Abstract
Implant failure is a serious complication in reverse shoulder arthroplasty. We determined the incidence of glenosphere disengagement in a cohort of 479 reverse shoulder prostheses (468 Delta III™ [DePuy International Ltd, Leeds, UK], 11 Aequalis™ [Tornier, Grenoble, France]). We also determined whether disengagement adversely affected clinical outcomes. The minimum followup was 12 months (mean, 28.6 months; range, 12–72 months). Disengagement of the glenosphere occurred in 16 of 479 shoulders (3.2%). In 13 patients, the disengagement was partial (clear step-off between the baseplate and the glenosphere) and was not associated with a poor functional outcome with this short-term followup. In three patients, the disengagement led to a fracture of the central screw, leading to a complete disengagement of the glenosphere from the baseplate, necessitating revision in two; the third refused revision. Partial disengagement was seen in five of 11 Aequalis™ prostheses (45.4%) and eight of 468 Delta III™ prostheses (1.7%). The three total disengagements with central screw breakage all occurred in Delta III™ prostheses. We believe differences in the type of locking screws may explain the differences observed between the two types of reverse prostheses.
Level of Evidence: Level III, retrospective study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
A reverse shoulder prosthesis is well accepted as treatment for glenohumeral arthritis associated with an irreparable tear of the rotator cuff. The specific design of the reverse prosthesis obviates the need for an intact rotator cuff by medializing the center of rotation of the glenohumeral joint and distalizing the insertion of the deltoid muscle, thereby increasing its lever arm [3, 8]. Since its introduction, many reports describe favorable functional results in patients with cuff tear arthropathy [1, 3, 5, 14, 15, 17–19, 21, 27, 28–31, 33], osteonecrosis of the humeral head, rheumatoid arthritis and irreparable cuff tears [17, 25, 35], tumors of the proximal humerus [10, 12], revision shoulder arthroplasty [4, 8, 9, 11, 17], and proximal humeral fractures [4, 6, 17]. Restoration of function and adequate pain relief seem consistent in all reports.
Constrained shoulder prostheses also have been advocated for treatment of cuff tear arthropathy. These prostheses, however, are associated with a high rate of complications and revisions [1, 20, 23, 24, 34]. In his original study, Post and Jablon [24] reported 21 complications (87.5%) and 13 revisions (54.1%) in 24 prostheses after a mean followup of 103 months. After redesigning the prosthesis, they noted six complications (7.6%) and three revisions (3.8%) in 78 prostheses after a mean followup of 46.5 months. An extended followup of 50 shoulders from the original series showed the modifications of the prosthesis resulted in a decrease of prosthetic failures but in an increase of prosthetic dissociation and aseptic loosening [23].
Medialization of the center of rotation as proposed by Grammont et al. [15, 16] seemingly reduces the risk of loosening of the glenoid component. Loosening of the baseplate from the glenoid remains a concern, but unscrewing of the glenoid components (baseplate-glenosphere) also has been described [3, 8, 13, 29]. Unscrewing of the glenoid components led to modification of the prosthetic design in 1995 using a Morse taper between the glenosphere and the baseplate. Despite these design modifications, two of us (LDW, PD) recently observed complete disengagement of the glenosphere from the baseplate (Fig. 1), a serious complication that also was observed in a French multicenter study and necessitated revision in 75% of the cases [22].
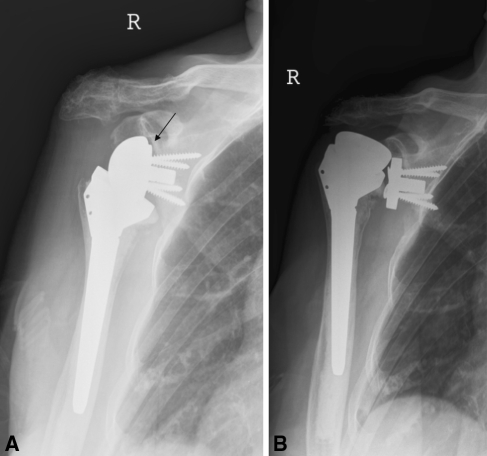
Fig. 1A–B.
(A) An asymptomatic partial disengagement (arrow) of the glenosphere is shown. The Constant-Murley score at this time was 61. A few months later, this patient (Patient 1) experienced severe pain and loss of function and the Constant-Murley score decreased to 10. (B) A radiograph shows a complete disengagement of the glenosphere with fracture of the central locking screw, necessitating revision of the prosthesis.
We therefore determined the incidence of this unusual complication in reverse shoulder arthroplasties and whether disengagement resulted in adverse clinical effects as compared with patients without radiographic evidence of disengagement. We also sought a possible explanation for the differences observed in the two types of reverse prostheses used in the study.
Materials and Methods
We retrospectively reviewed the clinical and radiographic data of 419 patients with 449 reverse shoulder arthroplasties from the French multicenter study (Omarthrose excentrée, Société Française de Chirurgie Orthopédique et Traumatologique, Paris, France, 2006) and 32 from the University Hospital Pellenberg (Pellenberg, Belgium). The French multicenter database includes 627 shoulder prostheses implanted for osteoarthrosis associated with a rotator cuff deficiency in 596 patients. The implants used in this series were 48 hemiarthroplasties (43 patients), 52 bipolar prostheses (47 patients), and 527 reverse shoulder arthroplasties (502 patients). Of these 527 reverse prostheses, 449 were implanted after 1995 in 419 patients (33 bilateral prostheses; 329 females, 120 males). We reviewed only these 419 patients with 449 reverse shoulder prostheses supplemented with all the reverse shoulder prostheses (n = 32; five males, 27 females) implanted at our institution (University Hospital Pellenberg) between 1995 and 2006. Two female patients died from cancer and were excluded from the study. Thus, we were able to analyze the clinical and radiographic data from 446 patients (33 bilateral prostheses; 354 females, 125 males) with 479 reverse shoulder prostheses. The minimum followup was 12 months (mean, 28.6 months; range, 12–72 months). The type of implant used was a Delta III™ reverse prosthesis (DePuy International Ltd, Leeds, UK) in 468 cases and an Aequalis™ prosthesis (Tornier, Grenoble, France) in 11 cases.
To determine whether disengagement was present, we reviewed all the available postoperative radiographic data from the patients until the time of last followup. Radiographic assessment included an anteroposterior (AP) view tangential to the baseplate and an axillary lateral view. We defined disengagement as a visible step between the baseplate and the prosthetic glenosphere on an axillary and/or AP view tangential to the baseplate (Fig. 2). The Constant-Murley score [7] obtained at the last followup was used to assess the clinical outcome.
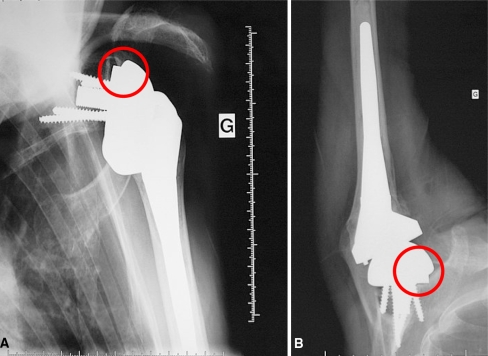
Fig. 2A–B.
(A) An AP view or (B) an axillary view can clearly show disengagement of the glenosphere from the baseplate (circle).
Results
The incidence of disengagement was 3.2% (16 patients with 16 shoulders among 479 shoulders; Table 1). In 13 patients, the disengagement was partial, ie, the central screw was not broken and the glenosphere remained seated on the baseplate but with a clear step. In three cases, the central screw was broken, leading to total disengagement of the glenosphere from the baseplate. A partial disengagement was present in eight of 468 Delta III™ prostheses (1.7%) and five of 11 Aequalis™ prostheses (45.4%). The three total disengagements occurred in Delta III™ prostheses.
Table 1.
Type of prosthesis, degree of disengagement, and length of followup for all patients diagnosed with a disengagement of the glenosphere
| Patient | Type of prosthesis* | Disengagement | Revision? | Followup (months) | Constant-Murley score [7] |
|---|---|---|---|---|---|
| 1 | Delta III | > 1 mm with fracture of central screw | Yes | 14 | 61 |
| 2 | Delta III | > 1 mm with fracture of central screw | Yes | 48 | 26 |
| 3 | Delta III | > 1 mm with fracture of central screw | No† | 12 | 52 |
| 4 | Delta III | > 1 mm with progressive disengagement | No | 72 | 59 |
| 5 | Delta III | > 1 mm with spontaneous reassembly | No | 24 | 57 |
| 6 | Aequalis | < 1 mm with spontaneous reassembly | No | 36 | 81 |
| 7 | Aequalis | > 1 mm with spontaneous reassembly | No | 36 | 70 |
| 8 | Aequalis | No disengagement immediately postoperatively but > 1 mm after 2 years | No | 24 | 63 |
| 9 | Aequalis | No disengagement immediately postoperatively but < 1 mm after 2 years | No | 24 | 45 |
| 10 | Delta III | < 1 mm | No | 24 | 64 |
| 11 | Delta III | < 1 mm | No | 12 | 75 |
| 12 | Delta III | < 1 mm | No | 24 | 57 |
| 13 | Delta III | < 1 mm | No | 36 | 73 |
| 14 | Delta III | < 1 mm | No | 24 | 53 |
| 15 | Aequalis | < 1 mm | No | 12 | 66 |
| 16 | Delta III | < 1 mm | No | 36 | 45 |
*Types of prostheses included Delta III™ (DePuy International Ltd, Leeds, UK) and Aequalis™ (Tornier, Grenoble, France); †Patients 1 to 3 had complete disengagement, but only Patients 1 and 2 had revision surgery; Patient 3 refused revision owing to financial reasons.
We observed no difference in clinical outcome at last followup between patients with partial disengagement and those without disengagement (Constant-Murley score of 59 in both groups). However, central screw breakage, leading to complete disengagement of the glenosphere, always led to a dramatic decrease of the Constant-Murley score, with a severe increase in pain and functional disability. There was no difference in Constant-Murley score for partial disengagement for the two types of prostheses and there was no relationship between the score and the amount of partial disengagement. In Patients 8 and 9, both with an Aequalis™ prosthesis in whom no initial disengagement was seen, disengagement could be seen after 2 years’ followup. Reassembly of a glenosphere that was disengaged on previous radiographs was noted in three patients (Patients 5–7; two Aequalis™ prostheses, one Delta III™ prosthesis) after a mean of 16 months. Thus far, only two patients in this had reoperations. Patient 1 had complete disengagement of her glenosphere, with sudden worsening of the Constant-Murley score (Fig. 1). Patient 2 underwent revision because of severe pain and disengagement of her glenosphere. At the time of revision, breakage of the central screw with asymmetric erosion of the baseplate was observed (Fig. 3). Patient 3 had progressive disengagement of his glenosphere but refused revision because of financial reasons.
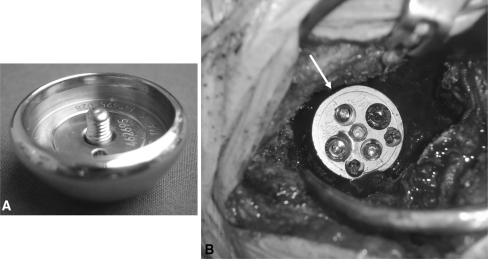
Fig. 3A–B.
Disengagement of the glenosphere from the baseplate results in abnormal motion of the glenosphere. This ultimately can result in (A) central screw breakage and (B) asymmetric wear of the baseplate (arrow).
Discussion
The reverse shoulder prosthesis has emerged as an excellent solution for patients with arthritis of the glenohumeral joint associated with deficiency of the rotator cuff. The initial good results of the reverse shoulder prosthesis for treatment of rotator cuff arthropathy have resulted in a dramatic increase in the use of this type of implant. Despite a good clinical outcome in most series, the complications associated with this procedure remain frequent [2, 32]. Bohsali et al. [2] reported a mean complication rate of 24.4% (range, 6.25%–50%). Unscrewing of the glenosphere to baseplate primarily occurred in prostheses used before 1995 [3, 8, 13, 29] and resulted in a change in the prosthetic design in 1995 to a Morse taper design with central screw fixation. It was believed this change of design completely resolved the problem of glenoid dissociation. Molé et al. [22], however, reported on one patient with an implant from 2001 who had disassembly of the glenosphere as a result of improper impaction of the Morse cone. Being confronted with three cases of complete disengagement of a glenosphere, we therefore determined the incidence of this complication.
The mean followup in our study is relatively short (28.6 months), clearly a limitation of our study. A longer followup most likely would show whether greater numbers of prostheses develop disengagement and whether asymptomatic disengagements can become symptomatic with time. Longer followup also would allow a better study of the natural history of the disengagement problem in terms of risk of central screw breakage. Moreover, our reported incidence of glenosphere disengagement may be too low because we could not always obtain a true AP view of the shoulder as a result of technical errors. Accurate measurement of the degree of disengagement necessitates radiographic views that are tangential to the baseplate. Variability in the quality of radiographs in this retrospective review may have resulted in underestimation of the incidence as small disengagements potentially may be missed in cases where the beam is not perfectly tangential.
We found 16 cases of disengagement (3.2%): in 13 cases, the disengagement was partial and there was still good contact between the sphere and the baseplate; in three cases, the disengagement had led to breakage of the central screw, leading to a total disengagement of the glenosphere from the baseplate. The presence of partial disengagement of the glenosphere was not associated with a difference in clinical outcome. Nevertheless, because metallic destruction can result from disengagement, the need for early revision is debatable. Roberts et al. [26] recently stated careful radiographic examination is required to reveal early complications with reverse shoulder prostheses. Our study confirms this statement because our examination of the postoperative radiographs of patients who underwent reverse shoulder arthroplasty revealed an incidence of glenosphere disengagement of 3.2%.
Improper seating of the glenosphere and potential instability between the baseplate can occur because of inadequate reaming of bone around the edge of the baseplate or interposition of bone or soft tissue between the glenosphere and the baseplate at the time of impaction. In the case of interpositioning of material in the Morse taper, the central screw will be tightened without locking the Morse taper. This will result in eventual motion between the glenosphere and the baseplate resulting from necrosis of the interposed tissue. The locking screws of the Aequalis™ and the Delta III™ prosthesis are different (Fig. 4): the locking screw of the Delta III™ prosthesis has less than 1-mm slack whereas the Aequalis™ prosthesis has 2-mm slack. Inadequate reaming or soft tissue interpositioning between the glenosphere and the baseplate also will induce disengagement in the Aequalis™ prosthesis, but because this system allows more slack, abnormal motion between the baseplate and the glenosphere will not occur. Because the locking screw of the Delta III™ prosthesis has less than 1-mm slack, spontaneous reassembly is possible only after breakage of the central screw. This screw failure is induced by a seesaw movement of the glenosphere onto the baseplate. In contrast, the Aequalis™ prosthesis central screw does not exhibit this seesaw movement because the slack is greater than 2 mm, explaining why spontaneous reassembly can occur. The two cases of spontaneous disassembly of the glenosphere (both Aequalis™ prostheses) can be explained by the fact that the glenosphere, although initially flush with the baseplate, was not completely locked by the conus.
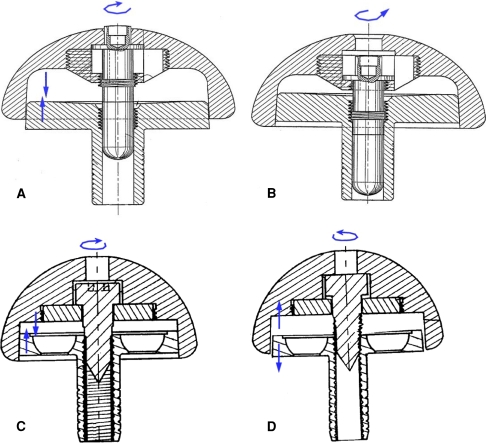
Fig. 4A–D.
The differences in the baseplate-glenosphere assembly between (A, B) the Aequalis™ prosthesis and (C, D) the Delta III™ prosthesis are shown. (A, B) The Aequalis™ locking screw is of the central locking type. When inserted, it falls into the thread of the baseplate. Tightening the locking screw brings the baseplate taper closer to the glenosphere taper. Once the screw is fully inserted, the entire thread of the screw is inside the baseplate. There is no more link between the locking screw and the glenosphere. As a consequence, the surgeon will not be able to unscrew the locking screw out of the glenosphere. Inadequate reaming of the glenoid or soft tissue interpositioning between the glenosphere and the baseplate will induce disengagement, but because the Aequalis™ prosthesis allows more slack, abnormal motion between the baseplate and glenosphere will not occur. (C, D) In the Delta III™ prosthesis, the thread of the locking screw is always in contact with the thread of the glenosphere. This makes removal of the glenosphere easier in revision cases, but when there is incomplete reaming or soft tissue interpositioning, the screw will not be seated entirely in the thread of the baseplate. This can result in abnormal motion between the baseplate and the glenosphere and may lead to central screw breakage.
To overcome this potentially serious type of impaction default, we advise the following: (1) excellent surgical exposure of the baseplate to prevent soft tissue interpositioning when mounting the glenosphere onto the baseplate; (2) thorough bony reaming around the glenoid with removal of all bony remnants to permit proper impaction of the glenosphere onto the baseplate; and (3) familiarity with the type of locking screws. Locking screws with limited slack, like those of the Delta III™ prosthesis, need more frequent screwing followed by tapering to ensure complete conical locking. When confronted with a patient with a disengaged glenosphere, we suggest (1) regular clinical and radiographic followups at 3- to 6-month intervals and (2) a CT scan, which may be helpful to determine whether there is screw breakage. In elderly patients with an asymptomatic disengagement that remains stable with time, we do not suggest performing revision. In younger patients and in patients with progressive disengagement, we advise revising the reverse prosthesis.
Footnotes
One or more of the authors (PD) have received funding from the Fund for Scientific Research, Flanders, Belgium.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-008-0578-8
References
- 1.Baulot E, Chabernaud D, Grammont PM. [Results of Grammont’s inverted prosthesis in omarthritis associated with major cuff destruction: apropos of 16 cases] [in French]. Acta Orthop Belg. 1995;61(suppl 1):112–119. [PubMed]
- 2.Bohsali KI, Wirth MA, Rockwood CA Jr. Complications of total shoulder arthroplasty. J Bone Joint Surg Am. 2006;88:2279–2292. [DOI] [PubMed]
- 3.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14(suppl S):147S–161S. [DOI] [PubMed]
- 4.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–540. [DOI] [PubMed]
- 5.Boulahia A, Edwards TB, Walch G, Baratta RV. Early results of a reverse design prosthesis in the treatment of arthritis of the shoulder in elderly patients with a large rotator cuff tear. Orthopedics. 2002;25:129–133. [DOI] [PubMed]
- 6.Cazeneuve JF, Cristofari DJ. [Grammont reversed prosthesis for acute complex fracture of the proximal humerus in an elderly population with 5 to 12 years follow-up] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2006;92:543–548. [DOI] [PubMed]
- 7.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed]
- 8.Delloye C, Joris D, Colette A, Eudier A, Dubuc JE. [Mechanical complications of total shoulder inverted prosthesis] [in French]. Rev Chir Orthop Reparatrice Appar Mot. 2002;88:410–414. [PubMed]
- 9.De Wilde L, Mombert M, Van Petegem P, Verdonk R. Revision of shoulder replacement with a reversed shoulder prosthesis (Delta III): report of five cases. Acta Orthop Belg. 2001;67:348–353. [PubMed]
- 10.De Wilde L, Plasschaert F. Prosthetic treatment and functional recovery of the shoulder after tumor resection 10 years ago: a case report. J Shoulder Elbow Surg. 2005;14:645–649. [DOI] [PubMed]
- 11.De Wilde L, Walch G. Humeral prosthetic failure of reversed total shoulder arthroplasty: a report of three cases. J Shoulder Elbow Surg. 2006;15:260–264. [DOI] [PubMed]
- 12.De Wilde LF, Plasschaert FS, Audenaert EA, Verdonk RC. Functional recovery after a reverse prosthesis for reconstruction of the proximal humerus in tumor surgery. Clin Orthop Relat Res. 2005;430:156–162. [DOI] [PubMed]
- 13.Favard L, Lautmann S, Sirveaux F, Oudet D, Kerjean Y, Huguet D. Hemiarthroplasty versus reverse arthroplasty in the treatment of osteoarthritis with massive rotator cuff tear. In: Walch G, Boileau P, Molé D, eds. 2000 prothèses d’épaule: recul de 2 à 10 ans. Paris, France: Sauramps Médical; 2001:261–268.
- 14.Frankle M, Siegal S, Pupello D, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff deficiency: a minimum two-year follow-up study of sixty patients. J Bone Joint Surg Am. 2005;87:1697–1705. [DOI] [PubMed]
- 15.Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–68. [DOI] [PubMed]
- 16.Grammont PM, Trouilloud P, Laffay JP, Deries X. Etude et réalisation d’une nouvelle prothèse d’épaule. Rhumatol. 1987;10:407–418.
- 17.Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty: survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88:1742–1747. [DOI] [PubMed]
- 18.Hatzidakis AM, Norris TR, Boileau P. Reverse shoulder arthroplasty: indications, technique and results. Tech Shoulder Elbow Surg. 2005;6:135–149. [DOI]
- 19.Jacobs R, Debeer P, Stoffelen D, De Smet L. Treatment of rotator cuff arthropathy with a reversed Delta shoulder prosthesis. Acta Orthop Belg. 2001;67:344–347. [PubMed]
- 20.Lettin AW, Copeland SA, Scales JT. The Stanmore total shoulder replacement. J Bone Joint Surg Br. 1982;64:47–51. [DOI] [PubMed]
- 21.Matsen FA 3rd, Boileau P, Walch G, Gerber C, Bicknell RT. The reverse total shoulder arthroplasty. J Bone Joint Surg Am. 2007;89:660–667. [DOI] [PubMed]
- 22.Molé D, Navez P, Garaud P. Reverse shoulder prosthesis: problems related to the glenoid. In: Walch G, Boileau P, Molé D, Favard L, Lévigne C, Sirveau F, eds. Reverse Shoulder Arthroplasty: Clinical Results, Complications, Revision. Montpellier, France: Sauramps Médical; 2006:289–301.
- 23.Post M. Constrained arthroplasty of the shoulder. Orthop Clin North Am. 1987;18:455–462. [PubMed]
- 24.Post M, Jablon M. Constrained total shoulder arthroplasty. Clin Orthop Relat Res. 1983;173:109–116. [PubMed]
- 25.Rittmeister M, Kerschbaumer F. Grammont reverse total shoulder arthroplasty in patients with rheumatoid arthritis and nonreconstructible rotator cuff lesions. J Shoulder Elbow Surg. 2001;1:17–22. [DOI] [PubMed]
- 26.Roberts CC, Ekelund AL, Renfree KJ, Liu PT, Chew FS. Radiologic assessment of reverse shoulder arthroplasty. Radiographics. 2007;27:223–235. [DOI] [PubMed]
- 27.Seebauer L, Walter W, Keyl W. Reverse total shoulder arthroplasty for the treatment of defect arthropathy. Oper Orthop Traumatol. 2005;17:1–24. [DOI] [PubMed]
- 28.Sirveaux F, Favard L, Oudet D, Huquet D, Lautman S. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive and non repairable cuff rupture. In: Walch G, Boileau P, Molé D, eds. 2000 prothèses d’épaule: recul de 2 à 10 ans. Paris, France: Sauramps Médical; 2001:247–252.
- 29.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff: results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86:388–395. [DOI] [PubMed]
- 30.Valenti PH, Boutens D, Nérot C. Delta 3 reversed prosthesis for osteoarthritis with massive rotator cuff tear: longterm results. In: Walch G, Boileau P, Molé D, eds. 2000 prothèses d’épaule: recul de 2 à 10 ans. Paris, France: Sauramps Médical; 2001:247–252.
- 31.Vanhove B, Beugnies A. Grammont’s reverse shoulder prosthesis for rotator cuff arthropathy: a retrospective study of 32 cases. Acta Orthop Belg. 2004;70:219–225. [PubMed]
- 32.Walch G, Wall B, Mottier F. Complications and revision of the reverse prosthesis, a multicenter study of 457 cases. In: Walch G, Boileau P, Molé D, Favard L, Lévigne C, Sirveau F, eds. Reverse Shoulder Arthroplasty: Clinical Results, Complications, Revision. Montpellier, France: Sauramps Médical; 2006:289–301.
- 33.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87:1476–1486. [DOI] [PubMed]
- 34.Wirth MA, Rockwood CA Jr. Complications of total shoulder-replacement arthroplasty. J Bone Joint Surg Am. 1996;78:603–616. [DOI] [PubMed]
- 35.Woodruff MJ, Cohen AP, Bradley JG. Arthroplasty of the shoulder in rheumatoid arthritis with rotator cuff dysfunction. Int Orthop. 2003;27:7–10. [DOI] [PMC free article] [PubMed]