Abstract
Stiffness is the most prevalent early local complication of primary total knee replacement, affecting approximately 6 to 7% of patients undergoing surgery. The definition of stiffness after total knee replacement in terms of restriction of the arc of motion has evolved in the last 2 decades as patients and physicians expect better postoperative functional outcomes. Gentle manipulation under anesthesia within 3 to 4 months of surgery improves the range of motion in most patients. However, approximately 1% of patients, including those in which the window for manipulation has passed, will require further surgical interventions, which may include arthroscopy with lysis of adhesions, open debridement with exchange of the polyethylene insert, or revision of one or more components. This review will focus on describing the etiology of the problem and the results of the different surgical interventions for stiffness after total knee replacement.
The prevalence of stiffness after total knee replacement
Joint stiffness requiring manipulation is the most common early disabling complication of total knee replacement (TKR). Pariente et al. [28] recently reviewed 5,714 TKRs of the Mayo Clinic Institutional Joint Registry. Manipulation under anesthesia was required in 399 cases (6.9%). Although 74% of those patients responded favorably, 14% required a revision for stiffness. Therefore, approximately 1% of all patients undergoing TKR required revision for stiffness. Similarly, Yercan et al. [39] recently reported that among 1,188 consecutive, posterior stabilized TKRs, 63 patients (5.3%) developed stiffness. Of the 56 patients available for analysis, 46 patients required manipulation and 10 (0.84% of the original cohort) required revision surgery. In the experience of one of the authors (AGDV) after 116 consecutive primary TKRs over the last 2 years, six patients (6 knees—5.1%) required manipulation; and one patient (1 knee—0.9%) required revision surgery. Thus, the incidence of postoperative stiffness was 6%.
The definition of stiffness
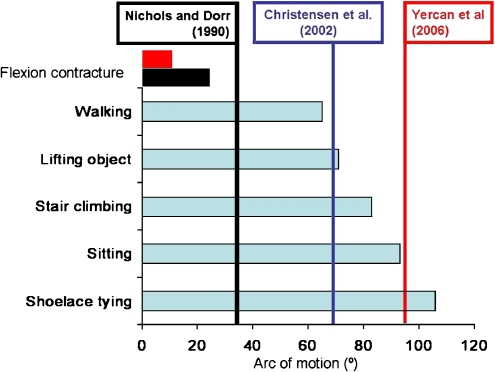
The definition of stiffness after TKR evolved over time, reflecting both patient and physician’s increasing expectations for function and range of motion (ROM) after surgery. Patients require a knee flexion of 65° to walk, 70° to lift an object from the floor, 85° for stair climbing, 95° for comfortable sitting and standing, and 105° for tying shoelaces [24, 31] (Fig. 1). Nichols and Dorr in 1990 [27] defined stiffness after TKR when there was a flexion contracture of 25° or the arc of motion was less than 45°. Christiensen et al. in 2002 [6] defined stiffness when the arc of motion was less than 70°. Finally, Yercan and coworkers in 2006 [39] defined stiffness when the flexion contracture was equal or greater than 10° or the arc of motion was less than 95° (Fig. 1). Many of these patients, especially those with severe limitation of ROM, have severe disabling pain that interferes with their activities of daily living and quality of life.
Fig. 1.
Histogram demonstrating the arc of motion required for activities of daily living and definitions of stiffness according to three publications [6, 27, 39]
The etiology of stiffness after TKR
Stiffness after TKR is a multifactorial problem in which preoperative, operative, and postoperative factors can be identified. Before primary surgery, the surgeon should recognize the predisposing factors for stiffness to better address patient’s expectation for postoperative ROM. During the evaluation of a patient who presents with a stiff TKR, the surgeon should attempt at identifying pre-, intra-, and postoperative factors that might have led to postoperative stiffness. This will allow to select the appropriate surgery and to address the patient’s expectations for function and range of motion before surgery.
Preoperative factors Patients presenting with posttraumatic osteoarthritis, those who underwent a prior high tibial osteotomy [15, 17], and those who present with a limited preoperative ROM are at an increased risk of developing postoperative stiffness [14, 30, 34].
The preoperative ROM is a strong predictor of the postoperative ROM after TKR. Ritter and Stringer [30] correlated postoperative flexion with preoperative flexion in a series of 145 consecutive TKR patients. Patients with limited preoperative flexion (equal or less than 75°) achieved a mean flexion of 85° 1 year after surgery; whereas those with mean preoperative flexion between 76° and 95° achieved a mean postoperative flexion of 95°. Patients with limited preoperative ROM still benefit from TKR. Montgomery, Haas et al. [26] followed 71 patients (82 TKR) with severe preoperative limitations of motion with an average flexion contracture of 22° and a maximum flexion of 58° for an average of 5.5 years (range 2 to 12 years). The average postoperative range of motion improved to 93° (range 35° to 130°) with an average maximum flexion of 94°. Fourteen knees (17%) had postoperative flexion contractures of 10° or less. No knees had a flexion contracture of >10°.
The role that obesity plays in the development of postoperative restriction of ROM is debatable. Shoji et al. [34] observed that obesity limits the postoperative ROM, presumably because of impingement of the posterior soft tissues, whereas Daluga et al. [8] did not find an association between obesity and postoperative stiffness.
Patients with history of stiffness after a TKR are at a higher risk of developing stiffness in a contralateral TKR. Lang et al. [22] recently reported that among 34 patients who had revision TKR for stiffness and 104 who had closed manipulations after primary TKR, 15 patients subsequently underwent contralateral primary TKA. Four of 15 study patients (26.7%) developed arthrofibrosis requiring manipulation. There was a significantly higher rate of closed manipulation in the study group (p = 0.007).
Intraoperative factors The technical errors leading to stiffness after TKR can be categorized in the following groups: retained osteophytes in the posterior condyles, imbalance of the flexion and extension gaps, malalignment, improperly sized components, and inaccurate patellofemoral joint reconstruction [4, 36]. These technical errors can often be detected on plain radiographs and can be differentiated from other sources of stiffness (i.e., arthrofibrosis). If revision surgery for stiffness is indicated, addressing these technical errors will increase the likelihood of a successful outcome.
Retained osteophytes: The incomplete resection of the posterior osteophytes can limit knee extension by impeding full excursion of the posterior capsule in extension. In addition, it can limit flexion through impingement with the posterior aspect of the polyethylene insert.
-
Imbalance of the flexion and extension gaps and improperly sized components: These two categories frequently overlap. A tight flexion gap can result from a posteriorly placed femoral component (Fig. 2). However, it is most frequently caused by implantation of an oversized femoral component (Fig. 3). Increasing the anterior–posterior (AP) diameter of the knee favors flexion contractures and the eventual need for manipulation. Deluga et al., [8] studied a matched paired group of 94 posterior stabilized TKR patients requiring manipulation and 41 posterior stabilized TKR patients who did not. They concluded that an increase in the AP diameter of the knee of 12% was the only independent variable predisposing to manipulation. Excessive tension of the posterior cruciate ligament (PCL) after implantation of cruciate retaining TKR can also limit postoperative ROM by restricting the flexion gap.
A tight extension gap frequently results from insufficient distal femoral resection and can lead to a flexion contracture. Tightness in flexion and extension usually indicates insufficient tibial resection or the insertion of a thicker than necessary polyethylene insert.
Elevation of the joint line has also been associated with the development of postoperative knee stiffness [11, 34]. Figgie et al. [11] followed 101 consecutive patients (116 posterior stabilized knees) for over 2 years and found that elevation of the joint line of at least 10 mm was associated with joint stiffness. Shoji et al. [34] reported similar findings when the joint line was elevated at least 16 mm.
Malalignment: It can occur in the coronal, sagittal, and rotational planes. In the coronal plane, an error of more than 5° may increase the likelihood of stiffness. In the sagittal plane, an excessively flexed or extended femoral component can limit ROM (Fig. 4). More frequently, anterior slope of the tibial component can limit ROM. An anterior tibial slope can result in hyperextension and recurvatum deformity and limited flexion. Conversely, a tibial tray with excessive posterior slope can limit extension and produce flexion instability.
Inaccurate patellofemoral joint reconstruction: Maltracking or tilting of the patella as a result of asymmetric resection, malrotation of the tibial or femoral component, or excessive tightness of the lateral retinaculum can produce restricted flexion by mechanical and pain-related pathways. Overstuffing the patellofemoral joint predisposes to tightness of the extensor mechanism and therefore to limited flexion (Fig. 5). This situation can be created through insufficient resection of the patella [34] or anterior placement of the femoral component when posterior referencing instrumentation is used. Bengs and Scott studied the effect of patellar thickness on intraoperative knee flexion and patellar tracking. They used custom patellar trials with a thickness of 2, 4, 6, and 8 mm more than the real implant. In 31 consecutive knees, they demonstrated that intraoperative passive knee flexion decreased 3° for every 2-mm increment of patellar thickness. Increased patellar thickness had no gross effect on patellar subluxation or tilt [4].
Miscellaneous causes: The effect of closing the capsule in flexion on the postoperative ROM is controversial. A prospective study of 75 primary TKRs randomized to undergo closure of the capsule and fascia in full extension or in 60° of flexion [25] showed no difference in postoperative ROM. Another study [10] found that closure of the fascia and capsule in 90° to 110° of flexion provided additional 5° of flexion at 1-year follow-up (117.9° vs. 112.9°).
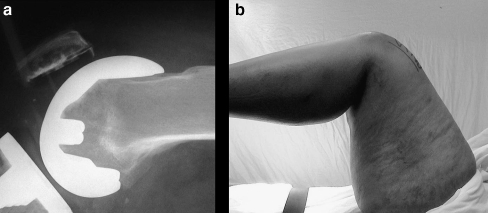
Fig. 2.
a and b: A posteriorly displaced femoral component results in a tight flexion gap and limited flexion
Fig. 3.
An oversized femoral component resulted in marked flexion contracture of 30° (a). Isolated downsizing of the femoral component resulted in correction of the flexion contracture (b)
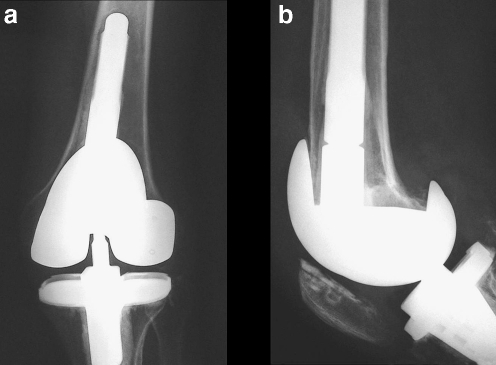
Fig. 4.
Oversized and flexed femoral component resulted in limited flexion and extension (a,b). Normal biomechanics isolated revision of the femoral component (c)
Fig. 5.
Overstuffed patellofemoral joint resulted in limited flexion
Postoperative factors
Postoperative factors potentially leading to knee stiffness and restriction of ROM include poor patient motivation and/or selection, deep infection, heterotopic ossification, pain management regimen, and aggressive anticoagulation therapy, which may result in the development of intraarticular hematomas with secondary stiffness. Keays et al. [19] demonstrated that Enoxaparin delayed the return of early flexion after TKR. Their study compared the effect of enoxaparin and aspirin, on restoration of ROM of two groups of 75 consecutive patients, matched for age, arthritic severity, and preoperative ROM. Patients on enoxaparin reached 90°, 100°, and 110° of flexion in 8.4, 10.4, and 12.4 days, respectively. Patients on aspirin reached the same goals in 6.8, 8.5, and 10.6 days, respectively (p < 0.001). No statistically significant difference in flexion was seen between the groups 15 months after surgery.
Surgical management of the stiff TKR
Manipulation under general or epidural anesthesia is generally successful in improving range of motion when used within the first 3 months of surgery. An excessively aggressive or a late manipulation of the knee can result in complications such as supracondylar femur fracture, patellar tendon avulsion, quadriceps tendon tears, hematoma formation, or wound dehiscence [40].
In the event of an unsuccessful manipulation or when the window for safe manipulation has passed [18], different surgical options may be considered. Among the possible surgical treatments for stiffness, we will discuss the role of arthroscopic lysis of adhesions, open debridement of the joint with exchange of the polyethylene insert, and revision TKR.
We performed a review of the PubMed literature without time limits to obtain information on clinical series of surgical interventions for stiff TKRs. We analyzed 16 publications with information on 198 surgical procedures and recorded the type of surgery, the average gain in ROM and follow-up. Unhappy or reoperated patients were considered failures.
Arthroscopy of the knee for stiffness
In the stiff TKR, a dense fibrous scar (Fig. 6) occupies the suprapatellar pouch and gutters. During open surgery for the treatment of stiffness, this fibrous scar is completely resected to allow exposure of the prosthetic components and improved motion. In the majority of patients with stiff TKR, the scar is abundant and dense in collagen fibers (Fig. 6). Therefore, the use of arthroscopy for the effective treatment of stiffness is limited for two reasons: first, the amount of scar tissue that can be efficiently resected through an arthroscopy is limited. Second, it is not possible to address any implant related causes of stiffness, exchange a polyethylene insert, or perform a posterior capsular release. On the other hand, it is a less invasive procedure and in selected cases proved to improve the ROM.
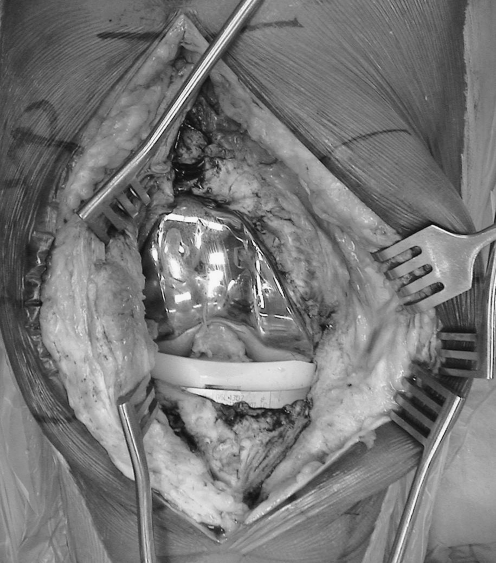
Fig. 7.
The suprapatellar pouch and gutters should be reestablished by removing all scar tissue. This will allow assessment of knee balance and removal of the components
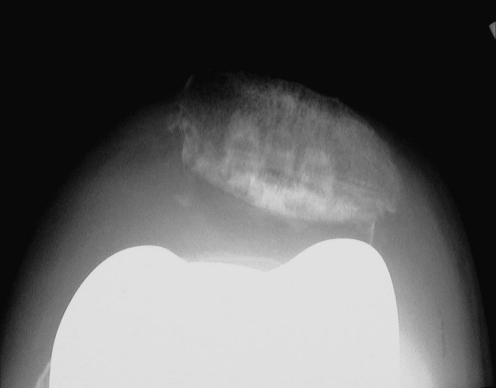
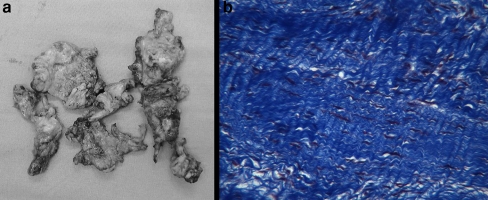
Fig. 6.
Dense fibrous scar occupying the suprapatellar pouch and gutters was resected (a). The histology specimen shows abundant collagen fibers (b) (Courtesy of Dr. Giorgio Perino)
Williams et al. [38] reported the clinical results of the arthroscopic release of the posterior cruciate ligament in nine patients with stiff, cruciate retaining TKRs at an average follow-up of 29 months after surgery. The mean knee flexion increased by 30°, the mean extension deficit was reduced to 1.5° (range 0 to 10). Two patients required a subsequent revision.
xWe analyzed seven peer reviewed publications between 1987 and 2006 collecting information on 49 arthroscopies for stiff TKR [3, 5, 9, 33, 35, 38, 39] . The follow up of these series ranged from 3 months to a year and the mean increase in the arc of motion was modest, ranging from 0° to 42°. Twelve of the 49 procedures (24.5%) failed. The previously mentioned inherent limitations of the arthroscopic approach may explain this high failure rate. Arthroscopy has the potential for scratching the femoral component that may lead to increased polyethylene wear.
Arthrolysis and liner exchange
In the presence of a combined flexion and extension deficit in a patient with a sound biomechanical reconstruction and well-fixed components, an open arthrolysis and the exchange of the polyethylene insert can be considered. During surgery, the removal of the insert allows access to the posterior capsule, which can be released from the femur or the tibia if anterior subluxation of the tibia is possible. Downsizing the polyethylene insert has a limited impact in the success of the operation, which vastly depends on the thorough debridement, excision of the fibrous tissue in the suprapatellar pouch, medial and lateral gutters and the posterior capsular release. If the component alignment, position, sizing, and/or fixation can be improved, this limited approach is not indicated.
We analyzed four peer reviewed publications [2, 16, 20, 39] between 2001 and 2006 encompassing 37 procedures with a follow up of 3 to 4 years. The average increase in the arc of motion was 20° to 40° and failure was detected in eight cases (21.6%). Some authors have reported discouraging results with this technique: Babis et al. [2] reported the results of isolated insert exchange and arthrolysis in seven patients with stiff TKRs at a mean of 12 months after the previous surgery. The inserts were downsized in average, 2.5 mm in relation to the primary inserts. During surgery, full extension and a mean of 100° of flexion was achieved in all patients. After an average follow up of 4.2 years, two knees were re-revised. Five knees had moderate (one knee) to severe (four knees) pain at final follow-up. The gain in the arc of motion was modest from 38.6° (range 15° to 60°) preoperatively to 58° postoperatively (range 40° to 70°).
Revision surgery
The best candidates for revision are those in whom identifiable causes of stiffness can be corrected. Revision surgery remains the most effective surgical treatment for stiffness after TKR. We reviewed seven publications [6, 13, 20, 21, 27, 29, 39] from 1990 to 2006, including 112 procedures after a follow up of 3 to 4 years. The mean increase in arc of motion was 16° to 50°, with 16 cases (14.3%) considered failures.
Surgical approach during revision surgery should allow visualization of the components for their removal, and lateralization of the extensor mechanism without excessive tension. The disruption of the extensor mechanism is catastrophic and of difficult solution. In most cases, periosteal dissection of the proximal and medial tibia allows for external rotation of the tibia and proper lateralization of the extensor mechanism. If this approach proves to be insufficient, a lateral release can help lateralize or evert the patella.
A quadriceps snip is frequently needed to enhance exposure and diminish tension on the extensor mechanism. Other extensile approaches such as a Coonse Adams patellar turndown or anterior tibial tubercle osteotomy are seldom required.
The quadriceps snip [12] allows easy extension of the standard midline incision by carrying the dissection of the tendon at the proximal end in an oblique direction (45°) from medial-distal to lateral-proximal. Closure is carried out in a side-to-side fashion.
The V-Y quadricepsplasty was first described by Coonse and Adams [7] in 1943 and modified by Scott and Siliski in 1985 [32] to preserve the superior lateral geniculate artery. Subsequently, the approach was modified by Aglietti [1] in an attempt to preserve the inferior lateral geniculate artery and became known as the patellar turndown. The Coonse-Adams V-Y quadricepsplasty extends the standard medial parapatellar approach by incising the medial apex of the quadriceps tendon in a 45° angle toward the proximal lateral tibia. The length of this downward component of the incision can be adjusted to the relative stiffness of each individual case.
A tibial tubercle osteotomy [37] can be a suitable alternative when lengthening of the extensor mechanism is not necessary. This approach extends the distal skin incision exposing the patellar tendon on the tibial tubercle. After careful dissection of the tendon, a coronal osteotomy cut and two transverse cuts, allows the whole tubercle to be hinged laterally, maintaining its soft-tissue envelope. The osteotomized tubercle will have a length of 7–8 cm, a width of 2–3 cm and a tapered thickness being thinner distally (5–7 mm) and thicker proximally (10 mm). The tubercle can be reattached with two or three cerclage wires or with screws.
Limited revision of the femoral component
Deciding which component to revise during a total knee revision for stiffness is not always clear. Isolated femoral revision can be attempted in a patient who has properly oriented and sized tibial component, with a joint line in the proper position, and without the presence of a patella baja. The revision of the femoral component allows the surgeon to increase the flexion and/or extension gaps according to the surgical findings and circumstances of each particular case (Fig. 8). In addition, isolated revision of the femoral component is technically easier than the isolated revision of the tibial component; the exposure is straightforward and allows full access to the posterior capsule both in the femoral and tibial sides for an extensive capsular release (Fig. 9) and may also allow use of implants of increased constraints (posterior stabilized and CCK knees).
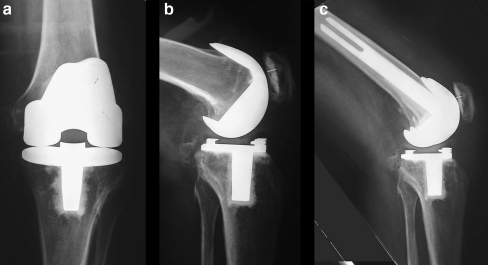
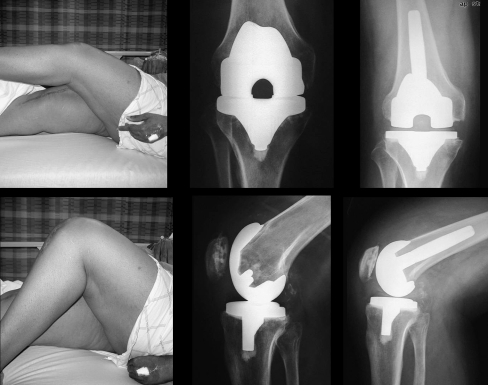
Fig. 8.
In a patient with a sound biomechanical knee reconstruction, and with a combined flexion and extension deficit; the isolated revision of the femoral component increased the flexion and extension gaps
Fig. 9.
Isolated femoral revision is technically easy and allows access to the posterior capsule
Rehabilitation guidelines
Rehabilitation after revision TKR for stiffness is paramount. Poor compliance with an intensive rehabilitation protocol after surgery can result in persistence or worsening of the stiffness. During the immediate postoperative period, the use of a pillow under the affected knee must be avoided as this may lead to a flexion contracture [23].
The postoperative weight-bearing status, and the active and passive range of motion depends on the surgical exposure, intraoperative findings, and type of reconstruction, and must be dictated by the surgeon.
Three basic principles must be observed. First: securing and protecting the osseous fixation and the soft tissue reconstruction. Second: limitation of the stress imposed on the extensor mechanism. Third: gradual and safe progression in the arc of motion to that achieved during surgery.
The rehabilitation protocol after a quadriceps snip approach does not differ from that of a standard parapatellar approach. When other extensile approaches are used (tibial tubercle osteotomy, Coonse Adams), a knee brace locked in extension for 6 weeks should be used during ambulation. At all other times, the maximum flexion allowed by the brace must be the one obtained at the time of surgery. Moderating the amount of stress imposed on the extensor mechanism is attained by avoiding active extension of the knee and straight-leg-raise exercises for 6 weeks. The knee brace can be discontinued after that time and active and gentle-active-assisted ROM can be started.
Final considerations
Stiffness is one of the most frequent complications after TKR. As the functional demands and arc of motion expected from patients and physicians continue to increase, so will the relative frequency of stiffness after TKR. The prevalence of stiffness after TKR can be lowered by careful patient selection, meticulous preoperative planning, and surgical technique. Surgery for a stiff TKR may be required in up to 1% of patients undergoing TKR. Some patients, however, will not benefit from any operation, particularly those with connective tissue disorders, those with no apparent identifiable cause for stiffness, posttraumatic osteoarthritis, or those addicted to narcotic medications. We observed that the functional results are generally better than the objective gain in ROM.
References
- 1.Aglietti P, Windsor RE, Buzzi R, Insall JN (1989) Arthroplasty for the stiff or ankylosed knee. J Arthroplasty 4:1–5 [DOI] [PubMed]
- 2.Babis GC, Trousdale RT, Pagnano MW, Morrey BF (2001) Poor outcomes of isolated tibial insert exchange and arthrolysis for the management of stiffness following total knee arthroplasty. J Bone Jt Surg Am 83-A:1534–1536 [DOI] [PubMed]
- 3.Bae DK, Lee HK, Cho JH (1995) Arthroscopy of symptomatic total knee replacements. Arthroscopy 11:664–671 [DOI] [PubMed]
- 4.Bengs BC, Scott RD (2006) The effect of patellar thickness on intraoperative knee flexion and patellar tracking in total knee arthroplasty. J Arthroplasty 21:650–655 [DOI] [PubMed]
- 5.Campbell ED, Jr. (1987) Arthroscopy in total knee replacements. Arthroscopy 3:31–35 [DOI] [PubMed]
- 6.Christensen CP, Crawford JJ, Olin MD, Vail TP (2002) Revision of the stiff total knee arthroplasty. J Arthroplasty 17:409–415 [DOI] [PubMed]
- 7.Coonse K, Adams JB (1943) A new operative approach to the knee joint. Surg Gynecol Obstet 77:344–347
- 8.Daluga D, Lombardi AV, Jr., Mallory TH, Vaughn BK (1991) Knee manipulation following total knee arthroplasty. Analysis of prognostic variables. J Arthroplasty 6:119–128 [DOI] [PubMed]
- 9.Diduch DR, Scuderi GR, Scott WN, Insall JN, Kelly MA (1997) The efficacy of arthroscopy following total knee replacement. Arthroscopy 13:166–171 [DOI] [PubMed]
- 10.Emerson RH, Jr., Ayers C, Higgins LL (1999) Surgical closing in total knee arthroplasty. A series followup. Clin Orthop Relat Res 368:176–181 [DOI] [PubMed]
- 11.Figgie HE, 3rd, Goldberg VM, Heiple KG, Moller HS, 3rd, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Jt Surg Am 68:1035–1040 [PubMed]
- 12.Garvin KL, Scuderi G, Insall JN (1995) Evolution of the quadriceps snip. Clin Orthop Relat Res 321:131–137 [PubMed]
- 13.Haidukewych GJ, Jacofsky DJ, Pagnano MW, Trousdale RT (2005) Functional results after revision of well-fixed components for stiffness after primary total knee arthroplasty. J Arthroplast 20:133–138 [DOI] [PubMed]
- 14.Harvey IA, Barry K, Kirby SP, Johnson R, Elloy MA (1993) Factors affecting the range of movement of total knee arthroplasty. J Bone Jt Surg Br 75:950–955 [DOI] [PubMed]
- 15.Haslam P, Armstrong M, Geutjens G, Wilton TJ (2007) Total knee arthroplasty after failed high tibial osteotomy long-term follow-up of matched groups. J Arthroplast 22:245–250 [DOI] [PubMed]
- 16.Hutchinson JR, Parish EN, Cross MJ (2005) Results of open arthrolysis for the treatment of stiffness after total knee replacement. J Bone Jt Surg Br 87:1357–1360 [DOI] [PubMed]
- 17.Katz MM, Hungerford DS, Krackow KA, Lennox DW (1987) Results of total knee arthroplasty after failed proximal tibial osteotomy for osteoarthritis. J Bone Jt Surg Am 69:225–233 [PubMed]
- 18.Keating EM, Ritter MA, Harty LD, Haas G, Meding JB, Faris PM, Berend ME (2007) Manipulation after total knee arthroplasty. J Bone Jt Surg Am 89:282–286 [DOI] [PubMed]
- 19.Keays AC, Mason M, Keays SL, Newcombe PA (2003) The effect of anticoagulation on the restoration of range of motion after total knee arthroplasty: enoxaparin versus aspirin. J Arthroplast 18:180–185 [DOI] [PubMed]
- 20.Keeney JA, Clohisy JC, Curry M, Maloney WJ (2005) Revision total knee arthroplasty for restricted motion. Clin Orthop Relat Res 440:135–140 [DOI] [PubMed]
- 21.Kim J, Nelson CL, Lotke PA (2004) Stiffness after total knee arthroplasty. Prevalence of the complication and outcomes of revision. J Bone Jt Surg Am 86-A:1479–1484 [PubMed]
- 22.Lang JE (2006) Clinical Outcomes in Patients with a History of Arthrofibrosis Undergoing Second Primary TKA. In: AAOS 2006 (American Academy of Orthopaedic Surgeons). Chicago, IL
- 23.Laskin RS, Beksac B (2004) Stiffness after total knee arthroplasty. J Arthroplast 19:41–46 [DOI] [PubMed]
- 24.Laubenthal KN, Smidt GL, Kettelkamp DB (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34–43 [DOI] [PubMed]
- 25.Masri BA, Laskin RS, Windsor RE, Haas SB (1996) Knee closure in total knee replacement: a randomized prospective trial. Clin Orthop Relat Res 331:81–86 [DOI] [PubMed]
- 26.Montgomery WH, 3rd, Insall JN, Haas SB, Becker MS, Windsor RE (1998) Primary total knee arthroplasty in stiff and ankylosed knees. Am J Knee Surg 11:20–23 [PubMed]
- 27.Nicholls DW, Dorr LD (1990) Revision surgery for stiff total knee arthroplasty. J Arthroplast 5:S73–77 (Suppl) [DOI] [PubMed]
- 28.Pariente GM, Lombardi AV, Jr., Berend KR, Mallory TH, Adams JB (2006) Manipulation with prolonged epidural analgesia for treatment of TKA complicated by arthrofibrosis. Surg Technol Int 15:221–224 [PubMed]
- 29.Ries MD, Badalamente M (2000) Arthrofibrosis after total knee arthroplasty. Clin Orthop Relat Res:177–183 [DOI] [PubMed]
- 30.Ritter MA, Stringer EA (1979) Predictive range of motion after total knee replacement. Clin Orthop Relat Res 143:115–119 [PubMed]
- 31.Schurman DJ, Parker JN, Ornstein D (1985) Total condylar knee replacement. A study of factors influencing range of motion as late as two years after arthroplasty. J Bone Jt Surg Am 67:1006–1014 [PubMed]
- 32.Scott RD, Siliski JM (1985) The use of a modified V-Y quadricepsplasty during total knee replacement to gain exposure and improve flexion in the ankylosed knee. Orthopedics 8:45–48 [DOI] [PubMed]
- 33.Scranton PE, Jr. (2001) Management of knee pain and stiffness after total knee arthroplasty. J Arthroplast 16:428–435 [DOI] [PubMed]
- 34.Shoji H, Solomonow M, Yoshino S, D’Ambrosia R, Dabezies E (1990) Factors affecting postoperative flexion in total knee arthroplasty. Orthopedics 13:643–649 [DOI] [PubMed]
- 35.Sprague NF, 3rd, O’Connor RL, Fox JM (1982) Arthroscopic treatment of postoperative knee fibroarthrosis. Clin Orthop Relat Res 166:165–172 [PubMed]
- 36.Stamos VP, Bono JV (2002) The stiff knee. In: Scuderi GR, Tria AJ (eds) Surgical Techniques in Total Knee Arthroplasty. Springer-Verlag, New York
- 37.Whiteside LA, Ohl MD (1990) Tibial tubercle osteotomy for exposure of the difficult total knee arthroplasty. Clin Orthop Relat Res 260:6–9 [PubMed]
- 38.Williams RJ, 3rd, Westrich GH, Siegel J, Windsor RE (1996) Arthroscopic release of the posterior cruciate ligament for stiff total knee arthroplasty. Clin Orthop Relat Res 331:185–191 [DOI] [PubMed]
- 39.Yercan HS, Sugun TS, Bussiere C, Ait Si Selmi T, Davies A, Neyret P (2006) Stiffness after total knee arthroplasty: prevalence, management and outcomes. Knee 13:111–117 [DOI] [PubMed]
- 40.Bong MR, Di Cesare PE (2004) Stiffness After Total Knee Arthroplasty. J Am Acad Ortho Surg 12:164–171 [DOI] [PubMed]