Abstract
Postoperative alignment of the implanted prosthesis in computer-navigated TKA has been reported to be superior to that using the conventional technique. There is an assumption that use of computer navigation techniques can make an inexperienced or occasional TKA surgeon perform more like an expert TKA surgeon. To assess improved accuracy in recreation of mechanical alignment in TKA performed using computer navigation, a retrospective review of the experience of one of the authors (WPY) before and after using computer navigation was performed. We reviewed the radiographic results of 104 TKAs (52 computer navigation, 52 conventional technique) and found the accuracy of postoperative radiographic alignment of the implanted prosthesis was not improved by using computer navigation as judged by (1) overall limb alignment (case: varus 1.3°; control: varus 0.3°); (2) femoral component alignment (case: 90.3°; control: 90.3°); and (3) tibial component alignment (case: 89°; control: 90°). Significant factors that affected postoperative overall mechanical alignment in the current navigation series included severity of the preoperative deformity, amount of error in making bone cuts, and experience of the surgeon in using the computer navigation system.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Malalignment in TKA can lead to early mechanical failure of the prosthesis [11, 27]. It is recommended that the limb should be aligned so that the two compartments of the TKA are loaded evenly [14, 15]. The postoperative mechanical axis of the lower limb should be a straight line passing through the center of the hip, the center of the knee, and the center of the ankle. However, some authors agree this objective may not be practically obtainable in every TKA [15]. Satisfactory position of a TKA prosthesis is commonly accepted to be an alignment within 3° from this ideal [1, 6, 7, 12, 17, 18, 22, 23, 28, 33]. Aseptic loosening of the prosthesis has been reported to be more common in knees implanted in an alignment greater than 3° varus [26].
Radiographic alignment of the implanted prosthesis in navigated TKA is reported to be superior to that performed by conventional instrumentation [1, 2, 4, 6–8, 12, 13, 17, 20–23, 25, 28, 29, 34]. If an outlier in the lower limb mechanical alignment is defined as greater than 3° from the neutral position, the majority of the TKA series performed using the conventional jig-based technique reported a satisfactory alignment rate of approximately 70% [1–3, 5–10, 12, 13, 16–24, 28, 29, 31–34]. However, the results of most of the computer navigation TKA series were much more favorable, reporting satisfactory alignment of 90% to 100% [1, 17, 22, 23, 28, 29, 34]. Some surgeons have suggested this improved predictability of postoperative radiographic alignment with computer navigation TKA occurs with experienced and inexperienced surgeons [30]. This leads to the assertion that use of the computer navigation technique in TKA can make the inexperienced or occasional TKA surgeon more like the expert TKA surgeon. However, this is not substantiated by the available literature. Because many studies regarding this subject have been performed in high-volume tertiary referral centers, there is concern whether similarly good results can be obtained by the average orthopaedic surgeon [3]. Despite the fact that radiographic alignment of the implanted prosthesis is superior in computer navigation TKA, outliers greater than 3° are still unavoidable in most of the reported series [1, 7, 8, 12, 17, 22, 23]. The potential reasons leading to these outliers are not discussed in adequate detail in the literature.
The aim of this article is to report the radiographic results of a series of computer navigation TKAs done in a hospital with a lower-volume total knee practice. The primary research objective was to examine whether there was improved accuracy in postoperative radiographic alignment of the implanted prosthesis performed using computer navigation TKA versus conventional instrumentation TKA as judged by (1) overall limb alignment relative to the mechanical axis of the lower limb, (2) femoral component alignment relative to the mechanical axis of the femur, and (3) tibial component alignment relative to the mechanical axis of the tibia. The second research objective was to study the factors that affected the accuracy of computer-navigated TKA in regard to (1) overall limb alignment, (2) femoral component alignment, and (3) tibial component alignment. These include patient factors (age, gender, diagnosis, and coronal plane deformity of the knee measured on preoperative standing long films of the whole lower limb) and surgeon factors (experience of the surgeon in performing navigation-based surgery and intraoperative bone cut error).
Materials and Methods
To assess the improved accuracy in recreation of mechanical alignment in the TKA performed using computer navigation, a retrospective review of the experience of one of the authors (WPY) before and after using computer navigation was performed. Patients were recruited into the analysis based on the following inclusion criteria: (1) the operation was primary TKA; (2) the diagnosis was end-stage arthritis of the knee; and (3) the operating surgeon was WPY. Patients were excluded from analysis if malrotation was found in the standing long films of the whole lower limb. The case series was a consecutive series of the author’s initial experience using the computer navigation technique from January 2004 to October 2006. The control series was a selected series from matching cases of the author’s previous experience using conventional instrumentation (femur intramedullary alignment guide and tibial extramedullary alignment guide) from January 2001 to December 2004. A power analysis was conducted to determine the required sample size. Because the reported percentages of satisfactory lower limb mechanical alignment were 70% to 75% in the majority of conventional technique TKA series [1–3, 5–10, 12, 13, 16–24, 28, 29, 31–34] and 90% to 100% in computer navigation TKA series [1, 17, 22, 23, 28, 29, 34], it was assumed there should be an improvement in satisfactory alignment of at least 15% using the computer navigation technique. The sample size estimation was performed using a power of 80%, a level of significance of 5%, an estimate of a significant reduction of 15% of outliers greater than 3° in mechanical alignment of the lower limb in the computer navigation group when compared with the conventional jig-based group, and an estimate of a standard deviation of 30% in the variation of reported results in the conventional jig-based series. This suggested at least 64 TKAs should be included.
Fifty-four consecutive image-free computer navigation TKAs were performed by the author from January 2004 to October 2006. The author had experience performing 100 conventional technique TKAs (femur intramedullary alignment system and tibia extramedullary alignment system). The average number of TKAs performed each year was approximately 25. The operations were performed using either VectorVision® (BrainLAB AG, Munich, Germany; 15 knees) or Ci™ (BrainLAB; 39 knees) image-free navigation TKA software. Both of these machines were developed by BrainLAB and the software share similar workflow and basic assumptions. The navigation system was used only for navigation of the bone cuts in all cases. Implantation of the prosthesis was not navigated. Standing long radiographs of the whole lower limb were taken 6 weeks after the index operation. The radiographs were repeated if we observed malrotation of the lower limbs on the radiographs. Malrotation was assumed to be present when the femoral condyles were found to be asymmetric or the width of the medial and lateral keels of the tibial tray were not the same. We excluded two knees because of persistent malrotation observed on repeated radiographs of the whole lower limb. One patient had rheumatoid arthritis and one patient had hemophiliac arthropathy. Both had multiple joint involvement stemming from the arthritic situation. Thus, the case series was composed of 52 navigation TKAs. There were eight males and 25 females. Fourteen patients received unilateral TKAs, and 19 patients received one-stage sequential bilateral TKAs. We operated on 49 knees because of primary osteoarthritis of the knee and three knees because of rheumatoid arthritis.
We compared this case series with an historical control series of 52 TKAs performed by the author using a conventional instrumentation technique (femur intramedullary alignment guide and tibia extramedullary alignment guide). The historical control series was chosen by the operating surgeon (WPY) on the basis of age, gender, and body height without any information on results of the radiographic measurement (either preoperative or postoperative). No major differences were found between the two series in terms of age, gender, body height, diagnosis leading to the operation, or preoperative lower limb deformity observed on the standing coronal plane radiographs of the whole lower limb (Table 1).
Table 1.
Demographics of computer navigation TKAs (cases) and conventional jig-based TKAs (controls)
| Factor | Computer navigation TKAs (cases) | Conventional jig-based TKAs (controls) | p Value |
|---|---|---|---|
| Age (years)* | 69 ± 9.2 (48–89) | 66.3 ± 7.6 (49–81) | 0.105 (independent t test) |
| Gender: male/female | 8/25 | 5/28 | Chi square 0.99/0.32 |
| Unilateral TKA | 14 patients (14 knees) | 14 patients (14 knees) | |
| One-stage sequential bilateral TKAs | 19 patients (38 knees) | 19 patients (38 knees) | |
| Diagnosis: osteoarthritis/rheumatoid arthritis | 31/2 | 33/0 | Chi square 3.089/0.079 |
| Body height (cm)* | 150 ± 8 (124–163) | 151 ± 8 (135–172) | 0.441 (independent t test) |
| Preoperative mechanical alignment* | Varus 14° ± 8° (varus 3° to varus 38°) | Varus 13° ± 7° (valgus 1° to varus 34°) | 0.85 (independent t test) |
*Values are expressed as mean ± standard deviation, with range in parentheses.
The prosthesis used in the navigation group was a posterior-stabilized design (18 LPS-Flex, Zimmer, Inc, Warsaw, IN; 34 PFC®, DePuy Orthopaedics, Inc, Warsaw, IN). The prosthesis used in the historical control group was an LCS® rotating-platform knee (Depuy).
All radiographic measurements were done using postoperative standing radiographs of the whole lower limb. Mechanical axis of the lower limb, alignment of the femoral prosthesis with respect to the mechanical axis of the femur in the coronal plane, and alignment of the tibial prosthesis with respect to the mechanical axis of the tibia in the coronal plane were determined. Two independent observers (WPY, ZJL) were involved. One of the observers (WPY) was the operating surgeon and the other was an observer (ZJL) who was blinded to the results. Repeated measurements of the radiographs were done with an interval of at least a 1-week between them. Ideal alignment of mechanical axis of the lower limb was defined as a collinear line joining the center of the hip, the center of the prosthetic knee, and the center of the ankle. Ideal alignment of the femoral and tibial prostheses in the coronal plane were defined as an alignment perpendicular to the mechanical axis of the corresponding bone. A surgical outlier was defined as a deviation greater than 3° from the ideal alignment. The results of the two series were compared. The null hypothesis stated there was no difference in postoperative overall limb alignment measured on the standing radiographs of the whole lower limb between computer navigation TKA and conventional technique TKA. This was examined by an independent t test. Statistical significance was assumed if p < 0.05.
We studied the potential factors that might affect accuracy of the alignment in the navigation group. These included patient factors (age, gender, diagnosis, and coronal plane deformity of the knee measured on preoperative standing long films of the whole lower limb) and surgeon factors (experience of the surgeon in performing navigation-based surgery and intraoperative bone cut error). We documented intraoperative errors in bone cuts by noting the navigation values recorded at the time of verification of the cut accuracy.
We conducted a literature review of the available reports of image-free navigation TKAs. A Medline search of all available English series of image-free computer navigation TKAs from January 2003 to February 2007 was performed. The series was included in the analysis only if the postoperative radiographic measurement was measured with reference to the mechanical axes of the femur and tibia. Satisfactory alignment of the prosthesis was defined as a deviation of 3° or less from the perpendicular to the corresponding mechanical axis. We identified 13 clinical series for comparison with the current navigation series (Table 2). Seven studies were prospective, randomized studies [1, 7, 23, 25, 28, 29, 34] and six were retrospective case-control series [2, 12, 17, 20–22]. We compared the characteristics of the patients and the radiographic results of the current case series with those in the literature. The average age of the patients in our study was comparable with patient ages in most of the reported series. However, the preoperative coronal plane deformity in our navigation series (varus 3° to varus 38°, average varus 14°) was in general much more severe than reported coronal plane deformities.
Table 2.
Summary of clinical studies of computer navigation TKA
| Study | Ethnic origin | Age of patients (years)* | Body height (cm)* | Preoperative deformity* | Postoperative deformity* (satisfactory alignment) | Satisfactory femoral prosthesis alignment | Satisfactory tibial prosthesis alignment |
|---|---|---|---|---|---|---|---|
| Current study | Asia | 69 ± 9.2 (48–89) | 150 ± 8 (124–163) | Varus 14° ± 8° (varus 3° to varus 38°) | Varus 1.3° ± 3.3° (71%) | 94.3% | 86.5% |
| Sparmann et al. [28] | Germany | 67.4 | (100%) | 100% | 82% | ||
| Stockl et al. [29] | Austria | 68.2 | Varus 3° | Varus 0.3° (100%) (± 5°) | |||
| Bathis et al. [1] | Germany | 68.7 | Varus 8.4° | 0° (96%) | 92% | 98% | |
| Victor and Hoste [34] | Belgium | 72 | 164 (150–176) | Varus 0.4° | 0° (100%) | ||
| Matsumoto et al. [22] | Japan | Varus 0.6° (93%) | |||||
| Decking et al. [8] | Germany | 64.7 | Varus 1.5° (52%) (± 2°) | ||||
| Kim et al. [17] | United States | 68 | Varus 0.4° (94%) | ||||
| Bolognesi and Hofmann [2] | United States | 98% | 100% | ||||
| Haaker et al. [12] | Germany | 68 | 167 (150–188) | Varus 6.3° | Varus 0.77° (79%) | ||
| Chin et al. [7] | Singapore | 67.3 | Varus 1.58° (80%) | 93.3% | 93.9% | ||
| Martin and Strempel [21] | Austria | 70.6 | Varus 9° | Varus 2° (81%) | 95.2% | 95.2% | |
| Matziolis et al. [23] | Germany | 71 | Varus 1.4° (97%) | 100% | 100% | ||
| Malik et al. [20] | United Kingdom | 63.9 | Varus 0.68° |
Prosthesis alignment in the coronal plane is considered satisfactory if the absolute error is 3° or less from ideal alignment of the prosthesis in the coronal plane unless specified otherwise: ± 2°, ± 5° = within 2°, 5° from optimal alignment, respectively; *values are expressed as mean ± standard deviation.
Results
There was no improved accuracy in postoperative radiographic alignment of the implanted prosthesis performed using computer navigation TKA versus conventional instrumentation TKA as judged by the overall alignment relative to the mechanical axis of the lower limb (computer navigation series, varus 1.3° ± 3°; historical control series, varus 0.3° ± 3°; p = 0.1, independent t test; beta error = 0.377) (Table 3). Outliers greater than 3° were observed in 29% of the navigation series and 25% of the conventional jig-based series (p = 0.356, chi square test). Extreme outliers greater than 5° were observed in 10% of the navigation series and 12% of the control series (p = 0.538, chi square test) (Table 4).
Table 3.
Comparison between alignment of computer navigation TKA and conventional technique TKA
| Parameter | Computer navigation TKA* | Conventional technique TKA* | Independent t test |
|---|---|---|---|
| Preoperative mechanical alignment of the lower limb in the coronal plane | Varus 14° ± 8° | Varus 13° ± 8° | p = 0.397 Beta error = 0.134 |
| Postoperative mechanical alignment of the lower limb in the coronal plane | Varus 1.3° ± 3° | Varus 0.3° ± 3° | p = 0.1 Beta error = 0.377 |
| Postoperative distal lateral femoral angle | 90.3° ± 1.9° | 90.3° ± 1.7° | p = 0.999 Beta error = 0.05 |
| Postoperative proximal medial tibial angle | 89° ± 2° | 90° ± 2° | p = 0.01 Beta error = 0.743 |
*Values are expressed as mean ± standard deviation.
Table 4.
Amount of outliers in computer navigation TKAs versus conventional TKAs
| Parameter | Computer navigation TKAs (All 52 cases) | Computer navigation TKAs (First 20 cases) | Computer navigation TKAs (subsequent 32 cases) | Conventional TKAs |
|---|---|---|---|---|
| Postoperative mechanical alignment | ||||
| Outlier > 3° | 29% | 45% | 19% | 25% |
| Outlier > 5° | 10% | 20% | 3% | 12% |
| Outlier > 7° | 6% | 15% | 0% | 0% |
| Outlier > 10° | 0% | 0% | 0% | 0% |
| Alignment of femoral components | ||||
| Outlier > 3° | 5.7% | 10% | 3% | 5.7% |
| Outlier > 5° | 2% | 5% | 0% | 0% |
| Outlier > 7° | 0% | 0% | 0% | 0% |
| Outlier > 10° | 0% | 0% | 0% | 0% |
| Alignment of tibial components | ||||
| Outlier > 3° | 13.5% | 25% | 6% | 9.6% |
| Outlier > 5° | 0% | 0% | 0% | 0% |
| Outlier > 7° | 0% | 0% | 0% | 0% |
| Outlier > 10° | 0% | 0% | 0% | 0% |
There was no statistical difference between the two groups in terms of the error of alignment of the femoral prosthesis in the coronal plane (postoperative distal lateral femoral angle in the navigation series: 90.3° ± 1.9°; control series: 90.3° ± 1.7°; p = 0.999, beta error = 0.05) (Table 3). If a surgical outlier was defined as a deviation greater than 3° from the ideal position, 94.3% of the femoral components in the navigation and conventional technique groups were considered to have satisfactory alignment. One extreme outlier greater than 5° was found in the navigation group but there were none in the control group (Table 4).
The tibial tray was implanted in a slightly more varus alignment in the computer navigation group (postoperative proximal medial tibial angle, 89° ± 2°) than in the conventional technique group (90° ± 2°) (p = 0.01, independent t test) (Table 3). Outliers greater than 3° were found in 13.5% of the tibial components in the navigation group and 9.6% in the control group (p = 0.186, chi square test). No extreme outlier was detected in either group (Table 4).
The significant factors that affected postoperative overall mechanical alignment in the navigation series included severity of the preoperative deformity (p = 0.028, independent t test), amount of error in making bone cuts (p = 0.012, Pearson correlation coefficient = 0.258), and experience of the surgeon (p = 0.023, independent t test) (Table 5). There was a higher error in postoperative mechanical alignment of the whole lower limb if the knee had been more extensively deformed before the operation, if the amount of bone cut errors was greater (Fig. 1), and if it was one of the surgeon’s early attempts using computer navigation technology (Fig. 2). Results of the navigation series compared favorably with results of the control series if the surgeon’s initial 20 navigation TKAs were removed from the overall case series. The amount of satisfactory lower limb alignment in the last 32 navigation TKAs was 81% (versus control group: 75%; p = 0.166, chi square test). Only 3% of extreme outliers greater than 5° were found (versus 12% in the control group; p = 0.006, chi square test) (Table 4).
Table 5.
Factors affecting results of computer navigated TKA
| Factor | Overall limb alignment relative to mechanical axis | Alignment of femoral prosthesis | Alignment of tibial prosthesis |
|---|---|---|---|
| Age | NS (p = 0.743) | NS (p = 0.155) | NS (p = 0.237) |
| Gender | NS (Type II error = 0.2) | NS (Type II error = 0.081) | p = 0.04 |
| Male | 0.3° ± 2.5° | 1.3° ± 1° | 1.2° ± 1° |
| Female | 1.6° ± 3.5° | 1.5° ± 1.2° | 2° ± 1.2° |
| Preoperative alignment | p = 0.028 | NS (Type II error = 0.053) | NS (Type II error = 0.342) |
| Varus > 15° | 2.7° ± 3.9° | 1.4° ± 1.5° | 2.2° ± 0.9° |
| Varus < 15° | 0.6° ± 2.8° | 1.5° ± 1° | 1.6° ± 1.3° |
| Diagnosis leading to operation | NS (Type II error = 0.065) | NS (Type II error = 0.087) | NS |
| Osteoarthritis | 1.3° ± 3.4° | 1.4° ± 1.2° | 1.8° ± 1.1° |
| Rheumatoid arthritis | 0.6° ± 1.4° | 1.8° ± 1.4° | 1.8° ± 2.4° |
| Experience of surgeon | p = 0.023 | NS (Type II error = 0.065) | p = 0.029 |
| Author first 20 computer navigation TKAs | 2.6° ± 3.8° | 1.8° ± 1.8° | 2.7° ± 1.3° |
| Author subsequent computer navigation TKAs | 0.4° ± 2.7° | 1.4° ± 1° | 1.6° ± 1.1° |
| Error in making bone cuts (documented by the navigation machine intraoperatively) | p = 0.012 | NS (p = 0.129) | NS (p = 0.308) |
Values are expressed as mean ± standard deviation; NS = not significant.
Fig. 1.
Error in making bone cuts (with reference to the navigation system) was compared with the error of alignment of the prosthesis on a postoperative radiograph (degrees) (+ = varus error; - = valgus error).
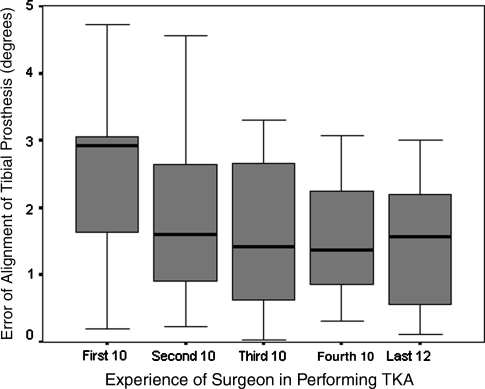
Fig. 2.
The experience of the surgeon in performing computer navigation TKA influenced radiographic alignment of the implanted tibial prostheses. The box represents the interquartile range that contains 50% of the value. The whiskers are lines extending from the box to the highest and the lowest values. The horizontal line in the box represents the mean.
Accuracy of the alignment of the implanted femoral prosthesis in the navigation series was not associated with any of the patient or surgeon factors studied (Table 5). However, if the surgeon’s early experience using the computer navigation technology was removed from the analysis, 97% of the alignments of the implanted femoral prostheses in the navigation series were satisfactory (control group: 94.3%; p = 0.244, chi square test). No extreme outlier was detected (Table 4).
Accuracy of the alignment of the tibial prosthesis was related to the gender of the patients (p = 0.04, independent t test) and experience of the surgeon (p = 0.029, independent t test) (Table 5). Female gender was associated with inferior postoperative radiographic alignment of the implanted prosthesis (Table 5). More error was found in the surgeon’s first 20 navigation TKAs (Fig. 2). If only the results of the last 32 navigation TKAs were studied, two outliers greater than 3° (6%) were found in the implanted tibial component in the computer navigation series (control group: 9.6%; p = 0.222, chi square test) (Table 4).
There was good intraobserver and interobserver agreement in all of the measurements performed (Table 6).
Table 6.
Interobserver and intraobserver error
| Parameter | Observer 1 | Observer 2 | Interobserver error (independent t test) | Intraobserver error (independent t test) | ||
|---|---|---|---|---|---|---|
| First measurement* | Second measurement* | First measurement* | Second measurement* | |||
| Postoperative mechanical axis | 1.3° ± 3.3° | 1.4° ± 3.4° | 1.2° ± 3.4° | 1.3° ± 3.4° | p = 0.796 Beta error = 0.058 | p = 0.944 Beta error = 0.051 |
| Distal lateral femoral angle | 90.2° ± 1.9° | 90.3° ± 1.9° | 90.2° ± 1.9° | 90.3° ± 1.9° | p = 0.924 Beta error = 0.051 | p = 0.787 Beta error = 0.058 |
| Proximal medial tibial angle | 89° ± 1.9° | 88.9° ± 1.9° | 89.2° ± 1.9° | 89.1° ± 1.9° | p = 0.471 Beta error = 0.111 | p = 0.674 Beta error = 0.07 |
*Values are expressed as mean ± standard deviation.
Discussion
Radiographic alignment of the implanted prosthesis in navigated TKA is reported to be superior to that performed using conventional instrumentation in the majority of published reports [1, 2, 4, 6–8, 12, 13, 17, 20–23, 25, 28, 29, 34]. It is believed the use of computer navigation in TKA can make an inexperienced or occasional TKA surgeon more like an expert TKA surgeon. The objective of our study was to examine whether there was improved accuracy in postoperative radiographic alignment of the implanted prosthesis performed using computer navigation TKA versus conventional instrumentation TKA as judged by (1) overall limb alignment, (2) femoral component alignment, and (3) tibial component alignment. The results of our case-control study did not support the assumption of an automatic advantage. The use of computer navigation technology did not improve the accuracy in recreation of mechanical alignment in TKA when compared with the conventional jig-based technique in a hospital with a lower-volume total knee practice. Alignment of implanted femoral (94.3% satisfactory) and tibial prostheses (86.5% satisfactory) in the current navigation surgery group was good but not superior when compared with that of the historical control group (94.3% and 90.4%, respectively). The volume of the operations performed by the surgeon and the experience in using computer navigation technology might be contributing factors.
The retrospective nature of our case-control series potentially introduced bias during selection of the control group, although the author (WPY) was not aware of the results of radiographic measurement at the time of the selection. The amount of satisfactory overall mechanical alignment (75%) in the control series was comparable with reported amounts [1–3, 5–10, 12, 13, 16–24, 28, 29, 31–34]. (Table 7). However, accuracy of implantation of the femoral and tibial components (94.3% and 90.4% satisfactory, respectively) was better than reported accuracy rates (Table 7). Readers should be aware of the potential bias present in this type of retrospective case-control study. The other two major limitations in the methodology of our study included the use of two navigation systems (despite the fact they were designed by the same company, shared the same operating philosophy, and followed similar workflow) and the difference in the design of the prosthesis used (although the computer navigation technique theoretically should work well regardless of the design of the prosthesis because the focus is on accuracy of the bone cuts, not the specific implant design nor instrumentation used).
Table 7.
Radiographic alignment of prostheses using conventional jig-based technique*
| Study | Overall lower limb alignment | Femoral component | Tibial component |
|---|---|---|---|
| Current study | 75% | 94.3% (IM) | 90.4% (EM) |
| Sparmann et al. [28] | 87% | 72% | 90% |
| Bathis et al. [1] | 78% | 86% (IM) | 94% (EM) |
| Chauhan et al. [6] | 71% | 91% (IM) | 91% (EM) |
| Bolognesi and Hofmann [2] | 90% (IM) | 92% (EM) | |
| Chin et al. [7] | 63% | 65% (IM) | 53% (IM) |
| 84% (EM) | |||
| Haaker et al. [12] | 72% | 88% (IM) | 92% (EM) |
| Kim et al. [17] | 73% | ||
| Kim et al. [18] | 82% | 91% (IM) | 93% (EM) |
| Matziolis et al. [23] | 75% | 89% | 82% |
| Patil et al. [24] | 87% (IM) | ||
| Tillett et al. [33] | 86% | 64% (IM) (±2°) | |
| 96% (IM) (±4°) | |||
| 68% (EM) (±2°) | |||
| 88% (EM) (±4°) | |||
| Engh and Petersen [10] | 88% (IM) | 82% (EM) (± 2°) | |
| 69% (EM) | |||
| Matsumoto et al. [22] | 67% | 70% (± 2°) | 77% (± 2°) |
| Cates et al. [5] | 58% (± 2°) | 86% (IM) | 73% (EM) (± 2°) |
| 72% (EM) | |||
| Hart et al. [13] | 70% (± 2°) | ||
| 93% (± 4°) | |||
| Victor and Hoste [34] | 73.5% (± 2°) | ||
| Decking et al. [8] | 36% (± 2°) | 80% (IM) (± 2°) | 80% (EM) (± 2°) |
| 68% (± 4°) | 92% (IM) (± 4°) | 96% (EM) (± 4°) | |
| Ishii et al. [16] | 96% (± 5°) | 90% (IM) (± 4°) | 88% (IM) (± 4°) |
| 88% (EM) (± 4°) | |||
| Maestro et al. [19] | 89% (± 5°) | 96% (IM) (± 4°) | 87% (IM) (± 4°) |
| 84% (EM) (± 4°) | |||
| Stockl et al. [29] | 94% (± 5°) | ||
| Brys et al. [3] | 43% (EM) (± 2°) | 94% (IM) (± 2°) | |
| 85% (EM) (± 2°) | |||
| Dennis et al. [9] | 72% (IM) (± 2°) | ||
| 88% (EM) (± 2°) | |||
| Teter et al. [31] | 91% (IM) (± 4°) | 94% (IM) (± 4°) | |
| 92% (EM) (± 4°) |
*Satisfactory alignment is defined as within 3° from optimal alignment unless specified otherwise: ± 2°, ± 4°, ± 5° = within 2°, 4°, 5° from optimal alignment, respectively; IM = intramedullary alignment system; EM = extramedullary alignment system.
Another potential source of error was that the use of the navigation system was limited to the bone cuts and was stopped before final cementing of the implants. Furthermore, we measured postoperative mechanical alignment of the lower limb and positions of the implanted prostheses using standing radiographs of the whole lower limb. There is concern regarding the accuracy of using plain radiographs in this type of assessment, especially if malrotation is present. Despite the attempt to minimize this error by repeating the radiographs if malrotation of the lower limb was observed, readers should be aware of this limitation.
The average postoperative limb alignment relative to the mechanical axis of the lower limb in our navigation series was varus 1.3°. This is comparable with reported alignment (Table 2). If an outlier was defined as greater than 3° from the ideal position, considerably more outliers were found in our navigation series (71% satisfactory alignment) than in the literature (79%-100% satisfactory alignment) (Table 2). The percentage of extreme outliers greater than 5° was as much as 10% (Table 4).
The coronal plane alignment of 94.3% of the femoral prosthesis and 86.5% of the tibial prosthesis in our navigation series were considered satisfactory. The accuracy of the implanted femoral prosthesis with regard to the mechanical axis of the femur was within reported ranges (92%–100% satisfactory) (Table 2). However, the degree of accuracy of the implanted tibial prosthesis achieved in our navigation series generally was less than those in published series (Table 2).
Significant factors that affected postoperative overall mechanical alignment in our navigation series included severity of the preoperative deformity (p = 0.028), amount of error in bone cuts (p = 0.012), and experience of the surgeon in using the computer navigation system (p = 0.023) (Table 5). The preoperative coronal plane deformity in our navigation series (varus 3° to varus 38°; average varus 14°) generally was much more severe than those reported (Table 2). This might partly account for the observed inferior result in our series. The large preoperative deformity might be multiplanar and have resulted in errors in creation of the image-free coordinate system and therefore accounted for some of the imprecision. In addition, accuracy of overall mechanical alignment increased with the experience of the surgeon in using the navigation system (Fig. 2). If the results of the surgeon’s first 20 navigation TKAs were removed from the overall analysis, the amount of satisfactory overall mechanical alignment improved from 71% to 81% (Table 4). This still was inferior to those in the majority of reports of computer navigation series (Table 2). Although it was better than that of the historical control series (75% satisfactory), this amount of improvement was not significant (p = 0.166, chi square test).
The accuracy of postoperative alignment of the femoral prosthesis in our study was not associated with any of the factors investigated (including patient factors and surgeon factors). Removal of the results of the surgeon’s first 20 navigation TKAs improved the percentage of satisfactory alignment in the navigation series from 94.3% to 97%. However, this did not result in a significant improvement when compared with the conventional jig-based technique (control group: 94.3%; p = 0.244, chi square test).
More errors were observed in postoperative alignment of the tibial prosthesis in female patients (p = 0.04, independent t test) and the surgeon’s first 20 navigated TKAs (p = 0.029, independent t test). The percentage of satisfactory tibial alignment with regard to the mechanical axis of the tibia improved from 86.5% to 94% if the surgeon’s early attempts using the navigation system were removed from the analysis. This was comparable to published results (Table 2). The difference between accuracy of tibial alignment in the navigation series and the historical control series (90.4%) was not significant (p = 0.222, chi square test).
Accuracy in postoperative radiographic alignment of an implanted prosthesis was not improved by using a computer navigation system in a hospital with a lower-volume total knee practice as judged by (1) overall limb alignment relative to mechanical axis of the lower limb (case 71% versus control 75%), (2) femoral component alignment relative to mechanical axis of the femur (case 94.3% versus control 94.3%), and (3) tibial component alignment relative to mechanical axis of the tibia (case 86.5% versus control 90.4%). Significant factors that affected overall postoperative mechanical alignment in the current navigation series included severity of the preoperative deformity (p = 0.028), amount of error in making bone cuts (p = 0.012), and experience of the surgeon in using the computer navigation system (p = 0.023). However, the limitations of our study in terms of its retrospective nature, the use of two navigation systems, the difference in the design of the prostheses used, and the use of plain radiographs for measurement suggest caution in interpreting these results.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bathis H, Perlick L, Tingart M, Luring C, Zurakowski D, Grifka J. Alignment in total knee arthroplasty: a comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86:682–687. [DOI] [PubMed]
- 2.Bolognesi M, Hofmann A. Computer navigation versus standard instrumentation for TKA: a single-surgeon experience. Clin Orthop Relat Res. 2005;440:162–169. [DOI] [PubMed]
- 3.Brys DA, Lombardi AV Jr, Mallory TH, Vaughn BK. A comparison of intramedullary and extramedullary alignment systems for tibial component placement in total knee arthroplasty. Clin Orthop Relat Res. 1991;263:175–179. [PubMed]
- 4.Callaghan JJ, Liu SS, Warth LC. Computer-assisted surgery: a wine before its time: in the affirmative. J Arthroplasty. 2006;21(4 suppl 1):27–28. [DOI] [PubMed]
- 5.Cates HE, Ritter MA, Keating EM, Faris PM. Intramedullary versus extramedullary femoral alignment systems in total knee replacement. Clin Orthop Relat Res. 1993;286:32–39. [PubMed]
- 6.Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique: a randomized, prospective trial. J Bone Joint Surg Br. 2004;86:372–377. [DOI] [PubMed]
- 7.Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618–626. [DOI] [PubMed]
- 8.Decking R, Markmann Y, Fuchs J, Puhl W, Scharf HP. Leg axis after computer-navigated total knee arthroplasty: a prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282–288. [DOI] [PubMed]
- 9.Dennis DA, Channer M, Susman MH, Stringer EA. Intramedullary versus extramedullary tibial alignment systems in total knee arthroplasty. J Arthroplasty. 1993;8:43–47. [DOI] [PubMed]
- 10.Engh GA, Petersen TL. Comparative experience with intramedullary and extramedullary alignment in total knee arthroplasty. J Arthroplasty. 1990;5:1–8. [DOI] [PubMed]
- 11.Fehring TK, Odum S, Griffin WL, Mason JB, Nadaud M. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315–318. [DOI] [PubMed]
- 12.Haaker RG, Stockheim M, Kamp M, Proff G, Breitenfelder J, Ottersbach A. Computer-assisted navigation increases precision of component placement in total knee arthroplasty. Clin Orthop Relat Res. 2005;433:152–159. [DOI] [PubMed]
- 13.Hart R, Janecek M, Chaker A, Bucek P. Total knee arthroplasty implanted with and without kinematic navigation. Int Orthop. 2003;27:366–369. [DOI] [PMC free article] [PubMed]
- 14.Hood RW, Vanni M, Insall JN. The correction of knee alignment in 225 consecutive total condylar knee replacements. Clin Orthop Relat Res. 1981;160:94–105. [PubMed]
- 15.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed]
- 16.Ishii Y, Ohmori G, Bechtold JE, Gustilo RB. Extramedullary versus intramedullary alignment guides in total knee arthroplasty. Clin Orthop Relat Res. 1995;318:167–175. [PubMed]
- 17.Kim SJ, MacDonald M, Hernandez J, Wixson RL. Computer assisted navigation in total knee arthroplasty: improved coronal alignment. J Arthroplasty. 2005;20(7 suppl 3):123–131. [DOI] [PubMed]
- 18.Kim YH, Kim JS, Yoon SH. Alignment and orientation of the components in total knee replacement with and without navigation support: a prospective, randomised study. J Bone Joint Surg Br. 2007;89:471–476. [DOI] [PubMed]
- 19.Maestro A, Harwin SF, Sandoval MG, Vaquero DH, Murcia A. Influence of intramedullary versus extramedullary alignment guides on final total knee arthroplasty component position: a radiographic analysis. J Arthroplasty. 1998;13:552–558. [DOI] [PubMed]
- 20.Malik MH, Wadia F, Porter ML. Preliminary radiological evaluation of the Vector Vision CT-free knee module for implantation of the LCS knee prosthesis. Knee. 2007;14:19–21. [DOI] [PubMed]
- 21.Martin A, von Strempel A. Two-year outcomes of computed tomography-based and computed tomography free navigation total knee arthroplasties. Clin Orthop Relat Res. 2006;449:275–282. [DOI] [PubMed]
- 22.Matsumoto T, Tsumura N, Kurosaka M, Muratsu H, Kuroda R, Ishimoto K, Tsujimoto K, Shiba R, Yoshiya S. Prosthetic alignment and sizing in computer-assisted total knee arthroplasty. Int Orthop. 2004;28:282–285. [DOI] [PMC free article] [PubMed]
- 23.Matziolis G, Krocker D, Weiss U, Tohtz S, Perka C. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty: three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am. 2007;89:236–243. [DOI] [PubMed]
- 24.Patil S, D’Lima DD, Fait JM, Colwell CW Jr. Improving tibial component coronal alignment during total knee arthroplasty with use of a tibial planning device. J Bone Joint Surg Am. 2007;89:381–387. [DOI] [PubMed]
- 25.Perlick L, Bathis H, Perlick C, Luring C, Tingart M, Grifka J. Revision total knee arthroplasty: a comparison of postoperative leg alignment after computer-assisted implantation versus the conventional technique. Knee Surg Sports Traumatol Arthrosc. 2005;13:167–173. [DOI] [PubMed]
- 26.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed]
- 27.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper. Why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. [DOI] [PubMed]
- 28.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A. Positioning of total knee arthroplasty with and without navigation support: a prospective randomised study. J Bone Joint Surg Br. 2003;85:830–835. [PubMed]
- 29.Stockl B, Nogler M, Rosiek R, Fischer M, Krismer M, Kessler O. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res. 2004;426:180–186. [DOI] [PubMed]
- 30.Stulberg BN, Zadzilka JD. Computer-assisted surgery: a wine before its time: in opposition. J Arthroplasty. 2006;21(4 suppl 1):29–32. [DOI] [PubMed]
- 31.Teter KE, Bregman D, Colwell CW Jr. Accuracy of intramedullary versus extramedullary tibial alignment cutting systems in total knee arthroplasty. Clin Orthop Relat Res. 1995;321:106–110. [PubMed]
- 32.Teter KE, Bregman D, Colwell CW Jr. The efficacy of intramedullary femoral alignment in total knee replacement. Clin Orthop Relat Res. 1995;321:117–121. [PubMed]
- 33.Tillett ED, Engh GA, Petersen T. A comparative study of extramedullary and intramedullary alignment systems in total knee arthroplasty. Clin Orthop Relat Res. 1988;230:176–181. [PubMed]
- 34.Victor J, Hoste D. Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res. 2004;428:131–139. [DOI] [PubMed]