Abstract
Fifty-seven consecutive patients (58 knees) with an acute, isolated, posterior cruciate ligament (PCL) injury were treated nonoperatively. Clinical, radiographic, and functional assessment was performed at a mean follow-up of 6.9 years (range 2 to 19.3 years) after the initial diagnosis. At the time of initial documentation of the injury, the posterior drawer test was grade A in 17 knees and grade B in 41 knees. The mean preinjury Tegner activity level was 7 (range 4 to 10). At latest follow-up, 38 knees had no pain, 14 had mild pain, and 6 had moderate pain on exertion. Fifty-four knees had no swelling, 3 had mild, intermittent swelling, and 1 had a moderate swelling on exertion. The posterior drawer test was grade A in 14 knees and grade B in 44 knees. The mean Lysholm-II knee score was 85.2 points (range 51 to 100 points) and the mean Tegner activity level was 6.6 (range 3 to 10). Based on Lysholm-II knee scoring system, the results were excellent in 23 knees (40%), good in 30 knees (52%), fair in 2 knees (3%), and poor in 3 knees (5%). No statistically significant correlation (p = 0.097) was seen between the grade of PCL laxity and Lysholm-II knee score. Plain radiographs showed mild (grade I) medial compartment osteoarthritis (OA) in 7 knees, and moderate (grade II) medial compartment OA in 3 knees. Mild patellofemoral OA was seen in 4 knees. We believe that most patients with acute, isolated PCL injuries do well with nonoperative treatment at a mean follow-up of 6.9 years. The level of evidence for this retrospective cohort study is level III.
Key words: natural history, acute/isolated posterior cruciate ligament injury, nonoperative treatment
Introduction
In clinical practice, the posterior cruciate ligament (PCL) injuries are rare compared to anterior cruciate ligament injuries. The incidence of PCL injuries is reported to be between 1 and 47% of acute knee ligament injuries [1–9]. Clancy and Sutherland [10] suggested that up to 40% of PCL injuries are isolated injuries. In recent years, there is an apparent increase in the incidence of PCL injuries, possibly because of an increase in the number of road traffic accidents, increased participation in recreational and competitive sports, and improved awareness and clinical diagnostic skills. Some clinicians [11–13] have reported that isolated PCL injuries are frequently missed on physical examination of the knee.
Most reports on PCL injuries are retrospective studies of acute and chronic PCL injuries that include a mixed population of both isolated and combined ligamentous injuries of the knee [5, 11, 12, 14–28]. Based on these reports, it is difficult to derive a conclusion regarding the ideal management of patients with acute, isolated PCL injuries. Various authors have reported on the results of nonoperative treatment of isolated PCL tears [6, 13, 20, 23, 25, 28–37].
The purpose of our retrospective study is to report clinical, radiographic, and functional results of nonoperative management of patients with acute, isolated PCL injuries. Our study is focused on the nonoperative treatment of patients with acute, isolated PCL injury of the knee.
Materials and methods
Between January 1977 and December 1994, a total of 62 consecutive patients with acute, isolated PCL injuries were treated by the senior authors. Patients with knee dislocations, chronic PCL injuries, and those with associated injuries (either to the posterolateral corner or the medial aspect of the knee) were excluded from this study. Patients with bony avulsion of either the tibial or the femoral attachment of the PCL were also eliminated from the study. All patients were treated nonoperatively with quadriceps muscle rehabilitation with or without bracing. A home-based rehabilitation program was given to all patients with emphasis on gaining range of motion (ROM) in the knee and strength in the lower extremity.
Of the 62 patients, 5 could not be located for follow-up. Fifty-seven patients (58 knees) were evaluated in 1997 by one author (DVP). Of the 58 knees, 17 had a partial and 41 had a complete PCL injury. A detailed subjective, objective, functional, and radiographic assessment was performed for these 58 knees. These patients were not seeking treatment for their knee symptoms at the time of follow-up, thereby minimizing the selection bias. The mean age of the patients at the time of diagnosis of PCL injury was 27.9 years (range 13 to 49 years). There were 44 men and 13 women. The right knee was involved in 34 cases and the left in 24. The details of the cause of injury are shown in Table 1. The majority of the patients were involved with recreational and competitive sporting activities before the injury. Six patients were playing professional football at the National Football League (NFL) level.
Table 1.
Cause of injury
| Cause of Injurya | No. of Knees |
|---|---|
| Football | 12 |
| Motor vehicle accident | 9 |
| Skiing | 7 |
| Soccer | 5 |
| Baseball | 3 |
| Rugby | 2 |
| Softball | 2 |
| Lacrosse | 2 |
| Basketball | 2 |
| Water skiing | 2 |
| Frisbee | 1 |
| Domestic fall | 11 |
aNote that these injuries were sustained by falling on a flexed knee, anterior blow to the flexed knee and in some cases by hyperextension at the knee.
All patients were seen acutely (range 2 to 40 days) after the initial injury; they all had pain with or without knee swelling and difficulty with activities of daily living or sports. The mean knee flexion at the time of initial evaluation was 125° (range 95 to 140°) and the mean extension loss at initial evaluation was 2° (range 0 to 10°).
The subjective assessment included Lysholm-II knee score as reported by Tegner and Lysholm [38], the Tegner activity level [38], and the International Knee Documentation Committee (IKDC) assessment [39]. The original Lysholm score was reported by Lysholm and Gillquist [40] in 1982. The Lysholm-II knee score is a modification of the original Lysholm knee score. The Lysholm-II knee score was graded as excellent, good, fair, or poor as suggested by Odensten et al. [41]. Patients with a score of 91–100 were regarded as excellent, 77–90 as good, 68–76 as fair, and <68 as poor.
The IKDC form [39] mainly involves four areas (subjective assessment, symptoms, ROM, and ligament examination). Each parameter is qualified as normal, nearly normal, abnormal, or severely abnormal. The results of the four areas are used for grading purpose. The worst qualification within the parameter is taken as the group qualification. The worst group qualification is then taken as the final evaluation.
In addition to the abovementioned scoring systems, patients were also asked to subjectively rate the performance of their knees with activities of daily living and sports on a scale of 0 (poor) to 100 (normal).
The objective assessment consisted of physical examination and KT-1000 arthrometer (MedMetric, Inc., San Diego, CA, USA) evaluation [42]. A detailed physical examination of both knees was performed and findings of the ROM, effusion, joint-line tenderness, crepitus, associated laxity of other ligaments (if any), posterior sag of the tibia, posterior drawer test, pivot shift test, and reverse pivot shift test [43] were recorded. The thigh atrophy was measured at a point 10 cm proximal to the superior pole of the patella and was compared with that of the opposite normal knee.
We believe that the traditional grading system for the posterior drawer of 1+, 2+, and 3+ is inherently ambiguous because it relies on the subjective estimation by the examiner of the number of millimeters of posterior translation of the tibia on the femur. Noyes et al. [44] have abandoned this grading system altogether. We have devised a more simplified clinical grading system based on the assessment of the posterior drawer test performed with the knee in 90° of flexion. The grading system is:
Normal: No loss of tibial offset.
Grade A: Slight loss of tibial offset when applying a posterior force to the tibia with the knee at 90° of flexion.
Grade B: The tibia is flush with the femur.
Grade C: The tibia is able to be displaced behind the femur.
In our opinion, this grading system has been more reproducible in our clinic because it relies on displacement of the tibia relative to basic landmarks, rather than displacement based on number of millimeters. The use of this simple and practical grading system has been reported by MacGillivray et al. [45].
In the present study, we have evaluated patients with grade A (partial) and grade B (complete) PCL injuries. Grade C PCL injuries are frequently associated with additional injury to the posterolateral corner or the medial aspect of the knee. Patients who have had an associated injury to the posterolateral corner or the medial aspect of the knee were excluded from this study as our paper is focused on nonoperative treatment of patients with acute, isolated injuries to the PCL.
Preoperative KT-1000 measurements were not possible for all patients because the instrumented device was not available for patients studied between 1977 and 1988. At latest follow-up, the KT-1000 measurements were performed using the technique reported by Daniel et al. [42]. First, the quadriceps neutral angle was determined on the noninjured side. Then, the following measurements were performed with both knees flexed to the quadriceps at a neutral angle: the posterior laxity from the resting position using 89 N posterior force and the active anterior translation (with quadriceps contraction) from the resting position. The results of both these measurements were added to obtain the corrected posterior drawer laxity.
The radiographic evaluation consisted of anteroposterior weightbearing view, the 45° posteroanterior flexion weightbearing view [46], lateral view, and Merchant’s view [47] for both patellae. The radiographs were graded as grade 0, normal; grade I, mild degenerative changes (less than 2 mm of narrowing of the apparent joint space and the presence of small intercondylar or pericondylar osteophytes); grade II, moderate degenerative changes (2 to 3 mm of narrowing of the apparent joint space, periarticular sclerosis, and the presence of intercondylar or pericondylar osteophytes); and grade III, severe degenerative changes (more than 3 mm of narrowing of the apparent joint space, and the presence of extensive osteophytes). None of the patients had positive radiographic changes in their knees at the time of initial outpatient visit.
Each of the 57 patients was requested to have a radioisotope (Technetium 99m methylene diphosphonate) bone scan. A total of 20 patients agreed to have a bone scan. The purpose of the bone scan was to assess the presence of degenerative changes in the knee at an early stage. We asked the patients whether they would like to undergo bone scan irrespective of the presence or absence of clinical symptoms. Seventeen of the 20 patients were selected at random from the database for bone scan assessment, whereas the remaining 3 patients had a bone scan because of persistent knee symptoms. These three patients were initially asymptomatic but subsequently developed clinical symptoms at an average of 28 months (range 22 to 32 months) after the initial injury.
The diagnosis of PCL tear was made by a detailed history and physical examination in 10 knees, with the addition of magnetic resonance imaging (MRI) in 42 knees, and by arthroscopic evaluation in 21 of the 58 knees. Overall, 15 of 58 knees had both MRI and arthroscopic assessment, whereas 10 of 58 knees had neither MRI nor arthroscopic evaluation; in the latter group the diagnosis was made by physical examination. The distinction between partial and complete PCL injuries was made on the basis of arthroscopic findings and MRI studies. Of the 48 knees that had MRI and/or arthroscopic evaluation, 8 knees had a partial PCL tear and 40 knees had a complete PCL tear. Of the 10 knees that were solely evaluated by physical examination, 9 had a grade A (partial) PCL injury and one had a grade B (complete) PCL injury. Overall, based on physical examination and MRI and arthroscopic assessment, 17 knees had a grade A (partial) PCL tear and 41 knees had a grade B (complete) PCL tear.
At the time of initial injury, MRI was available for 42 of 58 knees. In the earlier part of our study, MRI was done to identify associated meniscal and/or chondral damage and to confirm the clinical diagnosis of PCL tear. Six knees had a partial PCL tear and 36 knees had a complete PCL tear based on MRI findings.
Twenty-one of the 58 knees had an arthroscopic assessment for suspected meniscal and/or chondral injury. On arthroscopic evaluation, 2 knees had a partial PCL tear and 19 knees had a complete PCL tear. Six of the 21 knees undergoing arthroscopic evaluation had associated meniscal tears (4 medial and 2 lateral) at the time of the initial PCL injury. All 6 meniscal tears were treated by arthroscopic partial meniscectomy with preservation of a stable rim. One patient sustained a bilateral PCL injury (on separate occasions) while playing football. At arthroscopy, a grade IV chondral lesion (exposed subchondral bone) was seen in the medial femoral condyle in both knees. These lesions were treated by arthroscopic debridement and curettage at the base of the crater. Two other patients had a grade II chondral injury (a partial thickness defect with fissures on the surface that do not reach subchondral bone or exceed 1.5 cm in diameter) to the medial femoral condyle and retropatellar surface (as seen at arthroscopy) at the time of initial injury. None of these three patients with chondral lesions had an associated meniscal lesion.
Statistical analysis
Chi-square analysis, Student’s t test, Pearson’s correlation coefficient, and Spearman’s rank correlation coefficient were used for the statistical analysis of the results. The Mann–Whitney U test (two groups) was used for unpaired data. Significance was accepted at a p value of less than 0.05.
Results
Symptoms
At latest follow-up evaluation, there was no pain in 38 knees (66%), mild pain in 14 knees (24%), and moderate pain on exertion in 6 knees (10%). There was no swelling in 54 knees (93%), mild, intermittent swelling in 3 knees (5%), and moderate swelling on exertion in 1 knee (2%). Fifty-two patients (91%) had no giving way whereas 5 patients (9%) complained of occasional giving way, especially while going downstairs. On detailed questioning, we noted that these patients mainly complained of “buckling” of the knee while going downstairs rather than true rotatory giving way as seen with twisting, cutting, or pivoting activities. Sixteen patients (28%) complained of occasional stiffness in the knee. Five patients (9%) had mild difficulty in stop/start activities, and 13 (23%) had slight difficulty with jump/land activities.
Eleven patients (19%) complained of slight difficulty in walking, especially on uneven surfaces. None of the patients had moderate problems with walking and none required a walking aid. Twelve patients (21%) had slight problems while running. Eight patients (14%) complained of mild pain with stairs. None of the patients required a banister for support.
Subjective assessment
Lysholm-II knee score at the time of initial PCL injury was not available. At latest follow-up, the mean Lysholm-II knee score was 85.2 ± 10 (range 51 to 100). Based on the Lysholm-II knee score grading system reported by Odensten et al. [41], the results were excellent in 23 knees (40%), good in 30 knees (52%), fair in 2 knees (3%), and poor in 3 knees (5%). The mean preinjury Tegner activity level was 7 (range 4 to 10). At latest follow-up, the mean Tegner activity level was 6.6 ± 1.8 (range 3 to 10). Functional evaluation was performed using the single-legged hop test. The mean hop distance for the PCL-deficient knee was 132 ± 27 cm (range 37 to 196 cm). The mean ratio of the hop distance for the involved and the noninvolved extremity was 0.95.
All 57 patients had completed the IKDC form [39]. Based on the IKDC grading system, none of the patients had a normal result. Six patients (6 knees) had a nearly normal result, 50 patients (51 knees) had an abnormal result, and one patient had a severely abnormal result. The deficiency of grading results based on IKDC system is discussed under the “Discussion” section. The mean subjective rating scale for the knee performance with activities of daily living and sports was 84 ± 12.3 (range 30 to 100).
Objective findings
Physical examination
Although four patients complained of subjective knee swelling, on physical examination, only one patient had a demonstrable, mild effusion in the knee at the time of latest review. None of the patients had medial or lateral joint-line tenderness. There was no thigh atrophy in 19 knees. Thirty knees had between 0.5 and 1 cm of thigh atrophy, 8 had between 1.5 and 2 cm of thigh atrophy, and 1 had >2 cm of thigh atrophy compared to the opposite extremity. The average flexion in the PCL-deficient knee was 138° (range 130 to 150°) and the average extension loss was 1° (range 0 to 4°).
The posterior drawer test (with the knee flexed at 90° and the tibia in neutral rotation) was grade A (partial PCL tear) in 14 knees and grade B (complete PCL tear) in 44 knees. None of the knees had a clinically diagnosed grade C PCL laxity at latest follow-up. One important clinical finding noted in this study was that the posterior translation of the tibia decreased in all 58 knees when the posterior drawer test was performed at 90° of knee flexion with the tibia in internal rotation. The tibiofemoral step-off was clinically assessed during physical examination using our grading system for PCL injuries. None of the patients had abnormal medial or lateral collateral ligament laxity at follow-up. None of the patients had a positive external rotation recurvatum test [48] or a positive reverse pivot shift test [43] compared with the opposite normal extremity.
KT-1000 Arthrometer evaluation
The details of the results of KT-1000 evaluation performed at latest follow-up are shown in Table 2. The mean corrected posterior translation of the tibia was 7.9 ± 1.6 mm (range 5 to 11 mm). The mean side-to-side difference from the opposite, noninjured knee was 5.6 ± 1.4 mm (range 3 to 9 mm).
Table 2.
Results of KT-1000 arthrometer evaluation at latest follow-up (no. of knees = 56)
| Mean Corrected Posterior Translation of the Tibia on KT-1000 Evaluation (mm) | No. of Knees |
|---|---|
| 0–2 | 0 |
| 3–5 | 7 |
| 6–10 | 48 |
| >10 | 1 |
Findings of KT-1000 assessment for two knees are excluded because one patient had a bilateral PCL injury.
Radiographic findings
Plain radiographs
At latest follow-up, degenerative changes in the medial compartment were seen in 10 (17%) of the 58 knees. Of these 10 knees, mild (grade I) degenerative changes were seen in 7 and moderate (grade II) degenerative changes were seen in 3 (Fig. 1). None of the knees had grade III (severe) degenerative changes. Mild patellofemoral osteoarthritis (OA) was seen in four knees (7%). Five patients had mild (grade I) degenerative changes in the opposite knee (three involving the medial compartment and two involving the lateral compartment). Three patients had mild (grade I) degenerative changes in the patellofemoral joint of the opposite knee. The association between the severity of degenerative changes in various compartments of the knee and the length of follow-up is shown in Table 3.
Fig. 1.
A 24-year-old athlete sustained an isolated grade B PCL injury while playing football. This was treated nonoperatively. At 16.5-years of follow-up, the plain radiograph of the right knee shows grade II (moderate) degenerative changes in the medial compartment
Table 3.
Association between the severity of degenerative changes in various compartments of the knee and the length of follow-up (total no. of knees = 58)
| Radiographic Changes | No. of Knees | |||
|---|---|---|---|---|
| 0–5 Yearsa | 6–10 Yearsa | 11–15 Yearsa | 16–20 Yearsa | |
| Medial compartment | ||||
| Grade 0 | 16 | 26 | 6 | 0 |
| Grade I | 1 | 4 | 1 | 1 |
| Grade II | 1 | 0 | 1 | 1 |
| Grade III | 0 | 0 | 0 | 0 |
| P–F joint | ||||
| Grade 0 | 17 | 28 | 7 | 2 |
| Grade I | 1 | 2 | 1 | 0 |
| Grade II | 0 | 0 | 0 | 0 |
| Grade III | 0 | 0 | 0 | 0 |
| Lateral compartment | ||||
| Grade 0 | 17 | 29 | 7 | 2 |
| Grade I | 1 | 1 | 1 | 0 |
| Grade II | 0 | 0 | 0 | 0 |
| Grade III | 0 | 0 | 0 | 0 |
Grade 0 = normal, grade I = mild degenerative changes (less than 2 mm of narrowing of the apparent joint space and the presence of small intercondylar or pericondylar osteophytes), grade II = moderate degenerative changes (2 to 3 mm of narrowing of the apparent joint space, periarticular sclerosis, and the presence of intercondylar or pericondylar osteophytes), grade III = severe degenerative changes (more than 3 mm of narrowing of the apparent joint space, and presence of extensive osteophytes)
aLength of follow-up
Radioisotope bone scan findings
Seventeen asymptomatic patients had had radioisotope bone scan at a mean follow-up of 77 months (range 64 to 156 months) since initial injury, whereas three patients had a bone scan because of persistent knee symptoms. Of the 20 patients, 17 had a normal bone scan. All these 17 patients had normal plain radiographic findings in the knee as well. These 17 patients with normal bone scans and radiographs were the 17 asymptomatic subjects.
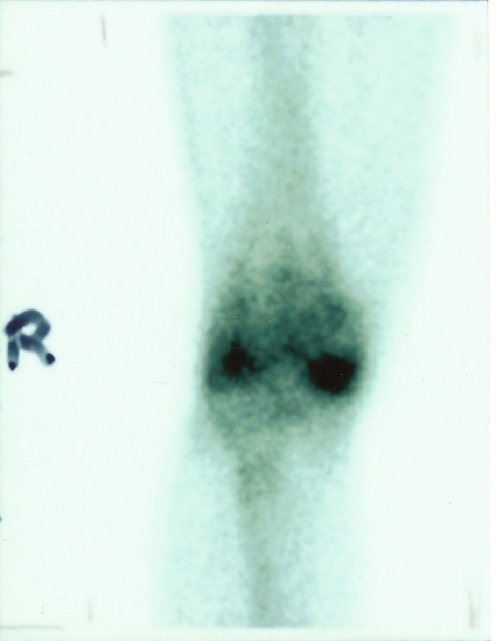
One patient had a mild focal uptake in the medial compartment at 87 months since the original injury. When last seen, this patient had no significant symptoms in his knee and has an excellent functional result. Two patients had a moderate focal uptake of the radioactive isotope in the medial compartment and patellofemoral area at 25 and 32 months, respectively, after the initial injury (Fig. 2). Plain radiographs of the knees in both cases showed moderate degenerative changes in the medial and patellofemoral compartments. Both patients were athletically active individuals and had a grade B initial PCL laxity. They also had grade II chondral damage (as seen at arthroscopy) to the medial femoral condyle and retropatellar surface at the time of initial injury. These two patients are included in our study as they had initial nonoperative treatment for 26 and 34 months, respectively, and subsequently had progressive deterioration of knee symptoms. These two patients underwent a PCL reconstruction at 26 and 34 months, respectively, after the initial injury.
Fig. 2.
A 33-year-old male sustained an isolated grade B PCL tear in the right knee while skiing. At initial arthroscopic evaluation, grade III chondral injury was noted in the medial femoral condyle. Because of persistent knee symptoms, a radioisotope bone scan was performed at 32 months after the initial injury. The bone scan shows a moderate focal uptake of the radioactive isotope in the medial femorotibial compartment
Return to sports
Six patients played professional football at the NFL level. These six players have now retired. All six players played actively at the NFL level for a mean of 121.6 months (range 86 to 160 months) before their retirement. One patient completed Ironman Triathlon twice. Thirty-seven patients (65%) returned to recreational sports. Twenty-four of these 37 patients played at the preinjury level and 13 of 37 patients played at a decreased level. Five patients played different sports compared to the preinjury sports, and eight had decreased or stopped their sporting activities because of reasons unrelated to the PCL-injured knee, such as change in the lifestyle and interests with increasing age or busy work schedule.
One patient (a professional NFL player) had sustained bilateral PCL injuries (on separate occasions) while playing football. At initial arthroscopic assessment, a grade IV chondral lesion (exposed subchondral bone) in the medial femoral condyle was seen in both knees. The chondral lesions in both knees were treated by debridement and drilling of the subchondral bone to increase vascularity and stimulate healing. To date, no PCL reconstruction has been undertaken for this patient. At present, he has retired from professional football and has reduced his activity level. He has mild pain and swelling in both knees on exertion. He participates in recreational basketball and jogging.
Arthroscopy findings
As mentioned under the “Radioisotope bone scan findings” section, two athletically active individuals with a grade B initial PCL laxity had arthroscopic evaluation of their knees at the time of initial injury and grade II chondral damage was noted in the medial femoral condyle and retropatellar surface. Both patients underwent a PCL reconstruction at 26 and 34 months, respectively, after the initial injury. At the time of PCL reconstruction, grade III degenerative changes (fissuring to the level of subchondral bone in an area with a diameter of more than 1.5 cm) in the medial compartment and retropatellar surface were seen in both cases.
Nonoperative treatment failures
The conservative treatment was abandoned for two patients because of clinical deterioration of symptoms and PCL reconstruction was performed for both these athletically active patients who had a grade B initial PCL laxity. These two patients underwent a PCL reconstruction at 26 and 34 months, respectively, after the initial injury. One patient was reviewed at 102 months after the PCL reconstruction and has an excellent functional result (Lysholm-II knee score 94). He plays softball and tennis at the recreational level. The other patient was seen at 38 months after PCL surgery. He has a good functional result (Lysholm-II knee score 86) and he participates in jogging, cycling, tennis, and football at the recreational level. No deterioration in the severity of degenerative changes on plain radiographs was seen at latest review.
One patient sustained a reinjury to his knee as a result of a fall at 71 months after the initial PCL injury. At arthroscopy, a degenerative tear in the posterior segment of the medial meniscus was noted and this was treated by partial meniscectomy. In addition, a peripheral tear of the posterior third of the lateral meniscus was also found and arthroscopic lateral meniscal repair was performed. Grade II chondral changes in the medial femoral condyle were noted. The patient has no meniscal symptoms and has a satisfactory knee function at follow-up of 114 months since the initial PCL injury.
Correlation with findings
No significant correlation was seen between the prevalence of pain and length of follow-up (p > 0.05). No statistically significant correlation (p = 0.097) was seen between the Lysholm-II knee score and the objective PCL laxity. Patients with a grade A PCL laxity had a mean Lysholm-II knee score of 84.2 ± 12.3 and those with a grade B PCL laxity had a mean Lysholm-II knee score of 85.6 ± 9.2. No significant correlation was seen between KT-1000 findings and the Lysholm-II knee score (p > 0.05).
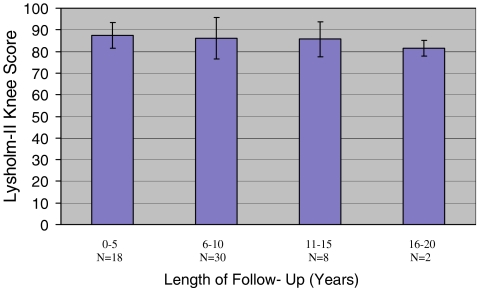
There was no significant correlation between Lysholm-II knee scores and the length of follow-up (Pearson’s correlation r = −0.14, p = 0.3; Spearman rank correlation = −0.1, p = 0.5; Fig. 3). To rule out the effect of advancing age on knee function, we correlated the age of the patients at follow-up vs Lysholm-II knee score. There was no correlation (Pearson’s correlation r = −0.14, p = 0.5) between patients’ age and the Lysholm-II knee score.
Fig. 3.
Lysholm-II knee score vs length of follow-up
There was no significant correlation (Student’s t test = −0.5, p = 0.6; Mann–Whitney U test, p = 0.13) between Lysholm-II knee score and radiographic degenerative changes. Similarly, no correlation (chi-square = 2.2, p = 0.1) was seen between the grade of PCL laxity and radiographic degenerative changes. No correlation (p = 0.5) was noted between the length of follow-up and severity of radiographic degenerative changes.
There was a statistically significant correlation between the objective PCL laxity (as noted on physical examination) and the KT-1000 arthrometer findings of PCL laxity (p < 0.05). There was no correlation between the KT-1000 findings and the presence of pain, giving way, or degenerative changes on radiographs.
Discussion
It is generally believed that the true prevalence of isolated PCL injuries is difficult to determine as many of these injuries may be missed during the initial physical examination. It is possible that there are many patients with undiagnosed PCL ligament injuries who subsequently have not found it necessary to seek the advice of a physician [20, 25]. A high index of suspicion and a detailed knowledge of the physical examination tests are necessary for an accurate diagnosis. We believe that the clinical diagnosis of acute, isolated PCL tears can be reliably made by a detailed history and a thorough physical examination. Rubinstein et al. [49] conducted a blinded, randomized, and controlled study to determine the accuracy of the clinical examination in the setting of isolated, chronic PCL tears. The results of their study showed that the accuracy for detecting a PCL tear was 96% with 90% sensitivity and 99% specificity.
Many authors have reported on the results of nonoperative management of the PCL-deficient knee [6, 13, 20, 23, 25, 28–37]. Boynton and Tietjens [33] retrospectively evaluated 38 patients with isolated, nonoperatively treated PCL injuries at a mean follow-up of 13.4 years (range 5 to 38 years). They concluded that the prognosis for the isolated PCL-deficient knee is variable; some patients experience significant symptoms and articular deterioration, whereas others are essentially asymptomatic and maintain their usual knee function. Shelbourne et al. [34] reported a prospective study of the natural history of acute, isolated, nonoperatively treated PCL-deficient knees in 133 patients. The mean follow-up after initial documentation of the PCL injury was 5.4 years (range 2.3 to 11.4 years). They concluded that patients with acute, isolated PCL injuries can be managed by nonoperative measures and a satisfactory knee function can be obtained in most cases.
We believe that the traditional grading system for the posterior drawer of 1+, 2+, and 3+ is inherently ambiguous as it relies on the subjective estimation by the examiner of the number of millimeters of posterior translation of the tibia on the femur. Often, published reports will quote posterior drawer results as 1+, 2+, or 3+ and interchange these results with grades 1, 2, 3, or 4 injuries to the PCL, without indicating where the tibia is in relation to the femur. Noyes et al. [44] have abandoned this grading system altogether. In their chapter on PCL injuries, Noyes et al. [44] state that “...PCL tears are divided into 2 groups based on the millimeters of increased posterior tibial displacement, indicating either undamaged (<10 mm) or insufficient (>10 mm) secondary restraints. This division is somewhat arbitrary because it is difficult, without using stress radiography under defined loading conditions, to determine the exact increase in posterior tibial translation with PCL ruptures.”
We have therefore devised a more simplified grading system for the posterior drawer test. The system does not seek to determine if an injury is partial or complete. Rather, it assesses the competence of whatever ligament or ligament remnant is present. In our opinion, this grading system has been more reproducible in our clinic because it relies on displacement of the tibia relative to basic landmarks, rather than displacement based on number of millimeters. The use of this simple and practical clinical grading system has been reported by MacGillivray et al. [45].
Physicians have debated and will continue to debate the degree of injury to the PCL in the grade B or C category. This is complicated by the presence of partial injuries and the fact that PCL injuries will often heal in an elongated, nonfunctional position. Thus, grading as to the degree of injury is somewhat arbitrary and a system that simply states the position of the tibia on the femur will be easier to use and eliminate biases in reporting results.
We are aware that there is no evidence in the existing literature that grade A PCL laxity is always a partial tear and a grade B PCL laxity is always a complete tear. In our study, 17 knees had a grade A PCL laxity and 41 knees had a grade B PCL laxity at the time of initial injury. At latest follow-up, 14 knees had a grade A PCL laxity and 44 knees had a grade B PCL laxity. Despite objectively demonstrable PCL laxity, these patients had similar functional knee scores; patients with a grade A PCL laxity had a mean Lysholm-II knee score of 84.2 points and patients with a grade B PCL laxity had a mean Lysholm-II knee score of 85.6 points.
One interesting finding in this study was that there was a predictable decrease in the posterior translation of the tibia when the posterior drawer test was performed with the tibia in 20° of internal rotation compared to posterior translation of the tibia performed with the tibia in neutral rotation. We noted this finding in all 58 knees that were examined. We did not objectively measure the decrease in the posterior tibial translation using KT-1000 arthrometer and, therefore, it is difficult to comment on the precise amount of reduction of the posterior tibial translation that occurs with the tibia in 20° of internal rotation. A similar clinical observation has been made by JA Bergfeld in the early 1980s (Bergfeld, personal communication, 1997) and since then, he has consistently observed this finding in his clinical practice.
In the current study, we found that the KT-1000 arthrometer was accurate in detecting and grading the PCL laxity. A statistically significant correlation (p < 0.05) was seen between the objective PCL laxity (as noted on physical examination) and the findings of PCL laxity as measured by the KT-1000 arthrometer. We believe that the KT-1000 arthrometer can be used for objective documentation of the grade of PCL laxity and is useful for subsequent follow-up examinations. We are aware that stress radiography may be used for objective documentation of the PCL injury [50, 51]. However, stress radiography of the knee was not performed in our series.
In our study, based on the Lysholm-II knee score, 40% of the knees had an excellent result, 52% had a good result, 3% had a fair result, and 5% had a poor result after nonoperative treatment of acute, isolated PCL injuries. Patient who had poor clinical results were mainly involved with heavy manual labor and were unable to perform work that involved deep squatting of the knee and kneeling activities. At latest follow-up, the mean Lysholm-II knee score was 85.2 (range 51 to 100) and the mean Tegner activity level was 6.6 (range 3 to 10). Based on these results, we believe that patients with acute, isolated grade A and grade B PCL laxity do fairly well with nonoperative treatment at an average follow-up of 6.9 years (range 2 to 19.3 years) after the initial diagnosis. It is difficult to predict or identify as to which patients with acute, isolated PCL tear would do well with nonoperative treatment and which patients would not. We agree with other authors [6, 13, 20, 23, 25, 28–30, 32–37] in that patients with an isolated, partial or complete injury of the PCL usually have acceptable functional results when treated nonoperatively. If longer-term follow-up demonstrates more progressive degeneration, then a case could be made for early operative reconstruction.
Based on the IKDC evaluation [39], none of the knees had a normal result, 6 knees had a nearly normal result, 51 knees had an abnormal result, and one knee had a severely abnormal result. At a glance, these results seem rather disappointing and do not correlate well with the results of Lysholm-II knee score as described earlier. As mentioned previously under the “Materials and methods” section, the IKDC form [39] mainly involves four areas (subjective assessment, symptoms, ROM, and ligament examination). Each parameter is graded as normal, nearly normal, abnormal, or severely abnormal. The results of these four areas are used for grading purpose. The worst qualification within the parameter is taken as the group qualification, and the worst group qualification is then taken as the final evaluation. On careful analysis, we found that the major disadvantage of using the IKDC form for overall grading of results of nonoperative treatment of PCL injuries in our study was the group qualification 4 (ligament examination). According to the group qualification 4 (ligament examination), patients who have a 3- to 5-mm (i.e., grade A) posterior translation of the tibia will get a nearly normal result and those with a 6-to 10-mm (i.e., grade B) posterior translation of the tibia will have an abnormal result although the patient has no symptoms and has an excellent knee function with activities of daily living and sports. The results of our study have shown that there is no correlation between the objective PCL laxity and Lysholm-II knee score (p = 0.097). We therefore believe that it may be inappropriate to grade the results of nonoperative treatment of PCL injury solely using the IKDC knee evaluation form.
In our study, there was no correlation between the Lysholm-II knee score and the length of follow-up. In other words, the Lysholm-II knee scores were approximately the same regardless the length of follow-up after initial injury (Fig. 1). Torg et al. [25] also found no correlation between the time from injury and the functional outcome of the knee. No correlation was found between the objective PCL laxity and the Lysholm-II knee score. In other words, patients with a grade A or grade B PCL laxity had similar Lysholm-II knee scores. Dandy and Pusey [20], Cross and Powell [12], Shelbourne et al. [34], and Shelbourne and Muthukaruppan [37] also found no correlation between the objective PCL laxity (as determined by posterior drawer test) and knee function. Torg et al. [25] reported that there was no correlation between posterior knee laxity (as measured by a KT-1000 arthrometer) and the functional status of the patient.
The prevalence of intraarticular abnormalities in patients with PCL injuries has been reported by Geissler and Whipple [52]. However, their study included patients with both acute and chronic PCL injuries. It is difficult to know whether all meniscal lesions in their study were clinically significant and symptomatic. Moreover, no control group of patients was presented in their study.
The true prevalence of meniscal abnormalities in patients with isolated PCL injuries is difficult to determine because most studies have reported the results of PCL tears mixed with other ligamentous injuries, and also because of the fact that the results are mostly based on physical examination rather than direct observation at surgery [5, 6, 13, 15, 18, 22]. In our study, 6 of 21 patients undergoing arthroscopic evaluation were found to have associated meniscal tears (4 medial and 2 lateral) at the time of initial injury. Only one patient had a subsequent meniscal tear during the study period, ranging from 2 to 19.3 years. Based on this data, we believe that subsequent meniscal tears are unlikely to occur in patients with acute, isolated, nonoperatively treated PCL injuries. In our opinion, patients with unidirectional, isolated PCL instability do not have a rotational instability and, therefore, are less likely to sustain damage to their menisci, in contrast to patients with ACL deficiency. Furthermore, a PCL injury usually occurs on an unloaded foot. Therefore, the axial loads required to injure the meniscus are not present. The patients’ histories in our study indicated that the PCL injury occurred on an unloaded foot. We agree with Shelbourne et al. [34] in that PCL laxity allows the tibia and the menisci to shift posteriorly, which puts the menisci in a nonweightbearing position and prevents meniscal tears.
An association between articular cartilage damage and PCL injury has been reported by various studies [32, 52–54]. It is possible that associated chondral damage sustained at the time of initial PCL injury may have influenced the ultimate functional result of the knee in our series. In the present study, 21 of the 58 knees had arthroscopic evaluation at the time of initial injury. It is possible that the remaining 37 knees that did not have arthroscopy may have sustained chondral damage of varying degree. However, it should be noted that 42 of the 58 knees that underwent MRI evaluation at the time of initial injury did not show chondral or osteochondral damage. It should be noted that these were early MRI studies and less proficient at detecting chondral injury.
In patients with PCL-deficient knees, degenerative changes in the medial compartment and patellofemoral joint have been noted by various authors [5, 6, 22, 31]. Some authors [10, 30, 33] have reported that progressive arthrosis should be expected after a PCL injury; however, the conclusions from these studies were drawn in large part from populations of patients with both acute and chronic, isolated and combined PCL injuries, and frequently these populations were symptomatic patients who sought treatment. Skyhar et al. [55] in a biomechanical study using ten cadaveric knees reported that medial compartment pressure was significantly elevated after sectioning of the PCL, whereas patellofemoral pressures and quadriceps load were significantly elevated after combined sectioning of the PCL and the posterolateral complex.
In the present study, based on plain radiographs, seven knees had mild degenerative changes in the medial compartment, three knees had moderate degenerative changes in the medial compartment, and four knees had mild degenerative changes in the patellofemoral joint at a mean follow-up of 6.9 years. Moreover, 17 of the 20 knees (selected randomly from the database) had a normal radioisotope bone scan. We believe that this is an encouraging finding. A further long-term follow-up of the patients in our study is needed to comment on the prevalence of degenerative changes and symptoms in a PCL-deficient knee. Dejour et al. [30] have suggested that at least 15 to 20 years or even more may elapse between the presence of chondral lesions and the development of established OA of the knee. In our study, no correlation was noted between the degenerative changes as seen on plain radiographs and the length of follow-up (i.e., time interval from the initial PCL injury). Parolie and Bergfeld [6] and Torg et al. [25] have previously reported a similar finding. In our study, no correlation was seen between the radiographic findings and the grading of PCL laxity or the Lysholm-II knee score.
Our study has a few limitations. First, this is a retrospective study known to be associated with inherent selection bias. Second, the mean follow-up in this study is 6.9 years. It would be helpful to have a further longer-term data on our patient population. The strength of our study is that we have focused on the outcome of nonoperative management of a pure group of patients with acute, isolated PCL injury. Future research should include prospective, long-term, and controlled studies comparing the results of nonoperative treatment with the results of surgical reconstruction for isolated PCL injuries. Such efforts should help us in refining the current recommendations for the management of acute, isolated PCL-deficient knees. Until then, the findings of the nonoperative management of acute, isolated PCL deficiency would serve as a baseline against which the results of PCL reconstructive surgery can be compared.
Conclusion
We report the intermediate-term results of nonoperative treatment of acute, isolated (partial or complete), PCL-deficient knee. We present the clinical, radiographic, and functional results of 57 patients (58 knees) with acute, isolated PCL injuries that were followed at an average follow-up of 6.9 years (range 2 to 19.3 years). A clear differentiation between the isolated PCL injury and combined ligamentous injuries must be made to determine an appropriate treatment plan. We currently believe that patients with acute, isolated, complete PCL tears with up to 10 mm of posterior tibial translation (anterior border of tibial plateau flush with the anterior surface of the femoral condyles with the knee at 90° of flexion) can be treated nonoperatively and a satisfactory functional result can be obtained in majority of the patients at an intermediate-term follow-up. In the present study, no correlation was observed between the degree of PCL laxity and subjective knee function.
Acknowledgments
We thank Eva M. Anisko, BA for her help in collaborating the patient data and Margaret G. E. Peterson, PhD for statistical analysis of the data.
References
- 1.O’Donoghue DH (1959) Surgical treatment of injuries to ligaments of the knee. JAMA 169(13):1423–1431 [PubMed]
- 2.Clendenin MB, DeLee JC, Heckman JD (1980) Interstitial tears of the posterior cruciate ligament of the knee. Orthopedics 3:764–772 [DOI] [PubMed]
- 3.DeHaven KE (1980) Diagnosis of acute knee injuries with hemarthrosis. Am J Sports Med 8(1):9–14 [DOI] [PubMed]
- 4.Lysholm J, Gillquist J (1981) Arthroscopic examination of the posterior cruciate ligament. J Bone Joint Surg [Am] 63-A(3):363–366 [PubMed]
- 5.Hughston JC, Degenhardt TC (1982) Reconstruction of the posterior cruciate ligament. Clin Orthop Relat Res 164:59–77 [PubMed]
- 6.Parolie JM, Bergfeld JA (1986) Long-term results of nonoperative treatment of isolated posterior cruciate ligament injuries in the athlete. Am J Sports Med 14(1):35–38 [DOI] [PubMed]
- 7.Johnson JC, Bach BR Jr (1990) Posterior cruciate ligament [Current concepts review]. Am J Knee Surg 3:143–153
- 8.Fanelli GC, Giannotti BF, Edson CJ (1994) The posterior cruciate ligament arthroscopic evaluation and treatment [Current concepts review]. Arthroscopy 10(6):673–688 [DOI] [PubMed]
- 9.Schulz MS, Russe K, Weiler A, et al. (2003) Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg 123(4):186–191 [DOI] [PubMed]
- 10.Clancy WG Jr, Sutherland TB (1994) Combined posterior cruciate ligament injuries. Clin Sports Med 13(3):629–647 [PubMed]
- 11.Trickey EL (1968) Rupture of the posterior cruciate ligament of the knee. J Bone Joint Surg [Br] 50-B(2):334–341 [PubMed]
- 12.Cross MJ, Powell JF (1984) Long-term followup of posterior cruciate ligament rupture: a study of 116 cases. Am J Sports Med 12(4):292–297 [DOI] [PubMed]
- 13.Fowler PJ, Messieh SS (1987) Isolated posterior cruciate ligament injuries in athletes. Am J Sports Med 15(6):553–557 [DOI] [PubMed]
- 14.Kennedy JC, Grainger RW (1967) The posterior cruciate ligament. J Trauma 7(3):367–377 [DOI] [PubMed]
- 15.Hughston JC, Bowden JA, Andrews JR, et al. (1980) Acute tears of the posterior cruciate ligament. Results of operative treatment. J Bone Joint Surg [Am] 62-A(3):438–450 [PubMed]
- 16.Trickey EL (1980) Injuries to the posterior cruciate ligament: diagnosis and treatment of early injuries and reconstruction of late instability. Clin Orthop Relat Res 147:76–81 [PubMed]
- 17.Fleming RE Jr, Blatz DJ, McCarroll JR (1981) Posterior problems in the knee. Posterior cruciate insufficiency and posterolateral rotatory insufficiency. Am J Sports Med 9(2):107–113 [DOI] [PubMed]
- 18.Loos WC, Fox JM, Blazina ME, et al. (1981) Acute posterior cruciate ligament injuries. Am J Sports Med 9(2):86–92 [DOI] [PubMed]
- 19.Balkfors B (1982) The course of knee-ligament injuries. Acta Orthop Scand Suppl 198:1–99 [PubMed]
- 20.Dandy DJ, Pusey RJ (1982) The long-term results of unrepaired tears of the posterior cruciate ligament. J Bone Joint Surg [Br] 64-B(1):92–94 [DOI] [PubMed]
- 21.Bianchi M (1983) Acute tears of the posterior cruciate ligament: clinical study and results of operative treatment in 27 cases. Am J Sports Med 11(5):308–314 [DOI] [PubMed]
- 22.Clancy WG Jr, Shelbourne KD, Zoellner GB, et al. (1983) Treatment of knee joint instability secondary to rupture of the posterior cruciate ligament. Report of a new procedure. J Bone Joint Surg [Am] 65-A(3):310–322 [PubMed]
- 23.Satku K, Chew CN, Seow H (1984) Posterior cruciate ligament injuries. Acta Orthop Scand 55(1):26–29 [DOI] [PubMed]
- 24.Tibone JE, Antich TJ, Perry J, et al. (1988) Functional analysis of untreated and reconstructed posterior cruciate ligament injuries. Am J Sports Med 16(3):217–223 [DOI] [PubMed]
- 25.Torg JS, Barton TM, Pavlov H, et al. (1989) Natural history of the posterior cruciate ligament-deficient knee. Clin Orthop Relat Res 246:208–216 [PubMed]
- 26.Barrett GR, Savoie FH (1991) Operative management of acute PCL injuries with associated pathology: long-term results. Orthopedics 14(6):687–692 [DOI] [PubMed]
- 27.Whipple TL, Ellis FD (1991) Posterior cruciate ligament injuries. Clin Sports Med 10(3):515–527 [PubMed]
- 28.Flandry FC, Wolfe MW, Martino JA, et al. (1996) The natural history of the posterior cruciate ligament-deficient knee. Orthop Trans 20:7
- 29.Longenecker SL, Hughston JC (1987) Long-term follow-up of isolated posterior cruciate injuries. Am J Sports Med 15:628
- 30.Dejour H, Walch G, Peyrot J, et al. (1988) The natural history of rupture of the posterior cruciate ligament. Fr J Orthop Surg 2:112–120 [PubMed]
- 31.Keller PM, Shelbourne KD, McCarroll JR, et al. (1993) Nonoperatively treated isolated posterior cruciate ligament injuries. Am J Sports Med 21(1):132–136 [DOI] [PubMed]
- 32.Shino K, Horibe S, Nakata K, et al. (1995) Conservative treatment of isolated injuries to the posterior cruciate ligament in athletes. J Bone Joint Surg [Br] 77–B(6):895–900 [PubMed]
- 33.Boynton MD, Tietjens BR (1996) Long-term followup of the untreated isolated posterior cruciate ligament-deficient knee. Am J Sports Med 24(3):306–310 [DOI] [PubMed]
- 34.Shelbourne KD, Davis TJ, Patel DV (1999) The natural history of acute, isolated, non-operatively treated posterior cruciate ligament injuries. A prospective study. Am J Sports Med 27(3):276–283 [DOI] [PubMed]
- 35.Iwamoto J, Takeda T, Suda Y, et al. (2004) Conservative treatment of isolated posterior cruciate ligament injury in professional baseball players: a report of two cases. Knee 11(1):41–44 [DOI] [PubMed]
- 36.Toritsuka Y, Horibe S, Hiro-Oka A, et al. (2004) Conservative treatment for rugby football players with an acute isolated posterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc 12(2):110–114 [DOI] [PubMed]
- 37.Shelbourne KD, Muthukaruppan Y (2005) Subjective results of nonoperatively treated, acute, isolated posterior cruciate ligament injuries. Arthroscopy 21(4):457–461 [DOI] [PubMed]
- 38.Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49 [PubMed]
- 39.Hefti F, Müller W, Jakob RP, et al. (1993) Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc 1(3–4):226–234 [DOI] [PubMed]
- 40.Lysholm J, Gillquist J (1982) Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med 10(3):150–154 [DOI] [PubMed]
- 41.Odensten M, Lysholm J, Gillquist J (1983) Long-term follow-up study of a distal iliotibial band transfer (DIT) for anterolateral knee instability. Clin Orthop Relat Res 176:129–135 [PubMed]
- 42.Daniel DM, Stone ML, Barnett P, et al. (1988) Use of the quadriceps active test to diagnose posterior cruciate-ligament disruption and measure posterior laxity of the knee. J Bone Joint Surg [Am] 70-A(3):386–391 [PubMed]
- 43.Jakob RP, Hassler H, Stäubli H-U (1981) Observations on rotatory instability of the lateral compartment of the knee. Experimental studies on the functional anatomy and pathomechanism of the true and reversed pivot shift sign. Acta Orthop Scand Suppl 191:1–32 [DOI] [PubMed]
- 44.Noyes FR, Barber-Westin SD, Grood ES (2001) Newer concepts in the treatment of posterior cruciate ligament ruptures. In: Insall JN, Scott WN (eds) Surgery of the knee, 3rd edn. Churchill Livingstone, Philadelphia pp 850–852
- 45.MacGillivray JD, Shubin Stein BE, Park M, et al. (2006) Comparison of tibial inlay versus transtibial techniques for isolated posterior cruciate ligament reconstruction: minimum 2-year follow-up. Arthroscopy 22(3):320–328 [DOI] [PubMed]
- 46.Rosenberg TD, Paulos LE, Parker RD, et al. (1988) The forty-five-degree posteroanterior flexion weight-bearing radiograph of the knee. J Bone Joint Surg [Am] 70-A(10):1479–1483 [PubMed]
- 47.Merchant AC, Mercer RL, Jacobsen RH, et al. (1974) Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg [Am] 56-A(7):1391–1396 [PubMed]
- 48.Hughston JC, Norwood LA Jr (1980) The posterolateral drawer test and external rotational recurvatum test for posterolateral rotatory instability of the knee. Clin Orthop Relat Res 147:82–87 [PubMed]
- 49.Rubinstein RA Jr, Shelbourne KD, McCarroll JR, et al. (1994) The accuracy of the clinical examination in the setting of posterior cruciate ligament injuries. Am J Sports Med 22(4):550–557 [DOI] [PubMed]
- 50.Stäubli H-U, Jakob RP (1990) Posterior instability of the knee near extension. A clinical and stress radiographic analysis of acute injuries of the posterior cruciate ligament. J Bone Joint Surg [Br] 72-B(2):225–230 [DOI] [PubMed]
- 51.Hewett TE, Noyes FR, Lee MD (1997) Diagnosis of complete and partial posterior cruciate ligament ruptures. Stress radiography compared with KT-1000 arthrometer and posterior drawer testing. Am J Sports Med 25(5):648–655 [DOI] [PubMed]
- 52.Geissler WB, Whipple TL (1993) Intraarticular abnormalities in association with posterior cruciate ligament injuries. Am J Sports Med 21(6):846–849 [DOI] [PubMed]
- 53.Hamada M, Shino K, Mitsuoka T, et al. (2000) Chondral injury associated with acute isolated posterior cruciate ligament injury. Arthroscopy 16(1):59–63 [DOI] [PubMed]
- 54.Strobel MJ, Weiler A, Schulz MS, et al. (2003) Arthroscopic evaluation of articular cartilage lesions in posterior-cruciate-ligament-deficient knees. Arthroscopy 19(3):262–268 [DOI] [PubMed]
- 55.Skyhar MJ, Warren RF, Ortiz GJ, et al. (1993) The effects of sectioning of the posterior cruciate ligament and the posterolateral complex on the articular contact pressures within the knee. J Bone Joint Surg [Am] 75-A(5):694–699 [DOI] [PubMed]