Abstract
The surgical treatment of patients with neglected developmental dysplasia of the hip (DDH) has been the subject of controversy. We asked if age affected outcome in patients with neglected DDH with unilateral or bilateral dislocation who underwent one-stage combined procedures. We retrospectively reviewed the results of 40 patients (51 hips) treated with a one-stage combined procedure consisting of open reduction, pelvic osteotomy, and femoral shortening. The average age at the time of surgery was 5.4 years for Group I (bilateral dislocation, 22 hips) and 6.7 years for Group II (unilateral dislocation, 29 hips). Mean followup was 5.4 years for Group I and 6.7 years for Group II. According to the modified score system of Trevor et al, 13 hips rated excellent, three were good, and six were fair in Group I; the ratings were 14, nine, and six hips respectively in Group II. Four patients had a limb-length discrepancy of approximately 1.5 cm in Group I. Twelve hips in Group I and 18 hips in Group II had osteonecrosis of varying severity. Our data suggest the outcomes of the children who were 5.5 years or younger in Group I and 8 years or younger in Group II were better.
Level of Evidence: Level IV, case series. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Developmental dysplasia of the hip (DDH) remains a perplexing and unsolved problem in older children [14] and older children with DDH are more difficult to treat [10, 11]. Treatment modalities include various nonoperative or operative approaches (open reduction, and pelvic or femoral osteotomies) [6, 12, 18]. We believe a one-stage surgical approach in late-diagnosed DDH seems the most reasonable treatment based on our review of the literature [6, 8, 12, 19]. However, there is considerable variability in the anatomy of older children with DDH and lesser ability of their bones to remodel. In particular, there are substantial variations in the degree of acetabular anteversion and dysplasia patients with unilateral disease and patients with bilateral DDH may have differing anatomy on the two sides [3]. In addition, secondary changes in the soft tissue and bone may lead to a more complex or protracted course of treatment. For these reasons, age and laterality may influence outcomes and be important in deciding a treatment approach [3, 8].
We asked whether age associated with unilateral or bilateral dislocation influences a combined clinical and radiographic score (modified from Trevor et al. [23]) in patients with neglected DDH who underwent one-stage combined procedures, and whether age influenced acetabular development (acetabular index) and risk of osteonecrosis.
Materials and Methods
We retrospectively reviewed the medical records of 55 patients with previously untreated DDH (minimum age of 3) who underwent a one-stage combined open reduction, pelvic osteotomy, and femoral shortening between 1996 and 2002. We excluded 15 patients who had an associated muscular or chromosomal disorder (n = 4) or who did not have followup (n = 11). This left 40 patients (51 hips): 33 girls and seven boys. Thirteen patients had dislocation of the left hip, 16 had dislocation of the right, and 11 had bilateral dislocation. The hips were grouped at their latest review according to bilateral (Group I, 11 patients with 22 hips) or unilateral (Group II, 29 patients) dislocations. In Group I, the average age at the time of surgery was 5.4 years (range, 3–9.5 years). Six patients (12 hips) were younger than 5.5 years, four patients (8 hips) were older than 5.5 years at the time of operation; one patient had surgery on one hip before age 5.5 years, and at 5.5 years for the other hip. In Group II, the average age at the time of surgery was 6.7 years old (range, 3.1–10 years). Twenty-two of 29 patients were younger than 8 years old (Fig. 1A–B), and seven were older than 8 years old (Fig. 2A–B) (Table 1). No patients underwent preoperative traction. We evaluated the initial radiographs using the method of Tönnis [22]. In Group I there were three Tönnis Type III and 19 Tönnis Type IV hips; in Group II there were four Tönnis Type III and 25 Tönnis Type IV hips. The minimum followup was 4 years (mean, 5.4 years; range, 4–8.5 years) for Group I and 4.5 years (mean, 6.7 years; range, 4.5–10 years) for Group II.
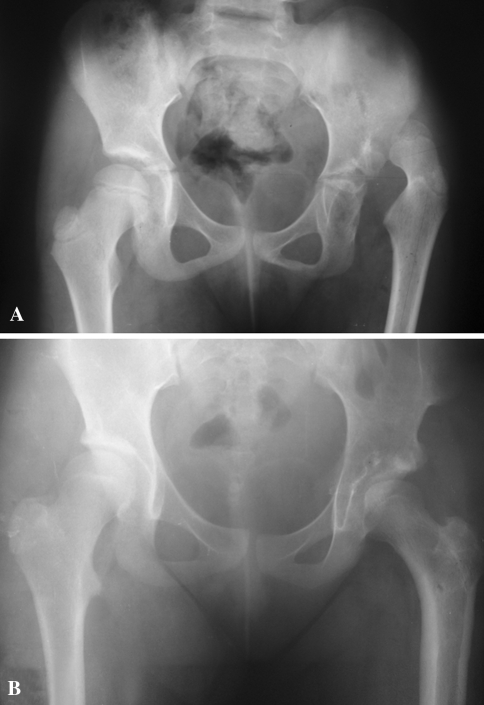
Fig. 1A–B.
(A) Radiographs of a 6.5-year-old girl revealed a Tönnis Grade IV dislocation of the left hip. (B) Open reduction combined with shortening osteotomy, derotation of the femur, and Salter osteotomy was performed. Followup was 10 years (score = 19 points).
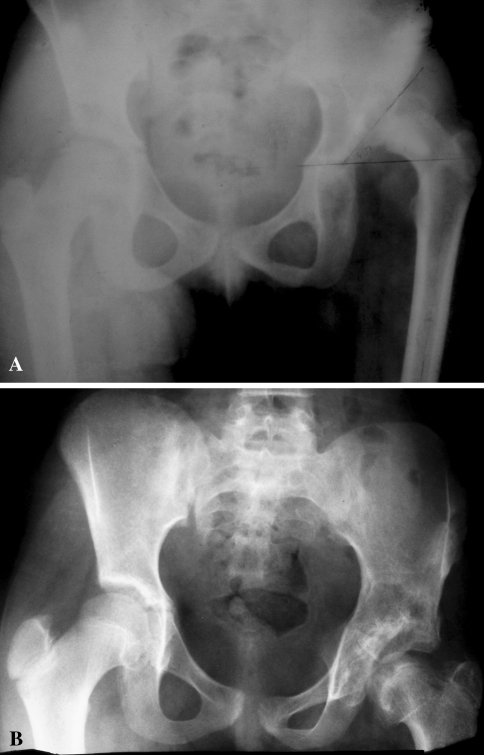
Fig. 2A–B.
(A) An 8.6-year-old girl presented with a Tönnis Grade IV dislocation of the left hip. (B) Open reduction was combined with shortening osteotomy, derotation of the femur, and Salter osteotomy. Followup was 7.5 years (score = 16 points).
Table 1.
Method of assessment using the modified score system of Trevor et al. [23]
| Symptoms/Signs | Severity (points) | |
|---|---|---|
| Pain | ||
| None | 3 | |
| Occasional | 2 | |
| Persistent | 1 | |
| Movement | ||
| Full | 5 | |
| Slight limitation but no fixed deformity | 4 | |
| More than half the normal range | 3 | |
| Less than half the normal range but some fixed deformity | 2 | |
| Little | 1 | |
| Limp | ||
| Absent | 1 | |
| Present | 0 | |
| Function* | ||
| Full | 3 | |
| Slightly limited | 2 | |
| Severely limited | 1 | |
| Radiological features | ||
| CE of Wiberg [24] | ||
| Age < 14 years | Age ≥ 14 years | |
| ≥20° | ≥25° | 4 |
| 15°–19° | 20°–24° | 3 |
| 10°–14° | 15°–19° | 2 |
| <10° | <15° | 1 |
| Appearance of femoral head | ||
| Normal | 3 | |
| Partial coxa plana or coxa magna | 2 | |
| Complete coxa plana or other severe deformity | 1 | |
| Shenton’s line | ||
| Intact | 1 | |
| Broken | 0 | |
*as described by the patient and assessed in the followup clinic.
The one-stage procedure consisted of open reduction, Salter osteotomy, femoral derotation, and shortening osteotomy. The surgical approach was made with two incisions. One of them was a Smith-Peterson incision and the other was lateral proximal femoral. We performed the soft tissue procedure according to the original Salter technique. The capsule was incised in a T-shape, with one cut parallel to the acetabular rim, extending from the inferior to the posterosuperior aspect of the acetabulum, and a transverse incision along the femoral neck. The transverse acetabular ligament was divided. An anterior approach to the hip, innominate osteotomy, psoas tendon release, femoral derotation, and shortening osteotomy were routine procedures. The femur was osteotomized at the level of the subtrochanteric femur through a lateral incision and shortened by 1 cm to 2.5 cm, in order to achieve a force-free reduction. The derotation of the femur was performed in association with the shortening. The amount of correction of derotation or femoral shortening was decided intraoperatively under direct visualization. Varus position was not added to decrease the neck shaft angle. None of the femoral heads were fixed to the acetabulum by a Kirschner wire for maintenance of reduction.
Postoperatively we applied a hip spica cast. The cast was removed after 6 weeks, and a full-time abduction brace was worn for 6 weeks.
Clinical and radiological evaluations were carried out in accordance with a modified score system of Trevor et al. [21, 23] (Table 1). The maximum score on this system is 20 points and the minimum 5. Hips with a score of 18–20 points were considered excellent, 15–17 good, 12–14 fair, and below 12 poor. The evaluations and measurements were made by an orthopaedic surgeon (OC) who was not involved in care of the patients. The same surgeon also assessed radiographs at diagnosis, immediately postoperatively, and at the latest review. The preoperative radiographs showed the amount of displacement of the femoral head and the acetabular index [22]. The reduction of the femoral head, situation of the iliac osteotomy, and the femoral plating were reviewed in radiographs of the hip immediately after operation. The latest followup radiographs were used to measure the acetabular index and the center-edge angle of Wiberg [24]. Radiographic evidence of osteonecrosis (ON) in the femoral head was evaluated according to the system of Kalamachi and MacEwen [13]: Grade I = changes affecting the ossific nucleus; Grade II = lateral physeal damage; Grade III = central physeal damage; and Grade IV = total damage to the femoral head and physis. We measured the limb length clinically from anterosuperior iliac spine to medial malleoli. We considered differences less than 1 cm to reflect equal limb lengths given the variability and inaccuracy of this measure.
We used the nonparametric Mann-Whitney U test (for numerical data) and Fisher’s exact test (for categorical data) to evaluate differences in outcomes between different age groups. For Group I we used 5.5 years to determine differences between ages and for Group II we used 8 years; these were arbitrarily chosen. Spearman’s correlation analysis was used to determine magnitude of correlations between patients’ ages and the scores. Analyses were performed using SPSS 12.0 (SPSS Inc, Chicago, IL).
Results
In Group I, the mean modified scores of patients younger than 5 years of age was greater (p = 0.039) than those older than 5.5 years of age (18 ± 2.9 and 15.3 ± 3.3, respectively). We observed a negative correlation (r = 0.546, p = 0.009) between patients’ ages and their scores. In Group II we observed higher (p = 0.033) scores in children younger than 8 years of age, compared with those older than 8 years of age (17 ± 2.8 and 14.6 ± 2.1, respectively). At the end of followup, according to the modified scores, in Group I’s 11 bilateral dislocations 13 hips (59.1%) were rated excellent (Fig. 3A–B), three hips (13.6%) were good, and six hips (27.3%) were fair. In Group II (29 unilateral dislocations), 14 hips (48.3%) were rated excellent, nine hips (31%) were rated good, and six hips (20.7%) were fair. We observed a negative correlation (p = 0.001) between patients’ ages and their scores in Group II (r = −0.574).
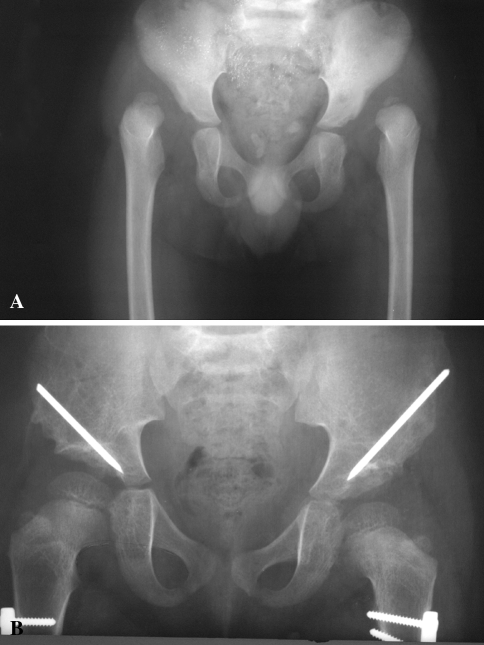
Fig. 3A–B.
(A) Radiographs show Tönnis Grade IV dislocation in a 3-year-old girl with bilateral hip dislocation. (B) One-stage combined surgery was performed on the right side and on the contralateral side 3 months later. The 5-year postoperative radiograph (score = 20 points).
In Group I the acetabular index decreased from a preoperative mean of 36.9° (range, 31°–44°) to 20.2° (range, 15°–26°) at followup. The mean center-edge angle was 25.5° (range, 14°–36°) at followup. In Group II the acetabular index decreased from a mean of 38° (range, 29°–50°) preoperatively to 18.9° (range, 12°–32°) at followup. The mean center-edge angle was 28° (range, 14°–38°) at followup (Table 2).
Table 2.
Summary of patient data
| Case | Gender | Age (years) | Followup (years) | Acetabular index (degrees) | CE [24] | Modified Trevor system [23] | AVN [13] | |
|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | |||||||
| 1* | F | 4.5 | 8.5 | 42 | 17 | 30 | 20 | |
| 5 | 8 | 38 | 15 | 36 | 19 | |||
| 2* | F | 3.5 | 5.5 | 31 | 18 | 26 | 17 | I |
| 4 | 6 | 30 | 19 | 26 | 19 | I | ||
| 3* | F | 3.5 | 5 | 43 | 16 | 34 | 20 | |
| 3.8 | 5 | 44 | 17 | 32 | 20 | |||
| 4* | F | 4 | 5 | 38 | 20 | 35 | 20 | |
| 4.5 | 4.5 | 40 | 23 | 15 | 12 | III | ||
| 5* | F | 3 | 5 | 35 | 26 | 24 | 20 | |
| 3.3 | 4.7 | 32 | 23 | 28 | 20 | |||
| 6* | F | 4 | 6 | 41 | 26 | 14 | 12 | II |
| 4.5 | 5.5 | 34 | 17 | 31 | 16 | |||
| 7* | M | 5 | 5 | 34 | 17 | 26 | 19 | |
| 5.5 | 4.5 | 35 | 24 | 15 | 12 | II | ||
| 8* | F | 6 | 6 | 38 | 20 | 22 | 18 | I |
| 6.5 | 5.5 | 40 | 19 | 23 | 18 | I | ||
| 9* | F | 7 | 4.4 | 31 | 16 | 32 | 18 | II |
| 7.4 | 4 | 33 | 15 | 30 | 12 | IV | ||
| 10* | F | 7 | 5 | 38 | 26 | 22 | 20 | |
| 7.3 | 4.7 | 37 | 24 | 15 | 12 | IV | ||
| 11* | F | 9 | 6 | 40 | 22 | 24 | 16 | I |
| 9.5 | 5.5 | 41 | 24 | 15 | 12 | III | ||
| 12 | F | 3.1 | 6 | 31 | 14 | 35 | 20 | |
| 13 | F | 3.2 | 6.5 | 29 | 14 | 32 | 19 | I |
| 14 | M | 4.4 | 6.5 | 40 | 14 | 34 | 20 | |
| 15 | M | 4.6 | 5.5 | 45 | 30 | 30 | 18 | I |
| 16 | M | 5.4 | 6.4 | 35 | 12 | 38 | 18 | |
| 17 | F | 5.5 | 10 | 45 | 23 | 16 | 13 | IV |
| 18 | F | 5.5 | 5 | 36 | 19 | 31 | 19 | |
| 19 | F | 5.6 | 6 | 44 | 14 | 36 | 18 | |
| 20† | F | 5.8 | 7 | 32 | 16 | 34 | 15 | I |
| 21 | M | 6 | 8 | 40 | 20 | 30 | 20 | |
| 22 | F | 6.2 | 7 | 36 | 20 | 29 | 17 | I |
| 23 | F | 6.4 | 6.2 | 35 | 16 | 32 | 19 | |
| 24 | M | 6.4 | 5 | 29 | 20 | 25 | 20 | |
| 25 | F | 6.5 | 10 | 31 | 20 | 33 | 19 | I |
| 26†† | F | 6.8 | 6 | 36 | 23 | 14 | 12 | II |
| 27 | F | 7 | 5.5 | 50 | 19 | 15 | 12 | II |
| 28 | F | 7.2 | 5 | 40 | 14 | 32 | 18 | I |
| 29 | M | 7.4 | 6.4 | 38 | 19 | 26 | 15 | I |
| 30 | F | 7.4 | 8 | 39 | 24 | 20 | 12 | III |
| 31 | F | 7.5 | 4.5 | 37 | 21 | 20 | 17 | II |
| 32 | F | 7.8 | 6 | 38 | 21 | 24 | 16 | |
| 33 | F | 7.9 | 10 | 40 | 19 | 26 | 18 | |
| 34 | F | 8.2 | 5.5 | 46 | 32 | 21 | 15 | IV |
| 35 | F | 8.4 | 7 | 41 | 16 | 30 | 15 | II |
| 36 | F | 8.4 | 8 | 37 | 16 | 26 | 15 | II |
| 37 | F | 8.6 | 7.5 | 39 | 18 | 35 | 16 | I |
| 38 | F | 8.6 | 6 | 35 | 18 | 35 | 18 | |
| 39 | F | 9 | 5.8 | 34 | 18 | 23 | 12 | III |
| 40 | F | 10 | 7 | 36 | 17 | 32 | 12 | IV |
* = patients with bilateral DDH; CE = center edge; AVN = avascular necrosis; † = postoperative supracondylar femoral fracture; †† = postoperative femoral shaft fracture.
Osteonecrosis of the femoral head occurred in 12 hips in Group I and 18 hips in Group II (Fig. 4A–C) (Table 2). In Group II osteonecrosis occurred in more children (p = 0.011) older than 5.5 years than those 5 years old or younger (eight of nine versus four of 13, respectively). However, we found no difference in numbers of patients with osteonecrosis in those 8 years old or younger and those over 8 years old (12 of 22 versus six of seven, respectively).
Fig. 4A–C.
(A) Radiographs of a 5.5-year-old girl show a Tönnis Grade IV dislocation of the left hip. (B) Open reduction was combined with shortening osteotomy, derotation of the femur, and Salter osteotomy. Type IV ON developed 1 year later. (C) Followup was 10 years (score = 13 points).
We encountered no cases of nerve or vessel damage or deep wound infections. At the time of followup examination all 11 patients in Group I had equal limb length. We found a limb length discrepancy of more than 1.5 cm in four patients in Group II, three of whom noticeably limped. A supracondylar femoral fracture developed in one patient during rehabilitation postoperatively at 2.5 months. One patient suffered from femoral shaft fracture following minor trauma 2 weeks after the abduction brace was removed. Both fractures were treated with casting and both healed without complications.
Discussion
Early treatment of DDH is desirable because results of treatment depend upon the age of the patient when treatment begins [3, 4, 6–8]. We asked if age affected outcome in patients with neglected DDH with unilateral or bilateral dislocation who underwent one-stage combined procedures.
Our study had major limitations. The medical records were reviewed retrospectively; we did not see patients at final followup specifically for this study, and the medical records might not be entirely reliable. Limb length, in particular, could be subject to variations. We used a categorical rating system; these are often subject to greater interobserver variability; the scoring system of Trevor et al. [23] was reported in 1975 and has never been validated against any independent measure. Further, all measurements were carried out by a single author (OC). That eliminates interobserver variability, but might introduce systematic bias and we do not have data on the interobserver variability of our measurements. Because followup ranged from 4 to 10 years, the long-term clinical outcome of procedures is not known in terms of osteoarthritis and other possible problems.
The age at which open reduction is no longer reasonable in a child is unknown, although the indications for surgery appear to broaden every few years [19]. We believe the one-stage approach to all hip abnormalities in late-diagnosed DDH is reasonable; there remains some potential for growth and remodeling [4, 8, 14], although the potential decreases by age 8.
Several authors accept a surgical approach but also suggest the results are worse as age increases [1, 14, 18]. Large series of neglected DDH were presented by Ashley et al. [1], Klisic et al. [15, 16], and Galpin et al. [7], who advocate open reduction with concurrent shortening of the femur and report satisfactory results. Ryan et al. [19] reported on 18 children (25 hips) with previously untreated DDH who had a one-stage combined operation between the ages of 3 and 10 years. Twenty-three (92%) of those hips had Iowa hip scores of 80 to 100 an average of 10.5 years after the procedure. The authors recommended the procedure, which can result in remodeling of the acetabulum and the formation of a functional hip, for patients from 3 to 10 years of age. Most studies include several modalities of treatment, and it is difficult to analyze the influence of a specific factor or treatment [9]. Karakaş et al. [14] reported the results of one-stage combined operations in 47 children (55 hips) who were at least 4 years old. Forty-seven hips had been managed with preoperative traction. They obtained 67% clinically and 65% radiographically good or excellent results according to McKay and Severin criteria an average of 7.5 years after surgery. Ganger et al. [8] reviewed 42 patients (54 hips) in which 18 hips were treated with open reduction and 36 hips were treated with one-stage combined procedures. The mean patient age at the time of surgery was 4 years. After a mean followup of 3.5 years, 43 hips (80%) were classified as good or excellent results according to Severin classification. Dimitriou and Cavadias [4] reviewed 52 patients (67 hips) whose age at the time of surgery ranged from 3 to 14 years. After a mean followup period of 11 years, 66 hips (98%) were rated 14 to 20 points according to Muller and Sedon criteria. Forlin et al. [6] reviewed 24 hips of 20 patients treated after the age of 4 years (range, 4–12 years). The mean length of followup was 5 years. Seventy percent of the hips had excellent or good results according to McKay and Severin criteria. They reported worse outcomes in patients older than 7 years at the time of surgery. In our series, there were 11 patients (22 hips) in the bilateral dislocation group (Group I). Of the 11 patients, seven (13 hips) were younger than 5.5 years old and five (nine hips) were older than 5.5 years old at the time of the surgery. Our results suggest patients who had bilateral DDH and were treated with a one-stage combined procedure before the age of 5.5 years had better results than did patients who had the operation after that age. Modified scores of Trevor et al. [23] showed the patients with DDH who were treated with a one-stage combined operation before the age of 8 years had better results than did patients who had the operation after that age. We also observed a negative correlation between patients’ ages and their scores in Group II. Our results are similar to other reports [16, 17, 19, 20]. The followup period in our study has not been long enough to provide an adequate long-term evaluation of the primary operation.
Osteonecrosis of the femoral head is still a severe complication after treatment of DDH [2, 9]. Our patients who had bilateral DDH and were treated with a one-stage combined operation before the age of 5.5 years had better results in regard to ON than did patients who had the operation after the age of 5.5 years. These data support those of other investigators [14, 19]. Ryan et al. [19] reported 13 patients (three of 15 hips) younger than 7 years old suffered ON, whereas this ratio increased to 70% in 5 patients (10 hips) older than 7 years old. However, the ON outcome shows the patients with DDH treated by one-stage combined operations before the age of 8 years were not different from patients who had the operation after age 8. Although the prevalence of ON was high in our study (35.3%, types II, III, and IV), it is similar to that reported in studies using similar methods for the evaluation of ON [5, 13, 19].
Surgery before the age of 8 years for unilateral and 5.5 years for bilateral hip dislocation had better results than surgery after that age. However, age and unilateral or bilateral dislocation should not be an absolute criterion for decision-making. A thorough case-by-case evaluation is preferable.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ashley RK, Larsen LJ, James PM. Reduction of dislocation of the hip in older children. A preliminary report. J Bone Joint Surg Am. 1972;54:545–550. [PubMed]
- 2.Böhm P, Klinger HM, Küsswetter W. The Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in young adults. Arch Orthop Trauma Surg. 1999;119:186–189. [DOI] [PubMed]
- 3.Browne RS. The management of late diagnosed congenital dislocation and subluxation of the hip-with special reference to femoral shortening. J Bone Joint Surg Br. 1979;61:7–12. [DOI] [PubMed]
- 4.Dimitriou JK, Cavadias AX. One-stage surgical procedure for congenital dislocation of the hip in older children. Long-term results. Clin Orthop Relat Res. 1989;246:30–38. [PubMed]
- 5.Domzalski M, Synder M. Avascular necrosis after surgical treatment for development dysplasia of the hip. Int Orthop. 2004;28:65–68. [DOI] [PMC free article] [PubMed]
- 6.Forlin E, Munhoz da Cunha LA, Figueiredo DC. Treatment of developmental dysplasia of the hip after walking age with open reduction, femoral shortening, and acetabular osteotomy. Orthop Clin North Am. 2006;37:149–160. [DOI] [PubMed]
- 7.Galpin RD, Roach JW, Wenger DR, Herring JA, Birch JG. One-stage treatment of congenital dislocation of the hip in older children, including femoral shortening. J Bone Joint Surg Am. 1989;71:734–741. [PubMed]
- 8.Ganger R, Radler C, Petje G, Manner HM, Kriegs-Au G, Grill F. Treatment options for developmental dislocation of the hip after walking age. J Pediatr Orthop B. 2005;14:139–150. [DOI] [PubMed]
- 9.Gulman B, Tuncay IC, Dabak N, Karaismailoglu N. Salter’s innominate osteotomy in the treatment of congenital hip dislocation. A Long-Term Review. J Pediatr Orthop. 1994;14:662–666. [DOI] [PubMed]
- 10.Graf R. Fundamentals of sonographic diagnosis of infant hip dysplasia. J Pediatr Orthop. 1984;4:735–740. [DOI] [PubMed]
- 11.Graf R. The use of ultrasonography in developmental dysplasia of the hip. Acta Orthop Traumatol Turc. 2007;41(Suppl 1):6–13. [PubMed]
- 12.Inan M, Harma A, Ertem K, Germen B, Bowen RJ. Successful treatment of high congenital dislocated hips in older children by open reduction, pelvic and femoral osteotomy with external fixator stabilization (average 8.2 years of age). J Pediatr Orthop B. 2005;14:405–409. [DOI] [PubMed]
- 13.Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62:876–888. [PubMed]
- 14.Karakas ES, Baktir A, Argun M, Turk CY. One-stage treatment of congenital dislocation of the hip in older children. J Pediatr Orthop. 1995;15:330–336. [DOI] [PubMed]
- 15.Klisic P, Jankovic L. Combined procedure of open reduction and shortening of the femur in treatment of congenital dislocation of the hips in older children. Clin Orthop Relat Res. 1976;119:60–69. [PubMed]
- 16.Klisic P, Jankovic L, Basara V. Long-term results of combined operative reduction of the hip in older children. J Pediatr Orthop. 1988;8:532–534. [DOI] [PubMed]
- 17.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–1792. [DOI] [PubMed]
- 18.Papavasiliou VA, Papavasiliou AV. Surgical treatment of developmental dysplasia of the hip in the periadolescent period. J Orthop Sci. 2005;10:15–21. [DOI] [PubMed]
- 19.Ryan MG, Johnson LO, Quanbeck DS, Minkowitz B. One-stage treatment of congenital dislocation of the hip in children three to ten years old. Functional and radiographic results. J Bone Joint Surg Am. 1998;80:336–344. [DOI] [PubMed]
- 20.Salter RB, Dubos JP. The first fifteen years’ personal experience with innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip. Clin Orthop Relat Res. 1974;98:72–103. [DOI] [PubMed]
- 21.Shih CH, Shih HN. One-stage combined operation of congenital dislocation of the hips in older children. J Pediatr Orthop. 1988;8:535–539. [DOI] [PubMed]
- 22.Tönnis D. Surgical treatment of congenital dislocation of the hip. Clin Orthop Relat Res. 1990;258:33–40. [PubMed]
- 23.Trevor D, Johns DL, Fixsen JA. Acetabuloplasty in the treatment of congenital dislocation of the hip. J Bone Joint Surg Br. 1975;57:167–174. [PubMed]
- 24.Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Acta Chir Scand. 1939;83(Suppl 58):33–38.