Introduction
Insomnia is the most common sleep disorder affecting millions of people as either a primary or comorbid condition. Insomnia has been defined as both a symptom and a disorder, and this distinction may affect its conceptualization from both research and clinical perspectives. However, whether insomnia is viewed as a symptom or a disorder, it nevertheless has a profound effect on the individual and society. The burden of medical, psychiatric, interpersonal, and societal consequences that can be attributed to insomnia underscores the importance of understanding, diagnosing, and treating the disorder.
Insomnia Prevalence
The prevalence of insomnia varies depending on the specific case definition. Broadly speaking, insomnia has been viewed as a symptom and as a disorder in its own right. Insomnia has also been defined by subtypes based on frequency, duration (acute versus chronic) and etiology. This picture is further complicated by considerations of insomnia as either a comorbid condition; as a symptom of a larger sleep, medical, or psychiatric disorder; or as a secondary disorder (Harvey, 2001). An illustration of this idea is the overlap between insomnia and depression. Do insomnia and depression co-exist in an individual as separate disorders? Or is insomnia only one symptom in the larger context of depression? Or did insomnia secondarily developed as a distinct disorder from a primary depressive disorder?
The three main diagnostic manuals, International Classification of Sleep Disorders (ICSD-2) (American Academy of Sleep Medicine, 2005), Diagnostic and Statistic Manual (DSM IV-TR) (American Psychiatric Association, 2000), and International Classification of Disease (ICD-10) (World Health Organization, 1992), vary in their approach to defining insomnia (see Table 1). ICSD-2 subdivides insomnia into descriptive, etiologic categories. Examples include Adjustment Insomnia (or, insomnia temporally related to an identifiable stressor) and Psychophysiological Insomnia (increased arousal and conditioned sleep difficulty) (American Academy of Sleep Medicine, 2005; see Table 2). These categories also contain insomnia due to a mental disorder, substance, or medical condition. The DSM IV-TR, on the other hand, separates out Primary Insomnia (insomnia symptoms associated with distress or daytime impairment) from other “dyssomnias,” such as a breathing-related sleep disorder (American Psychiatric Association, 2000). ICD-10 utilizes the broadest approach, categorizing insomnia based on underlying pathology: nonorganic insomnia and nonorganic disorder of the sleep-wake schedule (World Health Organization, 1992) (see Table 2) [This version of table 2 contains only the ICSD definition of insomnia]. Duration of insomnia (at least 1 month of symptoms) is noted in ICSD-2 and DSM IV-TR; however frequency of symptoms is broached only in ICD-10 [please define insomnia according to ICD and DSM].
Table 1.
Insomnia Diagnostic Categories
| ICSD-2 Insomnia Categories: |
| Adjustment insomnia (acute insomnia) |
| Psychophysiological insomnia |
| Paradoxical insomnia |
| Idiopathic insomnia |
| Insomnia due to mental disorder |
| Inadequate sleep hygiene |
| Behavioral insomnia of childhood |
| Insomnia due to drug or substance |
| Insomnia due to medical condition |
| Insomnia not due to substance or known |
| physiological conditions, unspecified |
| (Nonorganic insomnia NOS) |
| Physiological (organic) insomnia, unspecified |
| ICD-10 Insomnia Categories: |
| Nonorganic insomnia |
| Nonorganic disorder of the sleep-wake schedule |
| DSM-IV-TR Insomnia Categories: |
| Primary insomnia |
| Insomnia related to [Axis I or II category] |
Table 2.
Insomnia Definition
| ICSD-2 General Criteria for Insomnia: |
| 1. A complaint of difficulty initiating sleep, difficulty maintaining sleep, or waking up too early or sleep that is chronically unrestorative or poor in quality. In children, the sleep difficulty is often reported by the caretaker and may consist of observed bedtime resistance or inability to sleep independently. |
| 2. The above sleep difficulty occurs despite adequate opportunity and circumstances for sleep. |
| 3. At least one of the following forms of daytime impairment related to the nighttime sleep difficulty is reported by the patient: fatigue or malaise; attention, concentration, or memory impairment; social or vocational dysfunction or poor school performance; mood disturbance or irritability; daytime sleepiness; motivation, energy, or initiative reduction; proneness for errors or accidents at work or while driving; tension, headaches, or gastrointestinal symptoms in response to sleep loss; concerns or worries about sleep. |
| DSM-IV-TR Criteria for Primary Insomnia: |
| 1. The predominant complaint is difficulty initiating or maintaining sleep, or nonrestorative sleep, for at least 1 month. 2. The sleep disturbance (or associated daytime fatigue) causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. |
| 3. The sleep disturbance does not occur exclusively during the course of Narcolepsy, Breathing-Related Sleep Disorder, Circadian Rhythm Sleep Disorder, or a Parasomnia. |
| 4. The disturbance does not occur exclusively during the course of another mental disorder (e.g., Major Depressive Disorder, Generalized Anxiety Disorder, a delirium). |
| 5. The disturbance is not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication) or a general medical condition. |
| ICD-10 Criteria for Nonorganic Insomnia: |
| A condition of unsatisfactory quantity and/or quality of sleep, which persists for a considerable period of time, including difficulty falling asleep, difficulty staying asleep, or early final wakening. Insomnia is a common symptom of many mental and physical disorders, and should be classified here in addition to the basic disorder only if it dominates the clinical picture. |
As a result of these differences in insomnia case definitions, estimates of insomnia prevalence have varied widely, from 10–40% (Ford & Kamerow, 1989; Kuppermann et al., 1995; Ustun et al., 1996; Bixler et al., 1979; Simon & Von Korff, 1997; Mellinger et al., 1985; Ohayon, 2002; Ancoli-Israel & Roth, 1999). This problem is demonstrated by the findings of a prevalence study from South Korea. When insomnia was defined by frequency (symptoms occurring at least three nights per week), 17% of randomly selected subjects from the population qualified for the diagnosis. If the symptom of difficulty maintaining sleep was the defining factor, 11.5% of the sample was affected. However, using the more stringent criteria from DSM-IV, 5% of the sample qualified for the diagnosis (Ohayon & Hong, 2002). Similar disparities were shown in a prevalence study from France (Leger et al., 2000). According to a 2005 statement by the National Institutes of Health, insomnia has a prevalence of 10% if the definition necessitates daytime distress or impairment (National Institutes of Health, 2005).
Given all the information available, the prevalence of insomnia symptoms may be estimated at 30% and specific insomnia disorders at 5–10% (Roth, 2007).
Several risk factors for insomnia have been identified. Female sex, advanced age, depressed mood, snoring, low levels of physical activity, comorbid medical conditions, nocturnal micturation, regular hypnotic use, onset of menses, previous insomnia complaints, and high level of perceived stress have all been implicated as risk factors; the first three factors in particular, female sex, advanced age, and depressed mood, are consistent risk factors (Morgan, 2003; Klink et al., 1992; Morgan & Clarke, 1997; Su et al., 2004; Johnson et al., 2006b; Ford & Kamerow, 1989; Murata et al., 2007).
Precipitants of insomnia have also been studied. Bastien et al. (Bastien et al., 2004) examined precipitating factors of insomnia and found that family, work or school, and health events proved to be the most common precipitants (Bastien et al., 2004). Another study of psychosocial stressors in Japan demonstrated that employees with greater intragroup conflict and job dissatisfaction had greater risk for insomnia (Nakata et al., 2004).
Knowledge of both risk factors and possible precipitants of insomnia can help to guide the evaluation and treatment of insomnia. Questions about psychosocial stressors at home and at work in high risk individuals, such as those experiencing depression or who are female or elderly, can help to shape and direct patient care.
Insomnia Impact
Insomnia and Psychiatric Conditions
An estimated 40% of individuals with insomnia have a comorbid psychiatric condition (Ford & Kamerow, 1989; McCall, 2001). In a review of epidemiological studies, Taylor et al. (Taylor et al., 2003) found that insomnia predicted depression, anxiety, substance abuse or dependence, and suicide (Taylor et al., 2003). In fact, the correlation between insomnia and later development of depression within 1–3 years is particularly strong (Riemann & Voderholzer, 2003). Johnson et al. (Johnson et al., 2006a) found that in a community sample of adolescents that in 69% of cases, insomnia preceded comorbid depression, while an anxiety disorder preceded insomnia 73% of the time (Johnson et al., 2006a). In a large group of subjects aged 15 to 100 years, insomnia either appeared before (>40%) or at the same time (>22%) as mood disorders. This study also found that insomnia appeared at the same time (>38%) of the time or after (34%) as anxiety disorders (Ohayon & Roth, 2003).
As further evidence of morbidity, individuals with insomnia complaints in the last year but without any previous psychiatric history were shown to have an increased risk of first onset major depression, panic disorder, and alcohol abuse the following year when compared to controls (Weissman et al., 1997). Furthermore, adolescents who completed suicide were found to have higher rates of insomnia in the week preceding death than community control adolescents (Goldstein et al., 2008).
Taken as a whole, these findings underscore the impact of insomnia on the individual while suggesting a possible relationship between insomnia and psychiatric disorders. The nature of this relationship has yet to be established. Insomnia could be an early symptom, part of a prodrome, of a depressive or anxiety disorder. Similarly, insomnia might also exist as a separate, comorbid disorder that either gave rise to or developed from a psychiatric condition. In either case the need to address insomnia and psychiatric disorders together remains important.
Insomnia and Medical Conditions
Associations between insomnia and a variety of medical conditions have also been established. Taylor et al. (Taylor et al., 2007) found that in a community-based sample chronic insomniacs reported more heart disease, hypertension, chronic pain, as well as increased gastrointestinal, neurologic, urinary, and breathing difficulties. The converse was also shown to be true, in which subjects with hypertension, chronic pain, breathing, gastrointestinal, and urinary problems complained of insomnia more often than non-insomniacs (Taylor et al., 2007). Others have also found increased odds ratios for insomnia in a variety of medical conditions, ranging from congestive heart failure to hip impairment (Katz & McHorney, 1998).
Ancoli-Israel (Ancoli-Israel, 2006) emphasized the different ways that insomnia and chronic medical conditions may relate to each other: sleep complaints may function as a symptom of a disorder, such as congestive heart failure and Cheyne-Stokes respiration gastroesophageal reflux disease and increased arousals. In other cases, insomnia may be a component of the etiology of a disorder, such as diabetes mellitus (Ancoli-Israel, 2006).
The connection between cardiovascular disease and insomnia bears specific attention. After adjusting for age and coronary risk factors, a risk ratio of 1.5–3.9 between difficulty falling asleep and coronary heart disease has been demonstrated (Schwartz et al., 1999). Men who experienced difficulty falling asleep were also shown to have a threefold risk of death secondary to coronary heart disease (Mallon et al., 2002).
The relationship between chronic pain and insomnia is also of particular clinical relevance. In one study, more than 40% of insomniacs reported having at least one chronic painful physical condition. Moreover, chronic pain was in turn associated with shorter sleep duration and decreased ability to resume sleep following arousal (Ohayon, 2005). Tang et al. (Tang et al., 2007) found that 53% of chronic pain patients had scores suggestive on the Insomnia Severity Index of clinical insomnia versus 3% of subjects without pain (Tang et al., 2007).
Socioeconomic Impact of Insomnia
In addition to psychiatric and medical comorbidities, insomnia is associated with substantial personal and societal consequences. One study that examined the effect of insomnia on primary care patients found insomniacs had double the number of days with restricted activity due to illness (Simon & Von Korff, 1997). Another study showed that more insomniacs rated their quality of life as poor (22%) when compared to subjects without any sleep complaints (3%) (Hajak et al., 2001). Insomnia has also been shown to have a detrimental effect on health-related quality of life to the same degree as chronic disorders such as depression and congestive heart failure (Katz & McHorney, 2002). When the economic costs that encompass health care use, workplace effects of absenteeism, accidents, and increased alcohol consumption secondary to insomnia were considered, the annual cost was estimated to be between $35 to $107 billion a year (Chilcott & Shapiro, 1996; Stoller, 1994). Insomnia has not been found to be associated with increased risk of death, however (Phillips & Mannino, 2005).
Health care utilization, as defined by increased office visits and rates of hospitalization, is consistently higher in insomniacs than in subjects without sleep complaints (Leger et al., 2002; Novak et al., 2004). In fact, the direct costs incurred through inpatient, outpatient, pharmacy, and emergency room usage is greater in insomniacs regardless of age (Ozminkowski et al., 2007). An evaluation of the direct health care costs of insomnia in 1995 placed estimates at $13.9 billion in the United States and $2.1 billion in France (Walsh & Engelhardt, 1999; Leger et al., 1999).
Function in the workplace is also negatively affected. Insomniacs miss work twice as often as good sleepers, with absenteeism particularly prominent in men and blue-collar workers (Leger et al., 2006). The extra cost of work absenteeism secondary to insomnia, through decreased productivity and salary replacement, is then brought to bear on employers (Godet-Cayre et al., 2006).
Insomnia Pathogenesis
Insomnia is often believed to arise from a state of “hyperarousal.” In the physiological hyperarousal model, an elevated level of alertness throughout the day and night makes it difficult to sleep. In support of this theory, insomniacs have been found to have an increased whole body metabolic rate when compared with normal sleepers (Bonnet & Arand, 1997; Stepanski et al., 1988). They also score higher than normal sleepers on a Hyperarousal Scale, and, even during the day when complaining of fatigue, insomniacs still take a longer time to fall asleep (Pavlova et al., 2001; Bonnet & Arand, 1995).
On functional neuroimaging, insomniacs show increased cerebral glucose metabolism both during sleep and wake states (Nofzinger et al., 2004). On electroencephalography (EEG), insomniacs demonstrate increased beta activity and lower delta activity (Krystal et al., 2002; Perlis et al., 2001). From an endocrine perspective, insomniacs, like patients with major depressive disorder, demonstrate corticotropin releasing factor hyperactivity, thus suggesting a role for hypothalamic-pituitary-adrenal axis dysfunction (Roth et al., 2007).
Insomnia Evaluation
The cornerstone of the insomnia evaluation is a detailed history obtained during the patient interview. While the approach to the interview may vary depending on the practitioner, key points should be covered in order to ensure a thorough evaluation. Additional assessment tools, such as the sleep-wake diary, actigraphy, and in specific cases polysomnography, can supplement the information obtained in the interview. A list of diagnoses and comorbid conditions to consider during the insomnia evaluation can be found in Table 3.
Table 3.
Insomnia Differential Diagnosis and Common Comorbidities
| (References: Buysse(Buysse, 2005); Sateia et al. (Sateia et al., 2000)) | |
| Medical Conditions: | |
| Cardiovascular | congestive heart failure, arrythmia, coronary artery disease |
| Pulmonary | COPD, asthma |
| Neurologic | stroke, Parkinson’s disease, neuropathy traumatic brain injury |
| Gastrointestinal | gastroesophageal reflux |
| Renal | chronic renal failure |
| Endocrine | diabetes, hyperthyroidism |
| Rheumatologic | rheumatoid arthritis, osteoarthritis, fibromyalgia, headaches |
| Sleep Disorders: | |
| Restless legs syndrome | |
| Periodic limb movement disorder | |
| Sleep apnea | |
| Circadian rhythm disorder | |
| Parasomnias | |
| Nocturnal panic attacks | |
| Nightmares | |
| REM behavior disorder | |
| Psychiatric Conditions: | |
| Depression | |
| Anxiety | |
| Panic disorder | |
| Post-traumatic stress disorder | |
| Medications: | |
| Decongestants | |
| Antidepressants | |
| Corticosteroids | |
| Beta-agonists | |
| Beta-antagonists | |
| Stimulants | |
| Statins | |
| Substances: | |
| Caffeine | |
| Alcohol | |
| Nicotine | |
| Cocaine | |
Patient interview
1. Detailed information about the nature of the complaint is necessary; if insomnia is related to sleep onset, sleep maintenance, early morning awakening, nonrestorative sleep quality, or a combination of these problems. Information obtained here may help to guide the diagnosis, such as a sleep onset complaint resulting from Restless Legs Syndrome as opposed to an early morning awakening presenting as part of a depressive disorder.
Additional information about the onset, course and duration, current presentation, frequency, severity, and precipitating or alleviating factors also helps to define the problem. In particular, a lifelong course with an onset in the absence of medical and psychiatric comorbidities may suggest a primary insomnia as opposed to a secondary insomnia that develops in late adulthood in the context of chronic pain.
2. Discussion of the sleep-wake routine. The sleep schedule, including bed time, sleep latency, number and length of nighttime awakenings, sleep reinitiation time, wake time, time spent in bed, and total sleep time should be reviewed. A patient’s preferred bedtime may not coincide with actual bedtime, as in a circadian rhythm disorder. Similarly, nighttime awakenings due to nightmares from PTSD as opposed to awakenings from nocturia due to prostate enlargement suggest different disorders.
The daytime routine with a review of work schedule, eating and exercise times, and duration and timing of naps is also important. Eating and exercise times that occur in close temporal relation to bedtimes may inhibit the patient’s ability to fall asleep. Moreover, naps of long duration that occur in the late afternoon or evening may have a similar negative effect on sleep latency and continuity.
3. Discussion of daytime functioning and associated symptoms. This category may include: daytime sleepiness, fatigue, difficulty with memory and concentration, depression, anxiety, irritability, impairment at work, school or home, and overall quality of life. A report of daytime impairment and patient distress may underscore the severity of symptoms, and thus highlight the need to aggressively treat insomnia. In this area, collateral report from family, teachers, or coworkers may prove helpful if the patient is unaware of the extent of his/her symptoms. Safety issues such as the negative effect on driving and work performance in potentially hazardous areas should be broached and may provide an opportunity for patient education.
4. Sleep conditions and routines. The conditions of the room used for sleep (example- effect of light, temperature, and noise); use of TV, computer, or radio both in the pre-bedtime routine and during periods of nighttime awakenings; the effect of anxiety during sleep latency and sleep reinitiation periods; and the presence of clock-watching before and during sleep times. Too much noise or light exposure in the sleeping room may inhibit sleep initiation. Similarly, clock-watching with each nighttime awakening may only further heighten an already raised level of anxiety. Specific difficulty falling asleep at home but not while out of town may suggest insomnia related to the bedroom environment.
5. Previous treatments tried and their effects and side effects. Treatments may include over the counter, homeopathic, herbal, or prescription medications as well as behavioral therapies. In addition to providing information on potential treatments that may not have been offered to the patient yet, information obtained in this area may provide a sense of the kind of treatment the patient is looking for.
6. Symptoms of other sleep disorders that could be affecting the complaint. Conditions such as restless legs syndrome, periodic limb movement disorder, sleep apnea, and sleep phase syndromes should be considered as possible contributors to insomnia.
7. Review of comorbid medical conditions that could play a role in the presentation. General categories to consider include: cardiovascular, pulmonary, neurologic, gastrointestinal, renal, endocrine, and rheumatologic.
8. Review of underlying psychiatric conditions and psychosocial stressors. Eliciting symptoms of depression, bipolar disorder, anxiety, panic – including nocturnal panic attacks, and psychosis can help to clarify the diagnostic picture while emphasizing the need to obtain or continue psychiatric care.
9. Review of substance use, including nicotine, alcohol, and caffeine. This discussion should cover amount, frequency, and time of day the substance is used as all of these substances may contribute to an insomnia complaint. Patient education about the effects of nicotine, alcohol, and caffeine on sleep should also be undertaken if it appears that substance use has a negative effect on sleep quality.
10. Review of family history of sleep, medical, and psychiatric disorders.
Physical and mental status exam
1. The physical exam may reveal signs consistent with sleep apnea (obesity, enlarged neck circumference, crowded orophaynx) as well as thyroid, cardiac, respiratory, and neurologic disorders.
2. The mental status exam may yield information about the patient’s mood, affect, level of alertness, and ability to attend.
Collateral sources interview
Interview of the patient’s bed partner or family members, if possible, to elicit symptoms of which the patient may be unaware. This part of the evaluation may also help to corroborate and expand upon the patient’s original description. Revelation about respiratory symptoms (snoring, apneas, or gasping) could suggest a sleep-disordered breathing etiology, while report of repeated limb movements may move the diagnosis towards RLS or PLMD.
Objective data
1. Actigraphy
Actigraphy helps to characterize rest-activity patterns and may have some utility as an objective measure when used in conjunction with a sleep-wake dairy and formal interview. For insomniacs actigraphy can provide information about circadian rhythms and sleep patterns (Morgenthaler et al., 2007). Compared with polysomnography, however, actigraphy in insomniacs has had variable results: it has been found to both over and underestimate total sleep time (Vallieres & Morin, 2003; Sivertsen et al., 2006; Sadeh & Acebo, 2002). Another study found that actigraphy was well validated by polysomnography with respect to number of awakenings, wake time after sleep onset, total sleep time, and sleep efficiency (Lichstein et al., 2006). When using actigraphy increasing the duration of recording to more than 7 days may improve the reliability of sleep time estimates (Van Someren, 2007).
2. Polysomnography
Polysomnography is not routinely used in the evaluation of insomnia; the onus of the diagnosis lies instead on the patient interview. According to 2003 practice parameters established by the American Academy of Sleep Medicine, specific cases may apply when polysomnography is warranted. These cases include suspicion of sleep-related breathing disorders or periodic limb movement disorders, uncertain initial diagnosis, treatment failure, and arousals leading to violent behavior (Littner et al., 2003).
3. Sleep diaries
Sleep diaries recorded over 1–2 weeks can help track a patient’s sleep-wake patterns. Information including actual sleep-wake times, duration of time in bed, and day to day variability in sleep-wake times can be gathered from the diaries (see Figure 1).
Figure 1.
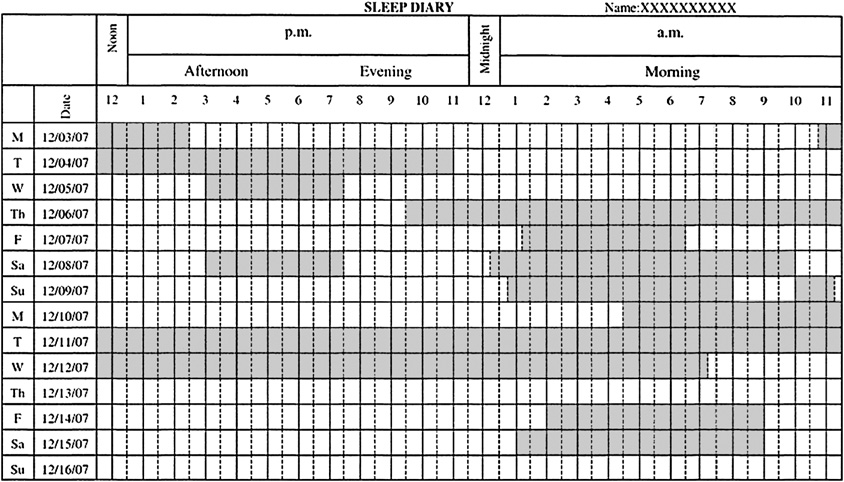
Sleep Diary
Summary
Insomnia is thought to result from a state of “hyperarousal.” As a result of this elevated state of alertness, sleep may prove difficult. Formulating a clinical definition of insomnia has proven a challenge. Nevertheless, some enduring characteristics of insomnia include difficulty with sleep initiation or maintenance, early morning awakening, and nonrestorative sleep in the setting of daytime impairment or distress in the setting of adequate sleep opportunity. With these characteristics in mind the prevalence of insomnia is thought to be approximately 10%.
The evaluation of insomnia emphasizes the interview, during which information about the specific complaint, comorbid sleep, medical, or psychiatric conditions, family histories, medication, and substance use may be gathered. Additional information from collateral sources, sleep diaries, actigraphy, and polysomnography may also prove useful.
Insomnia is a disorder that has far-reaching effects: medical, psychiatric, personal, and societal consequences have all been linked with insomnia. The cost of insomnia can be measured not just in dollars, but also in impaired quality of life from comorbid conditions and impaired interpersonal relationships.
Acknowledgments
Supported by NIH grants MH24652 and AG20677
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- American Academy of Sleep Medicine. The International Classification of Sleep Disorders, Second Edition (ICSD-2): Diagnostic and Coding Manual. Second Edition 2005. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) Fourth Edition, Text Revision. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Ancoli-Israel S. The impact and prevalence of chronic insomnia and other sleep disturbances associated with chronic illness. The American Journal of Managed Care. 2006;12:S221–S229. [PubMed] [Google Scholar]
- Ancoli-Israel S, Roth T. Characteristics of insomnia in the United States: results of the 1991 National Sleep Foundation Survey. I. Sleep. 1999;22 Suppl 2:S347–S353. [PubMed] [Google Scholar]
- Bastien CH, Vallieres A, Morin CM. Precipitating factors of insomnia. Behavioral Sleep Medicine. 2004;2:50–62. doi: 10.1207/s15402010bsm0201_5. [DOI] [PubMed] [Google Scholar]
- Bixler EO, Kales A, Soldatos CR, Kales JD, Healey S. Prevalence of sleep disorders in the Los Angeles metropolitan area. American Journal of Psychiatry. 1979;136:1257–1262. doi: 10.1176/ajp.136.10.1257. [DOI] [PubMed] [Google Scholar]
- Bonnet MH, Arand DL. 24-hour metabolic rate in insomniacs and matched normal sleepers. Sleep. 1995;18:581–588. doi: 10.1093/sleep/18.7.581. [DOI] [PubMed] [Google Scholar]
- Bonnet MH, Arand DL. Hyperarousal and insomnia. Sleep Medicine Reviews. 1997;1:97–108. doi: 10.1016/s1087-0792(97)90012-5. [DOI] [PubMed] [Google Scholar]
- Buysse DJ. Sleep Disorders and Psychiatry. Arlington, VA: American Psychiatric Publishing, Inc.: American Psychiatric Publishing Review of Psychiatry; 2005. [Google Scholar]
- Chilcott LA, Shapiro CM. The socioeconomic impact of insomnia. Pharmacoeconomics. 1996;10:1–14. doi: 10.2165/00019053-199600101-00003. [DOI] [PubMed] [Google Scholar]
- Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? Journal of the American Medical Association. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- Godet-Cayre V, Pelletier-Fleury N, Le Vaillant M, Dinet J, Massuel MA, Leger D. Insomnia and absenteeism at work. Who pays the cost? Sleep. 2006;29:179–184. doi: 10.1093/sleep/29.2.179. [DOI] [PubMed] [Google Scholar]
- Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J.Consult Clin.Psychol. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajak G SINE Study Group, & Study of Insomnia in Europe. Epidemiology of severe insomnia and its consequences in Germany. European Archives of Psychiatry and Clinical Neuroscience. 2001;251:49–56. doi: 10.1007/s004060170052. [DOI] [PubMed] [Google Scholar]
- Harvey AG. Insomnia: symptom or diagnosis? Clinical Psychology Review. 2001;21:1037–1059. doi: 10.1016/s0272-7358(00)00083-0. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, Breslau N. The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. Journal of Psychiatric Research. 2006a;40:700–708. doi: 10.1016/j.jpsychires.2006.07.008. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Roth T, Schultz L, Breslau N. Epidemiology of DSM-IV insomnia in adolescence: lifetime prevalence, chronicity, and an emergent gender difference. Pediatrics. 2006b;117:e247–e256. doi: 10.1542/peds.2004-2629. [DOI] [PubMed] [Google Scholar]
- Katz DA, McHorney CA. Clinical correlates of insomnia in patients with chronic illness. Archives of Internal Medicine. 1998;158:1099–1107. doi: 10.1001/archinte.158.10.1099. [DOI] [PubMed] [Google Scholar]
- Katz DA, McHorney CA. The relationship between insomnia and health-related quality of life in patients with chronic illness. Journal of Family Practice. 2002;51:229–235. [PubMed] [Google Scholar]
- Klink ME, Quan SF, Kaltenborn WT, Lebowitz MD. Risk factors associated with complaints of insomnia in a general adult population. Archives of Internal Medicine. 1992;152:1634–1637. [PubMed] [Google Scholar]
- Krystal AD, Edinger JD, Wohlgemuth WK, Marsh GR. NREM sleep EEG frequency spectral correlates of sleep complaints in primary insomnia subtypes. Sleep. 2002;25:630–640. [PubMed] [Google Scholar]
- Kuppermann M, Lubeck DP, Mazonson PD, Patrick DL, Stewart AL, Buesching DP, et al. Sleep problems and their correlates in a working population. Journal of General Internal Medicine. 1995;10:25–32. doi: 10.1007/BF02599573. [DOI] [PubMed] [Google Scholar]
- Leger D, Guilleminault C, Bader G, Levy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25:625–629. [PubMed] [Google Scholar]
- Leger D, Guilleminault C, Dreyfus JP, Delahaye C, Paillard M. Prevalence of insomnia in a survey of 12,778 adults in France. Journal of Sleep Research. 2000;9:35–42. doi: 10.1046/j.1365-2869.2000.00178.x. [DOI] [PubMed] [Google Scholar]
- Leger D, Levy E, Paillard M. The direct costs of insomnia in France. Sleep. 1999;22:S394–S401. [PubMed] [Google Scholar]
- Leger D, Massuel MA, Metlaine A. Professional correlates of insomnia. Sleep. 2006;29:171–178. [PubMed] [Google Scholar]
- Lichstein KL, Stone KC, Donaldson J, Nau SD, Soeffing JP, Murray D, et al. Actigraphy validation with insomnia. Sleep. 2006;29:232–239. [PubMed] [Google Scholar]
- Littner M, Hirshkowitz M, Kramer M, Kapen S, Anderson M, Bailey D, et al. Practice parameters for using polysomnography to evaluate insomnia. Sleep. 2003;26:754–757. doi: 10.1093/sleep/26.6.754. [DOI] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of middle-aged Swedish population. Journal of Internal Medicine. 2002;251:207–216. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- McCall WV. A psychiatric perspective on insomnia. Journal of Clinical Psychiatry. 2001;62 Suppl 10:27–32. [PubMed] [Google Scholar]
- Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment: Prevalence and correlates. Archives of General Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- Morgan K. Daytime activity and risk factors for late-life insomnia. Journal of Sleep Research. 2003;12:231–238. doi: 10.1046/j.1365-2869.2003.00355.x. [DOI] [PubMed] [Google Scholar]
- Morgan K, Clarke D. Risk factors for late-life insomnia in a representative general practice sample. Br.J.Gen.Pract. 1997;47:166–169. [PMC free article] [PubMed] [Google Scholar]
- Morgenthaler T, Alessi C, Friedman L, Owens J, Kapur V, Boehlecke B, et al. Practice parameters for the use of actigraphy in the assessment of sleep and sleep disorders: an update for 2007. Sleep. 2007;30:519–529. doi: 10.1093/sleep/30.4.519. [DOI] [PubMed] [Google Scholar]
- Murata C, Yatsuya H, Tamakoshi K, Otsuka R, Wada K, Toyoshima H. Psychological factors and insomnia among male civil servants in Japan. Sleep Medicine. 2007;8:209–214. doi: 10.1016/j.sleep.2007.01.008. [DOI] [PubMed] [Google Scholar]
- Nakata A, Haratani T, Takahashi M, Kawakami N, Arito H, Kobayashi F, et al. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Social Science and Medicine. 2004;59:1719–1730. doi: 10.1016/j.socscimed.2004.02.002. [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. Bethesda, MD: NIH State-of-the-Science Conference Statement on Manifestations and Management of Chronic Insomnia in Adults. 2005
- Nofzinger EA, Buysse DJ, Germain A, Price JC, Miewald JM, Kupfer DJ. Functional neuroimaging evidence for hyperarousal in insomnia. American Journal of Psychiatry. 2004;161:2126–2131. doi: 10.1176/appi.ajp.161.11.2126. [DOI] [PubMed] [Google Scholar]
- Novak M, Mucsi I, Shapiro CM, Rethelyi J, Kopp MS. Increased utilization of health services by insomniacs--an epidemiological perspective. Journal of Psychosomatic Research. 2004;56:527–536. doi: 10.1016/j.jpsychores.2004.02.007. [DOI] [PubMed] [Google Scholar]
- Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Medicine Reviews. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Ohayon MM. Relationship between chronic painful physical condition and insomnia. Journal of Psychiatric Research. 2005;39:151–159. doi: 10.1016/j.jpsychires.2004.07.001. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Hong SC. Prevalence of insomnia and associated factors in South Korea. Journal of Psychosomatic Research. 2002;53:593–600. doi: 10.1016/s0022-3999(02)00449-x. [DOI] [PubMed] [Google Scholar]
- Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. Journal of Psychiatric Research. 2003;37:9–15. doi: 10.1016/s0022-3956(02)00052-3. [DOI] [PubMed] [Google Scholar]
- Ozminkowski RJ, Wang S, Walsh JK. The direct and indirect costs of untreated insomnia in adults in the United States. Sleep. 2007;30:263–273. doi: 10.1093/sleep/30.3.263. [DOI] [PubMed] [Google Scholar]
- Pavlova M, Berg O, Gleason R, Walker F, Roberts S, Regestein Q. Self-reported hyperarousal traits among insomnia patients. Journal of Psychosomatic Research. 2001;51:435–441. doi: 10.1016/s0022-3999(01)00189-1. [DOI] [PubMed] [Google Scholar]
- Perlis ML, Smith MT, Andrews PJ, Orff H, Giles DE. Beta/Gamma EEG activity in patients with primary and secondary insomnia and good sleeper controls. Sleep. 2001;24:110–117. doi: 10.1093/sleep/24.1.110. [DOI] [PubMed] [Google Scholar]
- Phillips B, Mannino DM. Does Insomnia Kill? Sleep. 2005;28:965–971. doi: 10.1093/sleep/28.8.965. [DOI] [PubMed] [Google Scholar]
- Riemann D, Voderholzer U. Primary insomnia: a risk factor to develop depression? Journal of Affective Disorders. 2003;76:255–259. doi: 10.1016/s0165-0327(02)00072-1. [DOI] [PubMed] [Google Scholar]
- Roth T. Insomnia: definition, prevalence, etiology, and consequences. J.Clin.Sleep Med. 2007;3:S7–S10. [PMC free article] [PubMed] [Google Scholar]
- Roth T, Roehrs T, Pies R. Insomnia: pathophysiology and implications for treatment. Sleep Medicine Reviews. 2007;11:71–79. doi: 10.1016/j.smrv.2006.06.002. [DOI] [PubMed] [Google Scholar]
- Sadeh A, Acebo C. The role of actigraphy in sleep medicine. Sleep Medicine Reviews. 2002;6:113–124. doi: 10.1053/smrv.2001.0182. [DOI] [PubMed] [Google Scholar]
- Sateia MJ, Doghramji K, Hauri PJ, Morin CM. Evaluation of chronic insomnia. An American Academy of Sleep Medicine review. Sleep. 2000;23:243–308. [PubMed] [Google Scholar]
- Schwartz S, McDowell AW, Cole SR, Cornoni-Huntley J, Hays JC, Blazer D. Insomnia and heart disease: a review of epidemiologic studies. Journal of Psychosomatic Research. 1999;47:313–333. doi: 10.1016/s0022-3999(99)00029-x. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M. Prevalence, burden, and treatment of insomnia in primary care. American Journal of Psychiatry. 1997;154:1417–1423. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- Sivertsen B, Omvik S, Havik OE, Pallesen S, Bjorvatn B, Nielsen GH, et al. A comparison of actigraphy and polysomnography in older adults treated for chronic primary insomnia. Sleep. 2006;29:1353–1358. doi: 10.1093/sleep/29.10.1353. [DOI] [PubMed] [Google Scholar]
- Stepanski E, Zorick F, Roehrs T, Young D, Roth T. Daytime alertness in patients with chronic insomnia compared with asymptomatic control subjects. Sleep. 1988;11:54–60. doi: 10.1093/sleep/11.1.54. [DOI] [PubMed] [Google Scholar]
- Stoller MK. Economic effects of insomnia. [Review] Clinical Therapeutics. 1994;16:873–897. discussion 854. [PubMed] [Google Scholar]
- Su TP, Huang SR, Chou P. Prevalence and risk factors of insomnia in community-dwelling Chinese elderly: a Taiwanese urban area survey. Aust.N.Z.J.Psychiatry. 2004;38:706–713. doi: 10.1080/j.1440-1614.2004.01444.x. [DOI] [PubMed] [Google Scholar]
- Tang NK, Wright KJ, Salkovskis PM. Prevalence and correlates of clinical insomnia co-occurring with chronic back pain. Journal of Sleep Research. 2007;16:85–95. doi: 10.1111/j.1365-2869.2007.00571.x. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Lichstein KL, Durrence HH. Insomnia as a health risk factor. Behavioral Sleep Medicine. 2003;1:227–247. doi: 10.1207/S15402010BSM0104_5. [DOI] [PubMed] [Google Scholar]
- Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- Ustun TB, Privett M, Lecrubier Y, Weiller E, Simon G, Korten A, et al. Form, frequency and burden of sleep problems in general health care: a report from the WHO Collaborative Study on Psychological Problems in General Health Care. European Psychiatry. 1996;11:S5–S10. [Google Scholar]
- Vallieres A, Morin CM. Actigraphy in the assessment of insomnia. Sleep. 2003;26:902–906. doi: 10.1093/sleep/26.7.902. [DOI] [PubMed] [Google Scholar]
- Van Someren EJ. Improving actigraphic sleep estimates in insomnia and dementia: how many nights? Journal of Sleep Research. 2007;16:269–275. doi: 10.1111/j.1365-2869.2007.00592.x. [DOI] [PubMed] [Google Scholar]
- Walsh JK, Engelhardt CL. The direct economic costs of insomnia in the United States for 1995. Sleep. 1999;22:S386–S393. [PubMed] [Google Scholar]
- Weissman MM, Greenwald S, Nino-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. General Hospital Psychiatry. 1997;19:245–250. doi: 10.1016/s0163-8343(97)00056-x. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Geneva: World Health Organization; The ICD-10 classification of mental and behavioural disorders. Clinical descriptions and diagnostic guidelines. 1992


