Introduction
The posterior approach is the most common approach used in the United States. Its main advantages include (1) less extensive tissue dissection, (2) better visualization of the acetabulum, (3) lower incidence of heterotopic bone formation, and (4) preservation of the abductor mechanism. Historically, the posterior approach in primary total hip arthroplasty (THA) was associated with an increased risk of postoperative dislocation compared to the anterolateral or the transtrochanteric approach [1–3]. The senior author (P.M.P.) has described a posterior soft tissue repair reattaching the short external rotators and the posterior capsule to the greater trochanter. This repair has subsequently resulted in a significant reduction of the risk of postoperative dislocation [4]. The current review describes the surgical technique used by the senior author and discusses alternative techniques, biomechanical foundations, and the clinical outcome of patients undergoing primary THA thorough a posterior approach with soft tissue repair.
Surgical technique
The patient is positioned in the lateral decubitus position for a standard posterior approach. Through a straight posterior incision, the fascia lata and the gluteus maximus muscle are identified. It is the philosophy of the senior author (P.M.P.) to use an adequate incision length because a meticulous repair will require good exposure. Currently the average incision length is about 6 in.
The fascia lata is incised and the gluteus maximus is finger-split along its fibers. A Charnley retractor is inserted to improve visualization of the posterior capsule and short external rotators. Using electrocautery, the posterior fat tissue and remnants of the bursa are divided, thereby preserving a layer of tissue that later can be closed over the short external rotators. Proximally, the posterior boarder of the gluteus medius, and, distally, the proximal boarder of the quadratus femoris muscle are identified. The piriformis tendon is palpated and a thin, bent Hohmann retractor is inserted over the tendon between the gluteus medius and minimus to expose the short external rotators (Fig. 1). Distally, an Aufranc retractor is inserted between the quadratus femoris muscle and the distal part of the posterior capsule. Successively the hip is positioned in internal rotation to improve the access to the insertion of the piriformis and conjoined tendon. Considering that both tendons are inserted in the piriformis fossa further anterior than is generally expected, it is important to release the tendon as close to its anatomic position as possible. This will preserve maximum tendon length for a later tension-free repair. At its anatomic insertion the piriformis and conjoined tendon (common insertion of inferior gemellus, superior gemellus, and obturator internus muscle) will merge to form a single wide tendon belly. As long as two separate tendons are released, it is likely that the tendon was cut far away from its insertion site in the piriformis fossa. As soon as the tendon is released, two no. 2 Ethibond sutures are looped through the short external rotator tendons twice, and the tendons are pulled posterior to expose the posterior capsule (Fig. 2). Then, the posterior boarder of the gluteus minimus muscle is identified and a periosteal elevator is slit between the muscle and the posterior capsule. As soon as the gluteus minimus is elevated off the posterior capsule, the thin bent Hohmann retractor is repositioned underneath it, and the posterior capsule is incised. Using an electrocautery, the capsule incision is started at the 1o'clock position and descends anteriorly toward the greater troachanter. It is important to start the incision proximally because this part of the posterior capsule is thicker and will provide better anchorage for the repair sutures. Instead of turning the incision downwards along the intertrochanteric line, we recommend to continue releasing the capsule in line with the femoral neck underneath the greater trochanter to preserve as much capsule as possible. If the capsule is cut along the posterior boarder of the greater troachanter instead, the internal rotation contracture will leave the surgeon unable to preserve enough capsule tissue for a tension-free posterior repair. The capsule is subsequently released all the way around the femoral neck, and the incision is carried into the quadratus femoris to expose the lesser Trochanter (Fig. 3). We do not recommend tagging the posterior capsule at this point, because perfect placement of the tagging sutures should be guided by the position of the drill holes once the hip joint is replaced. After THA is finished, the posterior capsule and short external rotators are repaired. For posterior repair, two drill holes are placed into the posterolateral edge of the greater trochanter by using a 2.3-mm drill bit. The proximal drill hole should be oriented toward the piriformis fossa (Fig. 4), and the distal drill hole will exit about half an inch further distal. Next, the posterior capsule is approximated to the drill holes and the perfect location for the proximal and distal tagging sutures is chosen to minimize tension on the capsule (Fig. 5). Placing the sutures after insertion of the stem allows addressing changes in leg length. If the stem restores natural offset, repair of the capsule should be possible without excessive tension on the sutures. The posterior capsule is tagged using two no. 2 Ethibond sutures. Then, the proximal and distal suture from the short external rotators and the posterior capsule are pulled through the proximal and distal drill hole, respectively. Because we cut the threads for the short external rotators short and leave the ones for the capsule longer, we are able to identify the threads for the capsule and external rotators and tighten each of them separately. It is important to position the hip in slight abduction and neutral rotation before tightening the knots. As soon as the knots are tightened, internal rotation up to 30° should be possible without tension on the repair. The idea of the repair is not to provide stability within the normal range of motion; rather, it should rather resistance against dislocation in excessive internal rotation. All patients will have limits in their activities within the first 6 weeks to guarantee that the repair will heal before it is stressed. After irrigation, the quadratus femoris is repaired. It is essential to elevate the muscle before the sutures are passed through it to prevent injury to the sciatic nerve (Fig. 6). The muscle is repaired with two Vicryl figures of eight loops toward the Vastus lateralis muscle. Finally, the overlying bursa and fat tissue is closed over the repair with no. 0 Vicryl (Fig. 7).
Fig. 1.
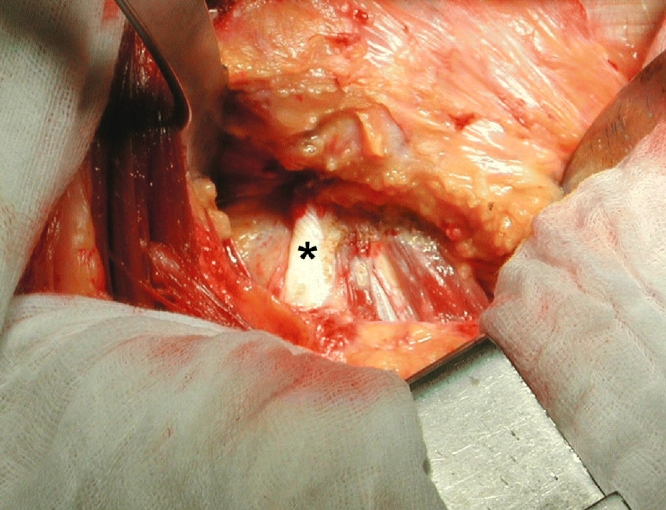
After exposure of the short external rotators (*piriformis tendon)
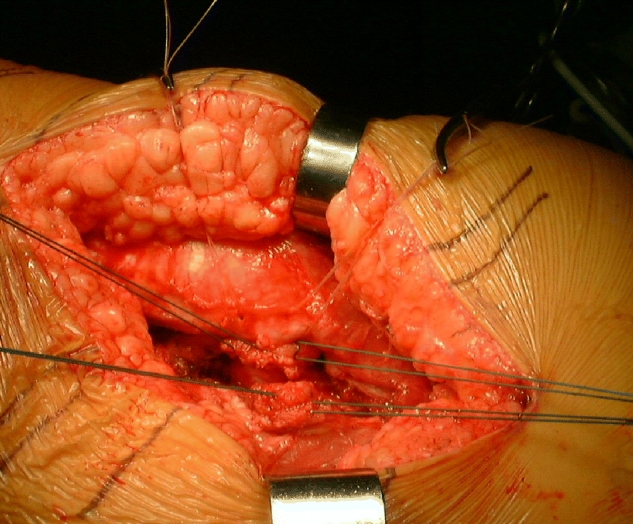
Fig. 2.
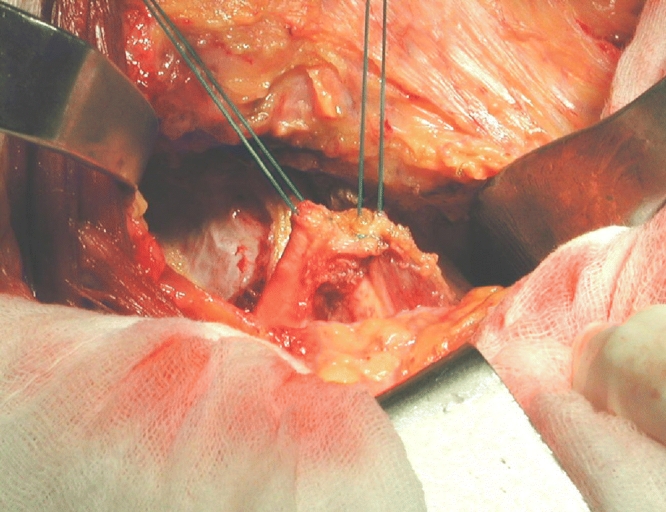
Ethibond tagging sutures are placed in the short external rotators
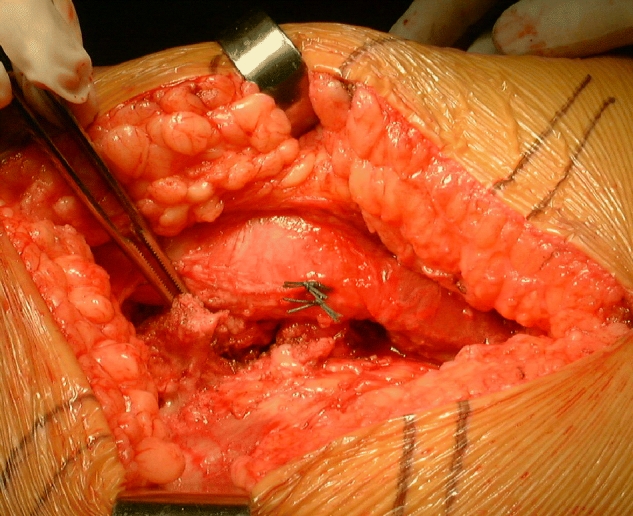
Fig. 3.
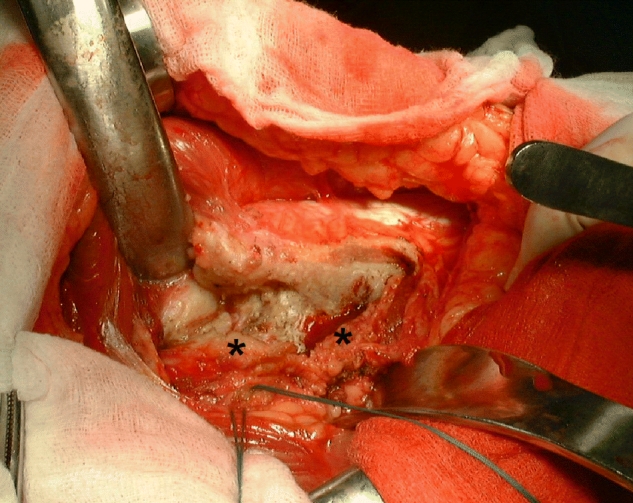
The capsule (*) is released closed to its insertion at the femoral neck
Fig. 4.
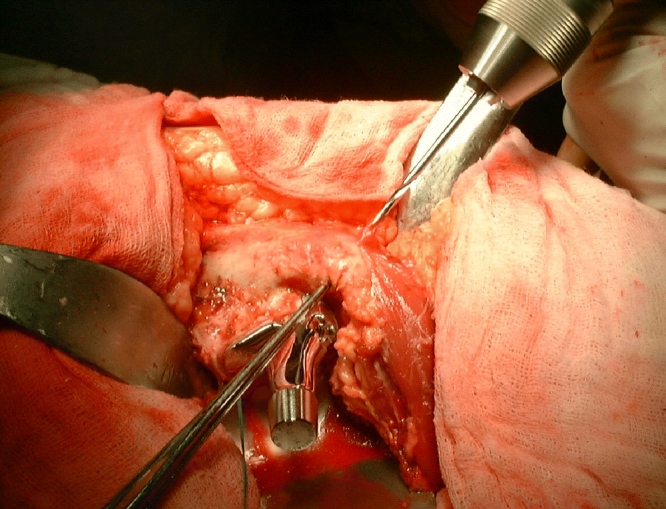
The proximal drill hole is oriented towards the piriformis fossa
Fig. 5.
Tagging sutures in the short external rotators and in the posterior capsule in line with the pull through sutures in the greater Trochanter drill holes
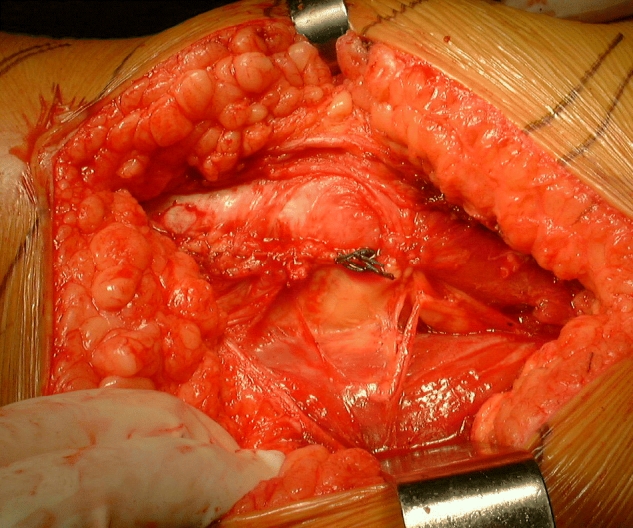
Fig. 6.
After repair of the short external rotators. The quadratus femoris muscle is elevated and reattached to the Vastus lateralis
Fig. 7.
After repair of the posterior capsule, external rotators, quadratus femoris, and the overlying soft tissues
A number of different posterior repair techniques have been described in the literature. Some authors have advocated releasing the capsule and the overlying external rotators as a single layer [5]. The rational behind this technique is that a thicker tissue sleeve will improve the quality of the repair. However, in the authors' experience this technique makes it more difficult to preserve a maximum length for both the capsule and the external rotators. Moreover, in a current MRI study, several patients showed failure in the repair of short external rotators but integrity of the capsular attachment underlying the importance of repairing both layers separately.
Drill holes in the greater trochanter to anchor the repair have been associated with a 0.9% incidence of greater trochanter fracture [6]. This risk can be minimized by using a 2.3-mm or a 2.0-mm drill bit instead of a 2.7-mm drill [5]. The senior author has performed more than 5,000 THA and has not encountered this complication.
Some authors have recommended the use of no. 2 Fiberwire (Arthrex®, Naples, FL, USA) for posterior repair [5]. However, it is questionable whether a stronger suture material really is necessary because the repair tends to fail by suture pullout rather than breakage of the suture material [7]. Instead, it might be advisable to use Krackow stitches to strengthen the fixation of the short external rotators [8, 9].
Results of the posterior repair
At the Hospital for Special Surgery, Robinson et al. [2] presented the first clinical evidence suggesting that reattaching the short external rotators to the greater trochanter reduces the incidence of postoperative dislocation from 7.5% to 1% in patients who had a posterior approach. Weiss and Jacobs [10] later advocated repair of both the short external rotators and the posterior capsule. In the same year, Hedley and coworkers [11] reported the first large series of patients with a posterior approach and repair of the short external rotators and the posterior capsule. Hedley et al. used six to eight no. 1 Vicryl sutures and reattached these through towel clip holes in the lateral boarder of the greater trochanter. Out of 259 patients operated on between 1986 and 1989, only two patients experienced a postoperative dislocation, both secondary to a traumatic event.
Kao and Woolson [12] reported less encouraging results after excising the anterior and posterior capsule and only repairing the piriformis tendon. In a small series of 10 patients, they used metal clips in the piriformis tendon and the greater trochanter to evaluate the integrity of the repair. Eight out of 10 patients had failure of the piriformis tendon repair and one of the remaining two patients had a postoperative dislocation. As a result, the authors abandoned the posterior repair. Considering that two out of 10 patients experienced an early dislocation the study clearly underlines the detrimental effect of excising and not repairing the posterior capsule.
In 1998 the senior author presented his data on a meticulous repair of not only the capsule and the external rotators, but also the quadratus femoris muscle belly and the overlying fat and bursa tissue [4]. Instead of towel clips, Pellicci and Poss used drill holes in the greater trochanter to anchor the repair. In addition, they used nonabsorbable no. 2 Ethibont sutures for a more durable repair. With the introduction of the posterior repair, both Pellicci and Poss recognized a significant drop in the incidence of postoperative dislocations from 4.0% to 0% and 6.2% to 0.8% [4].
Ko and coworkers [9] reported on the impact of the posterior repair in patients undergoing hemiarthroplasty for hip fractures. The authors used a T-shaped capsule incision and performed a side-to-side closure of the vertical limb with no. 1 Vicryl and reattachment of the transverse limb using no. 5 Ethibond. To augment the suture fixation to the short external rotators, they used Krackow stitches. This technique led to a drop in the incidence of postoperative dislocation from 1.9% between 1986 and 1997 to 0% between 1998 and 1999.
Using a similar technique as the one described by the senior author (P.M.P.), Suh and coworkers [13] reported a decrease in postoperative dislocation from 6.4% without repair to 1% after repairing the capsule and the short external rotators. Other authors have reported similar results using a posterior capsular repair only [6, 14].
In a cadaver study, Mihalko and Whiteside [7] were able to show that posterior repair reduces internal rotation and increases the torque forces needed to dislocate the hip joint after primary THA. If hips after a repair of the posterior capsule and piriformis tendon were dislocated, the repair never failed completely. Four out of six cadavers showed suture pulled out of the inferior capsule sutures with dislocation in 90° flexion. The authors also recognized a more normal load deflection curve in patients with a posterior soft tissue repair compared to those without a repair. According to this study, repair of the capsule and the external rotators is recommend and is superior to no repair or repair of the piriformis tendon only.
The clinical and biomechanical data are in contrast to in vivo studies evaluating the integrity of the posterior repair [12, 15]. Although the poor results reported by Kao and Woolson in 10 patients are explained by the fact that the authors excised the posterior capsule and only repaired the piriformis tendon, the high failure rate presented by Stählin and coworkers is more difficult to explain. Stählin et al. used a wire stitched to the piriformis and conjoined tendon and marked the greater trochanter attachment using a tantalum marker. A distance of 25 mm between both markers or double the distance measured intraoperatively was considered a failure of the repair. In three out of 20 hips, the short external rotator repair failed within the first day after surgery and in 12 it failed within 3 months, accounting for an overall failure rate of 75%. There are three explanations for these poor results. First, the authors noted that they were not able to release the piriformis tendon at its bony insertion in the piriformis fossa and had to leave a short tendon cuff at its insertion. This could have increased the overall tension of the repair and led to early failure. Second, closing the posterior capsule and external rotators in one layer has the disadvantage that failure of the external rotator repair will automatically result in failure of the capsular attachment. We therefore recommend tying the capsule and external rotator using two separate Ethibond sutures. The last possible explanation is that although the repair ultimately fails, it provides a scaffold for tissue that fills the posterior death space and prevents dislocation and therefore explains the overall good clinical results after posterior soft tissue repair.
To better visualize the integrity of posterior repair, the authors enrolled 35 patients into a prospective MRI study. Under this study, patients will have evaluation of the repair within 4 days after surgery and at 3 months follow-up. This study will provide information on the integrity of the repair and will also visualize changes in the posterior soft tissues within the early postoperative period.
Discussion
Although the posterior approach has been associated with an increased incidence in postoperative dislocation and sciatic nerve injury, its alternative—a direct lateral or anterolateral approach—results in an up to 10% incidence of abductor weakness as well as an increased incidence of heterotopic bone formation and obturator and femoral nerve injuries [3, 16, 17]. Although surgeons have used these statements to defend their preferred surgical approach, a more recent metanalysis and the Cochrane database find not sufficient data in the literature to support either one of the above statements [18, 19]. Clinical follow-up studies have shown a significant decrease in the incidence of dislocation if a posterior soft tissues repair is utilized [4]. Although some studies reported early disruption of the repair in radiographic follow-up studies, the overwhelming number of clinical outcome studies seems to support the posterior capsule and the short external rotator repair. Studies reporting high failure rates underline the importance of minimizing tension on the repair by releasing the capsule and the external rotators as close to their bony insertion as possible and correct placement of the anchoring drill holes in the greater trochanter. Repairing both structures too tight limits the normal range of motion and will ultimately result in failure of the repair before tendon-bone healing occurred. It is also recommended to repair both the external rotators and the capsule [7] and reattach both using separate sutures [4]. The authors are currently performing a 3-month MRI follow-up study to investigate the integrity of the repair.
References
- 1.McCollum DE, Gray WJ. Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop. 1990;261:159–170. [PubMed] [Google Scholar]
- 2.Robinson RP, Robinson HJ, Salvati EA. Comparison of the transtrochanteric and posterior approaches for total hip replacement. Clin Orthop. 1980;147:143–147. [PubMed] [Google Scholar]
- 3.Vicar AJ, Coleman CR. A comparison of the anterolateral, transtrochanteric, and posterior surgical approaches in primary total hip arthroplasty. Clin Orthop. 1984;188:152–159. [PubMed] [Google Scholar]
- 4.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop. 1998;355:224–228. doi: 10.1097/00003086-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 5.Osmani O, Malkani A. Posterior capsular repair following total hip arthroplasty: a modified technique. Orthopedics. 2004;27:553–555. doi: 10.3928/0147-7447-20040601-10. [DOI] [PubMed] [Google Scholar]
- 6.White RE, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop. 2001;393:163–167. doi: 10.1097/00003086-200112000-00019. [DOI] [PubMed] [Google Scholar]
- 7.Mihalko WM, Whiteside LA. Hip mechanics after posterior structure repair in total hip arthroplasty. Clin Orthop. 2004;420:194–198. doi: 10.1097/00003086-200403000-00027. [DOI] [PubMed] [Google Scholar]
- 8.Krackow KA, Thomas SC, Jones LC. Ligament tendon fixation: analysis of a new stitch and comparison with standard techniques. Orthopedics. 1988;11:909–917. doi: 10.3928/0147-7447-19880601-11. [DOI] [PubMed] [Google Scholar]
- 9.Ko CK, Law SW, Chiu KH. Enhanced soft tissue repair using locking loop stitch after posterior approach for hip hemiarthroplasty. J Arthroplast. 2001;16:207–211. doi: 10.1054/arth.2001.20539. [DOI] [PubMed] [Google Scholar]
- 10.Weiss APC, Jacobs MA. Posterior augmentation during closure following total hip arthroplasty. Orthopedics. 1990;13:577–579. doi: 10.3928/0147-7447-19900501-17. [DOI] [PubMed] [Google Scholar]
- 11.Hedley AK, Hendren DH, Mead LP. A posterior approach to the hip joint with complete posterior capsular and muscular repair. J Arthroplast. 1990;5(Suppl):S57–S66. doi: 10.1016/s0883-5403(08)80027-7. [DOI] [PubMed] [Google Scholar]
- 12.Kao JT, Woolson ST. Priformis tendon repair after total hip replacement. Orthop Rev. 1992;21(2):171–174. [PubMed] [Google Scholar]
- 13.Suh KT, Park BG, Choi YJ. A posterior approach to primary total hip arthroplasty with soft tissue repair. Clin Orthop. 2004;418:162–167. doi: 10.1097/00003086-200401000-00026. [DOI] [PubMed] [Google Scholar]
- 14.Dixon MC, Scott RD, Schai PA, Stamons V. A simple capsulorraphy in a posterior approach for total hip arthroplasty. J Arthroplast. 2004;19:373–376. doi: 10.1016/j.arth.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Stählin T, Drittenbass L, Hersche O, Miehlke W, Munzinger U. Failure of capsular enhanced short external rotator repair after total hip replacement. Clin Orthop. 2004;420:199–204. doi: 10.1097/00003086-200403000-00028. [DOI] [PubMed] [Google Scholar]
- 16.Bischoff R, Dunlap J, Carpenter L, DeMouy E, Barrack R. Heterotopic ossification following uncemented total hip arthroplasty. Effect of the operative approach. J Arthroplast. 1994;9(6):641–644. doi: 10.1016/0883-5403(94)90118-X. [DOI] [PubMed] [Google Scholar]
- 17.Weale AE, Newman P, Ferguson IT, Bannister GC. Nerve injury after posterior and direct lateral approaches for hip replacement. J Bone Jt Surg. 1996;78:899–902. doi: 10.1302/0301-620x78b6.6603. [DOI] [PubMed] [Google Scholar]
- 18.Jolles BM, Bogoch ER. Surgical approach for total hip arthroplasty. Direct lateral or posterior? J Rheumatol. 2004;31:1790–1796. [PubMed] [Google Scholar]
- 19.Jolles BM, Bogoch ER. Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst Rev. 2004;1:CD 003828. doi: 10.1002/14651858.CD003828.pub2. [DOI] [PubMed] [Google Scholar]


