A 26-year-old male presented for magnetic resonance (MR) examination of the ankle for chronic ankle pain.
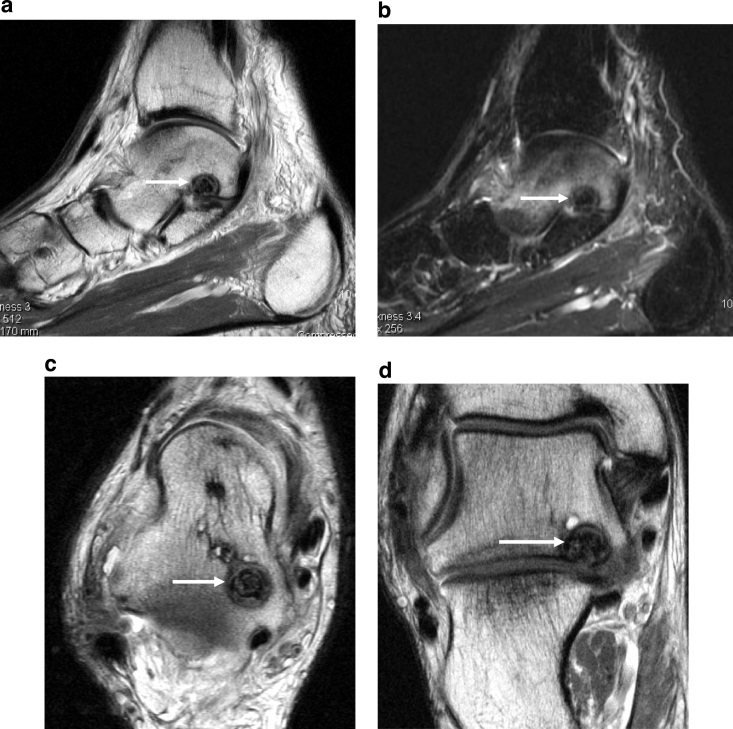
MR images of the ankle revealed marked intraosseous bone marrow hyperintensity involving the talus on the fast inversion recovery sequence (Fig. 1). In addition, at the anteromedial margin of the posterior facet of the talus, a round, sclerotic lesion was present with an associated mild to moderate reactive synovitis in the subtalar joint (Fig. 1). Findings were consistent with an osteoid osteoma.
Fig. 1.
Selected magnetic resonance (MR) images of the hindfoot demonstrating the osteoid osteoma. Sagittal fast spin echo image (a) demonstrates the central nidus and peripheral rim of reactive sclerosis (arrow). Sagittal fast inversion recovery sequence (b) again demonstrates the low-signal intensity (sclerotic) nidus (arrow); also, of note, is moderate reactive intraosseous edema in the talus. Axial fast spin echo MR image (c) demonstrates the lesion (arrow) along the posteromedial margin of the talus. Oblique coronal fast spin echo MR image (d) demonstrates the relationship of the lesion (arrow) to the subtalar joint
Patient was referred for computed tomography (CT)-guided radiofrequency ablation of the lesion. Preprocedure CT images of the ankle again demonstrate the well-marginated sclerotic lesion in the posterior facet of the talus with a hypodense rim and centrally calcified nidus (Fig. 2).
Fig. 2.
Selected computerized tomography (CT) images of the hindfoot viewed with bone algorithm. Sagittal image (a), oblique coronal (b), and axial (c) images demonstrate the sclerotic central nidus of the osteoid osteoma (arrow)
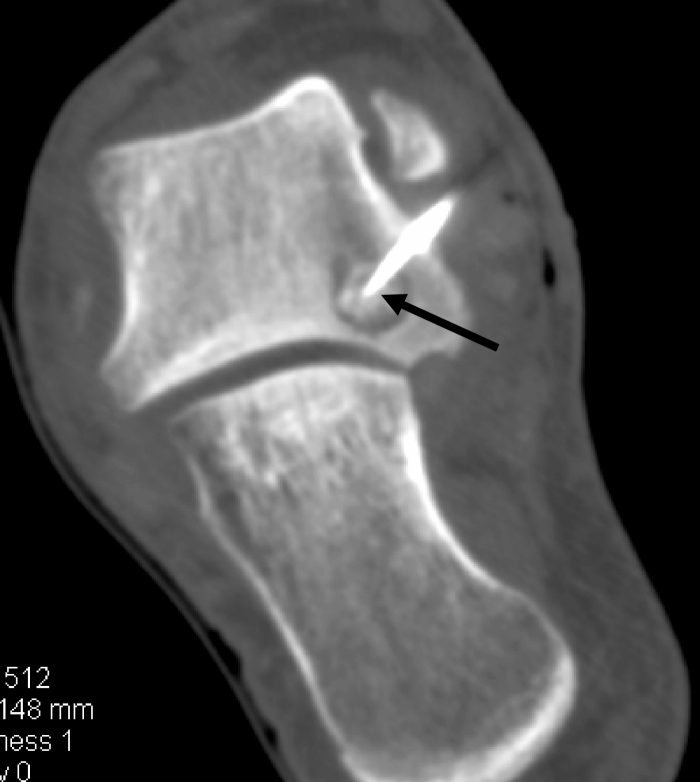
For the procedure, a radiofrequency probe was inserted into the lesion under CT guidance (Fig. 3). The probe was heated to 90°C for 6 min in the inferior and subsequently, the superior, portions of the lesion. The patient did well postprocedure.
Fig. 3.
Oblique coronal CT image taken during the radiofrequency ablation procedure with the patient in a lateral decubitus position, demonstrates the radiofrequency probe (arrow) centrally within the lesion
Discussion
Osteoid osteoma is a benign skeletal tumor composed of a vascular central nidus and a surrounding rim of reactive sclerotic bone. They are common in younger patients (below 25 years of age). Patients often present with night pain, characteristically relieved by aspirin, and improving with activity. Osteoid osteomas may occur in both cortical as well as cancellous bone.
Plain film radiographic diagnosis of osteoid osteoma is made by visualizing a radiolucent nidus with a moderate reactive sclerotic rim. Cortical-based lesions in the long bones may demonstrate fairly solid periosteal reaction. Plain film radiographic findings may be noncontributory; however, this depends on where the lesion is located and the ability to clearly visualize the area.
As the clinical signs and symptoms are often nonspecific, and can mimic those of other conditions, if the radiolucent nidus is not clearly identified, lesions may be confused with other entities such as a stress fracture. In addition, the nidus may not be clearly identified, especially with intra-articular lesions, further hindering radiographic diagnosis [1]. In questionable cases, further imaging may be obtained with CT or MR to better visualize the nidus [2].
Patients are often referred to MR examination with nonspecific clinical signs and symptoms, with osteoid osteoma often being an unexpected diagnosis. Lesions, especially in the femoral neck, may be mistaken for other etiologies such as a more aggressive neoplasm or stress fracture, especially if the nidus is small and the surrounding osseous reaction is pronounced [3, 4]. Lesions that are intra-articular may incite a reactive synovitis, occasionally further clouding the imaging diagnosis, especially if they occur in an unusual location such as the foot or ankle [5]. Cortical based lesions may also demonstrate a moderate amount of soft tissue involvement [6].
MR imaging should include thin-section, high-resolution images to clearly identify the nidus (see Fig. 1). At least one water-sensitive pulse sequence should be included to visualize the reactive edema surrounding the lesion, which can be marked especially in younger patients [7]. Consideration of the presence of an osteoid osteoma should be made, especially in the setting of undefined bone marrow edema pattern in a young patient. Osteoid osteomas can occur in a variety of locations throughout the axial and appendicular skeleton including the talus as described here [8].
Newer treatment options for osteoid osteoma include various imaging guided interventions, such as percutaneous laser photocoagulation, ethanol injection, and, more commonly, percutaneous radiofrequency (RF) ablation [9–12]. For radiofrequency ablation, fluoroscopic, or, more commonly, CT guidance, is used to guide an RF probe into the central nidus of the osteoid osteoma, which is then heated to approximately 90°C [11]. This procedure can be applied to osteoid osteomas throughout the musculoskeletal system, including the extremities as well as the axial skeleton [13, 14]. The procedure, on the whole, has demonstrated a high success rate, with some authors finding that larger lesions and lesions in a nondiaphyseal location in the long bones may have a higher recurrence rate [15, 16].
Advantages of using imaging guidance include the definitive localization of the needle within the nidus and direct visualization of the regional neurovascular structures; specifically, the posterior tibial nerve and artery in the case presented here. Minimal anesthesia (conscious sedation) is needed in contrast to operative treatment.
In summary, a high clinical index of suspicion for osteoid osteomas should be maintained for young patients presenting with nonspecific pain, often suggestive of a stress fracture, especially in the absence of undefinable antecedent trauma. In questionable cases, advanced imaging studies such as MR or CT should be pursued, with meticulous attention to thin-cut, high-resolution imaging. Imaging guidance can also be used for percutaneous treatment of these lesions, with a high clinical success rate [10].
References
- 1.Allen SD, Saifuddin A. Imaging of intraarticular osteoid osteoma. Clin Radiol. 2003;58(11):845–852. doi: 10.1016/S0009-9260(03)00213-7. [DOI] [PubMed] [Google Scholar]
- 2.Holsalkar HS, Garg S, Moroz L, Pollack A, Dormans JP. The diagnostic accuracy of MRI versus CT imaging for osteoid osteoma in children. Clin Orthop Relat Res. 2005;433:171–177. doi: 10.1097/01.blo.0000151426.55933.be. [DOI] [PubMed] [Google Scholar]
- 3.Davies M, Cassar-Pullicino VN, Davies AM, McCall IW, Tyrrell PN. The diagnostic accuracy of MR imaging in osteoid osteoma. Skelet Radiol. 2002;31(10):559–569. doi: 10.1007/s00256-002-0546-4. [DOI] [PubMed] [Google Scholar]
- 4.Goldman AB, Schneider R, Pavlov H. Osteoid osteoma of the femoral neck: report of four cases evaluated with isotopic bone scanning, CT and MR imaging. Radiology. 1993;186(1):227–232. doi: 10.1148/radiology.186.1.8416569. [DOI] [PubMed] [Google Scholar]
- 5.Francesco B, Andrea LA, Vincenzo S. Intra-articular osteoid osteoma of the lower extremity: diagnostic problems. Foot Ankle Int. 2002;23(3):264–267. doi: 10.1177/107110070202300314. [DOI] [PubMed] [Google Scholar]
- 6.Hogues P, Marti-Bonmati L, Aparisi F, Saborido MC, Garci J, Dosda R. MR imaging assessment of juxtacortical edema in osteoid osteoma in 28 patients. Eur Radiol. 1998;8(2):236–238. doi: 10.1007/s003300050370. [DOI] [PubMed] [Google Scholar]
- 7.Ehara S, Rosenthal DI, Aoki J, Fukuda K, Sugimoto H, Mizutani H, Okada K, Hatori M, Abe M. Peritumoral edema in osteoid osteoma on magnetic resonance imaging. Skelet Radiol. 1999;28(5):265–270. doi: 10.1007/s002560050513. [DOI] [PubMed] [Google Scholar]
- 8.Yeager BA, Schiebler ML, Wertheim SB, Schmidt RG, Torg JS, Perosio PM, Dalinka MK. MR imaging of osteoid osteoma of the talus. J Comput Assist Tomogr. 1987;11(5):916–917. doi: 10.1097/00004728-198709000-00038. [DOI] [PubMed] [Google Scholar]
- 9.Gangi A, Dietemann JL, Gasser B, Mortazavi R, Dosch JC, Dupuis M, Durckel J, Roy C. Percutaneous laser photocoagulation of osteoid osteomas. Semin Musculoskelet Radiol. 1997;1(2):273–280. doi: 10.1055/s-2008-1080148. [DOI] [PubMed] [Google Scholar]
- 10.Adam G, Neuerburg J, Vorwek D, Forst J, Gunther RW. Percutaneous treatment of osteoid osteomas: combination of drill biopsy and subsequent ethanol injection. Semin Musculoskelet Radiol. 1997;1(2):281–284. doi: 10.1055/s-2008-1080149. [DOI] [PubMed] [Google Scholar]
- 11.Woertler K, Vestring T, Boettner F, Winkelmann W, Heindel W, Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol. 2001;12(6):717–722. doi: 10.1016/s1051-0443(07)61443-2. [DOI] [PubMed] [Google Scholar]
- 12.Venbrux AC, Montague BJ, Murphy KP, Bobonis LA, Washington SB, Soltes AP, Frassica FJ. J Vasc Interv Radiol. 2003;14(3):375–380. doi: 10.1097/01.rvi.0000058420.01661.8c. [DOI] [PubMed] [Google Scholar]
- 13.Ramos L, Santos JA, Santos G, Guiral J. Radiofrequency ablation in osteoid osteoma of the finger. J Hand Surg (Am) 2005;30(4):798–802. doi: 10.1016/j.jhsa.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Marquardt B, Gebert C, Gosheger G, Steinbeck J, Lindner NJ. Percutaneous radiofrequency ablation of an osteoid osteoma of the scapula: a case report. J Shoulder Elb Surg. 2005;14(4):447–449. doi: 10.1016/j.jse.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Vanderschueren GM, Taminiau AH, Obermann WR, Berg-Huysmans AA, Bloem JL. Osteoid osteoma: factors for increased risk of unsuccessful thermal coagulation. Radiology. 2004;233(3):757–762. doi: 10.1148/radiol.2333031603. [DOI] [PubMed] [Google Scholar]
- 16.Cribb GL, Goude WH, Cool P, Tins B, Cassar-Pullicino VN,Mangham DC (2005) Percutaneous radiofrequency thermocoagulation of osteoid osteomas: factors affecting therapeuticoutcome. Skelet Radiol 9 (epub ahead of print) [DOI] [PubMed]