Abstract
Three different types of congenital hip disease in adults have been distinguished based upon the position of the femoral head relative to the acetabulum and the underlying pathoanatomy of the joint: (1) dysplasia; (2) low dislocation; and (3) high dislocation. To facilitate classification of borderline or ambiguous cases, we studied the morphologic variations of low and high dislocation as observed on the radiographs of 101 hips with low and 74 hips with high dislocation. In low dislocation, 54 hips (53.5%) had extended coverage of the true acetabulum (Type B1) and 47 hips (46.5%) had limited coverage (Type B2). Among the cases with high dislocation, a false acetabulum with an adjacent femoral head occurred in 46 hips (62.2%) (Type C1), and the femoral head was floating within the gluteal muscles in 28 hips (37.8%) (Type C2). The kappa value for interobserver agreement between two raters who made radiographic measurements was 0.963, and for intraobserver agreement between the two evaluations of the same observer it was 0.946 and 0.971, respectively. The two types of low and high dislocation were associated with high intra- and interobserver agreement. Whether these distinctions have clinical utility requires further validation.
Level of Evidence: Level III, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
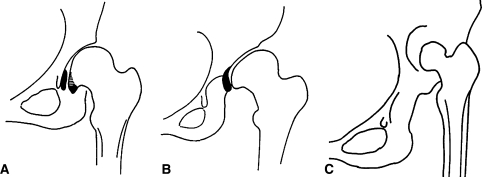
Congenital hip disease (also called developmental dysplasia of the hip or DDH) persisting into adulthood ranges from mild acetabular dysplasia to complete hip dislocation. Several classification systems have been proposed to describe the extent of hip involvement [2, 4, 6–9]. Chung [1] described in infants and children dysplastic hips without subluxation, hips with subluxation, and hips with frank dislocation in 1981. Wedge and Wasylenko [10, 11] in 1978 and 1979 and Weinstein [12] in 1987 also accepted the presence of three types of hip deformity in children, i.e. dysplasia, subluxation, and dislocation. Hartofilakidis et al. [7] adapted such a concept for adults (Table 1) relying on radiographic and morphologic criteria validated during THA to describe acetabular and femoral involvement. That classification included three types of increasing severity: dysplasia (Type A), low dislocation (Type B), and high dislocation (Type C) (Fig. 1). We have observed that cases of types B and C, each have distinct morphological subtypes based on the relationship of the true and false acetabulum in type B and on the presence and absence of a false acetabulum in type C.
Table 1.
Description of the Hartofilakidis et al. classification system [8] for congenital hip disease in adults and morphologic variations of low and high dislocation
| Congenital hip disease type | Description | Subtypes |
|---|---|---|
| Dysplasia | The femoral head is contained within the original acetabulum despite the degree of subluxation or proximal femoral migration | A |
| Low dislocation | The femoral head articulates with a false acetabulum that partially covers the true acetabulum to a varying degree | B1 |
| The false acetabulum covers more than 50% of the true acetabulum; resembles dysplasia | ||
| B2 | ||
| The false acetabulum covers less than 50% of the true acetabulum; resembles high dislocation | ||
| High dislocation | The femoral head is completely out of the true acetabulum and migrated superiorly and posteriorly to a varying degree | C1 |
| The femoral head articulates with a false acetabulum | ||
| C2 | ||
| No false acetabulum; the femoral head is free-floating within the gluteal musculature |
Fig. 1A–C.
The three main types of congenital hip disease in adults are (A) dysplasia, (B) low dislocation, and (C) high dislocation.
To ascertain whether these subtypes may be reliably identified we performed an interobserver and intraobserver variability study of our type B and C cases.
Materials and Methods
We retrospectively reviewed the radiographs of 175 hips—101 hips with low dislocation and 74 hips with high dislocation—in 130 patients obtained from the senior author’s (GH) database. All patients were adults and their mean age at the time the radiographs were taken was 50.8 years (range, 23–77 years).
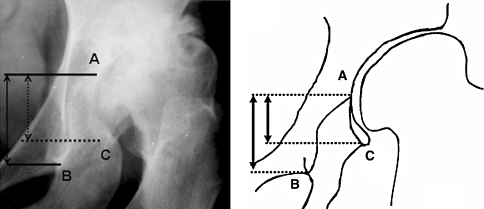
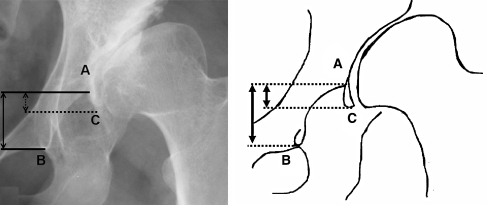
We identified two subtypes of low dislocation: dislocation with (1) extended or (2) limited overlap between the false and the true acetabulum. When the coverage is extended (Type B1) the overlap between the false and the true acetabulum is more than 50%, and when the coverage is limited (Type B2) the overlap is less than 50%. To estimate the amount of overlap, three points must be recognized on the radiograph: (1) the superior limit of the true acetabulum; (2) the inferior point of the teardrop; and (3) the most inferior point of the false acetabulum. The dimension of the true acetabulum in the vertical plane (distance AB) is measured as well as the overlap between the true and the false acetabulum (distance AC). In hips with Type B1 low dislocation, the ratio is greater than 50% (Fig. 2), whereas in hips with Type B2 low dislocation (Fig. 3), the ratio AC/AB × 100 is 50% or less. A hip with Type B1 low dislocation (Fig. 4A–C) may be erroneously classified as dysplasia, whereas a hip with Type B2 low dislocation may be classified as high dislocation (Fig. 4D–F).
Fig. 2.
The radiograph and a line drawing of a hip with Type B1 low dislocation are shown. Three points must be recognized on the radiograph: (A) the superior limit of the true acetabulum; (B) the inferior point of the teardrop; and (C) the most inferior point of the false acetabulum. The overlap (distance AC) between the true and the false acetabulum is more than 50% of the vertical diameter (distance AB) of the true acetabulum.
Fig. 3.
The radiograph and a line drawing of a hip with Type B2 low dislocation are presented. The false acetabulum covers almost completely the true acetabulum. The overlap (distance AC) between the true and the false acetabulum is less than 50% of the vertical diameter (distance AB) of the true acetabulum.
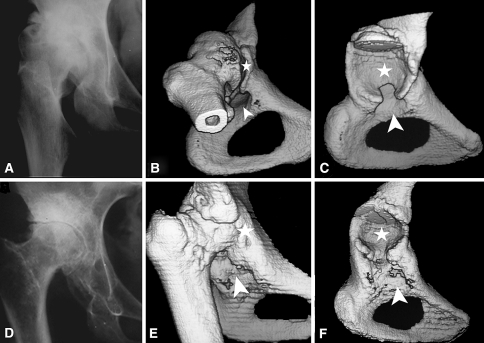
Fig. 4A–F.
The radiographic appearance and the corresponding 3-D computed tomography scan with and without the femoral head in the two subtypes of low dislocation are presented. (A–C) A case with the extended coverage Type B1 low dislocation (coverage more than 50%) is presented. Plain radiography of the hip (A) and 3-D computed tomography scan with (B) and without the femoral head (C) are shown. (D–F) A case with the limited coverage Type B2 low dislocation (coverage less than 50%) is shown. Plain radiographs of the hip (D) and 3-D computed tomography with (E) and without the femoral head (F) are presented. The arrowhead indicates the position of the true acetabulum and the asterisk the position of the false acetabulum.
In high dislocation, two subtypes were identified: (1) in Subtype C1 high dislocation, a false acetabulum is present (Figs. 5A, 6A–C), which may be in contact with the true acetabulum or it may lie at a distant site; and (2) in Type C2 high dislocation, there is no false acetabulum present (Figs. 5B, 6D–F) and the femoral head may be close to the true acetabulum or it may be high-riding within the gluteal musculature. In the latter type, the deformity of the femur is greatest among all types of DDH.
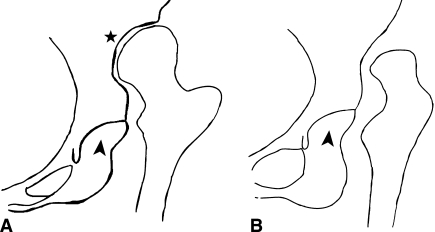
Fig. 5A–B.
The two subtypes of high dislocation are shown. (A) In Type C1 high dislocation, a false acetabulum is present in the iliac wing with which the femoral head articulates. The false acetabulum may be in contact with the true one or it may lie at a distant site. (B) In Type C2 high dislocation, there is no false acetabulum and the femoral head is free-floating within the gluteal muscles. The displacement of the femoral head may be small or significant. The arrowhead shows the position of the true acetabulum and the asterisk the position of the false acetabulum.
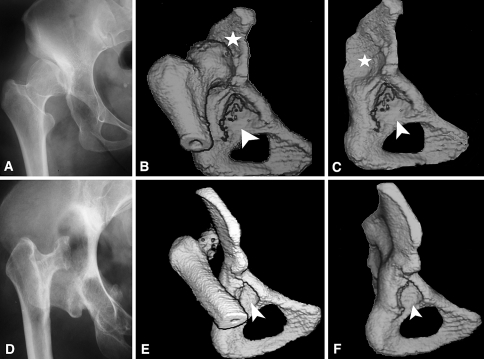
Fig. 6A–F.
The radiographic appearance and three-dimensional computed tomographic scan with and without the femoral head in the two subtypes of high dislocation are presented. (A–C) A case with Type C1 high dislocation; the false acetabulum (denoted by an asterisk) is in contact with the true one (denoted by an arrowhead). (D–F) In Type C2 high dislocation, there is no false acetabulum and the femoral head is free-floating within the gluteal muscles.
The radiographs of 130 patients (175 hips) were examined twice by two experienced hip surgeons (CKY, GCB). The first rating was used to measure interobserver agreement and the second rating, performed 2 months later, to measure intraobserver agreement. Interrater reliability was evaluated using the weighted kappa coefficient.
Assessment of inter- and intraobserver consistency was accomplished using the kappa coefficient as proposed by Fleiss [5]. The kappa value may vary between +1 (complete agreement) and 0 (agreement by chance) to −1 (complete disagreement). Sample size calculation was based on the primary outcome with the aim of showing a reliability that was at least substantial (kappa > 0.7); the power was set to 90% (α = 0.05, β = 0.10). Using this approach, a sample size of three observers and kappa of 20 radiographs per observer was calculated for each group. The analysis was performed using the SPSS version 13.00 statistical package (SPSS Inc, Chicago, IL).
Results
Among the 101 hips with low dislocation, 54 (53.5%) were Type B1 and 47 (46.5%) were Type B2. Among the 74 hips with high dislocation, there were 47 (63.5%) with Type C1 dislocation and 27 (36.5%) with Type C2 dislocation.
The interobserver agreement between the two raters who made radiographic measurements was 0.963. The intraobserver reliability between the two evaluations of the same observer was 0.946 and 0.971.
Discussion
Classification in DDH plays a critical role in preoperative planning, selection of operative technique and implants, and assessment of results. Hartofilakidis et al. [6–8] classification described three types of DDH, namely dysplasia and low and high dislocation. Our clinical experience suggested types B and C could be divided in two subtypes each due to distinct morphological variations found at surgery. However, this refinement of our classification could lead in disagreements between different observers. In this study we examined the interobserver and intraobserver agreement for these proposed subtypes.
Our radiographic measurements were performed by only two observers (CKY, GCB). These two observers were experienced hip surgeons blinded to the surgical findings. Less experienced observers might obtain different levels of reliability. The clinical importance of these subtypes is unknown. For example, whether B1 compared to B2 provides a better containment for the placement of a cup in the true acetabulum is unclear. Additionally, whether the natural histories of long-term outcomes of reconstructions differ between these subtypes is unknown.
One published study [3] reports sufficient intra- and interobserver reliability of the Hartofilakidis et al. [8] classification, with reported kappa values 0.79 and 0.75 respectively. In the present study, the description of the spectrum of morphologic forms of low and high dislocation was stated not to complicate the classification, but to increase its reliability providing further insight into the pathoanatomy of the acetabulum. However, in questionable cases, the underlying anatomy of the hip can be evaluated with 3-D computed tomography. With exclusion of the femoral head from the final image, the pathoanatomy of the acetabulum can be readily appraised to facilitate preoperative planning.
The deformity of the acetabulum and the femur in DDH is complex and may include malformation in all three planes. The amount of cephalic migration of the femoral head is used in the Crowe et al. classification [2], but it is not a definite criterion for judging the severity of hip malformation because the pathoanatomy of the acetabulum is variable and, as such, it is the primary factor that determines the severity of the deformity. The classification of Hartofilakidis et al. [8] is based on the morphology of the deformed acetabulum as observed on anteroposterior pelvis radiographs. It has been confirmed by comparing radiographic observations with intraoperative findings [6–8]. The implications of the current refinement are: (1) to increase the reliability of the original classification; (2) to identify differences in treatment choices and complications associated with the subtypes; and (3) to help control for confounding preoperative variables in assessing results.
Classification systems guide treatment, assist physicians in choosing the most appropriate nonsurgical or surgical solution to a given problem, and serve as a controlling variable in comparing outcomes; in some cases they may predict outcomes. Classification of any disease is usually performed using an order of increasing severity based on clinical, anatomic, radiographic, or survival criteria as well as on the level of function and the quality of life of the patients. A classification system that aspires to universal adoption, in addition to being reliable and valid, should be as simple as possible and easy to use in clinical practice. It should also include all types of deformity, and be accurate and easy to memorize.
Careful attention to the morphology of the acetabulum in hip radiographs in patients with DDH is necessary primarily to accurately classify the deformity and predict the acetabulum bone deficiencies encountered during THA and to select the proper reconstruction method and implants.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Chung SMK. Hip Disorders in Infants and Children. Philadelphia, PA: Lea & Febiger;1981.
- 2.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed]
- 3.Decking R, Brunner A, Decking J, Puhl W, Gunther KP. Reliability of the Crowe und Hartofilakidis classifications used in the assessment of the adult dysplastic hip. Skeletal Radiol. 2006;35:282–287. [DOI] [PubMed]
- 4.Eftekhar NS. Principles of Total Hip Arthroplasty. St Louis, MO: CV Mosby; 1978.
- 5.Fleiss JL. Statistical Methods for Rates and Proportions. 2nd ed. New York, NY: John Wiley & Sons; 1981:218.
- 6.Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital hip disease. J Bone Joint Surg Am. 2004;86:242–250. [DOI] [PubMed]
- 7.Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg Br. 1988;70:182–186. [DOI] [PubMed]
- 8.Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1996;78:683–692. [DOI] [PubMed]
- 9.Kerboul M, Mathieu M, Sauzieres P. Total hip replacement for congenital dislocation of the hip. In: Postel M, Kerboul M, Evrard J, Courpied JP, eds. Total Hip Replacement. New York, NY: Springer; 1987:51–66.
- 10.Wedge JH, Wasylenko MJ. The natural history of congenital disease of the hip. J Bone Joint Surg Br. 1979;61:334–338. [DOI] [PubMed]
- 11.Wedge JH, Wasylenko MJ. The natural history of congenital dislocation of the hip: a critical review. Clin Orthop. 1978;137:154–162. [PubMed]
- 12.Weinstein SL. Natural history of congenital hip dislocation (CDH) and hip dysplasia. Clin Orthop. 1987;225:62–76. [PubMed]