Abstract
Haglund's syndrome is a cause of retrocalcaneal pain. The clinical diagnosis of Haglund's syndrome is often confusing as the clinical picture may mimic other causes of hindfoot pain such as isolated retrocalcaneal bursitis or hindfoot involvement from more systemic arthropathies such as Reiter's syndrome or rheumatoid arthritis. With the increasing frequency of employing sonography as a diagnostic tool in the evaluation of foot and ankle pathology, recognition of the sonographic appearance of Haglund's complex is important. We report a case of Haglund's syndrome diagnosed and treated with sonography.
Haglund's syndrome is a constellation of soft tissue and bony abnormalities and represents one cause of retrocalcaneal pain consisting of inflammation of the regional soft tissues, e.g., retrocalcaneal bursitis, superficial tendo Achilles bursitis, and thickening and/or inflammation of the Achilles tendon, associated with a prominent bony contour of the posterior calcaneus [1]. Each of the soft tissue abnormalities can occur in isolation and need to be distinguished from the Haglund's complex, as the etiologic factors and treatment of these various entities are different.
The diagnosis is often made clinically, with imaging confirmation made by noting the prominence of the calcaneal bursal projection as well as increased density in the deep and superficial pre-Achilles bursae on a standing lateral radiograph [2]. There have been few case reports describing the ultrasound appearance of isolated retrocalcaneal bursitis, but none, to our knowledge, describing the constellation of findings consistent with Haglund's syndrome nor the utility of sonography to guide treatment [3].
We report a case of Haglund's syndrome, diagnosed clinically, confirmed radiographically, more specifically evaluated with sonography, and treated with sonographic-guided retrocalcaneal bursal injection.
Case presentation
A 48-year-old man with right retrocalcaneal pain for approximately 5 years presented with pain on palpation at the distalmost aspect of the Achilles tendon insertion. Subtalar joint range of motion was decreased in dorsiflexion, plantarflexion, inversion, and eversion.
Conventional lateral standing radiographs of the right ankle demonstrated an ovoid, or tear-shaped, density in between the calcaneus and the Achilles tendon insertion, which is normally radiolucent (Fig. 1). This area is the inferiormost aspect of the pre-Achilles fat pad (retrocalcaneal recess), and density in this region indicates retrocalcaneal bursitis. Mild convexity of the soft tissues superficial to the Achilles tendon insertion was present, consistent with superficial tendo Achilles bursitis. The Achilles tendon shadow was thickened and ill defined consistent with inflammation. The prominent osseous bursal projection in association with this constellation of soft tissue findings is consistent with the radiographic diagnosis of Haglund's syndrome (Fig. 1).
Fig. 1.
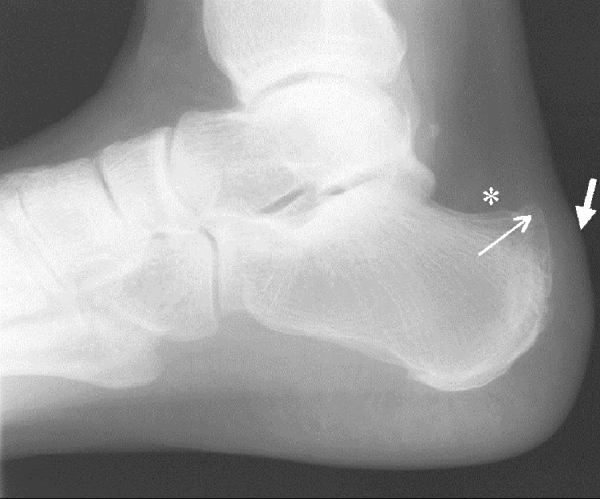
Lateral standing radiograph of the hindfoot demonstrates a prominent posterosuperior osseous calcaneal protuberance (arrow) with a vague, cloudy density in the deep retrocalcaneal bursa (*) consistent with retrocalcaneal bursitis. Superficial tendoAchilles bursitis is demonstrated by convexity of the soft tissues (short thick arrow) and an ill-defined Achilles tendon at its insertion consistent with inflammation
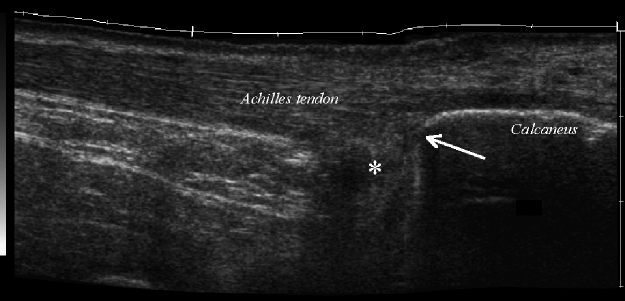
Sonographic evaluation of the right Achilles tendon was performed using a high-frequency (13 MHz) linear transducer (Siemens Sonoline Elegra; Siemens Medical Systems, Mountainview, CA, USA) with the patient prone. Sonographic evaluation demonstrated fusiform enlargement and inhomogeneity of the distal Achilles tendon with marked inhomogeneity of the tendon along its deep surface close to the enthesis, consistent with insertional tendinosis. The deep retrocalcaneal bursa contained complex hypoechoic fluid and a nodular echogenic soft tissue component consistent with retrocalcaneal bursitis (Fig. 2). Thickening of the superficial pre-Achilles bursa was also identified.
Fig. 2.
Longitudinal extended field of view sonographic image of the hindfoot demonstrates the prominent osseous protuberance at the posterosuperior margin of the calcaneus (arrow) and hypoechoic distention of the retrocalcaneal bursa (*). Thickening of the superficial tendon Achilles bursa is also present
Ultrasound guided injection of the retrocalcaneal bursa was performed with the patient prone and the foot maximally dorsiflexed. Topical povidone–iodine solution (Allegiance Healthcare Corp., McGaw Park, IL, USA) was used. Using a short-axis, transverse approach, a 13-MHz linear transducer was used to guide the injection. Given the superficial nature of the retrocalcaneal bursa, a short (1.5-inch), thin (25-gauge) needle was utilized. The linear echogenic needle tip was seen to enter the complex bursal fluid in the deep retrocalcaneal bursa during real-time evaluation. The probe was then readjusted into the longitudinal direction during the injection to observe the echogenic microbubbles fill the retrocalcaneal bursa (Fig. 3). A 2-mL mixture of 0.5 mL 1% lidocaine (Abbot Laboratories, North Chicago, IL, USA), 0.5 mL 0.5% bupivacaine (Sensorcaine, Astra Pharmaceuticals, Westborough, MA, USA) and 1.0 mL (40 mg) of triamcinolone (Kenalog, Apothecon, a Bristol-Myers Squibb Company, Princeton, NJ, USA) was injected.
Fig. 3.
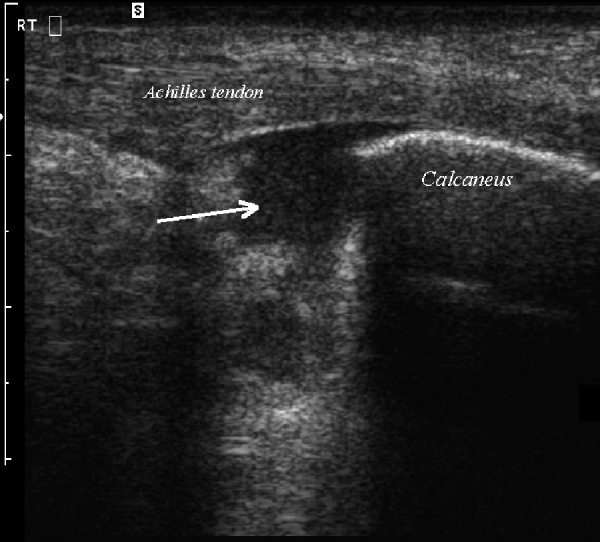
Longitudinal sonogram of the hindfoot after ultrasound guided retrocalcaneal bursal injection demonstrates hypoechoic material with internal low levels echoes distending the bursa, representing the injected steroid/anesthetic material (arrow)
Several minutes postinjection, the patient reported significant symptomatic improvement. A prescription orthotic device was dispensed to reduce excessive rearfoot motion and force on the Achilles tendon insertion point.
Discussion
Haglund's syndrome was first described in 1928 as retrocalcaneal bursitis in the setting of an abnormal protuberance of the posterosuperior border of the calcaneus, identified in the association with golf shoes, which have a hard posterior shoe contour [1]. Haglund's syndrome continues to be a not uncommon cause of retrocalcaneal pain, with swelling of the superficial tendo Achilles bursa, retrocalcaneal bursitis, Achilles tendinosis, and a prominent bursal projection of the calcaneus.
Clinically, a prominent calcaneal posterosuperior protuberance is observed, usually on the lateral side, often with swelling and regional inflammatory changes [4]. A rigid, plantarflexed first toe may predispose one to Haglund's deformity and retrocalcaneal bursitis by resulting in hindfoot varus [4]. In addition, prominent plantar osseous projections can also alter the bone–soft tissue interface of the hindfoot [5]. Clinically, by physical examination alone, it may be difficult to distinguish Haglund's syndrome from other causes of hindfoot pain such as Reiter's disease, rheumatoid arthritis, or isolated local conditions such as superficial tendo Achilles bursitis secondary to poor shoe fit. Distinguishing the specific etiology of focal from systemic causes of posterior hindfoot pain is essential to initiating appropriate treatment.
Radiographic features have been described, including a measurement method, (parallel pitch line) to confirm the presence of a prominent bursal projection and the Haglund's complex [2, 5]. When the posterior calcaneal border is prominent but subtle, objective measurement on the radiographic evaluation is important, to distinguish Haglund's syndrome from isolated retrocalcaneal bursitis, superficial tendo Achilles bursitis, or Achilles tendinosis. With more systemic conditions such as Reiter's syndrome or rheumatoid arthritis, retrocalcaneal bursitis is usually an isolated finding and more diffuse; additionally, associated erosive changes of the calcaneal bursal projection may be present.
Surgical treatment options, including retrocalcaneal decompression and calcaneal ostectomy or osteotomy, have varying results [4,6–8]. Inadequate bone resection can lead to recurrence of symptoms, with other postsurgical complications potentially including scar formation with nerve entrapment, weakening or rupture of the Achilles tendon, and nonunion of the calcaneal osteotomy [9].
Conservative treatment options include reassessment of the footwear the patient is currently wearing, the use of heel inserts, and oral anti-inflammatory medication [4]. The effects of heel elevation on the relationship between the calcaneal bursal projection and the Achilles tendon and retrocalcaenal bursa have been described [5]. Although the size of the calcaneal bursal projection remains the same when the heel is elevated, the plantar calcaneal pitch angle decreases and shifts the osseous calcaneal bursal projection away from the retrocalcaneal soft tissues, decreasing friction and irritation [5].
Previous ultrasound studies have reported 100% specificity but only 50% sensitivity in ultrasound diagnosis of retrocalcaneal bursitis, and were less sensitive in diagnosing superficial Achilles bursal involvement in the setting of spondyloarthropathy [3]. Their study however, employed a 7.5-MHz transducer, possibly accounting for the lower sensitivity in diagnosing superficial tendo Achilles bursal involvement. In the case reported here, a high-frequency, linear, 13-MHz transducer was used for examining the retrocalcaneal region. Both superficial and retrocalcaneal bursae as well as the Achilles tendon were evaluated as well as the superficial (dorsal) margin of the calcaneus noting the prominent bursal projection. As soon as the diagnosis of retrocalcaneal bursitis is established and the sonographic findings correlate with those of a Hagland's syndrome, anesthetic and steroid mixture injection can be performed as part of the examination.
Our experience with intrabursal injections is that patients do well immediately postinjection lasting several hours, from the local anesthetic properties of lidocaine and Sensorcaine. Patients then experience a short window of relapsed pain for the following 24–48 h until the anti-inflammatory effects of the Kenalog is established. As soon as the steroid takes effect, patients have reported a variable length of pain relief (ranging from weeks to months).
Clinically, the symptoms that lead the patient to seek medical care are often the pain and inflammation associated with retrocalcaneal bursitis and Haglund's syndrome from chronic friction and pressure from the calcaneal bursal projection. Using ultrasound guidance to inject the retrocalcaneal bursa is a simple, reliable method of ensuring accurate delivery of medication into the bursa and avoiding intratendinous injection. In the current case, the patient had complete relief of symptoms following the procedure. This nonsurgical treatment trial, combined with modifications in daily shoe wear, is an appropriate initial treatment for pain relief of Haglund's syndrome.
References
- 1.Haglund P. Beitrag zur Klinik der Achillessehne. Z Orthop Chir. 1927;49:49–58. [Google Scholar]
- 2.Pavlov H, Heneghan MA, Hersh A, Goldman AB, Vigorita V. The Haglund syndrome: initial and differential diagnosis. Radiology. 1982;144(1):83–88. doi: 10.1148/radiology.144.1.7089270. [DOI] [PubMed] [Google Scholar]
- 3.Olivieri I, Barozzi L, Padula A, DeMatteis M, Pierro A, Cantini F, Salvarani C, Pavlica P. Retrocalcaneal bursitis in spondyloarthropathy: assessment by ultrasonography and magnetic resonance imaging. J Rheumatol. 1998;25(7):1352–1357. [PubMed] [Google Scholar]
- 4.Stephens MM. Haglund's deformity and retrocalcaneal bursitis. Orthop Clin North Am. 1994;25(1):41–46. [PubMed] [Google Scholar]
- 5.Heneghan MA, Pavlov H. The Haglund painful heel syndrome: experimental investigation of cause and therapeutic implications. Clin Orthop. 1984;187:228–234. [PubMed] [Google Scholar]
- 6.Sella EJ, Caminear DS, McLarney EA. Haglund's syndrome. J Foot Ankle Surg. 1998;37(2):110–114. doi: 10.1016/s1067-2516(98)80089-6. [DOI] [PubMed] [Google Scholar]
- 7.Kolodziej P, Glisson RR, Nunley JA. Risk of avulsion of the Achilles tendon after partial excision for treatment of insertional tendonitis and Haglund's deformity: a biomechanical study. Foot Ankle Int. 1999;20(7):433–437. doi: 10.1177/107110079902000707. [DOI] [PubMed] [Google Scholar]
- 8.Watson AD, Anderson RB, Davis WH. Comparison of results of retrocalcaneal decompression for retrocalcaneal bursitis and insertional Achilles tendinosis with calcific spur. Foot Ankle Int. 2000;21(8):638–642. doi: 10.1177/107110070002100802. [DOI] [PubMed] [Google Scholar]
- 9.Reinherz RP, Smith BA, Henning KE. Understanding the pathologic Haglund's deformity. J Foot Surg. 1990;29(5):432–435. [PubMed] [Google Scholar]