Abstract
Operative management of displaced acetabular fractures yields better results than nonoperative management. Over the past decade, surgical approaches to the acetabulum and the surgical tactic for repair of common fracture patterns have been advanced. Excellent outcomes after repair of these injuries can be achieved. In some cases, as in the elderly, or in those cases in which there is significant destruction of the articular cartilage, primary total hip arthroplasty may provide the best solution. Removal of the femoral head allows for excellent exposure of the acetabulum, making it possible to stabilize most fractures without the need for extensile or intrapelvic approaches. The surgical technique that has been successfully used calls for gaining primary stability of the acetabular columns by open reduction and internal fixation and then using the acetabular component to replace the articular surface. The columns need not be anatomically reduced. Multiholed acetabular shells can be used as internal fixation devices by placing screws into the columns enhancing the stability of the repair. In older individuals with severe osteoporosis, a typical fracture pattern results in intrapelvic dislocation of the femoral head with a blowout fracture of the anterior column and medial wall. Reinforcement rings with cemented acetabular fixation can be used in these cases. The femoral head can be used as bulk bone graft to replace and reinforce the reconstruction. Techniques common to revision of failed acetabular components are helpful in this setting. The results of reconstruction of severe acetabular fractures with total hip replacement have been reported to be similar to those achieved for reconstruction of osteoarthritis.
Introduction
The average age of the population is growing, with the older than 65 years age group representing the fastest growing segment of the population. Because the elderly generation is maintaining an active lifestyle, the incidence of trauma leading to acetabular fractures in this segment of the population is becoming more common. Elderly patients with acetabular fractures may soon be the most typical age group to present with this fracture. Epidemiologic studies suggest that 4,000 acetabular fractures in elderly patients occur each year in the United States [1].
In the elderly, most acetabular fractures are pathologic fractures occurring through osteopenic bone and resulting from simple low-energy falls. Fractures resulting from traffic accidents, either in moving vehicles or pedestrians struck, also occur and are often severely comminuted with combined injuries to the acetabulum and femoral head. Because many of these patients have preexisting osteoporosis, the resulting fractures are often complex fracture patterns with extensive comminution and displacement. Older patients not affected by osteoporosis can present with the classic injury types described by Judet et al [2], but the osteoporotic patient usually presents with atypical fracture patterns. A fracture pattern seen commonly in geriatric patients results from falls directly onto the greater trochanter. This mechanism results in a comminuted fracture of the anterior column and medial wall in which the femoral head dislocates centrally into the pelvis [1] (Fig. 2a). In more severe cases, both column fracture patterns may occur, completely dissociating the acetabulum from the superior ilium.
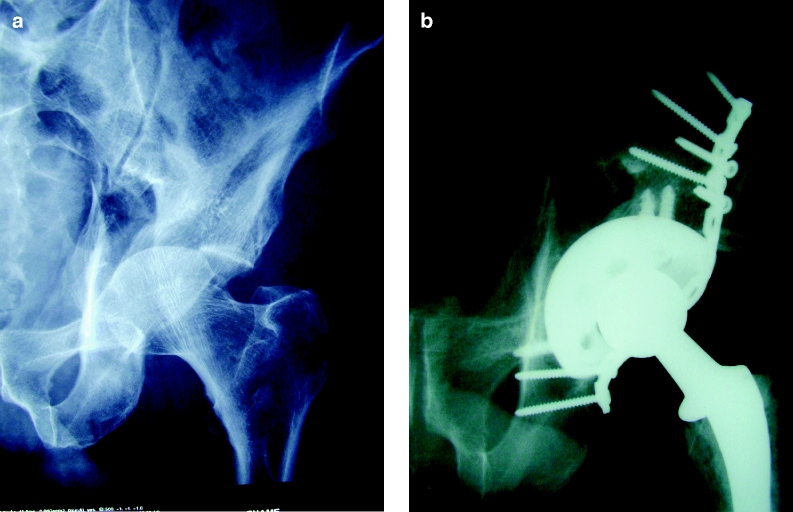
Fig. 2.
a A radiograph of the pelvis of a 75-year-old man who suffered a both-column acetabular fracture after falling from a tree. b A radiograph of the pelvis after ORIF of the columns with implantation of a multiholed acetabular component and femoral head graft
In this elderly population, nonoperative treatment of acetabular fractures very often leads to poor outcome. Minimally displaced fractures may be managed conservatively, but late displacement from unrecognized comminution is a risk. Because most acetabular fracture displacements have elements of rotation and not just translation, traction is usually ineffective in achieving acceptable reductions. Nonoperative care often commits the patient to 6 to 8 weeks of bed rest and non–weight bearing, which is associated with the common complications usually associated with fractures of the upper femur. Spencer [3] reviewed the results of conservative care in 25 elderly patients with acetabular fractures and found that 30% had completely unacceptable outcomes. In his experience, traction and recumbency need to be applied for longer than 6 weeks, requiring especially skillful nursing care that may not be available in this modern day [3].
Unfortunately, in the elderly population surgical repair yields only marginally better results [1]. The problems of gaining secure fixation in the osteoporotic bone of the pelvis in this patient population can be extremely unpredictable [4, 5]. Matta [5] was able to achieve anatomic reduction in only 44% of patients older than 60 years. Helfet et al [6] reported on a series of 18 patients with an average age of 67 years. The description of their operative experience clearly suggests that open reduction represents a more technically demanding approach than total hip replacement. Although the reported results suggest good to excellent outcomes at 3 years, several of the patients had significant risk factors, suggesting the potential need for future total hip replacement [6].
Several authors, most notably Mears and Velyvis [7], have recommended total hip arthroplasty for the geriatric acetabular fracture particularly if associated with comminution, impaction, or abrasive cartilage loss. Good to excellent results were achieved in more than 80% of their series, with maintenance of that result for 10 years follow-up. Anglen and his coauthors [4] pointed out the value of the “Gull Sign,” a radiographic finding that indicates impaction of the superomedial dome, in identifying acetabular fractures with a poor prognosis for acceptable hip function after open reduction and internal fixation (ORIF). Unfortunately, the aggregate experience with these injuries is sparse. As a result, this subject suffers from a lack of comparative studies and guidelines on which to base treatment recommendations.
In general, elderly patients are benefited from treatments that allow rapid mobilization from bed. Prolonged recumbency can lead to pulmonary compromise as well as generalized deconditioning, which requires prolonged dependency and often results in loss of ambulatory function. One option for the surgeon faced with a severe acetabular fracture in an elderly patient is to place the limb in traction to stabilize the fracture till healed then proceed with total hip replacement. This approach, however, requires prolonged bed rest and, as reported by Mears [1, 7], often results in an inferior outcome of the total hip replacement secondary to deformity and nonunion within the acetabulum.
Alternatively, repair of the acetabular fracture can be attempted, allowing the fracture to heal with total hip replacement performed in staged fashion, if needed. Proponents of this approach argue that stability and secure fixation of the acetabular component is more likely than when attempting total hip replacement in the unstable, fractured acetabulum. Recently, techniques for achieving stability of the fractured acetabulum sufficient to secure the acetabular component for immediate total hip replacement have been refined and tested. Immediate total hip replacement provides for immediate mobilization of the patient and avoids the risks associated with multiple surgical procedures. Therefore, in formulating an approach to the geriatric acetabular fracture, ORIF of simple fracture patterns is appropriate, but we feel strongly that comminuted, displaced, and impacted fractures are best treated by ORIF of the acetabular columns combined with immediate total hip replacement for joint restoration. This study presents an argument for a specific approach that has been used for this challenging injury.
Preoperative planning
Elderly patients with acetabular fractures should be approached as one approaches elderly patients with hip fracture. These patients should be placed in skeletal traction in the emergency department to immobilize the affected limb and relieve pain as the patient is prepared for surgery. The patient should be prepared for surgery with as little delay as possible. Medical clearance is advised to stabilize any acute medical problems, but prolonged workup of chronic medical conditions should be avoided. Venous thromboembolism, as with any hip fracture, is a risk, and prophylaxis is recommended. Low molecular weight heparin administered in prophylactic doses can be administered in the preoperative period. In the postoperative period, a prophylactic regimen similar to that for total hip replacement should be given until the patient is ambulating independently. Perioperative prophylactic antibiotics are mandatory. Regional anesthesia has particular advantages for this surgery by reducing intraoperative blood loss, reducing the risk of thromboembolism and helping to manage postoperative pain.
The challenge of performing total hip replacement in the setting of the acute acetabular fracture lies in achieving stable fixation of the acetabular component. Restoration of stability of the acetabular columns is required for stable acetabular fixation. The surgical techniques required for this were gleaned from revision surgery illustrated, for example, by the principles outlined by Gross et al [8] for revision of acetabular components in the setting of bone loss. In other words, open reduction of the acetabular columns provides the basic stability needed to fix the acetabular component, but absolute anatomic reduction is not required because of the planned arthroplasty. Bone grafts fabricated from the excised femoral head may be needed to fill defects in the medial wall or acetabular walls to ensure adequate acetabular cup fixation. In many cases, a surgical team with members familiar with both acetabular fracture repair and total hip replacement may be optimal.
Preoperative planning for these procedures demands a complete radiographic analysis of the fracture including computed tomographic (CT) scan. Accurate diagnosis of the fracture is needed to plan the operative approach for columnar restoration and to anticipate the need for special revision components. The radiographic examination should include the anteroposterior and oblique views of the pelvis, commonly known as the “Judet views” [9]. These 45-degree oblique views allow accurate description of the injury to the anterior and posterior columns as well as the medial wall. The CT scan improves the perception of the comminution of the articular surface and helps in the assessment of the degree of structural compromise of the acetabular walls. The CT scan will also accurately reveal the presence of a fracture of the femoral head. These studies help the surgeon prepare for the procedure. If significant disruption of either the anterior or posterior column is depicted, open reduction and stabilization of the columns will need to be performed. If the columns are intact but the medial wall is disrupted, the surgeon must be prepared to bone graft the defect or use a reinforcement ring to replace the medial wall. The radiographic assessment also dictates the direction of the surgical approach as described below.
The surgeon should have experience with revision acetabular surgery because the problems in achieving stability in the acute fracture are similar to those encountered in revising failed acetabular components [8]. Acetabular components with multiple holes for screw fixation and reinforcement rings such as the Burch-Schneider cage should be available.
The surgical exposure
The posterior approach to the hip joint commonly referred to as the Kocher-Langenbeck approach is usually adequate for exposure of the fracture. Excision of the femoral head provides for a very direct exposure of both the anterior and posterior walls as well as the posterior column and superior acetabular area (Fig. 1). Direct exposure of high anterior column components of the fracture would require an intrapelvic approach, but for the purposes of gaining stability and not perfect reduction, the posterior approach allows for indirect reduction and fixation of the anterior column with screws directed from back to front. As an alternative for the anterior column fracture with intact posterior column, Beaule et al [10] reported the use of a modified anterior approach with exposure of the high anterior column with simultaneous exposure of the acetabulum for insertion of total hip components via an anterior approach. This exposure uses the Smith-Peterson incision. The interior aspect of the iliac wing is exposed using the proximal limb of the incision allowing fixation of the anterior column, and the lower portion of the incision is used for direct exposure of the hip joint for performance of the total hip replacement.
Fig. 1.
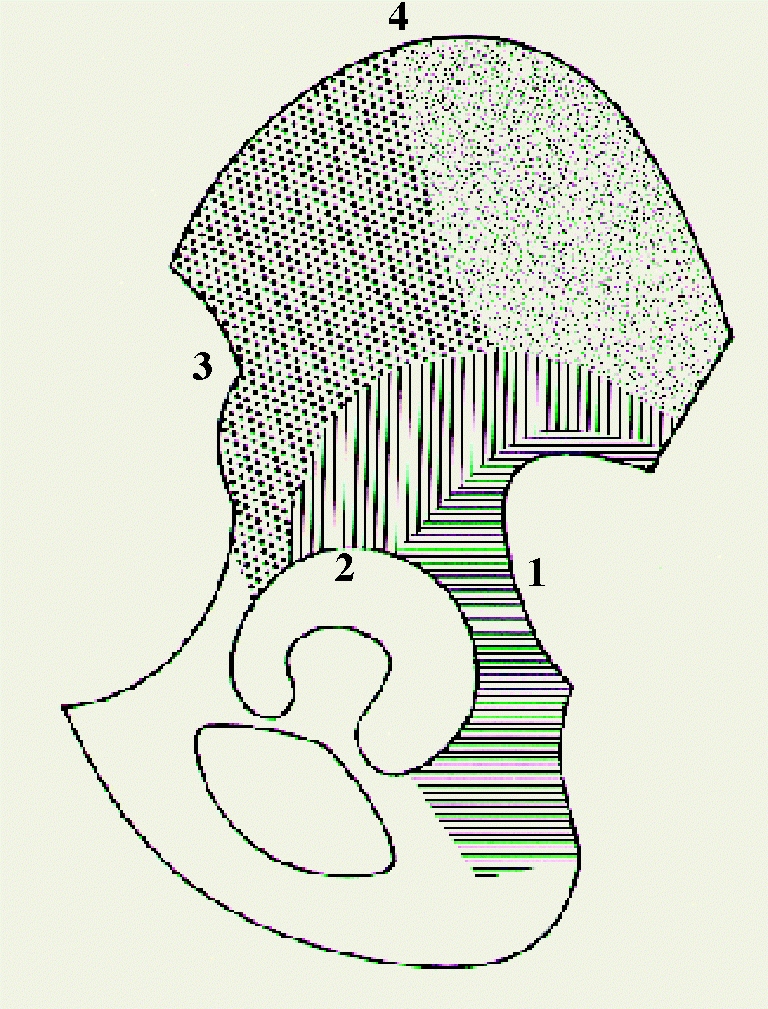
Acetabular exposure from the posterior approach after excision of the femoral head. The shaded area indicates the region accessible by this approach
Achieving stability of the acetabular columns
Column stability is achieved by using standard techniques of direct and indirect reduction with fixation using plates and screws. The posterior column is stabilized with typical posterior plates that also secure the posterior wall. Posterior to anterior lag screws can stabilize the anterior column. These screws are inserted after reduction and fixation of the posterior column. The insertion site for the posterior to anterior screw is above the acetabulum. The drill is directed anteriorly and inferiorly so that the screw traverses the fracture and runs down the anterior column to gain purchase in the superior pubic ramus. The use of cerclage cables, which encircle the columns by passing through the sciatic notch and up along the medial wall, was also described [11, 12]. This technique is advocated when bone quality is poor. It is particularly suited when combined with acute total hip replacement because it results in excellent primary stability of the columns, allowing for stable uncemented cup fixation. Mouhsine et al described a detailed technique for this surgery as well as their clinical results [13].
Once the columns are stabilized, the excised femoral head can be fashioned as a structural graft to bridge contained defects. Acetabular components with multiholed shells can then be used as internal fixation devices because they allow screws to be directed in multiple planes, thus gaining adequate fixation of both the cup and fracture.
The strategy is illustrated in the case presented in Fig. 2a. This 75-year-old man presented with this typical both-column fracture, evidenced by the spur sign, after falling from a tree. The fracture was exposed through a posterior approach. After removal of the femoral head, the anterior and posterior columns were reduced into a stable position and fixed with a posterior column plate and posterior to anteriorly directed lag screws. The femoral head was used as a structural graft to fill a contained superior and quadrilateral surface defect. A multiholed acetabular shell was then implanted and fixed with several screws aimed to reinforce the fracture fixation as well as to fix the cup (Fig. 2b). Excellent stability was achieved and the patient recovered excellent hip function with stable results as of 2-year follow-up.
If adequate column stability cannot be restored or in very elderly osteoporotic patients, use of reinforcement rings with cemented cup fixation is advised. A fracture pattern commonly seen in the older osteoporotic patient consists of a central fracture dislocation with associated anterior wall or column fracture (Fig. 3a). It is technically difficult to achieve stable anterior column and wall stability in this fracture except with an intrapelvic exposure. An alternate tactic is to extract the dislocated femoral head from the medial wall defect. It is denuded of cartilage and then replaced into the medial defect as a structural graft. A reinforcement ring is implanted to reconstruct the anterior wall defect and an all-poly cup is cemented directly into the ring to achieve a stable acetabular reconstruction (Fig. 3b).
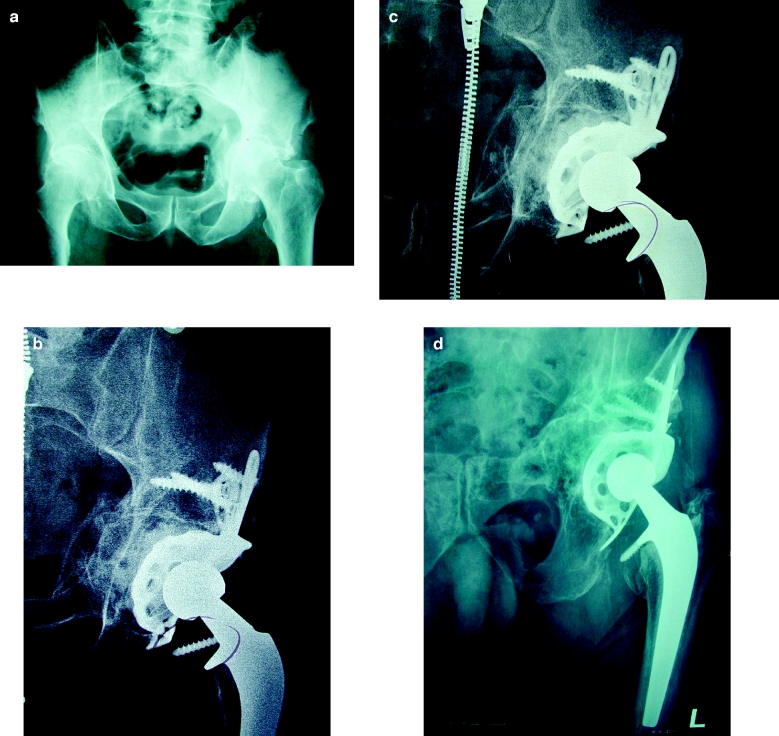
Fig. 3.
a A radiograph of the pelvis of an 88-year-old woman who fell, suffering a central fracture dislocation of the hip with displaced fracture of the anterior wall. b A radiograph of the hip after primary total hip arthroplasty using a reinforcement ring, femoral head bone graft, and cemented all-poly cup. c A radiograph at 1 year demonstrating stability of the cup with incorporation of the femoral head graft. d A radiograph taken 5 years after total hip replacement using an antiprotrusion cage for a central acetabular fracture dislocation for a 91-year-old man. The bone graft has fully incorporated, restoring acetabular bone stock
An 88-year-old woman was allowed to bear weight as tolerated immediately and is doing well 1 year after reconstruction (Fig. 3c). Figure 3d is a radiograph obtained at 5 years after repair of a central acetabular dislocation in a patient by using this tactic. This patient is now 91 years old. He has no complaint of hip pain, ambulates with a cane, and is pleased with his left hip function. The femoral head bone graft has completely incorporated resulting in excellent bone stock in the unlikely event that revision surgery would be required.
Postoperative rehabilitation
The postoperative care of these patients is identical to that of elderly hip fracture and total hip arthroplasty patients. As mentioned above, antibiotic prophylaxis is mandatory.
Ancef or vancomycin (for the penicillin-allergic patient) is administered within 1 hour of the time of incision. A strategy to minimize the risk of thromboembolism should be implemented. This strategy can be the same as that used for total hip replacement patients in the same institution. Prophylaxis for heterotopic ossification is also needed, as it can occur even in these elderly patients. Radiation treatment to the affected hip is usually used. A single dose of 800 rad (8 Gy) is effective in preventing significant heterotopic bone formation and has no risk of complications in this aged population.
These patients should be mobilized out of bed immediately after surgery. Weight bearing as tolerated with a walker is instituted on postoperative day 1 and ambulation is advanced as tolerated. Posterior hip dislocation precautions should also be observed. A protocol similar to the total hip replacement regimen is suitable.
Reported surgical results
Tidermark and his colleagues [14] reported on a series of 10 patients treated by this technique followed up for 33 months. There were no instances of loosening and all the bone grafts incorporated. All the patients were independent walkers with an average Harris hip score of 85. Mears and Velyvis [7] reported a series of 57 patients with 8- to 10-year follow-up. Eighty percent of these elderly patients had good to excellent Harris hip ratings and none required revision for loosening or mechanical failure.
Summary
In general, acute total hip replacement will provide the best functional outcome for the elderly patient with severe acetabular fracture. It seems that the trend toward treatment of displaced femoral neck fractures by total hip replacement will be mirrored in the treatment of displaced acetabular fractures in elderly patients [15]. Since reliable techniques are now well described for immediate use of total hip arthroplasty for these injuries, this approach should be considered as an efficient approach to care that is well suited to the elderly patient. The early clinical experience with this approach to treatment suggests that immediate total hip replacement yields results that are similar to total hip replacement performed for degenerative hip arthritis.
References
- 1.Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999;7:128–141. doi: 10.5435/00124635-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Judet R, Judet J, Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction—preliminary report. J Bone Joint Surg Am. 1964;46:1615–1646. [PubMed] [Google Scholar]
- 3.Spencer RF. Acetabular fractures in older patients. J Bone Joint Surg Br. 1989;71:774–776. doi: 10.1302/0301-620X.71B5.2584245. [DOI] [PubMed] [Google Scholar]
- 4.Anglen JO, Burd TA, Hendricks KJ, Harrison P. The gull sign: Harbinger of failure for internal fixation of geriatric acetabular fractures. J Orthop Trauma. 2003;17:625–634. doi: 10.1097/00005131-200310000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Matta JM. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after injury. J Bone Joint Surg Am. 1996;78:1632–1645. [PubMed] [Google Scholar]
- 6.Helfet DL, Borrelli J, DiPasquale T. Stabilization of acetabular fractures in elderly patients. J Bone Joint Surg Am. 1992;74:753–765. [PubMed] [Google Scholar]
- 7.Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures. J Bone Joint Surg Am. 2002;84:1–9. doi: 10.1302/0301-620X.84B1.12792. [DOI] [PubMed] [Google Scholar]
- 8.Gross AE, Allan DG, Catre M, Garbuz DS, Stocking I. Bone grafts in hip replacement surgery. Orthop Clin North Am. 1993;24:679–695. [PubMed] [Google Scholar]
- 9.Tile M, Rubenstein J (1995) Fractures of the pelvis and acetabulum. In: Tile M (ed), 2nd edn. Williams and Wilkins, Chapter 17
- 10.Beaule PE, Griffin DB, Matta JM. The levine anterior approach for total hip replacement for an acute acetabular fracture. J Orthop Trauma. 2004;18:623–629. doi: 10.1097/00005131-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kang CS, Min BW. Cable fixation in displaced fractures of the acetabulum. Acta Orthop Scand. 2002;73:619–624. doi: 10.1080/000164702321039561. [DOI] [PubMed] [Google Scholar]
- 12.Mouhsine E, Garofalo R, Borens O, Fischer J, Crevoisier X, et al. Acute total hip arthroplasty for acetabular fractures in the elderly. Acta Orthop Scand. 2002;73:615–618. doi: 10.1080/000164702321039552. [DOI] [PubMed] [Google Scholar]
- 13.Mouhsine E, Garofalo R, Borens O, Blanc C, Wettstein M, Leyvraz PF. Cable fixation and early total hip arthroplasty in treatment of acetabular fractures in elderly patients. J Arthroplast. 2004;19:344–348. doi: 10.1016/j.arth.2003.08.020. [DOI] [PubMed] [Google Scholar]
- 14.Tidermark J, Blomfeldt R, Ponzer S, Soderqvist A, Tornkvist H. Primary total hip arthroplasty with a Burch-Schneider antiprotrusion cage and autologous bone grafting for acetabular fractures in elderly patients. J Orthop Trauma. 2003;17:193–197. doi: 10.1097/00005131-200303000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Tidermark J, Ponzer S, Svensson O, Soderqvist A, Tornkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomized, controlled study. J Bone Joint Surg Br. 2003;85:380–388. doi: 10.1302/0301-620X.85B3.13609. [DOI] [PubMed] [Google Scholar]