, 4, 8, 18–21, 32]. The short-term results of patients treated with partial meniscectomy are excellent [3, 5, 23]. However, some studies have demonstrated the development of degenerative radiographic changes after partial meniscectomy [6, 7, 10, 26–28]. Due to the impractical nature of routine second-look arthroscopy and the previous limitations of conventional imaging modalities, the early effects of arthroscopic partial meniscectomy upon subchondral bone and articular cartilage have yet to be described. Recent advances in MRI technology have permitted the visualization of intraarticular components including articular cartilage [25]. The use of cartilage sensitive MRI to evaluate patients after arthroscopic partial meniscectomy has not been previously reported.
The authors hypothesize that arthroscopic partial meniscectomy results in early articular cartilage degeneration, even in the absence of clinical symptoms, and that these findings can be evaluated with cartilage-sensitive MRI. The purpose of this study was to analyze knee joint degenerative changes using cartilage-sensitive MRI techniques at a minimum of 5 years after isolated partial medial or lateral meniscectomy and to correlate these findings with clinical outcomes.
Materials and methods
Patients
A retrospective review of patients who underwent isolated arthroscopic partial medial or lateral meniscectomy was performed. Patients between the ages of 15 and 40 years at the time of partial medial or lateral meniscectomy were included. All subjects were evaluated at a minimum of 5-years postmeniscectomy. Patients with ligamentous injury, articular cartilage lesions, or combined lateral and medial meniscal pathology were excluded to allow a more accurate assessment of the effects of partial meniscectomy alone on the outcome measures. Three patients underwent partial meniscectomy within 4 to 7 months of failed meniscal repair (two medial and one lateral). No other patients had a history of prior knee surgery. Seventy-nine (79) patients who had a documented Outerbridge grade of 0 in the medial and lateral compartments at the time of index arthroscopy were identified by chart review. Fifty-eight (58) patients were contacted and 28 patients were available for follow-up MRI.
Operative reports from all patients were reviewed. The volume of meniscus excised could not be determined accurately, but the anatomic location of meniscectomy (anterior, middle, and/or posterior one-third) and extension of meniscectomy into the central, middle, or peripheral one-third of the meniscus was noted.
Follow-up evaluation
The follow-up assessment included the following: physical examination, functional, and cartilage-sensitive MRI examination of the operative knee. Physical examination of the knee assessed range of motion, clinical alignment, presence of an effusion, joint line tenderness, stability (Lachman, Pivot Shift), and provocative meniscal maneuvers (McMurray test, forced knee hyperflexion). Functional scoring included the Short Form-36 (SF-36) mental and physical component score, Lysholm score, Activities of Daily Living scale of the Knee Outcome Survey (ADL score), and Tegner activity score.
Magnetic resonance imaging was performed with a superconducting 1.5 Tesla unit (Signa, Horizon LX, General Electric Medical Systems, Milwaukee, WI), using a phased array send-receive knee coil (knee PA coil, MedRad, Indianola, PA). Images were obtained utilizing a previously validated cartilage pulse sequence as described by Potter et al. [25]. This sequence conforms with the following parameters: sagittal fast spin echo sequence with a repetition time (TR)/echo time (TE) 3,500–5,000/34 ms (effective), slice thickness 3.5 mm with no interslice gap, matrix 512 × 320–384, two excitations, variable receiver bandwidth of 32 kHz, echo train length 8–16, field of view 16 cm; coronal fast spin echo TR/TE 4,000–4,500/34 ms (effective), slice thickness 3.0 mm with no gap, matrix 512 × 256 at two excitations, echo train length 8–16, variable bandwidth of 32 kHz; sagittal fast spin echo with frequency-selective fat suppression (Chemsat, General Electric Medical Systems, Milwaukee, WI), TR/TE 4,000–4,500/40 ms (effective), slice thickness 3.5 to 4 mm with no gap, matrix 256 × 224 at two excitations, echo train length 8–12, variable bandwidth of 20.8 kHz.
Images were blindly assessed by a single examiner (HGP) for surface integrity and relative thickness of the articular cartilage using a modified Outerbridge classification [24]. All hyaline cartilage surfaces except the patella were assessed. Although the patella is well visualized by MRI, the focus of this study was compartment-specific chondral and subchondral changes after medial or lateral meniscectomy. The menisci were assessed for tears of the meniscal remnant and for new meniscal tears involving unoperated portions of the menisci. The signal characteristics of the subchondral bone were assessed on fat suppression sequences for the presence of subchondral edema. The high resolution, cartilage-sensitive sagittal images were used to assess subchondral trabecular sclerosis. Condylar squaring, consistent with Fairbanks’ [9] changes, was evaluated by dividing the condyle into tomographic sections on the coronal MR images and counting the number of sections involved with relative subchondral flattening or squaring of the condyles. This finding was graded as absent, involving less than 25% of the entire volume of the condyle, involving 25–50%, or involving greater than 50%. Osteophytes were denoted as absent, small (less than 2 mm), or large (greater than 2 mm). The morphology and signal characteristics of the anterior cruciate ligament, posterior cruciate ligament, collateral ligaments, and capsular structures were assessed.
Preoperative MRI evaluation was not performed using cartilage sensitive techniques in the majority of study patients. This prevented direct comparison of cartilage appearance on preoperative and follow-up imaging. However, all patients were documented to have grade 0 cartilage in the medial and lateral compartments at the index arthroscopy, and this has been previously shown to correlate well with cartilage-sensitive MRI findings [25].
Statistics
Statistical analysis was performed using SPSS for Windows (SPSS Inc., Chicago, IL). Fisher’s exact test was utilized for comparing proportions, the Mann–Whitney test was used for group mean comparison, and the Spearman rank correlation was used to assess variable correlation.
Results
Patient demographics
The partial medial meniscectomy group (group MM) was comprised of 18 knees in 17 subjects. Group MM consisted of 13 males and four females with a mean age of 26 years (range: 15–38 years) at the time of surgery. The mean body mass index (BMI) was 24.0 (range: 17.9 to 31.2), with normal BMI (<25) in 59% and elevated BMI (>25) in 41%. Detailed anatomic location of meniscectomy was available for 17 knees. All but one meniscectomy involved the posterior one-third of the meniscus, with 80% also involving the middle third and 13% extending into the anterior third. The meniscectomy involved only the central third (white–white zone) of the meniscus in 13%, extended into the middle third (red–white zone) in 47%, and extended into the peripheral third (red–red zone) in 40%.
The partial lateral meniscectomy group (group LM) was comprised of 12 knees in 12 subjects consisting of seven males and five females with a mean age of 27 years (range: 18–38 years) at time of surgery. The mean BMI was 26.2 (range: 19.3 to 45.6), with normal BMI (<25) in 45% and elevated BMI (>25) in 55%. Detailed anatomic location of meniscectomy was available for 10 knees. All meniscectomies involved the middle one-third of the meniscus, with 50% also involving the anterior third and 30% also involving the posterior third. The meniscectomy involved only the central third (white–white zone) of the meniscus in 10%, extended into the middle third (red–white zone) in 30%, and extended into the peripheral third (red–red zone) in 60%.
Partial medial meniscectomy (group MM)
Physical examination
Group MM patients were evaluated at a mean of 8.4 years (range: 5.5–11.6 years) postoperatively. At follow-up examination, all group MM patients had full range of motion (range: 0–145°). No patient had an effusion. Ligament stability tests (Lachman, Pivot Shift) were normal in all patients. Fifteen (82%) patients had neutral knee alignment, two (12%) had varus knee alignment, and one (6%) patient had valgus alignment by clinical observation. Four (24%) patients had medial joint line tenderness. Provocative meniscal maneuvers (McMurray, forced knee flexion) were positive in four (24%) patients.
Clinical outcomes
The SF-36 physical and mental component scores averaged 52.5 and 51.7, respectively. The Lysholm Knee Score averaged 91.9, the ADL Knee Score averaged 91.7, and the Tegner Activity Score averaged 4.8. (A Tegner score of 4 to 6 corresponds to physical fitness activities). The results are summarized in Table 1. One group MM patient underwent repeat arthroscopic partial medial meniscectomy for an adjacent meniscal tear 25 months after the index procedure, with final follow-up 5.4 years after the second procedure. No other group MM patient required additional surgery on the affected knee subsequent to arthroscopic partial medial meniscectomy.
Table 1.
Functional outcome scores
| Group MM (N = 18) | Group LM (N = 12) | |
|---|---|---|
| SF-36 physical component score | 52.5 ± 9.9 (range: 34.5–66.8) | 50.3 ± 8.9 (range: 29.5–58.3) |
| SF-36 mental component score | 51.7 ± 12.2 (range: 24.4–62.9) | 55.8 ± 4.0 (range: 48.0–62.2) |
| Lysholm knee score | 91.9 ± 9.7 (range: 68.0–100.0) | 91.4 ± 10.1 (range: 69.0–100.0) |
| ADL knee score | 91.7 ± 14.3 (range: 53.8–100.0) | 93.5 ± 9.0 (range: 75.0–100.0) |
| Tegner activity score | 4.8 ± 1.3 (range: 3.0–7.0) | 4.8 ± 1.9 (range: 3.0–9.0) |
The mean SF-36 physical and mental component score is 50 for normal, healthy individuals. The Lysholm and ADL are graded on a 100-point scale and the Tegner is graded on a 10-point scale.
MRI findings
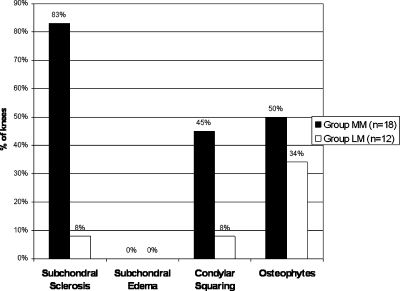
Each articular cartilage surface of the operative knee (medial femoral condyle, medial tibial plateau, lateral femoral condyle, lateral tibial plateau, trochlea) was graded using a modified Outerbridge classification. MRI evaluation of medial compartment cartilage surfaces (MTP and MFC) in group MM knees revealed the following Outerbridge grades: grade 0—16%; grade I—19%; grade II—44%; grade III—19%; and grade IV—0%. In contrast, lateral compartment cartilage surfaces (LTP and LFC) in group MM knees showed little change: grade 0—78%; grade I—19%; grade II—3%, grade III—0%; and grade IV—0%. MRI was used to determine the presence of medial compartment subchondral sclerosis (83%), bony edema (0%), condylar squaring (45%), and osteophytes (50%) (Fig. 1). MRI analysis also demonstrated the following: five knees (27%) with signal characteristics consistent with a tear of the medial meniscus remnant, one knee (6%) with a new tear of lateral meniscus, and one knee (6%) with a new low grade partial tear of the ACL. This patient had a normal Lachman (1 A).
Fig. 1.
Degenerative changes demonstrated by MRI in group MM and group LM
Partial lateral meniscectomy (group LM)
Physical examination
Group LM patients were evaluated at a mean of 7.1 years (range 5.4–11.1 years). All patients in this group had full range of motion (range: 0–145°). No patient had an effusion. Ten (84%) patients had neutral knee alignment and two (16%) had valgus knee alignment by clinical observation. Ligament stability tests (Lachman, Pivot Shift) were negative in all group LM patients. Provocative meniscal maneuvers (McMurray, forced knee flexion) were negative in all patients. One (8%) patient had lateral joint line tenderness.
Clinical outcomes
The SF-36 physical and mental component scores averaged 50.3 and 55.8, respectively. The Lysholm Knee Score averaged 91.4, the ADL Knee Score averaged 93.5, and the Tegner Activity Score averaged 4.8. Outcome measures for group LM are summarized in Table 1. No group LM patient required further surgery on the affected knee subsequent to arthroscopic partial lateral meniscectomy.
MRI findings
Evaluation of the lateral compartment cartilage surfaces (lateral tibial plateau and lateral femoral condyle) of group LM knees demonstrated the following modified Outerbridge grades: grade 0–38%; grade I—29%; grade II—29%; grade III—4%; and grade IV—0%. Medial compartment cartilage surfaces (MTP and MFC) in group LM knees showed the following: grade 0—71%; grade I—17%; grade II—8%, grade III—4%; and grade IV—0%. The presence of lateral compartment subchondral sclerosis (8%), edema (0%), condylar squaring (8%), and osteophytes (34%) is shown in Figure 1. MRI analysis also demonstrated that three knees (24%) had signal abnormalities consistent with tears of the lateral meniscus remnant (Fig. 2).
Fig. 2.
Magnetic resonance imaging of 26-year-old male 5.4 years status-post partial lateral meniscectomy. A retear of the lateral meniscal body is noted by the fluid imbibition present in the meniscal remnant (arrow)
Group MM versus group LM
Medial compartment cartilage change (Outerbridge grades II–IV) was significantly more common in group MM (64%) compared to group LM (12.5%) using Fisher’s exact test (p < 0.001). Lateral compartment cartilage change (II–IV) was significantly more common in group LM (33%) compared to group MM (3%) (p<0.01). Abnormal articular cartilage surfaces (Outerbridge grades II–IV) were noted on 23 (64%) of the 36 joint surfaces in the medial compartment of group MM knees (Fig. 3a, b). In group LM knees, abnormal cartilage surfaces were noted on 8 (33%) of the 24 lateral compartment cartilage surfaces. These findings are illustrated in Figure 4. There was a significantly increase in incidence of medial compartment cartilage change in group MM knees compared with lateral compartment cartilage change in group LM knees using Fisher’s exact test (p = 0.034).
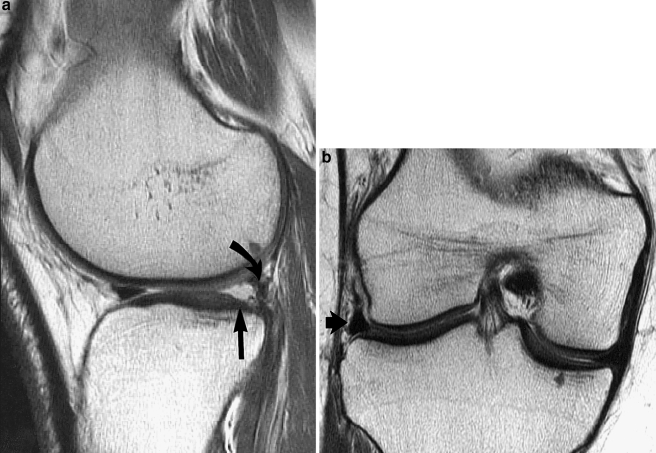
Fig. 3.
(a) Magnetic resonance imaging of a 39-year-old patient 10.5 years after partial medial meniscectomy. This image demonstrates partial thickness articular wear over the medial tibial plateau (straight arrow) with a small marginal osteophyte (curved arrow). In contrast, the articular cartilage over the lateral tibial plateau is full-thickness without wear. (b) Magnetic resonance imaging (sagittal fast spin echo) image of the same patient noted in (a) This image demonstrates the presence of degenerative meniscal remnant (curved arrow), anterior marginal osteophytes (short straight arrow), and moderate central articular cartilage wear over the medial tibial plateau (long straight arrow)
Fig. 4.
MRI cartilage appearance in medial compartment joint surfaces of group MM (MTP and MFC) versus lateral compartment joint surfaces of group LM (LTP and LFC)
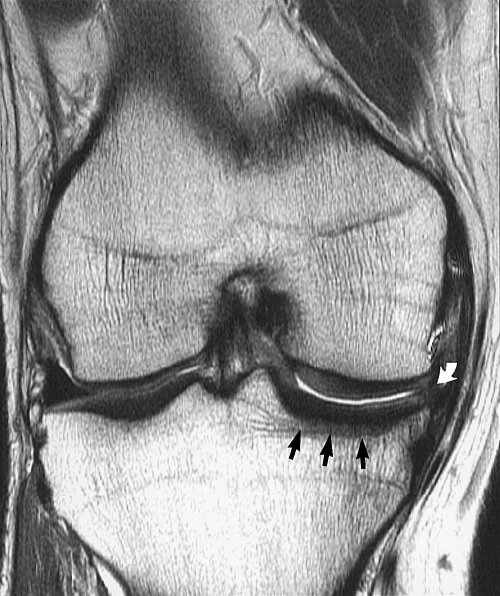
More severe cartilage wear (Outerbridge grades III–IV) was noted on seven (19%) of 36 medial compartment surfaces in group MM knees. Grade III–IV lesions were seen on one (4%) of 24 lateral compartment surfaces in group LM (Fig. 5a, b). A trend toward increased grade III–IV changes in MM patients compared to LM patients was noted but not significant using Fisher’s exact test (p = 0.125). Subchondral sclerosis was significantly more common in the medial compartment of group MM knees (83%) (Fig. 6) than in the lateral compartment of group LM knees (8%) (p < 0.001). Medial condylar squaring was also significantly more common in group MM knees (44%) than lateral condylar squaring in group LM knees (8%) (p < 0.05). The presence of osteophytes was noted in nine (50%) of 18 group MM knees (Fig. 3a, b) and in four (33%) of twelve group LM knees (p = 0.47) (Fig. 7).
Fig. 5.
(a) and (b) Magnetic resonance imaging of 26-year-old patient 7 years after lateral meniscectomy. This image demonstrates near full-thickness articular cartilage loss over the posterior margin of the lateral tibial plateau (straight arrow), with a small degenerative lateral meniscal remnant adjacent to the scarred fascicle (curved arrow). Subpanel B demonstrates the slight extrusion of the meniscal remnant (arrow) present
Fig. 6.
Magnetic resonance imaging of 26-year-old patient 10.3 years status-post after partial medial meniscectomy. This image demonstrates a small degenerative meniscal remnant that is extruded into the medial gutter (curved arrow). Note the subchondral sclerosis over the medial tibial plateau (straight arrows), as well as moderate articular cartilage wear over the weight-bearing area of the medial compartment
Fig. 7.
Magnetic resonance imaging of a 30-year-old patient 11 years after partial lateral meniscectomy. This image demonstrates moderate wear of the articular cartilage over the lateral compartment with small marginal osteophytes (arrow)
There was no significant difference in the functional outcome scores of group MM and LM patients at the follow-up interval by Mann–Whitney comparison (SF-36 Physical component score: p = 0.18; SF-36 Mental component score: p = 0.95; Lysholm: p = 0.96; ADL: p = 0.70; Tegner: p = 0.82).
Patient gender had no relationship to the severity of cartilage change in either group MM (p = 1.0) or group LM (p = 0.20). Body mass index (normal < 25 versus elevated > 25) did not show a statistically significant relationship to the presence of cartilage change in either group MM (p = 0.44) or group LM (p = 0.39). In addition, no correlation between patient age and severity of cartilage change was observed in either group MM (rs = 0.12) or group LM (rs = −.09). In group MM, a significant negative correlation was found between the severity of cartilage wear and Lysholm (rs = −0.740), ADL (rs = −0.755), and Tegner (rs = −0.562) scores. No such correlation was observed between cartilage wear and outcome scores in group LM.
Discussion
This study demonstrates that, despite good functional outcomes, partial medial or lateral arthroscopic meniscectomy resulted in local cartilage wear and degenerative subchondral changes at a minimum 5-year follow-up interval. The extent of these cartilage changes was detectable by MRI, which offers an ideal noninvasive modality for evaluating cartilage surfaces over time after meniscectomy. Of particular significance, these degenerative changes were detected in patients who had normal articular cartilage at the index procedure and who lacked negative prognostic indicators, suggesting the meniscectomy itself was responsible for the changes.
Historically, total meniscectomy represented the standard of care for patients with symptomatic meniscus tears. Long-term studies suggest that total meniscectomy results in both poor functional outcome and significant degenerative changes as noted on radiographs [2, 9, 14, 16, 17, 30]. These studies illustrated the clinical importance of the meniscus to long-term knee function. Early studies of open partial meniscectomy techniques demonstrated satisfactory results at 4- to 5-year follow-up [22, 23]. With the advent of arthroscopy, arthroscopic partial meniscectomy has supplanted open procedures as the treatment of choice for irreparable symptomatic meniscal tears. Patients who undergo arthroscopic partial meniscectomies recover more quickly and have higher functional scores than patients undergoing total or partial open meniscectomies at similar follow-up intervals [12, 23].
Recent studies have evaluated the clinical efficacy of arthroscopic partial meniscectomy in medium to long-term follow-up. At a minimum 5-year follow-up, Bolano and Grana [6] reported satisfactory knee function in 82% of patients who underwent arthroscopic partial medial meniscectomy. Additional studies have reported excellent to good results in 48 to 95% of patients at 12 to 14 years after surgery [7, 13, 29]. Factors associated with satisfactory subjective results are variable. Bolano and Grana [6] report that positive prognostic factors include age less than 40 years, symptoms less than 12 months duration, tear type, and ipsilateral cartilage Outerbridge grading less than grade II at the time of arthroscopy. Burks et al. [7] implicated ligamentous instability as a negative factor in predicting clinical outcome after arthroscopic partial meniscectomy. Schimmer et al. [29] report that preexisting damage to the articular cartilage at the time of arthroscopy has the most profound impact on long-term results of partial meniscectomies. These authors found that 62% of patients with cartilage lesions noted at the index arthroscopy rated excellent to good at 12 years versus 94.8% of patients with isolated meniscal tears. Higuchi et al. [13] also reported existing cartilage damage along with the volume of meniscus excised as factors predicting long-term results.
The radiographic changes associated with total meniscectomy are well documented, and numerous reports show similar radiographic changes after arthroscopic partial meniscectomy [5, 6, 10, 15, 26, 28]. At 5-year minimum follow-up, Bolano and Grana [6] noted that 62% of the patients in their series demonstrated Fairbanks’ changes after partial meniscectomy. Fauno and Nielsen [10] reported Fairbanks’ changes in 53% of partial meniscectomy patients at 8.5-year follow-up. Rangger et al. [26] reported the progression of osteoarthritic changes in 38% of medial and 24% of lateral meniscectomy patients at 4.5 years. Rockborn and Gilliquist [28] found that radiographic change was four times more likely to occur in the operative knee after partial meniscectomy when compared to the contralateral nonoperative knee. In the current literature, the proposed risk factors for postoperative radiographic change have been inconsistent. While Benedetto and Rangger [5] suggest that preexisting cartilage wear is a predictor of radiographic change after partial medial meniscectomy, others suggest that cartilage wear is not relevant [11, 26–28]. The volume of the excised meniscus has also been correlated with the development of radiographic change [13, 27]. Increased age [26], female sex [7], lateral meniscectomy [5, 15], and ACL insufficiency [7] have also been identified as possible negative prognostic factors.
The current study sought to assess both the clinical outcomes and the MRI appearance of the articular cartilage in patients after isolated partial meniscectomy. In an attempt to control for the confounding variables noted above, the study group was limited to patients who had undergone isolated partial medial or lateral meniscectomy. All patients with gross cartilage changes or ligamentous instability were excluded to allow a more accurate examination of the effect of partial meniscectomy on the medial or lateral compartment. The cartilage-sensitive MRI pulsing sequence used to evaluate these patients is relatively new at our institution and was not routinely being used when these patients underwent preoperative imaging. This prevented the direct comparison of preoperative and follow-up MRI findings. However, Potter et al [25] have previously identified cartilage-sensitive MRI as a novel and accurate tool for assessing articular cartilage changes. MRI cartilage grading using a cartilage-sensitive pulse sequence has been shown to have a sensitivity of 87%, specificity of 92%, and accuracy of 94% when compared to identification and grading of cartilage lesions during arthroscopy [25]. Since all patients with gross cartilage changes of the femoral or tibial articular surfaces at initial arthroscopy were excluded from this study, we feel confident that cartilage changes identified on follow-up MRI imaging were not related to the initial traumatic event.
It is apparent that despite a lack of clinical symptoms, cartilage wear does occur in the operative compartment after partial meniscectomy. MRI signal intensity and morphologic changes consistent with early articular cartilage degeneration were present in both partial medial and lateral meniscectomy patients at this intermediate follow-up interval. Abnormal cartilage, subchondral sclerosis, and condylar squaring were all significantly more frequent after partial medial meniscectomy than lateral meniscectomy. A trend toward increased severity (grades III and IV) of cartilage lesions after medial meniscectomy was noted but did not reach statistical significance. A larger study population may have revealed significant differences. Furthermore, if the rate of progression of cartilage degeneration is truly greater after medial meniscectomy, longer-term follow-up in this same cohort may reveal a significant relationship between medial meniscectomy and higher Outerbridge grade.
The functional outcomes of groups MM and LM were evaluated by four validated instruments. As in previous studies of similar follow-up, the average scores of patients in both groups were good to excellent [6, 7, 13, 29]. Patients who demonstrated more severe grades of cartilage wear after medial meniscectomy had relatively lower functional outcome scores. This suggests that clinical disability lags somewhat behind MRI evidence of articular cartilage degeneration after partial meniscectomy. The objective follow-up provided by MRI is a vital adjunct to the more subjective outcome measures, as this provides a more comprehensive understanding of the development of arthritis after meniscectomy.
Despite the overall excellent functional scores at this follow-up, the cartilage wear noted in these patients will likely have consequences on long-term function, especially if one hypothesizes that these findings are representative of a progressive local process that will ultimately result in symptomatic degeneration over time. This study presents new material regarding the use of cartilage-sensitive MRI as a noninvasive screening technique to detect preclinical degenerative changes. The early changes in articular cartilage and bony structures noted on MRI may help the clinician counsel patients with regard to activity level after surgery and ultimate prognosis. The patients involved in this study remained physically active with a high average postoperative Tegner score. This may have contributed to the cartilage changes observed on MRI. After partial meniscectomy, patients may be advised to curtail high-impact activities in light of the cartilage degeneration noted in this group of asymptomatic postmeniscectomy patients.
Knee alignment was assessed clinically in this study, with five of 30 knees showing some malalignment at follow-up. Weight-bearing lower extremity alignment radiographs were not obtained. Correlation of radiographic alignment with cartilage-sensitive MRI findings could be an important direction for future investigations. Another limitation of this study is the limited understanding of preoperative meniscal tear quality (i.e., acute, degenerative) and the characterization of tear morphology and degree. These parameters may effect the development of the MRI findings noted in the present study.
Conclusions
MRI evidence of articular cartilage wear and bony degeneration occurs in patients who undergo isolated partial medial or lateral meniscectomy at a minimum 5-year follow-up interval. Articular cartilage wear, subchondral sclerosis, and condylar squaring were significantly more common after medial meniscectomy than lateral meniscectomy. A trend toward increased severity in the medial meniscectomy group was noted but did not reach statistical significance. Overall, these changes did not affect functional scoring, which remained excellent using four different outcome measures. Only higher grade cartilage changes after medial meniscectomy correlated with lower functional outcomes, suggesting that functional disability lags behind MRI evidence of early degeneration. The results of this study support the use of cartilage-sensitive MRI analysis as a noninvasive screening technique to evaluate cartilage changes after arthroscopic partial meniscectomy, and may help to counsel the high-risk patient in regard to postoperative activity. Longer-term follow-up using cartilage-sensitive MRI has the potential to expand our current understanding of the natural history of isolated partial meniscectomy.
Acknowledgements
This study was supported by a grant from the Institute for Sports Medicine Research, New York, New York. The authors acknowledge the assistance of Stephen J. O’Brien, MD; David W. Altchek, MD; Thomas J. Wickiewicz, MD; and Russell F. Warren, MD in the completion of this manuscript.
References
- 1.Aagaard H, Verdonk R (1999) Function of the normal meniscus and consequences of meniscal resection. Scand J Med Sci Sports 9:134–140 [DOI] [PubMed]
- 2.Abdon P, Turner MS, Pettersson H, Lindstrand A, Stenstrom A, Swanson AJ (1990) A long-term follow-up study of total meniscectomy in children. Clin Orthop 257:166–170 [PubMed]
- 3.Aglietti P, Buzzi R, Bassi PB, Pisaneschi A (1986) Results of arthroscopic meniscectomy. Ital J Orthop Traumatol 12:315–325 [PubMed]
- 4.Baratz ME, Fu FH, Mengato R (1986) Meniscal tears: the effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee. A preliminary report. Am J Sports Med 14:270–275 [DOI] [PubMed]
- 5.Benedetto KP, Rangger C (1993) Arthroscopic partial meniscectomy: 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 1:235–238 [DOI] [PubMed]
- 6.Bolano LE, Grana WA (1993) Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at five years. Am J Sports Med 21:432–437 [DOI] [PubMed]
- 7.Burks RT, Metcalf MH, Metcalf RW (1997) Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy 13:673–679 [DOI] [PubMed]
- 8.Cox JS, Nye CE, Schaefer WW, Woodstein IJ (1975) The degenerative effects of partial and total resection of the medial meniscus in dogs’ knees. Clin Orthop 109:178–183 [DOI] [PubMed]
- 9.Fairbanks TJ (1948) Knee joint changes after meniscectomy. J Bone Joint Surg Br 30B:664–670 [PubMed]
- 10.Fauno P, Nielsen AB (1992) Arthroscopic partial meniscectomy: a long-term follow-up. Arthroscopy 8:345–349 [DOI] [PubMed]
- 11.Gillquist J, Hamberg P, Lysholm J (1982) Endoscopic partial and total meniscectomy. A comparative study with a short term follow up. Acta Orthop Scand 53:975–979 [DOI] [PubMed]
- 12.Hede A, Larsen E, Sandberg H (1992) Partial versus total meniscectomy. A prospective, randomised study with long-term follow-up. J Bone Joint Surg Br 74:118–121 [DOI] [PubMed]
- 13.Higuchi H, Kimura M, Shirakura K, Terauchi, M Takagishi K (2000) Factors affecting long-term results after arthroscopic partial meniscectomy. Clin Orthop 377:161–168 [DOI] [PubMed]
- 14.Jackson JP (1968) Degenerative changes in the knee after meniscectomy. Br Med J 2:525–527 [DOI] [PMC free article] [PubMed]
- 15.Jaureguito JW, Elliot JS, Lietner T, Dixon LB, Reider B (1995) The effects of arthroscopic partial lateral meniscectomy in an otherwise normal knee: a retrospective review of functional, clinical, and radiographic results. Arthroscopy 11:29–36 [DOI] [PubMed]
- 16.Johnson RJ, Kettelkamp DB, Clark W, Leaverton P (1974) Factors effecting late results after meniscectomy. J Bone Joint Surg Am 56:719–729 [PubMed]
- 17.Jorgensen U, Sonne-Holm S, Lauridsen F, Rosenklint A (1987) Long-term follow-up of meniscectomy in athletes. A prospective longitudinal study. J Bone Joint Surg Br 69:80–83 [DOI] [PubMed]
- 18.Krause WR, Pope MH, Johnson RJ, Wilder DG (1976) Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am 58:599–604 [PubMed]
- 19.Levy IM, Torzilli PA, Gould JD, Warren RF (1989) The effect of lateral meniscectomy on motion of the knee. J Bone Joint Surg Am 71:401–406 [PubMed]
- 20.Levy IM, Torzilli PA, Warren RF (1982) The effect of medial meniscectomy on anterior–posterior motion of the knee. J Bone Joint Surg Am 64:883–888 [PubMed]
- 21.McBride ID, Reid JG (1988) Biomechanical considerations of the menisci of the knee. Can J Sport Sci 13:175–187 [PubMed]
- 22.McGinity JB, Geuss LF, Marvin RA (1977) Partial or total meniscectomy: A comparative analysis. J Bone Joint Surg Am 59:763–766 [PubMed]
- 23.Northmore-Ball MD, Dandy DJ, Jackson RW (1983) Arthroscopic, open partial, and total meniscectomy. A comparative study. J Bone Joint Surg Br 65:400–404 [DOI] [PubMed]
- 24.Outerbridge RE, Dunlop JA (1975) The problem of chondromalacia patellae. Clin Orthop 110:177–196 [DOI] [PubMed]
- 25.Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB (1998) Magnetic resonance imaging of articular cartilage in the knee. An evaluation with use of fast-spin–echo imaging. J Bone Joint Surg Am 80:1276–1284 [DOI] [PubMed]
- 26.Rangger C, Klestil T, Gloetzer W, Kemmler G, Benedetto KP (1995) Osteoarthritis after arthroscopic partial meniscectomy. Am J Sports Med 23:240–244 [DOI] [PubMed]
- 27.Rockborn P, Gillquist J (1995) Outcome of arthroscopic meniscectomy. A 13-year physical and radiographic follow-up of 43 patients under 23 years of age. Acta Orthop Scand 66:113–117 [DOI] [PubMed]
- 28.Rockborn P, Gillquist J (1996) Long-term results after arthroscopic meniscectomy. The role of preexisting cartilage fibrillation in a 13 year follow-up of 60 patients. Int J Sports Med 17:608–613 [DOI] [PubMed]
- 29.Schimmer RC, Brulhart KB, Duff C, Glinz W (1998) Arthroscopic partial meniscectomy: A 12-year follow-up and two-step evaluation of the long-term course. Arthroscopy 14:136–142 [DOI] [PubMed]
- 30.Tapper EM, Hoover NW (1969) Late results after meniscectomy. J Bone Joint Surg Am 51:517–526 (passim) [PubMed]
- 31.Teurlings L (1999) Meniscal injuries. In: Arendt EA (ed) Orthopaedic knowledge update: sports medicine 2. American Academy of Orthopedic Surgeons, Rosemont, IL, pp 349–353
- 32.Walker PS, Erkman MJ (1975) The role of the menisci in force transmission across the knee. Clin Orthop 109:184–192 [DOI] [PubMed]