Abstract
Aim. In patients with malignant hilar obstruction, liver resection is associated with an increased risk of postoperative liver failure attributed to the need for major liver resection in a context of obstructive jaundice. To overcome this issue, most authors recommend preoperative biliary drainage (PBD). However, PBD carries risks of its own, including, primarily, sepsis and, more rarely, tumor seeding, bile peritonitis, and hemobilia. We, unlike most authors, have not used routine PBD before liver resection in jaundiced patients. Material and methods. Our series includes 62 patients who underwent major liver resection for cholangiocarcinoma; 33 of these had elevated bilurubin (60–470 µmol/l) and were operated without PBD. There were 43 extended right hepatectomies and 18 extended left hepatectomies. Results. Hospital deaths occurred in 5 patients (8%) including 3 of 33 jaundiced patients (9%, ns). All deaths occurred after extended right hepatectomy (12%), including 3 patients with a serum bilirubin level above 300 µmol/l and 2 with normal bilirubin. There were no deaths after left-sided resections, whatever the level of bilirubin. Conclusions. PBD can be omitted in the following situations: recent onset jaundice (<2–3 weeks), total bilirubin <200 µmol/l, no previous endoscopic or transhepatic cholangiography, absence of sepsis, future liver remnant >40%. These criteria include most patients requiring left-sided resections and selected patients requiring right-sided resections. In other cases, PBD is required, associated with portal vein embolization in the event of a small future liver remnant.
Introduction
Liver resections in jaundiced patients are associated with significant rates of mortality and morbidity due mainly to the development of postoperative liver failure. Therefore, preparation for surgery by preoperative biliary drainage (PBD) has been advocated before definitive surgery with the aim of reducing morbidity and mortality 1,2,3,4. More recently, induction of hypertrophy of the remaining liver by portal vein embolization has also become a frequent part of preparation for surgery 5. However, PBD is associated with complications of its own that may reduce its benefits substantially. These include mainly sepsis but also tumor seeding along biliary drain tracts.
Benefit
Five level-1 prospective randomized trials of preoperative PBD, including more than 300 patients, have failed to demonstrate a survival benefit of PBD, while all 5 showed increased morbidity and hospital stay with PBD 6,7,8,9,10. A meta-analysis of these studies by Sewnath et al. has confirmed individual analysis of each paper 11. In the same study, meta-analysis of 18 additional level-2 studies (non-randomized cohort comparisons) including close to 3000 patients showed the same lack of benefit and confirmed increased morbidity. When PBD-induced complications were removed from analysis, PBD was associated with a benefit. However, these trials included patients with various benign and malignant diseases, and most malignant lesions were located in the distal portion of the bile duct. Consequently, very few patients in these studies underwent liver resection. These studies clearly indicated that PBD was associated with specific complications which could outweigh the potential benefits of this technique.
Complications
Sepsis is the main complication of PBD 1,2,3,4,5,12. Cholangitis after PBD has been reported in 20–60% of cases and may compromise subsequent surgery with patient dropout. Intraoperative bile cultures have been found to be positive in 65% of patients with PBD, while the rate was 8% in patients without PBD. This may be associated with increased postoperative infections such as wound or intraperitoneal abscesses.
Implantation metastases can occur in up to 6% of cases after transhepatic PBD 13. Peritoneal and pleural metastases have also been reported. These complications clearly compromise the oncologic results of such procedures. Finally, bile peritonitis and hemobilia are other complications reported in association with PBD.
Specific indications
Despite these drawbacks and because liver resections in jaundiced patients are considered to carry a special risk, most authors continue to recommend PBD before resection of hilar cholangiocarcinoma.
In the absence of demonstrated benefits of PBD, our policy in patients undergoing liver resection for high malignant obstructive stricture has been to avoid systematic PBD. Direct cholangiography, either percutaneous or endoscopic, in jaundiced patients requires subsequent biliary drainage and therefore should be avoided prior to patient referral. This is possible with modern imaging, including MDCT and MRCP. Because we do not use routine PBD, we attempt to schedule surgery in patients with obstructive jaundice due to proximal bile duct cancer as quickly as possible. Our policy is to perform non-invasive preoperative imaging work-up followed by laparotomy in the same week.
Personal experience
In order to identify specific complications observed in jaundiced patients undergoing major liver resection, we undertook a case control study comparing morbidity and morbidity after liver resection in undrained jaundiced patients and matched patients without biliary obstruction 14. Our study showed that there were no differences for liver failure and mortality rates after liver resection in jaundiced and non-jaundiced patients. However, transfusion requirements and morbidity rate were significantly higher in patients with obstructive jaundice. Significant differences in postoperative complications included bile leaks and subphrenic abcesses, which occurred more frequently in jaundiced patients and accounted for increased hospital stay. The overall morbidity rate of 50% after liver resection in jaundiced patients was significantly higher than the 15% observed in non-jaundiced patients. This is probably secondary to dilatation of intrahepatic bile ducts and opening the intestinal tract. However, the incidence of bile leaks and subphrenic collections compared with those reported in patients having undergone PBD in whom bile infection secondary to PBD might represent an additional risk factor.
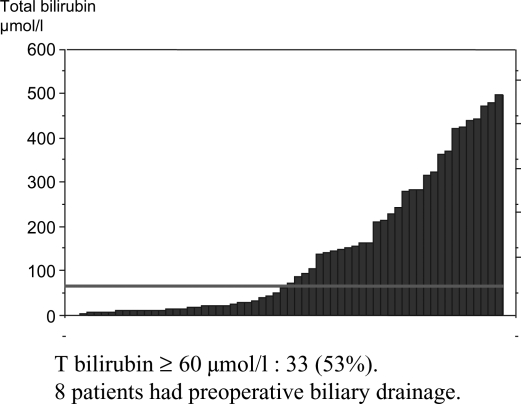
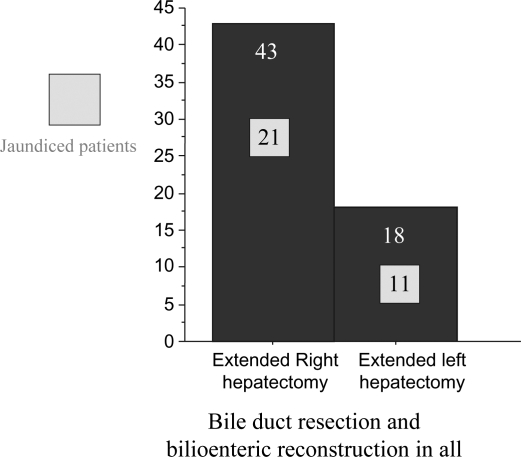
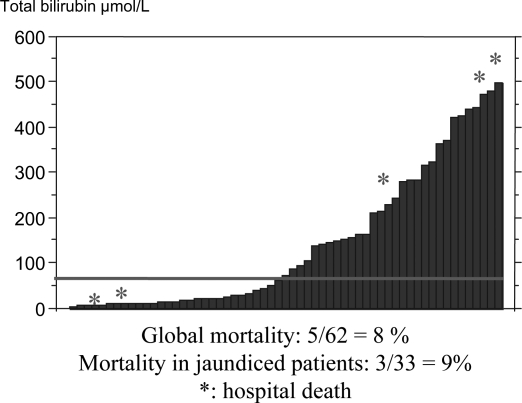
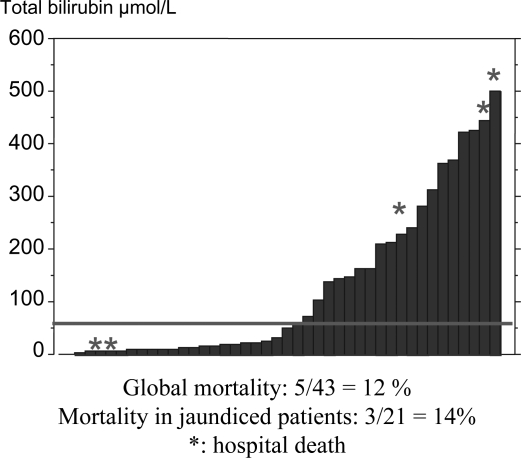
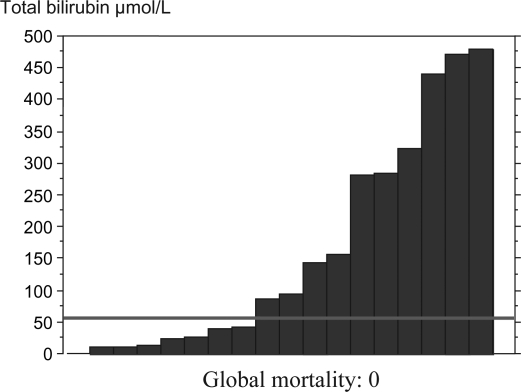
In the same study, the rate of liver failure in jaundiced patients was low (5%) and recovery of liver synthetic function, assessed by prothrombin activity, was identical to that of non-jaundiced patients. The mortality rate of 5% was also comparable to that reported after liver resection following PBD. Update of our series included 62 patients who had resection of hilar cholangiocarcinoma (Figure 1). Of these, 33 (52%) had a bilirubin level higher than 3 times the upper normal value at the time of surgery. All patients underwent major resection, including extended right hepatectomy in 43 cases and extended left in 18 (Figure 2). There were 5 deaths (8%) (Figure 3). All deaths occurred after extended right hepatectomy, including 3 patients with a serum bilirubin level above 300 µmol/l and 2 with normal bilirubin (Figure 4). There was no death after extended left hepatectomy, although this group included a majority of jaundiced, several with a bilirubin above 300 µmol/l (Figure 5).
Figure 1. .
Updated series: 62 patients with cholangiocarcinoma.
Figure 2. .
Operations performed.
Figure 3. .
Hospital mortality of the global series.
Figure 4. .
Hospital mortality of extended right hepatectomies.
Figure 5. .
Hospital mortality of extended left hepatectomies.
While we do not recommend routine use of PBD, there are cases where it is required. These are patients with a future liver remnant of less than 40% of total volume, those with cholangitis, long-standing jaundice, denutrition and hypoalbuminemia.
If PBD is used, it should drain the future remnant liver, and surgery should be scheduled after bilirubin is below twice the normal value. In the event of cholangitis or long duration drainage, PBD tubes should be changed. When the future remnant liver is deemed too small, preoperative portal vein embolization is indicated to induce hypertrophy of the future remnant liver, and preliminary PBD is required.
Conclusions
In conclusion, PBD is associated with specific complications, including sepsis and to a lesser extent, tumor seeding. It should not be performed systematically and specialized surgical evaluation should be performed before any type of direct cholangiography or PBD is performed.
PBD can be omitted in the following situations: recent onset jaundice (<2–3 weeks), total bilirubin <200 µmol/l, absence of sepsis, future liver remnant >40%.
These criteria include most patients requiring left-sided resections and selected patients requiring right-sided resections. In other cases, PBD is required, associated with portal vein embolization in the event of a small future liver remnant.
References
- 1.Nagino M, Nimura Y, Kamiya J, Kondo S, Kanai M, Miyachi M, et al. Preoperative management of hilar cholangiocarcinoma. J Hepatobil Pancreat Surg. 1995;2:215–23. [Google Scholar]
- 2.Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808–18. doi: 10.1097/00000658-199912000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. “Anatomic” right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg. 2006;243:28–32. doi: 10.1097/01.sla.0000193604.72436.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Miyagawa S, Makuuchi M, Kawasaki S. Outcome of extended right hepatectomy after biliary drainage in hilar bile duct cancer. Arch Surg. 1995;130:759–63. doi: 10.1001/archsurg.1995.01430070081016. [DOI] [PubMed] [Google Scholar]
- 5.Seyama Y, Makuuchi M. Current surgical treatment for bile duct cancer. World J Gastroenterol. 2007;13:1505–15. doi: 10.3748/wjg.v13.i10.1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hatfield AR, Tobias R, Terblanche J, et al. Preoperative external biliary drainage in obstructive jaundice. A prospective controlled clinical trial. Lancet. 1982;2:896–9. doi: 10.1016/s0140-6736(82)90866-2. [DOI] [PubMed] [Google Scholar]
- 7.Lai EC, Mok FP, Fan ST, et al. Preoperative endoscopic drainage for malignant obstructive jaundice. Br J Surg. 1994;81:1195–8. doi: 10.1002/bjs.1800810839. [DOI] [PubMed] [Google Scholar]
- 8.McPherson GA, Benjamin IS, Hodgson HJ, et al. Pre-operative percutaneous transhepatic biliary drainage: the results of a controlled trial. Br J Surg. 1984;71:371–5. doi: 10.1002/bjs.1800710522. [DOI] [PubMed] [Google Scholar]
- 9.Pitt HA, Gomes AS, Lois JF, et al. Does preoperative percutaneous biliary drainage reduce operative risk or increase hospital cost? Ann Surg. 1985;201:545–53. doi: 10.1097/00000658-198505000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith RC, Pooley M, George CR, et al. Preoperative percutaneous transhepatic internal drainage in obstructive jaundice: a randomized, controlled trial examining renal function. Surgery. 1985;97:641–8. [PubMed] [Google Scholar]
- 11.Sewnath ME, Karsten TM, Prins MH, Rauws EJ, Obertop H, Gouma DJ. A meta-analysis on the efficacy of preoperative biliary drainage for tumors causing obstructive jaundice. Ann Surg. 2002;236:17–27. doi: 10.1097/00000658-200207000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hochwald SN, Burke EC, Jarnagin WR, Fong Y, Blumgart LH. Association of preoperative biliary stenting with increased postoperative infectious complications in proximal cholangiocarcinoma. Arch Surg. 1999;134:261–6. doi: 10.1001/archsurg.134.3.261. [DOI] [PubMed] [Google Scholar]
- 13.Sakata J, Shirai Y, Wakai T, Nomura T, Sakata E, Hatakeyama K. Catheter tract implantation metastases associated with percutaneous biliary drainage for extrahepatic cholangiocarcinoma. World J Gastroenterol. 2005;11:7024–7. doi: 10.3748/wjg.v11.i44.7024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cherqui D, Benoist S, Malassagne B, Humeres R, Rodriguez V, Fagniez PL. Major liver resection for carcinoma in jaundiced patients without preoperative biliary drainage. Arch Surg. 2000;135:302–8. doi: 10.1001/archsurg.135.3.302. [DOI] [PubMed] [Google Scholar]