Abstract
Local excision of hilar cholangiocarcinomas results in long-term survival in only very few cases. Therefore, the combination of right or left liver resection and bile duct resection has been the standard treatment since about 1990. Five-year survival rates after curative resection could be improved to 30–40%. Recurrence is frequently seen locally, therefore more extended resection with adherence to the surgical principals of tumor resection, such as the “no-touch technique”, appears useful. Excellent results with 5-year survival rates up to 60% after curative resection can be achieved with right trisectionectomy together with principle en bloc hilar resection. Perioperative mortality is still high because of the small remaining liver volume.
It is now more than 40 years since the first reports of surgery for hilar cholangiocarcinoma, but generally accepted guidelines for the strategy of radical resections are still lacking for this disease 1,2. One major reason for this shortcoming may be the lack of randomized trials regarding the efficacy of the different surgical strategies, implementation of which is clearly aggravated by the rareness of the tumor. Therefore, our current knowledge about results of radical surgery for hilar cholangiocarcinoma is mainly based on the findings of observational studies.
First reports of larger series in the 1970s and 1980s reported long-term survival in some patients and improved overall survival figures after surgical resection 3,4,5. Based on the results of such studies, surgery as the only curative approach in hilar cholangiocarcinoma became the treatment of choice in suitable patients. However, with local excisions, including resection of the supraduodenal bile duct, cholecystectomy and portal lymphadenectomy with restoration of the bilioenteric continuity, curative resections were only achieved in a minority of patients and cure was rarely observed 6,7. Recurrence occurred frequently after such local excisions even after the curative nature of the procedure, with the liver hilum as the most frequent site of recurrence 8. Histomorphological analysis of tumor specimens and clinical experience with the cancer revealed that hilar cholangiocarcinoma did not seem to metastasize as early and frequently as other gastrointestinal cancers, but perineural invasion and lymphangiosis carcinomatosa, which can extend up to two centimeters from the tumor into the liver and distally into the hepatoduodenal ligament were described frequently 9,10,11. Therefore, the tumor cannot be radically resected by local excisions and today only exceptionally is hilar resection considered curative treatment in patients with hilar cholangiocarcinoma. Since the bile duct of the caudate lobe comes frequently as a direct branch from the bile duct bifurcation, it was thought that additional resection of the caudate lobe would significantly improve the survival rates after surgical resection 12. However, no survival advantage of additional caudate lobe resection has been documented so far.
As hilar cholangiocarcinoma extends centimeters behind its visible and palpable extensions, broadening of the tumor-free resection margins was considered to be crucial for the results after surgical resection. Owing to its anatomical location, the liver is in close contact with the tumor and direct infiltration is described frequently 13. Therefore, an additional resection of the right or left liver lobe is considered to be essential for a radical surgical approach. With the additional liver resection it is possible to get wide resection margins at the proximal ramification of the tumor and to resect eventual tumor infiltrations of the parenchyma as well. Most centers have adopted this approach over the past two decades and the results have clearly improved compared to hilar resection alone. Reported curative resection rates are around 70%, with long-term survival between 20% and 40% 14,15,16,17,18,19,20. The results of selected observational studies are depicted in Figure 1. Based on these observational studies of most of the hepatobiliary centers worldwide, hilar resection with additional major hepatectomy is currently accepted as the treatment of choice for hilar cholangiocarcinoma in suitable patients.
Figure 1. .
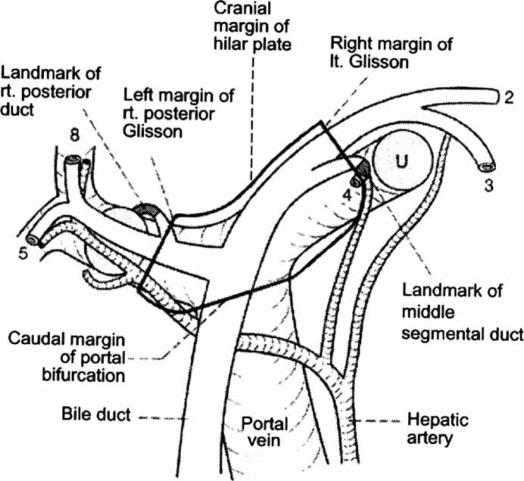
Schematic image of the hepatic hilum. The confluence of the right and left hepatic bile ducts is located on the right side of the hepatoduodenal ligament. The right hepatic artery runs on the dorsal side close to the common bile duct. The area of the hepatic hilum that can be approached without dissecting hepatic parenchyma is encircled by the continuous line 25.
The type and extent of the additional liver resection are still controversial, however. The efficacy of additional liver resection has been demonstrated in multiple series, although significant differences in long-term results after different types of liver resections have been much less reported. In a prospective study on 40 patients, Kondo et al. found a significant survival advantage for patients who underwent right hemihepatectomy 21. Compared to left lobe resection, the advantage probably comes from less extensive preparation during the right-sided lobectomy, since the biliary confluence lies on the right side of the hepatic hilum. Moreover, the right hepatic artery runs close to the bile duct bifurcation and does not have to be separated from the tumor during right-sided lobectomy, which probably leads to an increase in radicality.
We described a right trisectionectomy with en bloc portal vein and bile duct resection as an independent prognostic factor for survival after curative resection 19. The advantage of this procedure compared to major liver resection alone is probably due to increased radicality, because the right branch of the portal vein is in close contact with the tumor and is frequently infiltrated by the tumor. The right hepatic artery runs between the tumor and portal vein and is also often infiltrated, whereas the left artery runs on the left margin of the hepatoduodenal ligament and is almost never attached to the tumor. En bloc resection of extrahepatic bile ducts, portal vein bifurcation, and right hepatic artery, together with six liver segments I and VI to VIII is a principle advantage in oncological surgery, because only this technique follows the oncological rules of a “no-touch technique” 22. Taken together, the oncological principles of wide tumor-free resection margins, the avoidance of dissection near tumor tissue (no-touch technique) and the principle use of right trisectionectomy not only yield better results, but also allow for increased resectability. If the left lateral lobe of the liver on the other hand is too small or the portal vein of the left side is infiltrated by a tumor, as in Bismuth type VI cases, an extended left hepatectomy together with resection of the biliary system as far to the right side as possible is the second best choice. Here, dissection of the right hepatic artery and portal vein cannot be avoided, but with an R0 resection a 30% 5-year survival may still be achieved.
Right trisectionectomy, together with en bloc hilar resection, allows for encouraging long-term results with 5-year survival rates up to 60% after curative resection 19, but the postoperative mortality has to be taken into account. Hepatic failure is the most frequent cause of postoperative deaths after such extensive liver resections. Therefore, besides careful patient selection, a preoperative multimodal treatment approach is needed to optimize the remnant liver function. Such a multimodal approach includes recovery of damaged liver function and treatment of segmental cholangitis by sufficient biliary decompression and hypertrophy of and functional transition to the future remnant liver by portal embolization 23,24.
Consensus statements
Currently, hilar resection with additional major liver resection is the treatment of choice in suitable patients with right-sided hilar cholangiocarcinoma (low; multiple observational studies).
Right-sided hemihepatectomy and extended right-sided hemihepatectomy are the preferred procedures for additional liver resection (low, few observational studies).
The best results seem to be achieved by en bloc right trisectionectomy and portal vein resection (low, one observational study).
Hilar resection is currently considered a palliative procedure in these patients (low, multiple observational studies).
References
- 1.Altmeier WA, Gall EA, Zinninger MM, Hoxworth PL. Sclerosing carcinoma of the major intrahepatic bile ducts. Arch Surg. 1957;75:459–61. doi: 10.1001/archsurg.1957.01280150140015. [DOI] [PubMed] [Google Scholar]
- 2.Klatskin G. Adenocarcinoma of the hepatic duct at its bifurcation within the porta hepatis. Am J Med. 1965;38:241–56. doi: 10.1016/0002-9343(65)90178-6. [DOI] [PubMed] [Google Scholar]
- 3.Launois B, Campion JP, Brissot P, Gosselin M. Carcinoma of the hepatic hilus. Surgical management and the case for resection. Ann Surg. 1979;190:151–7. doi: 10.1097/00000658-197908000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Evander A, Fredlund P, Hovels J, Ihse I, Bengmark S. Evaluation of aggressive surgery for carcinoma of the extrahepatic bile ducts. Ann Surg. 1980;191:23–9. doi: 10.1097/00000658-198001000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blumgart LH, Hadjis NS, Benjamin IS, Beasley R. Surgical approaches to carcinoma at confluence of hepatic hilus. Lancet. 1984;1:66–70. doi: 10.1016/s0140-6736(84)90002-3. [DOI] [PubMed] [Google Scholar]
- 6.Beazley RM, Hadjis N, Benjamin IS. Clinicopathological subjects of high bile duct cancer: experience with resection and bypass surgical treatments. Ann Surg. 1984;199:623–36. doi: 10.1097/00000658-198406000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mizumoto R, Kawarada Y, Suzuki H. Surgical treatment of hilar carcinoma of the bile duct. Surg Gynecol Obstet. 1986;162:153–8. [PubMed] [Google Scholar]
- 8.Mittal B, Deutsch M, Iwatsuki S. Primary cancers of extrahepatic biliary passages. Int J Radiat Oncol Biol Phys. 1985;11:849–54. doi: 10.1016/0360-3016(85)90320-7. [DOI] [PubMed] [Google Scholar]
- 9.Pichelmayr R, Ringe B, Lauchart W, Bechstein WO, Gubernatis G, Wagner E. Radical resection and liver grafting as the two main components of surgical strategy in the treatment of proximal bile duct cancer. World J Surg. 1988;12:88–98. doi: 10.1007/BF01658489. [DOI] [PubMed] [Google Scholar]
- 10.Bhuiya MR, Nimura Y, Kamiya J, Kondo S, Fukata S, Hayakawa N, et al. Clinicopathologic studies on perineural invasion of bile duct carcinoma. Ann Surg. 1992;215:344–9. doi: 10.1097/00000658-199204000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ouchi K, Suzuki M, Hashimoto L, Sato T. Histologic findings and prognostic factors in carcinoma of the upper bile duct. Am J Surg. 1989;157:552–6. doi: 10.1016/0002-9610(89)90697-1. [DOI] [PubMed] [Google Scholar]
- 12.Mizumoto R, Suzuki H. Surgical anatomy of the hepatic hilum with special reference to the caudate lobe. World J Surg. 1988;12:2–10. doi: 10.1007/BF01658479. [DOI] [PubMed] [Google Scholar]
- 13.Sakamoto E, Nimura Y, Hayakawa N, Kamiya J, Kondo S, Nagino M, et al. The pattern of infiltration at the proximal border of hilar bile duct carcinoma: a histologic analysis of 62 resected cases. Ann Surg. 1998;227:405–11. doi: 10.1097/00000658-199803000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jarnagin WR, Fong Y, DeMatteo RP, Goner M, Burke EC, Bodniewicz BS J, et al. Staging, resectability and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507–17. doi: 10.1097/00000658-200110000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nimura Y, Kamiya J, Kondo S, Nagino M, Uesaka K, Oda K, et al. Aggressive preoperative management and extended surgery for hilar cholangiocarcinoma: Nagoya experience. J Hepatobil Pancreat Surg. 2000;7:155–62. doi: 10.1007/s005340050170. [DOI] [PubMed] [Google Scholar]
- 16.Todoriki T, Kawamoto T, Koike N, Takahashi H, Yoshida S, Kashiwagi H, et al. Radical resection of hilar bile duct carcinoma and predictors of survival. Br J Surg. 2000;87:306–13. doi: 10.1046/j.1365-2168.2000.01343.x. [DOI] [PubMed] [Google Scholar]
- 17.Tabata M, Kawarada Y, Yokoi H, Higashiquchi T, Isaji S. Surgical treatment for hilar cholangiocarcinoma. J Hepatobil Pancreat Surg. 2000;7:148–54. doi: 10.1007/s005340050169. [DOI] [PubMed] [Google Scholar]
- 18.Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Okaya T, et al. Parenchyma-preserving hepatectomy in the surgical treatment of hilar cholangiocarcinoma. J Am Coll Surg. 1999;189:575–83. doi: 10.1016/s1072-7515(99)00219-7. [DOI] [PubMed] [Google Scholar]
- 19.Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808–19. doi: 10.1097/00000658-199912000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klempnauer J, Ridder GJ, von Wasielewski R, Werner M, Weimann A, Pichlmayr R. Resectional surgery of hilar cholangiocarcinoma: a multivariate analysis of prognostic factors. J Clin Oncol. 1997;15:947–54. doi: 10.1200/JCO.1997.15.3.947. [DOI] [PubMed] [Google Scholar]
- 21.Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins. Results of a prospective study. Ann Surg. 2004;240:95–101. doi: 10.1097/01.sla.0000129491.43855.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jonas S, Steinmüller T, Neuhaus P. Surgical therapy of liver hilus tumors. Chirurg. 2001;72:775–83. doi: 10.1007/s001040170105. [DOI] [PubMed] [Google Scholar]
- 23.Nimura Y, Kamiya J, Kondo S, Nagino M, Kanai M. Technique of inserting multiple biliary drains and management. Hepatogastroenterology. 1995;42:323–31. [PubMed] [Google Scholar]
- 24.Nagino M, Kamiya J, Kanai M, Uesaka K, Sano T, Yamamoto H, et al. Right trisegment portal vein embolization for biliary tract carcinoma: technique and clinical utility. Surgery. 2000;127:155–60. doi: 10.1067/msy.2000.101273. [DOI] [PubMed] [Google Scholar]
- 25.Hirano S, Tanaka E, Shichinohe T, Suzuki O, Hazama K, Kitagami H, et al. Treatment strategy for hilar cholangiocarcinoma, with special reference to the limits of ductal resection in right-sided hepatectomies. J Hepateobil Pancreat Surg. 2007;14:429–33. doi: 10.1007/s00534-006-1190-5. [DOI] [PubMed] [Google Scholar]