Abstract
The Pembersal operation combines features of the Pemberton and Salter osteotomies. Results have usually been reported in patients with dysplasia but without frank dislocation. We asked if the following factors influence the outcome of the Pembersal operation in patients with dislocated hips: triradiate cartilage damage causing early closure; the acetabular index improvement; and the age of the patient at time of operation. We assessed triradiate cartilage damage, a modified McKay clinical classification, acetabular index, center-edge angles, Reimers index, acetabular depth-to-width ratios, Severin classification and Tönnis grading of 33 patients (44 hips) have been evaluated in this retrospective study. The mean age at surgery was 5 years (range, 1.5–14 years). The minimum followup was 5 years (mean, 10.5 years; range, 5–17 years). Preoperatively, three (7%) hips were Tönnis Grade 2, 10 (23%) were Grade 3, and 31 (70%) were Grade 4. Eight (18%) hips were Severin Class 1, 32 (73%) Class 2, and four (9%) were Class 3. According to McKay’s criteria satisfactory results with a rate of 76% were obtained. Premature closure of the triradiate cartilage occurred in eight (18%) hips and postoperative avascular necrosis of the femoral head in three (6%) hips. Satisfactory clinical and radiographic improvements in the aforementioned parameters can be obtained by Pembersal osteotomy.
Level of Evidence: Level IV, therapeutic case series. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Developmental dysplasia of the hip is one of the most common orthopaedic problems seen during childhood with reported incidences of 1 per 1,000 to 3.4 per 100 [8, 21]. Numerous surgical procedures for DDH have been described [5, 6, 23, 30]. Most surgeons are familiar with procedures described by Salter [22] in 1961 and by Pemberton [17] in 1965. Salter and Dubos [22, 23] described a transiliac innominate osteotomy in which the lower quarter of the pelvis is rotated forward, downward, and outward, that reoriented the acetabulum anterolaterally, thereby increasing the coverage of the femoral head. Pemberton [17] described an acetabuloplasty in which the ilial osteotomy ends at the posterior limb of the triradiate cartilage and the anterolateral rim of the acetabulum is hinged downward and laterally. Pemberton’s rationale was that “the axis of rotation should be within the acetabulum” and apparently not at the edge (i.e., the center of the triradiate cartilage. The asymmetry of the obturator foramina, as seen in both procedures, suggests rotation of the inferior quadrant of the pelvis.
A combined pelvic osteotomy (“Pembersal”) was described in 1985 by Perlik et al. [18]. The osteotomy combines key aspects of the Pemberton (pericapsular) and the Salter (innominate) osteotomies. The osteotomy avoids the center of the triradiate cartilage and is directed from the ilium extending into the ischial body across the posterior ilioischial limb of the triradiate cartilage, allowing the rotation of the lower part of the pelvis in addition to bending the acetabular roof at the triradiate cartilage [18]. Since 1989 we have been performing this so-called Pembersal operation. In contrast to some previously described series, 93% of the hips on which we have operated were frankly dislocated at the time of the initial surgery rather than merely dysplastic.
We asked whether: (1) there was any triradiate cartilage damage causing early closure; (2) the acetabular index could be substantially improved via the combined osteotomy; and (3) the age at surgery influenced various radiographic features ostensibly reflecting outcomes (acetabular index, the center-edge angles, the Reimers index, the acetabular depth-to-width ratios, the Severin classification, the Tönnis grading and the McKay’s criteria).
Materials and Methods
We retrospectively reviewed the records of 90 consecutive patients (115 hips) who underwent Pembersal pelvic osteotomy for DDH between 1989 and 1997. We excluded patients with inadequate records and short followup (n = 18), neuromuscular disorders (n = 2), connective tissue disorders (n = 3), or patients with previous hip surgery (n = 7). We were able to locate 33 patients (44 hips) (37% of the patients) with full documentation who could be contacted for followup. The mean age at the time of surgery was 5 years (range, 1.5–14 years). We separated our patients into two groups according to the age at which they were operated: younger (Group 1) and older (Group 2) than 4 years. There were 29 female and four male patients. Nineteen hips were on the right side and 25 were on the left. Eleven patients had bilateral dysplasia. The minimum followup time for the 37 patients included was 5 years (mean, 10.5 years; range, 5–17 years).
Preoperatively the patients were examined by the operating surgeon (AB). Clinical parameters such as pain, range of motion of the affected and the contralateral hips, instability, limp and Trendelenburg sign were collected. Anteroposterior (AP) radiographs of the pelvis were taken and the hips classified according to Tönnis [29]. According to this classification, Grade 1 means the cartilaginous head of the femur is laterally displaced by no more than 2/3 of its width (relative to the superior bony rim of the acetabulum). In Grade 2, the femoral head is laterally displaced by more than 2/3 of its width. If the femoral head is displaced upward by more than 1/3 of its height relative to the cartilaginous rim of the acetabulum, it is Grade 3. In Grade 4, the femoral head is completely dislocated and is separated from the acetabulum by the labrum or the constricted capsule. Preoperatively, according to Tönnis classification, three (7%) of the hips were Grade 2, 10 (23%) were Grade 3, and 31 (70%) were Grade 4.; thus 93% of the hips were dislocated at the time of the index operation. We further measured the acetabular index. The acetabular index of Hilgenreiner is formed by a line drawn from a point at the lower lateral edge of the ilium on the triradiate cartilage connected to the horizontal line of Hilgenreiner, and a second line drawn from the point on the ilium to the superior acetabular rim [9].
The surgical technique used was originally described by Perlik et al. [18] (Pembersal). All procedures were performed by the same surgeon (AB). The ilium was exposed subperiosteally through an anterior iliofemoral approach. Then the iliopsoas tenotomy was performed through its tendinous portion at the level of the triradiate cartilage, and an arthrotomy to inspect the joint cavity for the need of débridement of the pulvinar and assessment of the reduction was routinely performed. Neither excision nor radial incision of the labrum was performed. Subtrochanteric femoral shortening was performed via a lateral proximal femoral incision when the hips were classified as grade 3 and 4 according to Tönnis [29]. Thirty-one femurs (70%) were shortened an average of 2.5 cm (range, 1.5–7 cm). Pelvic osteotomy was performed 10 to 15 mm above the anterior inferior iliac spine to the body of the ischium, following the attachment of the joint capsule and paralleling the acetabular dome. To avoid entering the joint, an index finger was introduced into the acetabulum during the osteotomy. This osteotomy differs from the Pemberton procedure in that it continues through the ilioischial limb of the triradiate cartilage but not through the distal cortex. Opening the osteotomy creates a greenstick fracture through the remaining part of the ischial body. The lower quarter of the body was displaced forward and downward, resulting in anterolateral rotation of the acetabulum about an axis that passes through the ischial fracture and the symphysis pubis. And also, the acetabular roof was rotated downward and laterally with the triradiate cartilage acting like a hinge. As a result, the acetabulum was reoriented as in the Salter procedure, and deepened as in the Pemberton osteotomy. A triangular, curved bone graft was taken from the patient’s ipsilateral iliac crest and wedged into the osteotomy site. Because the osteotomy and the interposed graft are adequately stable we used no internal fixation.
Patients were kept in a 1½ spica cast for 6 weeks postoperatively. After removal of the cast, an abduction orthosis was applied for an additional 6 weeks. Range of motion exercises then began and weight bearing resumed as tolerated without any assisting device, such as crutches or walkers.
We (AB, MT) performed radiographic examinations just after the first intervention at the 6th and 12th weeks and 1 year after the operation. Additionally, after cast removal, clinical examinations were performed at the 6th and 12th weeks and 1 year after the operation. At the last followup all the patients were reevaluated clinically and radiographically by the same surgeon (AB). The patients were clinically evaluated according to the modified McKay’s criteria which consist of pain, range of motion of the affected and the contralateral hips, instability, limp and Trendelenburg sign (Table 1) [2]. We evaluated patients radiographically according to Severin’s criteria (Table 2) [25]. At the last followup the acetabular roof obliquity angle, the center-edge angle of Wiberg, the Reimers index and the acetabular depth-to-width ratios were also measured as radiographic parameters [7, 9, 12, 16, 20].
Table 1.
Modified criteria of McKay for clinical evaluation of results [2]
| Grade | Rating | Description |
|---|---|---|
| I | Excellent | Painless, stable hip; no limp, more than 15 degrees of internal rotation; negative Trendelenburg sign |
| II | Good | Painless, stable hip; slight limp, slight decrease in hip motion; negative Trendelenburg sign |
| III | Fair | Minimum pain; moderate stiffness; positive Trendelenburg sign |
| IV | Poor | Significant pain |
Table 2.
Severin’s criteria for radiographic evaluation of results [25]
| Class | Description | Center-edge angle [16] (degrees) |
|---|---|---|
| I | Normal appearance | ≥ 15 (5–13 yrs.) |
| ≥ 20 (>14 yrs.) | ||
| II | Mild deformity of the femoral head and neck or the acetabulum | ≥ 15 (5–13 yrs.) |
| ≥ 20 (> 14 yrs.) | ||
| III | Dysplasia or moderate deformity of the femoral head and neck or the acetabulum, or both | < 15 (5–13 yrs.) |
| < 20 (> 14 yrs.) | ||
| IV | Subluxation of the femoral head | |
| V | Articulation of the femoral head with a false acetabulum | |
| VI | Redislocation |
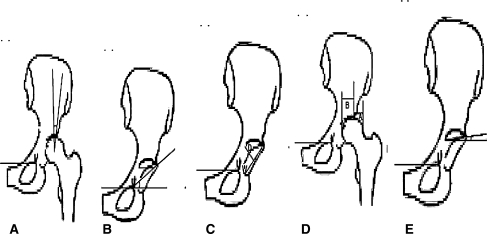
The acetabular index of Hilgenreiner is formed by a line drawn from a point at the lower lateral edge of the ilium on the triradiate cartilage connected to the horizontal line of Hilgenreiner, and a second line drawn from the point on the ilium to the superior acetabular rim [9]. The acetabular roof obliquity is used instead of acetabular index at the last followup as the patients were skeletally mature. This was the angle subtended by the line connecting the inferior-most edge of the roof of the acetabulum to the lateral-most edge of the acetabulum with a parallel horizontal line [12]. The center-edge angle of Wiberg is formed by a line parallel to the longitudinal body axis and by the line connecting the center of the femoral head (C) with the edge (E) of the acetabular roof [16]. The width of the femoral head parallel to Hilgenreiner’s line is measured as line (b), and the distance (a) from the lateral border of the femoral head to the Ombrédanne-Perkins line. The ratio (a/b)*100 assigns a percentage value to the degree of centering of the femoral head. This is the “Instability Index of Reimers” [20]. The acetabular depth-to-width ratios are measured in the following manner: the width of the acetabulum is measured from the most lateral point of the superior acetabular rim to the lower margin of the acetabulum (b), the depth of the acetabulum is measured on the perpendicular bisector of the width line (a); (a/b)*100 gives the ratio [7] (Fig. 1).
Fig. 1.
The five morphological measurements for acetabular dysplasia are (A) center-edge angle, (B) acetabular index of Hilgenreiner, (C) the acetabular depth-to-width ratio, (D) instability index of Reimers, and (E) acetabular roof obliquity.
We used the Wilcoxon test to determine differences between the mean preoperative and last followup acetabular index. The Mann-Whitney U test was used to determine differences in the parametric values (preoperative acetabular index and followup acetabular roof obliquity angle, the center-edge angle, the Reimers index, and the acetabular depth-to-width ratio) between the groups. The chi-square test was used to evaluate the nonparametric values, such as the preoperative Tönnis grade, and the followup Severin and McKay criteria between the groups. All values were recorded on a Microsoft Excel spreadsheet. Analyses were made using Statistical Package for the Social Sciences (Windows 2000; SPSS Version 13, Chicago, Ill.). A p value of < 0.05 was considered significant.
Results
According to modified McKay’s clinical criteria at the last followup 17 (38%) hips were excellent (Grade I), 17 (38%) good (Grade II), nine (20%) fair (Grade III), and one (4%) poor (Grade IV), (Table 3). Using Severin radiographic classification at the last followup, there were eight (18%) Class 1 hips, 32 (73%) Class 2 hips, and four (9%) Class 3 hips.
Table 3.
Clinical and radiological results of patients preoperatively and at last followup
| Preoperative Tönnis grade | Preoperative AI (range) | Followup AO (range) | Followup Severin class | Followup McKay grade | Followup C-E angle (range) | Followup RI | Followup D/W ratio (%) |
|---|---|---|---|---|---|---|---|
| 31 hips; G 410 hips; G 33 hips; G 2 | 37.6°(25–60°) | 12.5°(10–32°) | 8 hips; C 132 hips; C 24 hips; C 3 | 17 hips; G I17 hips; G II9 hips; G III1 hip; G IV | 29.1° (11–48°) | 0.18 (0–0.46) | 42.3 (25–59) |
| p < 0.05 | |||||||
AI = acetabular index; AO = acetabular roof obliquity angle; C-E = center-edge angle; RI = Reimers index; D/W = acetabular depth-to-width ratio.
Premature closure of the triradiate cartilage occurred in eight (18%) hips. These eight hips were in patients on whom we had operated early in our series.
The average acetabular index had decreased (t = 5.16, p < 0.05) from 37.6° (range, 25°−60°) preoperatively to 12.5° (range, 10°−32°) at the last followup.
The clinical outcomes as rated by McKay’s criteria, were similar (p > 0.05) in both groups. However, younger patient age at operation resulted in better radiological outcomes. The averages of the preoperative and followup acetabular index/roof obliquity angle, the followup center-edge angles were greater (p < 0.05) in group 1 than group 2, whereas the Reimers index, and the acetabular depth-to-width ratios were lesser in group 1 than in group 2 (p < 0.05 and, p = 0.0475, respectively) (Table 4). The preoperative and last followup Severin classifications and Tönnis grading between age groups improved (15 mild to moderate deformities according to Severin classification in group 1, and 21 in group 2; p < 0.05, 10 complete dislocation in group 1 versus 21 in group 2; p < 0.01) (Table 4). The patients illustrate these differences (Figs. 2–4).
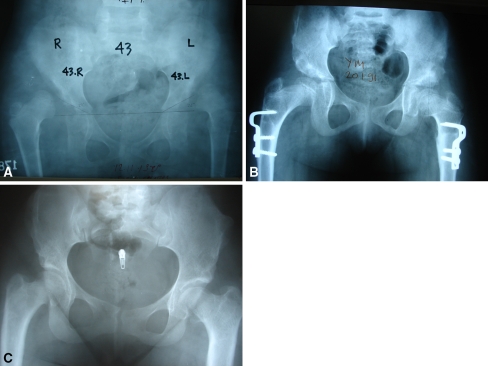
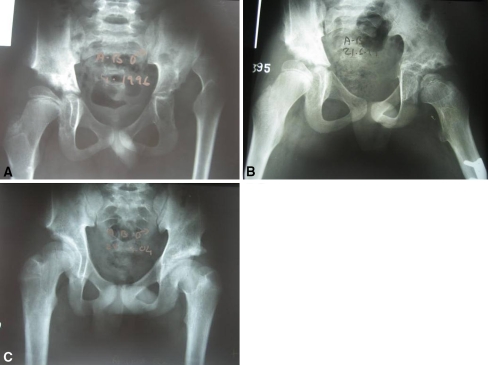
Fig. 3A–C.
A male patient was operated bilaterally at age 6. Femoral shortening of 2 cm was performed on the right side. (A) At initial presentation both hips were Tönnis Grade 4. Preoperative acetabular indices were 40° on the right side and 36° on the left. (B) An early followup radiograph is shown. He was followed for 15 years. (C) At the last control, he was pain-free. Radiographically, the acetabular indices were 10° bilaterally, the center-edge angles were 25° and 35°, the Reimers indices were 0.24 and 0.16, and the acetabular depth-to-width ratios were 59% and 43% at the right and left hips, respectively. Both hips were Class 2 according to Severin, and excellent according to modified McKay’s criteria.
Table 4.
Clinical and radiological results of patients according to age at operation preoperatively and at last followup
| Preop Tonnis grade | Preop AI (range) | Followup AO (range) | Followup Severin class | Followup MacKay criteria | Followup CE angle (range) | Followup RI (range) | Followup D/W (range) |
|---|---|---|---|---|---|---|---|
| 10→ 4 | 38.77° (25–60°) | 10.27° (0–26°) | 7→ 1 | E→ 10 | 30.54° (11–46°) | 0.16 (0–0.33) | 42.14% (31–55) |
| 9→ 3 | 14→ 2 | G→ 9 | |||||
| 3→ 2 | 1→ 3 | F→ 3 | |||||
| 21→ 4 | 36° (24–50°) | 15.23° (0–32°) | 1→ 1 | E→ 8 | 28.54° (14–48°) | 0.20 (0–0.46) | 42.36 (25–59) |
| 1→ 3 | 18→ 2 | G→7 | |||||
| 3→ 3 | F→ 6 | ||||||
| P→ 1 | |||||||
| x² = 13.302, p < 0.01 | U = 292, p < 0.05 | U = 335, p < 0.05 | x² = 6, p < 0.05 | x² = 2.821, p > 0.05 | U = 285, p < 0.05 | U = 315, p < 0.05 | U = 265, p = 0.0475 |
AI = acetabular index; AO = acetabular roof obliquity angle; C-E = center-edge angle; RI = Reimers index; D/W = acetabular depth-to-width ratio; Bold = Group 1 (22 hips), age range, 1.5–4 years; Italic = Group 2 (22 hips), age range, 5–14 years; E = excellent; G = good; F = fair; P = poor).
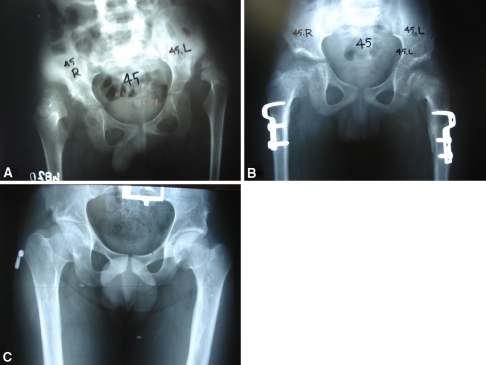
Fig. 2A–C.
A female patient was operated bilaterally (right hip at age 7 years and left at 8 years). Femoral shortening was performed bilaterally (2 cm at the right femur and 2.5 cm at the left). (A) At initial presentation both hips were Tönnis Grade 4. Preoperative acetabular index was 46° at the right site and 40° at the left. (B) An early followup radiograph is shown. She was followed for 17 years. (C) At the last followup, she was pain-free, had no limping, and was able to perform all daily activities with no limitation. Radiographically, the acetabular indices were 15° and 8°, the center-edge angles were 23° and 32°, the Reimers indices were 0.15 and 0.13, and the acetabular depth-to-width ratios were 46% at both the right and left hips. Both hips were Severin Class 2, excellent according to modified McKay’s criteria.
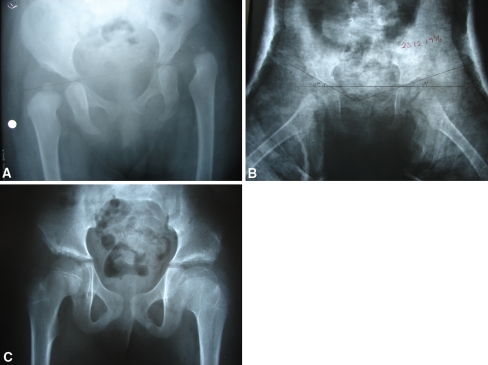
Fig. 4A–C.
The left hip of this female patient was operated at age 1.5 years. (A) In this preoperative radiograph, her hip was Tönnis Grade 3 initially. Preoperative acetabular index was 42°. (B) A radiograph immediately postoperative is shown. She was followed for 9 years. (C) At the last followup, she was pain-free with no limitation of hip range of motion. Radiographically, the acetabular index was 13°, the center-edge angle was 30°, the Reimers index was 0.16, and the acetabular depth-to-width ratio was 50%. The hip was Class 2 according to Severin, and excellent according to modified McKay’s criteria.
Complications occurred in 11 hips (10 patients): postoperative avascular necrosis of the femoral head in three (6%) hips and premature closure of the triradiate cartilage in eight (18%) hips. There were no redislocations, graft displacements, or infections. In one patient the osteotomy entered the joint, which was detected postoperatively by radiographs. At the last followup the hip radiographically was Severin Class 3 and clinically Grade II (good) according to modified McKay’s criteria (Fig. 5).
Fig. 5A–C.
The left hip of this male patient was operated at age 10 years. (A) In this preoperative radiograph, his hip was Tönnis grade 4 initially. Preoperative acetabular index was 26°. Femoral shortening of 2.5 cm was performed. (B) An early followup radiograph is shown (note the obvious premature closure of the left triradiate cartilage compared to the right). He was followed for 15 years. (C) At the last control, he was pain-free. Radiographically, the acetabular index was 20°, the center-edge angle was 30°, the Reimer’s index was 0.20, and the acetabular depth-to-width ratio was 45%. The hip was Class 2 according to Severin, and excellent according to modified McKay’s criteria.
Discussion
The Pembersal procedure combines features of the Salter osteotomy and the Pemberton acetabuloplasty. By performing this procedure, we asked if acetabular remodeling would be improved, thus promoting congruous and concentric normal hip development. Iatrogenic damage of the triradiate cartilage is the most discouraging complication of the Pembersal procedure, which may lead to unsuccessful results. We asked whether (1) there was any triradiate cartilage damage causing early closure; (2) the acetabular index could be substantially improved via the combined osteotomy; and (3) the age at surgery influenced various clinical and radiographic outcomes.
The major limitation of this study is the loss of patients to followup. This is due to the social security insurance system in our country. Most of our patients join this system only for a short period, during which time they address their health problems. However, they quit paying for insurance after surgery and lose their rights for further followup. This decreases the numbers of patients followed up, which is only 33 of 90 (37%) patients in our series. Although only one-third of the patients overall were evaluated, we presume those who maintain insurance and followup are similar to those who for primarily financial reasons do not.
Several authors have reported 71% to 94% major improvement in parameters such as the acetabular index, the center-edge angles, the Reimers index, the acetabular depth-to-width ratios, the Severin classification, the Tönnis grading and the McKay’s criteria of a Salter osteotomy with a mean followup of 5.5 to 30.9 years [1, 3, 6, 11, 23, 30] (Table 5). Complication rates, including bone graft displacement, migration of the K-wire, redislocation, hip flexion and abduction contractures, and avascular necrosis of the femoral head, were reported as an overall 30% by Bohm and Brzuske [3] 63.3% by Gulman et al. [5], and 6% by Hosny and Fattah [10].
Table 5.
Comparison of techniques
| Author | Year | Technique | Number of hips | Minimum followup (years) | Age at surgery (years) | % Severin’s I + II | Other factors reported |
|---|---|---|---|---|---|---|---|
| Gulman et al. [5] | 1994 | Salter | 52 | 8 years (mean, 13; range, 8–25) | Majority 1.5 to 4 years | 71 | |
| Karakas et al. [11] | 1995 | Salter | 55 | 2 years (mean, 7.5; range, 2–16) | 7.8 years | 65.4 | Shortening |
| Morin et al. [14] | 1998 | Salter | 122 | 3 years (mean, 12; range, 3–27) | 5.4 years | 70 | Shortening |
| Bohm and Brzuske [3] | 2002 | Salter | 73 | 26.2 years (mean, 30.9; range, 26.2–35.4) | 4.1 years | 88 | |
| Szepesi et al. [27] | 1996 | Pemberton | 80 | 1 year (mean, 5.3; range, 1–15) | 4.4 years | 79 | Shortening |
| Wada et al. [31] | 2003 | Pemberton | 17 | 5 years (mean, 9.4; range, 5–17.4) | 9.3 years | 76 | Previously operated |
| Thielemann et al. [28] | 2003 | Pemberton | 100 | 10.4 years (mean, 14.7; range, 10.4–19.5) | 4.4 years | 95.9 | |
| Perlik et al. [18] | 1985 | Combined Pelvic Osteotomy | 50 | 2 years (mean, 6; range, 2–18.8) | 7.3 years | 66 | Previously operated (in 62%) |
| Our series | 2007 | Pembersal | 44 | 5 years (mean, 10.5; range, 5–17 years) | 5.2 years | 91 | Shortening (in 70%) |
Pemberton and several others [17, 27, 28, 31] reported major improvements in parameters such as the acetabular index, the center-edge angles, the Reimers index, the acetabular depth-to-width ratios, the Severin classification, the Tönnis grading and the McKay’s criteria using Pemberton acetabuloplasty with rates of 83% to 96% with a mean followup of 5.3 to 14.6 years (Table 2). Complication rates were reported as an overall 0 to 5.5% in different series [4, 27], and complications included iliac bone fracture over the osteotomy, bone graft displacement, and mild paresis due to sciatic nerve injury.
Perlik et al. [18] reviewed their series of 50 hips in 44 children, 62% of whom had prior surgery. The patients underwent the Pembersal operation at a mean age of 7.3 years and had a mean followup of 6 years. They reported 54% satisfactory improvements in radiological parameters such as the acetabular index, the center-edge angle, the Reimers index, the acetabular depth-to-width ratios and clinically in McKay’s criteria and Tönnis grading and a 6% complication rate, including one graft displacement and two mild infections.
The recommended ages for Salter and Pemberton osteotomies are 1.5–6 and 1.5–14 years, respectively [17, 23]. Perlik et al. reported their range for combined pelvic osteotomy as 3 years and 8 months to 12 years and 8 months [18]. In our series the range for the Pembersal operation was 1 year and 6 months to 14 years. Our series differs from those in previous studies (Table 5) because we have performed the procedure as a primary attempt and 93% of the hips were dislocated, in contrast with the previous series in which all of the hips were dysplastic.
Premature closure secondary to injury of the triradiate cartilage results in a shallow dysplastic acetabulum [19]. The extent of the deformity depends on the patient’s age at injury and the specific area involved. Several authors reported premature triradiate cartilage closure after different types of pelvic osteotomies with satisfactory clinical results [13, 14, 19, 26]. They concluded acetabuloplasties performed adjacent to the triradiate cartilage typically do not have an adverse effect on its functions, but despite the low-risk injury long-term followup was recommended. They added premature closure was most likely to occur if the bone graft used to maintain the fragment displacement crossed the triradiate cartilage. The graft may cause a fusion effect. Special attention to the ilioischial limb is of great importance because this portion has the greatest potential of growth of the triradiate cartilage and its injury may cause deformation and subluxation of the hip joint [24]. The eight hips in which we identified premature closer were in patients on whom we had operated early in our series. As we gradually became more skillful, we manipulated gently and more carefully in order not to harm the triradiate cartilage. However, this combined pelvic osteotomy is potentially harmful to the cartilage and therefore the younger patients (≤ 4 years) tolerated it better than the older group.
Perlik et al., however, could not demonstrate premature closure of the posterior limb of the triradiate cartilage in his series and noted it was difficult to identify in the followup roentgenograms [18]. After physiological closure of the triradiate cartilage, the acetabular roof is less flexible, and presumably the Pemberton component of the procedure contributes less to the correction [18]. Additionally, violation of the growth center might be expected to cause premature closure; as Pemberton suggested, it does not appear to cause substantial problems and alter the final results [17].
The mean preoperative acetabular index and the mean followup acetabular roof obliquity angle, the center-edge angle of Wiberg, were greater in group 1 than group 2, whereas Reimers index and acetabular depth-to-width ratios were lesser in group 1 than in group 2. Based on these results, we tried to predict the ideal timing of the operation in order to obtain good clinical and radiographic results. Although the radiographic results were better in the younger age group, the clinical results were similar in both age groups.
In our series at the last followup, we detected radiographic dysplasia in 18% of the hips (six patients, eight hips) perhaps due to premature closure of the triradiate cartilage and likely reflecting iatrogenic damage. This damage may be because of the wide exposure of the iliac bone affecting the remodeling capacity of the triradiate cartilage or forced correction may be damaging the triradiate physis. Also, the graft crossing the triradiate cartilage may cause a fusion effect, as previously mentioned. One of these patients was 1.5 years old at the time of surgery, and the mean age of the other five patients was 8.8 years (range, 6–11 years). This implies the main cause for further dysplasia may not only be the iatrogenic damage to the triradiate cartilage, but also that, after age 4, wide exposure is needed to visualize the field and manipulate the osteotome, the flexibility of the iliac bone is decreased, and the remodeling capacity is already diminished, as mentioned by Bohm and Brzuske [3]. Theoretically, the earlier the damage to the triradiate cartilage, the worse the acetabular dysplasia would be expected, whereas the femoral head may further induce the acetabulum to reshape and mold.
Murphy et al. [15] reported the acetabular index of depth-to-width in patients with hips that did not develop severe arthritis by the age of 65 had a mean value of 48%, whereas dysplastic acetabula in which secondary osteoarthritis was more likely to develop had an average depth-to-width ratio of 31%. In our series, the mean acetabular depth-to-width ratio, the Reimers index, and the center-edge angle in the younger age group was 42.1%, 0.16, and 30.5°, respectively. The same values in the elderly group were 42.4%, 0.20 and 28.5°, respectively. These data suggest the younger the patient at the time of operation, the better the radiological outcomes will be. However, followup until the later decades of life is required to ascertain whether the age at the operation influences the risk of OA.
Considering 93% of the hips were dislocated initially and more than 50% of the patients in our series were older than 5 years, we believe our clinical and radiographic results are satisfactory. However, the relatively high rate of triradiate cartilage damage may be avoided by skilled surgical technique.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution either has waived or does not require approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Barrett WP, Staheli LT, Chew DE. The effectiveness of the Salter innominate osteotomy in the treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1986;68:79–87. [PubMed]
- 2.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg Am. 1984;66:412–420. [PubMed]
- 3.Bohm P, Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg Am. 2002;84:178–186. [DOI] [PubMed]
- 4.Faciszewski T, Kiefer G, Coleman SS. Pemberton osteotomy for residual acetabular dysplasia in children who have congenital dislocation of the hip. J Bone Joint Surg Am. 1993;75:643–649. [DOI] [PubMed]
- 5.Gulman B, Tuncay IC, Dabak N, Karaismailoglu N. Salter’s innominate osteotomy in the treatment of congenital hip dislocation: a long-term review. J Pediatr Orthop. 1994;14:662–666. [DOI] [PubMed]
- 6.Harkess JW. Arthroplasty of the hip. In: Canale ST, ed. Campbell’s Operative Orthopaedics, 10th ed. Philadelphia, PA: Mosby; 2003:315–482.
- 7.Heyman CH, Herndon CH. Legg-Perthes disease: a method for the measurement of the roentgenographic results. J Bone Joint Surg Am. 1950;32:767–778. [PubMed]
- 8.Hiertonn T, James U. Congenital dislocation of the hip: experiences of early diagnosis and treatment. J Bone Joint Surg Br. 1968;50:542–545. [PubMed]
- 9.Hilgenreiner WH. Classic. Translation: Hilgenreiner on congenital hip dislocation. J Pediatr Orthop. 1986;6:202–214. [PubMed]
- 10.Hosny GA, Fattah HA. Salter’s innominate osteotomy: the biologic stimulating effect. J Pediatr Orthop B. 1998;7:150–153. [PubMed]
- 11.Karakas ES, Baktir A, Argun M, Turk CY. One-stage treatment of congenital dislocation of the hip in older children. J Pediatr Orthop. 1995;15:330–336. [DOI] [PubMed]
- 12.Massie WK, Howorth MB. Congenital dislocation of the hip. Part I. Methods of grading results. J Bone Joint Surg Am. 1950;32:519–531. [PubMed]
- 13.McKay DW. Pemberton’s innominate osteotomy: indications, technique, results, pitfalls, complications. In: Tachdjian MO, ed. Congenital Dislocation of the Hip. New York, NY: Churchill Livingstone; 1982:543–554.
- 14.Morin C, Rabay G, Morel G. Retrospective review at skeletal maturity of the factors affecting the efficacy of Salter’s innominate osteotomy in congenital dislocated, subluxed and dysplastic hips. J Pediatr Orthop. 1998;18:246–253. [DOI] [PubMed]
- 15.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip: a study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. [DOI] [PubMed]
- 16.Ömeroglu H, Bicimoglu A, Agus H, Tumer Y. Measurement of center-edge angle in developmental dysplasia of the hip: a comparison of two methods in patients under 20 years of age. Skeletal Radiol. 2002;31:25–29. [DOI] [PubMed]
- 17.Pemberton PA. Pericapsular osteotomy of the ilium for treatment of congenital subluxation and dislocation of the hip. J Bone Joint Surg Am. 1965;47:65–86. [PubMed]
- 18.Perlik PC, Westin GW, Marafioti RL. A combination pelvic osteotomy for acetabular dysplasia in children. J Bone Joint Surg Am. 1985;67:842–850. [PubMed]
- 19.Plaster RL, Schoenecker PL, Capelli AM. Premature closure of the triradiate cartilage: a potential complication of pericapsular acetabuloplasty: case report. J Pediatr Orthop. 1991;11:676–678. [PubMed]
- 20.Reimers J. The stability of the hip in children: a radiological study of the results of muscle surgery in cerebral palsy. Acta Orthop Scand Suppl. 1980;184:1–100. [DOI] [PubMed]
- 21.Rosendahl K, Markestad T, Lie R. Developmental dysplasia of the hip: a population-based comparison of ultrasound and clinical findings. Acta Paediatr. 1996;85:64–69. [DOI] [PubMed]
- 22.Salter RB. The classic: innominate osteotomy in the treatment of congenital dislocation, subluxation of the hip by Robert B. Salter J Bone Joint Surg (Brit) 43B:3:518, 1961. Clin Orthop Relat Res. 1978;137:2–14. [PubMed]
- 23.Salter RB, Dubos JP. The first fifteen years’ personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. 1974;98:72–103. [DOI] [PubMed]
- 24.Scuderi G, Bronson MJ. Triradiate cartilage injury: report of two cases and review of the literature. Clin Orthop Relat Res. 1987;217:179–189. [PubMed]
- 25.Severin E. Congenital dislocation of the hip: development of the hip after reduction. J Bone Joint Surg Am. 1950;32:507–518. [PubMed]
- 26.Soini J, Ritsila V. Experimentally produced growth disturbance of the acetabulum in young rabbits. Acta Orthop Scand. 1984;55:14–17. [DOI] [PubMed]
- 27.Szepesi K, Rigo J, Biro B, Fazekas K, Poti L. Pemberton’s pericapsular osteotomy for the treatment of acetabular dysplasia. J Pediatr Orthop B. 1996;5:252–258. [PubMed]
- 28.Thielemann F, Schneider A, Köhler T, Dürrschmidt V, Günther KP. The pericapsular osteotomy of the ilium (Pemberton) in combination with a derotation and varisation osteotomy of the proximal femur: results after the end of the maturity process. Z Orthop. 2003;141:459–464. [DOI] [PubMed]
- 29.Tönnis D. An evaluation of conservative and operative methods in the treatment of congenital hip dislocation. Clin Orthop Relat Res. 1976;119:76–88. [PubMed]
- 30.Utterback TD, MacEwen GD. Comparison of pelvic osteotomies for the surgical correction of the congenital hip. Clin Orthop Relat Res. 1974;98:104–110. [DOI] [PubMed]
- 31.Wada A, Fujii T, Takamura K, Yanagida H, Taketa M, Nakamura T. Pemberton osteotomy for developmental dysplasia of the hip in older children. J Pediatr Orthop. 2003;23:508–513. [DOI] [PubMed]