Abstract
Treatment for idiopathic adhesive capsulitis or frozen shoulder of the shoulder is controversial. The hypothesis of the study is that intra-articular corticosteroid injection in the early stages of idiopathic adhesive capsulitis will lead to a razpid resolution of stiffness and symptoms. This is a retrospective cohort study of only patients with stage 1 or stage 2 adhesive capsulitis. The diagnosis was made by history and physical examination and only when other causes of pain and motion loss were eliminated. Stage 1 adhesive capsulitis was defined as significant improvement in pain and normalization of motion following intra-articular injection. Stage 2 included patients who had significant improvement in pain and partial improvement in motion following injection. Seven patients with stage 1 and 53 patients with stage 2 comprised the baseline cohort. The mean age was 52 years (range: 30 to 78); 46 patients were female and nine patients had diabetes mellitus. Patients completed a physical examination as well as a shoulder rating questionnaire for symptoms and disability. Criteria for resolution were defined as forward flexion and external rotation to within 15° of the contralateral side and internal rotation to within three spinal levels of the contralateral side. Forty-four of the patients out of 60 met the criteria for recovery at a mean of 6.7 months. The mode and median time to recovery was 3 months. The mean score at final follow-up for 41 patients using the shoulder-rating questionnaire of L’Insalata was 90 (range 52–100). The mean time to recovery for the stage 1 patients was 6 weeks (range: 2 weeks to 3 months), and it was 7 months for stage 2 patients (range: 2 weeks to 2 years). Glenohumeral corticosteroid injection for early adhesive capsulitis may have allowed patients to recover motion at a median time of 3 months. In many cases, the patients had improvement prior to the 3-month mark; however, that was the routine time for follow-up. Patients with stage 1 disease tended to resolve more rapidly than stage 2 patients. Prompt recognition of stage 1 and stage 2 idiopathic adhesive capsulitis and early injection of corticosteroid with local anesthesia may be both diagnostic and therapeutic.
Introduction
The treatment for idiopathic adhesive capsulitis or frozen shoulder of the shoulder remains controversial. Certain investigators have recommended “benign neglect,” based on the fact that the natural history of this condition has been purported to be self-resolving [22, 28]. Others have demonstrated that patients may not fully recover from the symptoms and disability of adhesive capsulitis, even with long-term follow-up [35]. Other treatment options documented in the literature include supervised physical rehabilitation [4, 6, 21, 30], nonsteroidal anti-inflammatory medications [16, 29], oral corticosteroid [3], intra-articular corticosteroid injection [6, 8, 9, 36], distension arthrography [18], closed manipulation [2, 12, 15, 20, 26], open surgical release, and arthroscopic capsular release [26, 27, 31, 34]. While surgery has been demonstrated to shorten the natural history of this condition [26], the complications associated with surgery and anesthesia are important considerations.
The rationale for glenohumeral joint corticosteroid injection is to attempt to reduce synovial inflammation to decrease capsular fibrosis and allow improvement of motion with a decreased time to functional recovery. We hypothesized that the use of intra-articular corticosteroid for stage 1 and 2 idiopathic adhesive capsulitis will lead to resolution of stiffness and symptoms.
Methods
All patients presenting to a single orthopedic surgeon (JAH) with stage 1 and stage 2 idiopathic adhesive capsulitis were identified over a 6-year period. Patients were identified by ICD-9 code 726.0 from the office records. The treating physician coded all cases that were believed to be idiopathic adhesive capsulitis 726.0 during the study period. The diagnosis of adhesive capsulitis was made based on history and clinical exam and confirmed by a non-image guided intra-articular injection (see below). This diagnosis was made when there was pain with loss of motion compared to the contralateral shoulder (including loss of ER in all cases) and only when other causes of pain and motion loss were eliminated [23–25, 32] Rotator cuff tendinopathy was eliminated based on physical findings, including normal strength and lack of impingement signs. Glenohumeral osteoarthritis and neoplasm were excluded by radiographs. Pain related to the acromioclavicular joint or biceps was ruled out based on lack of tenderness with palpation of these structures. MRI was not obtained routinely as adhesive capsulitis is a clinical diagnosis and we did not feel that the use of MRI was indicated on clinical grounds. Institutional review board approval was granted and informed consent was obtained for all patients.
This injection of corticosteroid and local anesthesia was used both to confirm the diagosis and stage and for therapeutic treatment. The patients were instructed in simple pendulum exercises and reexamined 15 min following the injection to evaluate pain, determine passive glenohumeral range of motion (ROM), and define the stage of adhesive capsulitis. If the patient had significant improvement in pain and normalization of motion within 30 min after the injection, this confirmed the diagnosis of stage 1 adhesive capsulitis. If the patient had a significant improvement in pain with partial improvement in ROM, a diagnosis of stage 2 adhesive capsulitis was made. Anti-inflamatory medication was recommended and patients were referred for out-patient physical therapy.
The physical examination included both an evaluation of the cervical spine and the shoulder. All patients had pain on palpation of the anterior and posterior capsule and pain that was exacerbated by ROM of the arm. Range of motion measurements, including active and passive forward flexion, abduction, internal rotation (measured by having the patient place the thumb to the highest possible spinous process), and external rotation in neutral abduction, were measured and recorded with the patient standing. On physical examination, all patients had a restriction of motion, including a lack of external rotation compared to the contralateral side in each case.
All patients had routine radiographic evaluation including anteroposterior views in internal and external rotation, axillary and outlet views to rule out glenohumeral arthritis, calcific tendinitis, a superiorly migrated humeral head, or other processes. Radiographs were negative in the patients described herein with the exception of evidence of disuse osteopenia. Patients with radiographic abnormalities or a history of preexisting shoulder pathology were excluded.
All patients presenting with a preliminary clinical diagnosis of stage 1 or stage 2 adhesive capsulitis based on the criteria described above were treated with an intra-articular injection of local anesthetic and corticosteroid. The glenohumeral joint was injected via a posterior approach using traditional posterior arthroscopic portal landmarks utilizing a 20-gauge spinal needle. The skin was lightly anesthetized using ethyl chloride spray and the needle was advanced until the capsule was penetrated. The solution injected contained 5 cm3 of 1% lidocaine, 3 cm3 of 0.25% marcaine, and 80 mg depomedrol (2 cm3). All patients received only one injection. Fluoroscopy was not used as the physician had extensive experience in shoulder surgery and arthroscopy.
Seven patients with stage 1 and 53 with stage 2 comprised our cohort at baseline. The mean age was 52 years (range: 30 to 78). Forty-six patients were female and 14 male. Nine patients had diabetes mellitus. Patients completed a shoulder rating questionnaire to measure symptoms and disability at final follow-up [19]. Detailed ROM assessments were performed preinjection, postinjection, and at all subsequent visits by the treating surgeon (JAH). Range of motion was measured by the physician without the use of a goniometer. This information was accessed by chart review.
In addition to the chart review, patients were contacted for final ROM assessments by a single independent examiner (RWM). The exact time to recovery of motion is difficult to determine because patient follow-up visits are usually at least 6 weeks apart and motion may be limited in one plane but not another. Therefore, it was determined a priori that patients who had regained motion to within 15° of the contralateral side in both forward flexion and external rotation as well as internal rotation to within three spinal levels of the contralateral side were considered recovered. It was felt that this amount of motion limitation was acceptable following treatment for this condition and that it would not cause functional limitations for the patients.
Results
Forty-four of the 60 patients studied met the criteria for recovery at a mean of 6.7 months. The mode and median time to recovery was 3 months. The mean score at final follow-up for 41 patients using a validated shoulder scale (shoulder rating questionnaire of L’Insalata et al. [19]) was 90 (range: 52 to 100). Nineteen patients did not complete the follow-up questionnaire because of unavailability. One patient who was stage 1 and six patients who were stage 2 were lost to follow up and had not resolved at 2 weeks and a mean of 2.6 months following the injection, respectively. This is a total of seven patients who were lost early to follow up prior to resolution, for a total follow up rate of 88% (53/60).
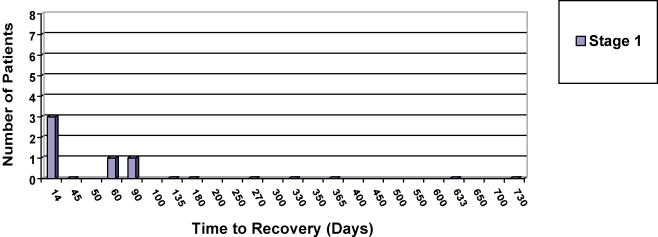
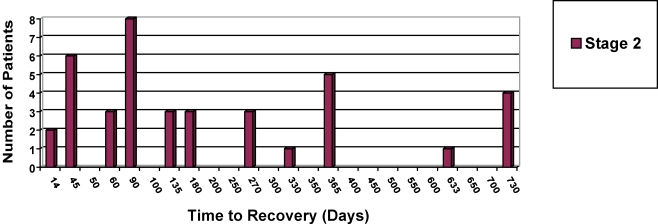
The mean time to recovery for stage 1 patients was 6 weeks (range: 2 weeks to 3 months) and 7 months for stage 2 patients (range: 2 weeks to 2 years). The mean time to recovery for the stage 2 group was affected by four patients who were not documented to have met the criteria for recovery until the 2-year mark (see Figs. 1 and 2). Fifteen patients met the criteria at 2 months or less.
Fig. 1.
Time from injection to recovery in days (stage 1). Recovery = maximum loss of 15° in external rotation and forward flexion or a maximum loss of internal rotation of three spinal levels, compared to the contralateral side
Fig. 2.
Time from injection to recovery in days (stage 2). Recovery = maximum loss of 15° in external rotation and forward flexion or a maximum loss of internal rotation of three spinal levels, compared to the contralateral side
Sixteen patients did not meet the criteria for recovery, and of those, seven underwent surgery for continuing pain and stiffness. The surgery was performed at a mean of 5.2 months postinjection (range: 1 to 10 months). These patients are discussed in greater detail below.
The duration of symptoms prior to injection and the time to recovery were found to be related, although this association was not statistically significant (Pearson r = 0.19; p = 0.23). In the group of patients successfully treated with intra-articular injection, the stage 1 patients recovered more rapidly than the stage 2 patients (mean of 38 days for stage 1 and 222 days for stage 2, p = 0.006; Mann–Whitney U test).
Two stage 1 patients were not followed to recovery. One lacked 20° of external rotation at 2 weeks postinjection prior to being lost to follow-up. The other lacked 30° of external rotation at 2 months, which persisted at the 3-year follow-up exam. Six stage 2 patients did not return for physical examination to determine whether they had recovered. These patients’ final physical examination prior to being lost to follow-up was at a mean of 2.6 months (range 0–4.5 months). One stage 2 patient was considered to have not recovered at 6 months following the injection due to the termination of the study period.
Nine patients in this cohort had diabetes mellitus. All were stage 2 at presentation. Five recovered following the injection at a mean of 9 months (range: 1.5 months to 2 years). Four went on to have surgery at a mean of 5.8 months postinjection (range: 1 to 10 months). Three of the patients who underwent surgery had significant remaining motion loss at final follow-up (although two had relatively high scores on the shoulder rating scale, 83 and 94, respectively). The fourth was lost to follow-up.
Three nondiabetic patients underwent arthroscopic capsular release at a mean of 3.2 months postinjection (range 1.5 to 5 months). One patient recovered forward flexion and external rotation to within the parameters of recovery specified by the study, although they lacked eight spinal levels of internal rotation. The second had significant ongoing motion loss at 5 years postoperatively; however, their shoulder rating score was 97. The third recovered full ROM.
Discussion
Neviaser and Neviaser initially described a staging system for adhesive capsulitis [25]. Their four stages ranged from synovial inflammation with limited motion to adhesive synovitis, to more mature adhesions with less synovitis, and finally to mature adhesions with limited motion. Subsequently, Hannafin et al. correlated clinical, arthroscopic, and histological findings to further refine the definition of the first three stages previously described [13]. In stage 1, the patient presents with pain and limited motion. In this first stage, full ROM is obtained on examination under anesthesia. Pathologic analysis reveals an inflammatory synovitis with normal underlying capsule. The second stage involved pain with limited ROM, which is not restored on exam under anesthesia. The pathology revealed synovial hyperplasia and capsular fibroplasia and fibrosis. The third stage is characterized by mild pain with marked loss of motion, minimal synovitis, and capsular fibroplasia with dense capsular scar formation. The fourth stage, or “thawing phase,” is unchanged from the description of Nevaiser.
To formulate a logical and scientific approach to the treatment of patients with adhesive capsulitis, it is necessary to understand the pathophysiology of this disease. A review of the literature reveals a multitude of strategies for treatment of patients with adhesive capsulitis, with extremely variable results. The lack of consistency in the published literature reflects a lack of understanding of the stages of adhesive capsulitis, which play a significant role both in diagnosis and in formulation of a treatment plan.
Conventional orthopedic wisdom is that nonoperative treatment of this condition will lead to recovery if the patients are followed over a long enough period of time. However, one long-term follow-up study demonstrated that at a minimum 3-year follow-up, 50% of patients reported pain or stiffness or both [35]. The mean time to recovery in this study was 12 months.
Other investigators studied the value of a home program for adhesive capsulitis and assessed improvement in shoulder function. They followed patients for a mean of 25 months, with a minimum of 6 months [28]. The investigators found that a statistically significant improvement in a shoulder rating scale (the simple shoulder test), as well as the physical function, role physical and bodily pain subscales of the SF-36. They concluded that the home program leads to improved self-assessed shoulder function. However, only 56% were able to place an 8-lb weight on a shelf, and only 66% were able to carry 20 lb at their side.
Others have studied the effects of arthroscopic debridement and release for this condition. While arthroscopic surgery has been shown to improve symptoms in these patients, the risks of complication and the recovery period associated with surgery make this treatment less desirable [26, 31, 38, 39].
These data and others present in the literature support the hypothesis that adhesive capsulitis is both an inflammatory and a fibrotic condition [7, 8, 11, 21, 33]. The hypervascular synovitis present in the early stages results in subsequent fibrosis of the subsynovium and capsule. Cytokines have been implicated in the inflammation and fibrosis described in adhesive capsulitis. Cytokines are also involved in the initiation and termination of repair processes in multiple musculoskeletal tissues, and their sustained production has been shown to result in tissue fibrosis [1, 5]. Rodeo et al. [33] reported an increase in transforming growth factor-β, platelet-derived growth factor, and hepatocyte growth factor staining in capsular biopsy specimens of patients with primary and secondary adhesive capsulitis and proposed that these cytokines are involved in the inflammatory and fibrotic cascades seen in adhesive capsulitis. A potential role of matrix metalloproteases, enzymes involved in extracellular matrix remodeling, in adhesive capsulitis has recently been described. In a series of 12 patients with inoperable gastric cancer treated with a synthetic matrix metalloproteinase inhibitor, six developed a frozen shoulder or a Dupuytren’s-like condition [17].
We hypothesized in this study that early treatment with intra-articular corticosteroid provides a chemical ablation of the synovitis, thus limiting the subsequent development of fibrosis and shortening the natural history of the disease. The self-limiting nature of adhesive capsulitis also supports the role of the synovium in initiation and regulation of the fibrotic process in the capsule. With resolution of the synovitis and termination of capsular scar formation, capsular remodeling and recovery of ROM occurs. This hypothesis is supported by the orthopedic and rheumatalogic literature [7, 33].
Van der Windt et al. compared glenohumeral injection of corticosteroid to 6 weeks of physical therapy for patients with “painful stiff shoulders.” It is unclear how many of these patients truly had adhesive capsulitis. They found significant improvements in pain, disability, and motion in the injection group at 3 and 7 weeks [37]. Response to intra-articular steroid was not related to stage of disease. However, at 26 and 52 weeks there was minimal or no difference between the two groups.
Gam et al. treated patients with adhesive capsulitis with either steroid injection or steroid injection and distension with 19 cm3 of Lidocane. They found that the distension with steroid group (12 patients) used fewer analgesics and had improved motion compared to the steroid-only group (eight patients). However, the visual analog pain scores for the groups were similar [10]. Again, the duration of symptoms and stage of adhesive capsulitis was not correlated with response to treatment. Bulgen et al. [6] randomized patients to treatment with steroid, physical therapy, ice, or benign neglect. The initial positive response to treatment was most marked in patients treated with steroid; however, no significant difference in final long-term outcome was reported when treatment groups were compared.
Hazleman [14] summarized numerous studies on the use of intra-articular corticosteroid and reported that success of treatment is dependent on the duration of symptoms. Patients treated within 1 month of onset of symptoms recovered in an average of 1.5 months. Patients treated within 2 to 5 months of onset of symptoms recovered in 8.1 months; patients treated 6 to 12 months after onset of symptoms required an average of 14 months for full recovery.
In this retrospective cohort study of glenohumeral corticosteroid injection for early adhesive capsulitis, we found that patients’ motion loss recovered at a median time of 3 months. In many cases, the patients had improved prior to the 3-month mark; however, that was the routine time point for follow-up. Patients with stage 1 disease tended to resolve more rapidly than the stage 2 patients, although the sample size was small (only seven patients with stage 1 were studied). Previous basic science work indicated that, early in the course of adhesive capsulitis, synovitis is present without capsular fibrosis [13]. In this setting, early chemical ablation of the synovitis would result in decreased scar formation in the capsule and potentially improved ROM.
The duration of symptoms prior to injection was related to the time to recovery, although this relationship was not statistically significant. This association would also be supported by the basic science research, as a prolonged symptomatic time period would allow for greater capsular fibrosis, which would then lead to a longer time to recovery. Patients with diabetes mellitus responded less well to corticosteroid injection, as the time to recovery was longer in five patients (mean 9 months; range 1.5 months to 2 years) and four others required arthroscopic release. Three of the four were left with significant motion loss and the fourth was lost to follow-up. Of three nondiabetic patients to undergo arthroscopic capsular release, only one regained full motion.
There are several weaknesses in this study. There was no control group, as the senior author did not feel it was ethically acceptable to not offer corticosteroid injection to patients with stage 1 or stage 2 adhesive capsulitis. While we believe that the stage of a given patient is relatively clear, it is possible that the interobserver reliability among surgeons for staging adhesive capsulitis might be low. To minimize this, it is essential to measure ROM prior to, and following, glenohumeral injection. It is possible some patients may have been excluded due to lack of response to injection, either because the injection was extra-articular or because it was intra-articular but the patient did not experience an improvement in their pain. This limits the generalizability of the study. Evaluation of ROM 15 min following injection allows the physician to assess motion loss secondary to capsular fibrosis, in contrast to motion loss preinjection, which can be caused by both pain and fibrosis.
It is difficult to define recovery for this condition. We elected to use recovery of ROM as our outcome. Range of motion is a continuous variable, with multiple follow-up measures in several planes of motion. For ease of interpretability, we converted recovery of range of motion to a binary variable (i.e., recovery or no recovery). While the recovery criteria were defined a priori based on what was felt to constitute a clinically relevant end-point, there is no standard available to determine recovery. During the study period, we attempted to evaluate ROM at 6-week intervals; however, not all patients returned for follow-up at these intervals and many had recovered at some point between evaluations. Therefore, some of the documented time intervals to recovery were longer than the true time to recovery because patients were only examined at specific time points. Additionally, patients did not present for follow-up at each time point, which also tended to increase the reported vs actual duration of time to recovery.
Another limitation of this research is that it is impossible to know with certainty that all injections were indeed intra-articular. It is common and routine practice for experienced shoulder surgeons at our institution to inject the glenohumeral joint without radiographic assistance. Therefore, the results are generalizeable to this type of practice. Lastly, surgery was defined as an end-point for certain patients in this study. The decision to have surgery is of course subjective; however, this is always the case, to varying degrees, with elective surgery.
In summary, corticosteroid injection in the early stages of adhesive capsulitis allows the patient to regain motion prior to developing severe fibrosis in many cases. Patients who were treated in stage 1 recovered more rapidly than those in stage 2. However, few patients were seen in stage 1 due to delays related to referral patterns. Prompt recognition of stage 1 and stage 2 idiopathic adhesive capsulitis and early injection of corticosteroid and local anesthesia are both diagnostic and therapeutic.
Footnotes
This project was funded by philanthropic support of Marcia Kapp.
References
- 1.Alman B, Greel D, Ruby L, Al E (1995) Regulation of growth and platelet-derived growth factor expression in palmar fibromatosis (Dupuytren’s disease) by mechanical strain. In: Trans Combined ORS Meeting [DOI] [PubMed]
- 2.Andersen NH, Sojbjerg JO, Johannsen HV, Sneppen O (1998) Frozen shoulder: arthroscopy and manipulation under general anesthesia and early passive motion. J Shoulder Elbow Surg 7(3):218–222 [DOI] [PubMed]
- 3.Binder AI, Bulgen DY, Hazleman BL, Roberts S (1984) Frozen shoulder: a long-term prospective study. Ann Rheum Dis 43(3):361–364 [DOI] [PMC free article] [PubMed]
- 4.Binder A, Hazleman BL, Parr G, Roberts S (1986) A controlled study of oral prednisolone in frozen shoulder. Br J Rheumatol 25(3):288–292 [DOI] [PubMed]
- 5.Border WA, Noble NA (1994) Transforming growth factor beta in tissue fibrosis. N Engl J Med 331(19):1286–1292 [DOI] [PubMed]
- 6.Bulgen DY, Binder AI, Hazleman BL, Dutton J, Roberts S (1984) Frozen shoulder: prospective clinical study with an evaluation of three treatment regimens. Ann Rheum Dis 43(3):353–360 [DOI] [PMC free article] [PubMed]
- 7.Bunker TD, Anthony PP (1995) The pathology of frozen shoulder. A Dupuytren-like disease. J Bone Joint Surg Br 77(5):677–683 [PubMed]
- 8.Dacre JE, Beeney N, Scott DL (1989) Injections and physiotherapy for the painful stiff shoulder. Ann Rheum Dis 48(4):322–325 [DOI] [PMC free article] [PubMed]
- 9.de Jong BA, Dahmen R, Hogeweg JA, Marti RK (1998) Intra-articular triamcinolone acetonide injection in patients with capsulitis of the shoulder: a comparative study of two dose regimens. Clin Rehabil 12(3):211–215 [DOI] [PubMed]
- 10.Gam AN, Schydlowsky P, Rossel I, Remvig L, Jensen EM (1998) Treatment of “frozen shoulder” with distension and glucorticoid compared with glucorticoid alone, a randomized controlled trial. Scand J Rheumatol 27:425–430 [DOI] [PubMed]
- 11.Grubbs N (1993) Frozen shoulder syndrome: a review of literature. J Orthop Sports Phys Ther 18(3):479–487 [DOI] [PubMed]
- 12.Haines JF, Hargadon EJ (1982) Manipulation as the primary treatment of the frozen shoulder. J R Coll Surg Edinb 27(5):271–275 [PubMed]
- 13.Hannafin JA, DiCarlo EF, Wickiewicz TL, Warren RF (1994) Adhesive capsulitis: capsular fibroplasia of the glenohumeral joint. J Shoulder Elbow Surg 3(Suppl 1):5
- 14.Hazleman BL (1972) The painful stiff shoulder. Rheumatol Phys Med 11(8):413–421 [DOI] [PubMed]
- 15.Helbig B, Wagner P, Dohler R (1983) Mobilization of frozen shoulder under general anaesthesia. Acta Orthop Belg 49(1–2):267–274 [PubMed]
- 16.Huskisson EC, Bryans R (1983) Diclofenac sodium in the treatment of painful stiff shoulder. Curr Med Res Opin 8(5):350–353 [DOI] [PubMed]
- 17.Hutchinson JW, Tierney GM, Parsons SL, Davis TR (1998) Dupuytren’s disease and frozen shoulder induced by treatment with a matrix metalloproteinase inhibitor. J Bone Joint Surg 80-B(5):907–908 [DOI] [PubMed]
- 18.Laroche M, Ighilahriz O, Moulinier L, Constantin A, Cantagrel A, Mazieres B (1998) Adhesive capsulitis of the shoulder: an open study of 40 cases treated by joint distention during arthrography followed by an intraarticular corticosteroid injection and immediate physical therapy. Rev Rhum Engl Ed 65(5):313–319 [PubMed]
- 19.L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG (1997) A self-administered questionnaire for assessment of symptoms and function of the shoulder. J Bone Joint Surg Am 79(5):738–748 [DOI] [PubMed]
- 20.Lundberg BJ (1969) The frozen shoulder. Clinical and radiographical observations. The effect of manipulation under general anesthesia. Structure and glycosaminoglycan content of the joint capsule. Local bone metabolism. Acta Orthop Scand Suppl 119:1–59 [PubMed]
- 21.Mao CY, Jaw WC, Cheng HC (1997) Frozen shoulder: correlation between the response to physical therapy and follow-up shoulder arthrography. Arch Phys Med Rehabil 78(8):857–859 [DOI] [PubMed]
- 22.Miller MD, Wirth MA, Rockwood CA Jr (1996) Thawing the frozen shoulder: the “patient” patient. Orthopedics 19(10):849–853 [DOI] [PubMed]
- 23.Neviaser JS (1980) Adhesive capsulitis and the stiff and painful shoulder. Orthop Clin North Am 11(2):327–331 [PubMed]
- 24.Neviaser RJ (1983) Painful conditions affecting the shoulder. Clin Orthop 173:63–69 [PubMed]
- 25.Neviaser RJ, Neviaser TJ (1987) The frozen shoulder. Diagnosis and management. Clin Orthop 223:59–64 [PubMed]
- 26.Ogilvie-Harris DJ, Myerthall S (1997) The diabetic frozen shoulder: arthroscopic release. Arthroscopy 13(1):1–8 [DOI] [PubMed]
- 27.Ogilvie-Harris DJ, Biggs DJ, Fitsialos DP, MacKay M (1995) The resistant frozen shoulder. Manipulation versus arthroscopic release. Clin Orthop 319:238–248 [PubMed]
- 28.O’Kane JW, Jackins S, Sidles JA, Smith KL, Matsen FA III (1999) Simple home program for frozen shoulder to improve patients’ assessment of shoulder function and health status. J Am Board Fam Pract 12(4):270–277 [DOI] [PubMed]
- 29.Owens-Burkhart H (1991) Management of frozen shoulder. In: Donatelli R (ed) Physical therapy of the shoulder. Churchill Livingstone, New York, pp 91–116
- 30.Placzek JD, Roubal PJ, Freeman DC, Kulig K, Nasser S, Pagett BT (1998) Long-term effectiveness of translational manipulation for adhesive capsulitis. Clin Orthop 356:181–191 [DOI] [PubMed]
- 31.Pollock RG, Duralde XA, Flatow EL, Bigliani LU (1994) The use of arthroscopy in the treatment of resistant frozen shoulder. Clin Orthop 304:30–36 [PubMed]
- 32.Reeves B (1975) The natural history of the frozen shoulder syndrome. Scand J Rheumatol 4(4):193–196 [DOI] [PubMed]
- 33.Rodeo SA, Hannafin JA, Tom J, Warren RF, Wickiewicz TL (1997) Immunolocalization of cytokines and their receptors in adhesive capsulitis of the shoulder. J Orthop Res 15(3):427–436 [DOI] [PubMed]
- 34.Segmuller HE, Taylor DE, Hogan CS, Saies AD, Hayes MG (1995) Arthroscopic treatment of adhesive capsulitis. J Shoulder Elbow Surg 4(6):403–408 [DOI] [PubMed]
- 35.Shaffer B, Tibone JE, Kerlan RK (1992) Frozen shoulder. A long-term follow-up. J Bone Joint Surg Am 74(5):738–746 [PubMed]
- 36.Steinbrocker O, Argyros TG (1974) Frozen shoulder: treatment by local injections of depot corticosteroids. Arch Phys Med Rehabil 55(5):209–213 [PubMed]
- 37.van der Windt DAWM, Koes BW, Deville W, Boeke AJP, de Jong BA, Bouter LM (1998) Effectiveness of corticosteroid injections versus physiotherapy for treatment of painful stiff shoulder in primary care. BMJ 317:1292–1296 [DOI] [PMC free article] [PubMed]
- 38.Warner JJ, Allen A, Marks PH, Wong P (1996) Arthroscopic release for chronic, refractory adhesive capsulitis of the shoulder. J Bone Joint Surg Am 78(12):1808–1816 [DOI] [PubMed]
- 39.Zuckerman JD, Cuomo F (1993) Frozen shoulder. In: Matsen FA, Fu FH, Hawkins RJ (eds) The shoulder: a balance of mobility and stability. American Academy of Orthopaedic Surgeons, Rosemont