Abstract
Early diagnosis of scapholunate interosseous ligament tears with distal radius fractures is likely important in treatment and outcome, but identification of these injuries has not been well explored. We asked whether there was a difference in the scapholunate interval between high-grade and low-grade tears of the scapholunate interosseous ligament in distal radius fractures, the best position of the wrists to identify any differences; we also asked what gap width accurately identified high-grade tears on fluoroscopic evaluation. We fluoroscopically evaluated the scapholunate gap in six different wrist positions and then performed arthroscopic examination in 45 distal radius fractures in 44 consecutive patients. The tears were classified as high-grade (Grade 3 or greater) or low-grade (Grade 2 or less) based on arthroscopic findings. We then compared the scapholunate gap measured on fluoroscopic images between the high-grade tear group and the low-grade tear group and between the different positions of the same wrist. The scapholunate gap was wider in the high-grade tear group than in the low-grade tear group and wider in ulnar deviation than in radial deviation. A 2-mm scapholunate gap appeared the best cutoff point for the fluoroscopic diagnosis. We concluded fluoroscopic examination is a good test for identifying high-grade tears of the scapholunate interosseous ligament in distal radius fractures.
Level of Evidence: Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
A high incidence of intercarpal soft tissue injuries has been noted in association with distal radius fractures. Injury to the scapholunate interosseous ligament (SLIL) has been reported to occur in 16% to 40% of patients with distal radius fractures [9, 23, 25], injury to the lunotriquetral ligament injury in 8.5% to 15% of patients [9, 25], and injury to the triangular fibrocartilage complex in 39% to 43% [9, 25].
The SLIL is one of the most important intercarpal ligaments. An isolated, complete tear of the SLIL results in scapholunate instability [19, 27, 28, 34] and in some patients leads to osteoarthritis of the wrist through a specific pattern, the so-called scapholunate advanced collapse wrist [33, 34]. Scapholunate interosseous ligament injury, when associated with distal radius fractures, causes progressive deterioration of the intercarpal relationship as well [6, 13, 30]. Patients with SLIL injury and associated distal radius fractures have worse wrist function than those with distal radius fracture alone [30]. Grade 3 SLIL injury associated with distal radius fractures results in increased scapholunate joint pain and scapholunate dissociation [6]. Early recognition and proper management of SLIL injuries may be helpful in predicting and preventing development of the chronic wrist disabilities in distal radius fractures [36].
Scapholunate interosseous ligament injuries can be diagnosed by various imaging modalities, including radiography, fluoroscopy, arthrography, MRI, and arthroscopy. Although wrist arthroscopy is the gold standard for evaluation of the scapholunate interval because it can directly evaluate the ligament and the scapholunate joint space [8], it cannot be performed in all patients with distal radius fractures because of invasiveness and cost. Fluoroscopy may be more appropriate as the first imaging method of SLIL injuries in that it is noninvasive and inexpensive. However, specific diagnostic criteria for SLIL injuries have not been determined. Some previous studies have been performed for kinematic analysis or as an aid to arthrographic evaluation of the scapholunate joint [3, 10, 21, 24].
We asked whether fluoroscopy could be used to identify differences in the scapholunate gap between high-grade and low-grade tears of the SLIL in distal radius fractures, what position of the wrist best identified any differences, and what gap width provided the highest accuracy on fluoroscopic evaluation in high-grade SLIL tears.
Materials and Methods
We fluoroscopically evaluated the scapholunate gap of 44 selected patients (45 fractures) with distal radius fractures in six different wrist positions in patients with distal radius fractures and then performed an arthroscopic examination. Wrists were classified as high-grade tear group (Grade 3 or greater in the system of Geissler et al. [9]) or low-grade tear group (Grade 2 or less) according to arthroscopic finding. The scapholunate gap measured on fluoroscopic images was compared between the high-grade tear group and the low-grade tear group and between the different positions of the same wrist. The best cutoff point of the scapholunate gap was obtained using receiver operating characteristic (ROC) curve analysis. Prior approval was obtained from our Institutional Review Board, and informed consent for participation in the study was provided by all of the patients evaluated.
We saw 72 patients with distal radius fractures between March 2003 and May 2004. For this study, we included patients with distal radius fractures with dorsal angulation greater than 20°, radial shortening greater than 5 mm, or intraarticular fracture with stepoff or gap greater than 1 mm. Patients (n = 6) with a history of wrist sprain for more than 4 weeks were excluded to rule out those with old SLIL injuries. With these criteria, we enrolled 44 patients (13 men, 31 women; average age, 50 years) with 45 fractures. According to Frykman’s classification [7], two fractures were Type I, five were Type II, 14 were Type III, 11 were Type IV, one was Type V, two were Type VI, one was Type VII, and nine were Type VIII. For 35 intraarticular fractures, the average maximum displacement in the initial radiograph was 1.4 ± 1.2 mm and the average maximum gap displacement in the initial radiograph was 2.5 ± 2.0 mm. The average maximum displacement correlated (r = 0.47, p = 0.04) with increasing grades of SLIL tear whereas the average maximum gap displacement did not (r = 0.29, p = 0.23). There were two open fractures with pinpoint-sized wounds (Gustilo and Anderson Type 1 [11]) on the volar-ulnar surface of the wrists. At the time of arthroscopy, SLIL injuries were classified (BCK) as described by Geissler et al. (Table 1) [2]. We considered wrists without injury and those with Grade 1 or 2 injury in the low-grade tear group and wrists with Grade 3 or 4 injury in the high-grade tear group. Our rationale for this classification was twofold. As the fluoroscopic diagnosis of SLIL injury is made by widening of the scapholunate joint space, low-grade tear of SLIL is not likely to be identified by fluoroscopy because by definition the scapholunate joint space cannot be widened with a probe or an arthroscope in this type of injury. However, high-grade tear of SLIL is likely to be identified by fluoroscopy as the scapholunate joint space can be widened with a probe or an arthroscope in this type of injury. Scapholunate diastasis is absent in all Grade 1 or 2 SLIL injuries associated with distal radius fractures whereas it is present in approximately ½ of Grade 3 and all Grade 4 SLIL injuries associated with distal radius fractures [16]. In addition, the clinical course of high-grade tear appears different from that of low-grade tear [22, 33, 34]. High-grade tear of the SLIL results in progressive deterioration of the wrist function [33, 34] whereas low-grade tear of SLIL does not [22]. To detect a mean difference of 0.5 mm in the scapholunate gap with 80% power, a sample size of 16 patients per treatment group was required. The low-grade tear group consisted of 18 females and eight males with an average age of 49.3 years (range, 22–85 years); 18 had injuries to the right wrist and eight to the left wrist. The high-grade tear group consisted of 12 females and six males with an average age of 50.5 years (range, 17–81 years); 10 had injuries to the right wrist and nine to the left wrist (one female patient had injuries to both wrists). Gender distribution and average age were similar (p > 0.05) between groups. Nine wrists did not have SLIL injuries, whereas six had Grade 1, 11 had Grade 2, 17 had Grade 3, and two had Grade 4 injuries.
Table 1.
Arthroscopic classification of scapholunate interosseous ligament injury by Geissler et al. [9]
| Grade | Scapholunate interosseous ligament in radiocarpal portal | Scapholunate joint in midcarpal portal |
|---|---|---|
| 1 | Attenuation or hemorrhage | No incongruency |
| 2 | Attenuation or hemorrhage | Incongruency, gap less than probe width |
| 3 | Incongruency or stepoff | Incongruency, probe passable between scaphoid and lunate |
| 4 | Incongruency or stepoff | Incongruency, 2.7-mm scope passable between scaphoid and lunate |
Modified from Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357–365. Reprinted with permission from Journal of Bone and Joint Surgery, Inc.
All fluoroscopic and arthroscopic examinations were performed by one surgeon (BCK) during surgery. Forty-three fractures underwent closed or mini-open reduction and fixation of extraarticular fragments with Kirschner wires under fluoroscopic guidance. When closed reduction was inadequate, mini-open reduction was performed by making a 1-cm dorsal midline incision centered over the fracture site and elevating the unreduced fracture fragment with a freer elevator. No open reductions, in which the dorsal capsule of the wrist was opened, were performed. Two radial styloid fractures underwent closed reduction and temporary fixation with Kirschner wires; these were replaced with cannulated screws after fluoroscopic and arthroscopic examinations.
All fluoroscopic examinations were performed after closed or mini-open reduction and Kirschner wire fixation. Under the guidance of a fluoroscope (OEC® 9800 Plus; GE Healthcare, Piscataway, NJ) and with the patient in the supine position, the forearm was pronated with the wrist in neutral deviation to determine the position in which the ulnar cortex of the scaphoid and the radial cortex of the lunate were sharply outlined in profile. Then, fluoroscopic images were taken at maximum magnification with the wrist in three positions: neutral, radial, and ulnar deviation. The magnification of the images, which was approximately three times, was provided by fluoroscopy and could be increased by lowering the position of the image intensifier with the C-arm set in an inverted position. Each fluoroscopic image included a 2-mm-wide Kirschner wire, which was placed on the ulnar side and between the palmar and dorsal surfaces of the wrist and used as a reference for later correction of magnification. The same procedure was performed in the forearm-supinated position, resulting in fluoroscopic images of a wrist in six different positions, ie, pronation ulnar deviation (PU), pronation neutral deviation (PN), pronation radial deviation (PR), supination ulnar deviation (SU), supination neutral deviation (SN), and supination radial deviation (SR). A true lateral image of each wrist, in which the volar cortex of the pisiform lay between the volar margins of the head of the capitate and the distal pole of the scaphoid (scaphoid-pisiform-capitate lateral), was acquired with the wrist in the neutral position [18]. All fluoroscopic images in all six positions were saved to a disk and later printed.
After fluoroscopic evaluation, standard arthroscopic examination of the radiocarpal and midcarpal joints was performed using a 1-mm-wide probe and a 2.7-mm-wide arthroscope [37]. Briefly, the wrist was suspended in a traction tower and 4.5 kg traction was applied. Traction with 4.5 kg did not displace previously fixed fracture fragments in any of our cases. A 3-4 and 4-5 portal was used to examine the radiocarpal joint. A midcarpal radial and midcarpal ulnar portal was used to examine the midcarpal joint. Intraarticular fragments were reduced and fixed during arthroscopic examination.
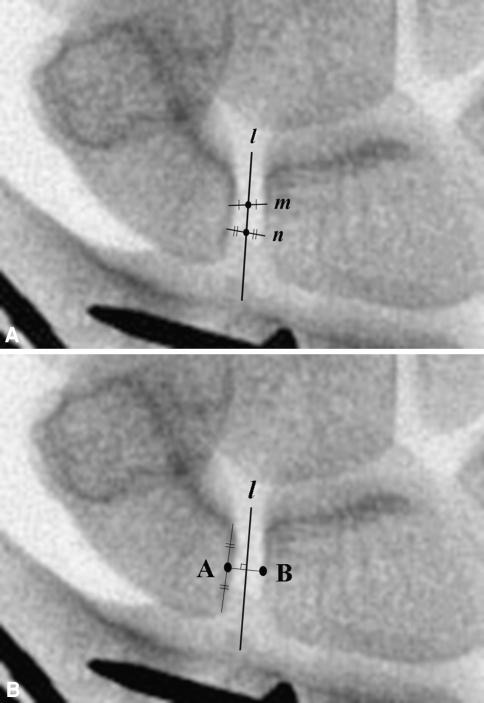
Two orthopaedic surgeons (BCK, HCA) measured each scapholunate gap on each of the six fluoroscopic images for each patient with electrical calipers (Mitutoyo, Kawasaki, Japan), which are accurate to 0.01 mm. A line was drawn from any point on the ulnar cortex of the scaphoid to any point on the radial cortex of the lunate (Line m, Fig. 1A), a second line was drawn in the same fashion (Line n, Fig. 1A), and a point was marked in the middle of each line. The two points were connected, making a line that bisected the scapholunate joint (Line l, Fig. 1A). Another line was drawn along the flat surface of the ulnar cortex of the scaphoid. From the middle of this line (Point A, Fig. 1B), a line vertical to the scapholunate joint-bisecting line was drawn to the radial cortex of the lunate (Point B, Fig. 1B). This line was named the scapholunate gap line and the length of this line was defined as the scapholunate gap (Fig. 1B).
Fig. 1A–B.
The measurement method of the scapholunate gap is shown. (A) A line was drawn from any point on the ulnar cortex of the scaphoid to any point on the radial cortex of the lunate (Line m) followed by a second line drawn in the same fashion (Line n). The point in the middle of each line was connected, making a line bisecting the scapholunate joint (Line l). (B) A drawing of a scapholunate gap line is shown. From the middle of the flat surface of the ulnar cortex of the scaphoid (Point A), a line was drawn vertical to Line l. Point B is the point where this line meets the radial cortex of the lunate. This line is called the scapholunate gap line and the length of this line is the scapholunate gap.
The scapholunate angle in the lateral image of each wrist in the neutral position was measured by two orthopaedic surgeons (BCK, HCA) with a goniometer and using the tangential method [8]. The measured scapholunate gap was corrected for differences in magnification with the aid of a 2-mm-wide Kirschner wire using the following ratio: true scapholunate gap = measured scapholunate gap × true width of 2-mm Kirschner wire/measured width of 2-mm Kirschner wire. Our measurement of the scapholunate gap showed an intraobserver intraclass correlation coefficient of 0.86 (95% confidence interval [CI], 0.75–0.92) as computed by a one-way random intraclass correlation model and an interobserver intraclass correlation coefficient of 0.73 (95% CI, 0.6–0.86) as computed by a two-way random intraclass correlation model, which corresponded to high agreement and substantial agreement, respectively [5, 29].
We used the Mann-Whitney U test to compare scapholunate gap in the same wrist position between the low-grade and high-grade tear groups to determine whether there was a difference in scapholunate gap between two groups. We used the Wilcoxon signed rank test to compare scapholunate gaps between two different wrist positions, ie, ulnar deviation versus radial deviation, ulnar deviation versus neutral deviation, and radial deviation versus neutral deviation with the forearm in supinated and pronated positions, to identify the best position of the wrist for the fluoroscopic evaluation. To determine the optimum cutoff point, or the diagnostic criterion, of the scapholunate gap for fluoroscopic diagnosis of high-grade SLIL tear, a ROC curve was fitted to the fluoroscopic data with arthroscopic diagnosis (high-grade tear or low-grade tear) as the reference standard. The cutoff value at the left upper corner of each curve, indicative of optimum threshold, was calculated, as well as the area under the curve, which is indicative of diagnostic accuracy. The sensitivity and specificity of fluoroscopic examination were calculated using this cutoff value. The association between the scapholunate gap and the grade of injury was analyzed using Spearman rank correlation. We used SPSS 11.0 software (SPSS Inc, Chicago, IL).
Results
The scapholunate gap in the high-grade tear group was wider than that in the low-grade tear group in all the tested positions (p = 0.001 in PR, p < 0.001 in PN, p = 0.008 in PU, p < 0.001 in SR, p < 0.001 in SN, and p < 0.001 in SU; Table 2). The scapholunate gap became wider (ρ = 0.61; p < 0.001) as grade of injury increased (Table 3).
Table 2.
The scapholunate gap (mm) in different positions of the wrist
| Group | PR | PN | PU | SR | SN | SU |
|---|---|---|---|---|---|---|
| Low-grade (n = 26) | 1.7 ± 0.4 | 1.9 ± 0.4 | 1.9 ± 0.6 | 1.7 ± 0.4 | 1.8 ± 0.3 | 1.9 ± 0.4 |
| High-grade (n = 19) | 2.1 ± 0.4 | 2.4 ± 0.5 | 2.4 ± 0.4 | 2.2 ± 0.3 | 2.5 ± 0.6 | 2.6 ± 0.7 |
| p value | 0.001 | < 0.001 | 0.008 | < 0.001 | < 0.001 | < 0.001 |
Values are mean ± standard deviation; PR = pronation radial deviation; PN = pronation neutral; PU = pronation ulnar deviation; SR = supination radial deviation; SN = supination neutral; SU = supination ulnar deviation.
Table 3.
Scapholunate gap (mm) according to the grading of scapholunate interosseous ligament injury in different positions of the wrist
| Grade of injury | PR | PN | PU | SR | SN | SU |
|---|---|---|---|---|---|---|
| Normal (n = 9) | 1.6 ± 0.4 | 1.8 ± 0.3 | 1.9 ± 0.4 | 1.5 ± 0.2 | 1.8 ± 0.3 | 1.9 ± 0.3 |
| Grade 1 (n = 6) | 1.5 ± 0.3 | 1.8 ± 0.3 | 1.7 ± 0.5 | 1.7 ± 0.2 | 1.7 ± 0.1 | 1.6 ± 0.2 |
| Grade 2 (n = 11) | 1.8 ± 0.4 | 2.1 ± 0.4 | 2.1 ± 0.7 | 1.9 ± 0.5 | 1.9 ± 0.4 | 2.1 ± 0.5 |
| Grade 3 (n = 17) | 2.1 ± 0.4 | 2.3 ± 0.4 | 2.3 ± 0.4 | 2.2 ± 0.3 | 2.5 ± 0.6 | 2.6 ± 0.7 |
| Grade 4 (n = 2) | 2.1 ± 0.6 | 3.0 ± 0.3 | 2.8 ± 0.6 | 2.3 ± 0.0 | 2.7 ± 0.6 | 2.8 ± 0.7 |
| Spearman’s ρ | 0.504 | 0.610 | 0.546 | 0.702 | 0.619 | 0.556 |
| p value | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 | < 0.001 |
Values are mean ± standard deviation; PR = pronation radial deviation; PN = pronation neutral; PU = pronation ulnar deviation; SR = supination radial deviation; SN = supination neutral; SU = supination ulnar deviation.
In the low-grade tear group, the average scapholunate gap in all wrist positions was less than 2 mm. The scapholunate gap was widest in ulnar deviation and narrowest in radial deviation (Table 2). The scapholunate gap was larger in ulnar deviation than in radial deviation when the forearm was supinated (p = 0.009) and pronated (p = 0.001). We found no difference between neutral deviation and ulnar deviation (Table 4).
Table 4.
Difference in scapholunate gap (mm) among positions in the same wrist
| Group | PN − PR | PN − PU | PU − PR | SN − SR | SN − SU | SU − SR |
|---|---|---|---|---|---|---|
| Low-grade(n = 26) | 0.2 ± 0.3 | −0.0 ± 0.4 | 0.3 ± 0.33 | 0.1 ± 0.4 | −0.11 ± 0.3 | 0.2 ± 0.4 |
| p value | < 0.001 | 0.777 | 0.001 | 0.137 | 0.103 | 0.009 |
| High-grade (n = 19) | 0.3 ± 0.3 | 0.0 ± 0.4 | 0.2 ± 0.4 | 0.3 ± 0.5 | −0.1 ± 0.6 | 0.4 ± 0.7 |
| p value | < 0.001 | 0.616 | 0.019 | 0.029 | 0.464 | 0.021 |
Values are mean ± standard deviation; PN = pronation neutral; PR = pronation radial deviation; PU = pronation ulnar deviation; SN = supination neutral; SR = supination radial deviation; SU = supination ulnar deviation.
In the high-grade tear group, the average scapholunate gap in all wrist positions was greater than 2 mm (Table 2). The scapholunate gap was widest in ulnar deviation and narrowest in radial deviation. The scapholunate gap was larger in ulnar deviation than in radial deviation when the forearm was supinated (p = 0.021) and pronated (p = 0.019) but not different with neutral and ulnar deviation (Table 4).
The mean scapholunate angle in the lateral position of the wrists was similar (p = 0.3) in the high-grade and low-grade tear groups (48° ± 4.3° and 50° ± 3.8°, respectively). All scapholunate angles were within the normal range, except for that of one patient with a Grade 4 injury who had a scapholunate angle of 75°.
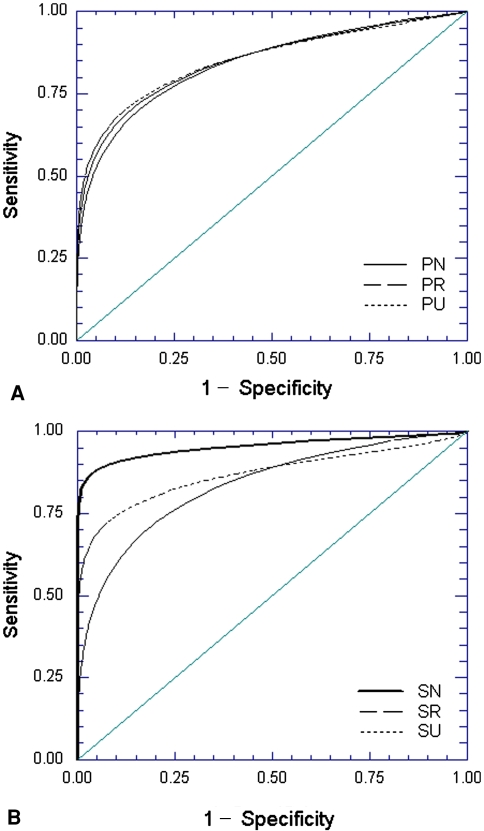
Diagnosis of high-grade tear by fluoroscopy was accurate according to ROC curve analysis, with the area under the curve ranging from 0.79 to 0.87. The diagnostic accuracy of fluoroscopy was similar with the six different wrist positions (Fig. 2; Table 5). The scapholunate gap at the left upper corner of each curve was 2.0 mm in PR, 2.0 mm in PU, 2.2 mm in PN, 2.1 mm in SR, 2.0 mm in SU, and 2.0 mm in SN (Fig. 2; Table 5). Using a 2-mm scapholunate gap as the cutoff point, the sensitivity and specificity of fluoroscopy were 94.7% and 76.9% in PU, 63.2% and 88.5% in PR, 78.9% and 61.5% in PN, 78.9% and 57.8% in SU, 68.4% and 80.8% in SR, and 84.2% and 80.8% in SN.
Fig. 2A–B.
ROC curves of fluoroscopy in the pronation (A) and supination (B) positions are shown. Both curves showed good detectability of scapholunate injury with the area under the curve being at least 0.79. The cutoff point of the scapholunate gap at the left upper corner of each curve was approximately 2 mm in all the wrist positions, which was chosen as a diagnostic criterion of high-grade SLIL injury. PN = pronation neutral; PR = pronation radial deviation; PU = pronation ulnar deviation; SN = supination neutral; SR = supination radial deviation; SU = supination ulnar deviation.
Table 5.
Quantitative analysis of each receiver operating characteristic curve
| Curve | PR | PN | PU | SR | SN | SU |
|---|---|---|---|---|---|---|
| Area under the curve (95% confidence interval) | 0.79 (0.65–0.93) | 0.80 (0.67–0.93) | 0.82 (0.68–0.95) | 0.87 (0.76–0.97) | 0.86 (0.75–0.97) | 0.82 (0.68–0.95) |
| Cutoff value of complete tear (mm)* | 2.03 | 2.21 | 2.02 | 2.05 | 2.02 | 2.03 |
* The cutoff value at the left upper corner; PR = pronation radial deviation; PN = pronation neutral; PU = pronation ulnar deviation; SR = supination radial deviation; SN = supination neutral; SU = supination ulnar deviation.
Discussion
High-grade SLIL tear associated with distal radius fractures is not rare [9, 16, 23, 25] and is likely to result in progressive deterioration of wrist function with increasing wrist pain [6, 13, 30]. Arthroscopy, which is the gold standard for the diagnosis, may not be readily available depending on the condition of the institution, the surgeon, or the insurance, whereas fluoroscopy is widely available, easy to use, and inexpensive. However, fluoroscopy has never been studied for diagnosis of SLIL injury associated with distal radius fractures. We evaluated the value of fluoroscopy in the diagnosis of SLIL injury associated with distal radius fractures, with the following specific questions: (1) was there a difference in scapholunate gap between high-grade and low-grade SLIL tears associated with distal radius fractures by fluoroscopy; (2) what was the best position of the wrist for fluoroscopic evaluation; and (3) what was the diagnostic criterion of high- grade SLIL tears that provides the highest accuracy on fluoroscopic evaluation.
Our study had several limitations. First, although the scapholunate gap was wider in the high-grade tear group, the difference was so small that magnification by the fluoroscope was required. The necessity for precise measurement tools and the somewhat complex measurement method therefore may limit the clinical applicability of this method. In addition, we did not measure the normal contralateral wrist. A wide scapholunate gap may be a normal variant, which could have been confirmed by comparison with the contralateral wrist [31]. Third, although we made efforts to exclude chronic, preexisting SLIL tear by history and arthroscopic findings, the differentiation between acute SLIL tear and chronic SLIL tear was unclear so we could not exclude the possibility of including patients with chronic SLIL tear or SLIL laxity in our analysis. To our knowledge, clear definitions of acute SLIL tear, chronic SLIL tear, and SLIL laxity in the setting of distal radius fractures have not been made. Additional studies are required to differentiate these injuries in distal radius fractures. Finally, we assessed only SLIL injuries associated with distal radius fractures, making it unclear whether our results can be applied to other types of SLIL injury.
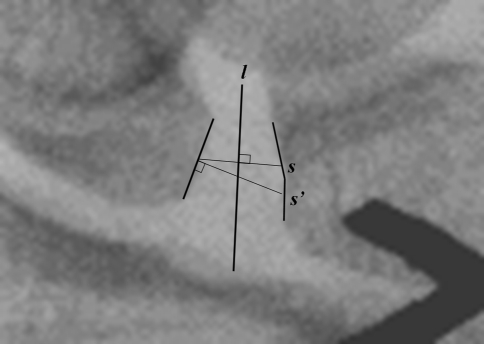
Our data suggest fluoroscopy accurately detects high-grade tears in the SLIL and a 2-mm gap was a suitable cutoff value for diagnosing high-grade tears of this ligament in patients with distal radius fractures. Previous studies have reported the criteria for abnormal widening of the scapholunate joint as varying from 2 mm to 5 mm using plain radiographs [1, 4, 12, 14, 20]. None of these studies described the measurement method in detail. The different criteria and lack of specific measurement methods stem from the anatomic characteristics of the scapholunate joint. First, the scapholunate joint is oriented obliquely, 12.5° to the volar surface of the distal radius [12]. This makes conventional posteroanterior projection of the wrist unable to obtain a perfect profile image of the scapholunate by which true width of the scapholunate joint can be observed. Second, the proximoulnar side of the scaphoid is round, making it difficult to specify a location for reproducible measurements. Third, the two cortices of the scapholunate joint are not always parallel. Fifteen percent of normal adult wrists show an inverted Y-shaped scapholunate joint [26]. When the two cortices are not parallel, the magnitude of the scapholunate gap varies depending on which part of the scapholunate joint was measured, proximal or distal. It also changes according to the method of measurement. In the inverted Y-shaped scapholunate joint, the gap line drawn vertical to the flat ulnar cortex of the scaphoid (Line S′, Fig. 3) is longer than the line drawn by the method used in this study (Line S, Fig. 3). The former method may lead to an inadvertently wider measurement of the scapholunate gap.
Fig. 3.
The magnitude of the measured scapholunate gap differs according to the measurement methods when the two cortices of the scapholunate joint are not parallel. Line S is the line drawn vertical to Line l (the line bisecting the scapholunate joint) from Point A (the point in the middle of the flat surface of the ulnar cortex of the scaphoid). Line S′ is the line drawn vertical to ulnar cortex of scaphoid from Point A. When the scapholunate joint has an inverted Y-shape, like the one in this figure, Line S′ is longer than Line S. When both cortices of the scapholunate joint are parallel, the length of Line S′ is the same as that of Line S.
We made efforts to avoid these biases. For example, a perfect profile image of the scapholunate joint was obtained by fluoroscopic control. Because the middle portion of the scapholunate joint showed the most consistent and narrowest scapholunate gap and the least measurement variance, the gap was measured at the midportion of the flat surface of the ulnar cortex of the scaphoid [26]. A complex method of measurement, which included drawing a line bisecting the scapholunate joint and a scapholunate gap line vertical to it, was devised to make the measurement more consistent regardless of the shape of the joint.
In the high-grade tear group, the scapholunate angle in lateral projection was within the normal range, except for that of one patient with a Grade 4 injury, a finding in agreement with those of other studies (Table 6) [9, 35]. A normal scapholunate angle has been reported in patients with Grade 3 SLIL injury associated with distal radius fractures [9] and in patients with complete tear of the SLIL [35]. In biomechanical studies, a complete tear of the ligament with intact secondary stabilizers of the scapholunate joint did not result in radiographic abnormality such as increased scapholunate angle or widened scapholunate gap [2, 15, 19, 27, 28]. Radiographic abnormality was observed only under a loaded condition [15, 19]. We suspect most of the patients with a high-grade tear of the SLIL associated with distal radius fractures have a partial tear or complete tear of the SLIL with intact secondary stabilizers, so-called predynamic or dynamic instability [32].
Table 6.
Scapholunate angle in patients with high-grade tear of scapholunate interosseous ligament
The scapholunate gap in the high-grade tear group was larger than that in the low-grade tear group and was positively associated with arthroscopic grading of the SLIL injury. The gap difference between groups or grades, however, was less than 1 mm, a magnitude requiring image magnification and precise measurement tools to detect accurately. This may explain why some previous biomechanical studies failed to detect gap widening in wrists with completely torn SLILs if the secondary stabilizers were intact [2, 14, 19]. Other studies, however, have observed gap widening in wrists with partial or complete tears using more precise measurement tools [15, 27].
We found the scapholunate gap was wider with the wrist in ulnar or neutral deviation than in radial deviation in the low-grade and the high-grade tear groups. This was seen in other studies [15, 28]. When assessing the scapholunate joint with a fluoroscope, the degree of SLIL injury may be best evaluated in ulnar or neutral deviation.
The ROC curve of a test with better detectability is always closer to the left and upper border of the graph and area under the curve is wider [17]. Therefore area under the ROC curve is used as an index of diagnostic detectability of a test [17]. The cutoff point at the left upper corner of the ROC curve is where the best tradeoff between sensitivity and specificity occurs. We found the optimal cutoff value was 2 mm.
Our data suggest fluoroscopic examination can accurately diagnose high-grade tears of the SLIL in distal radius fractures.
Acknowledgments
We thank Dr. Hee Chan Ahn for assistance with measurement of fluoroscopic images and data arrangement.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Belsole RJ. Radiography of the wrist. Clin Orthop Relat Res. 1986;202:50–56. [PubMed]
- 2.Blatt G. Capsulodesis in reconstructive hand surgery: dorsal capsulodesis for the unstable scaphoid and volar capsulodesis following excision of the distal ulna. Hand Clin. 1987;3:81–102. [PubMed]
- 3.Braunstein EM, Louis DS, Greene TL, Hankin FM. Fluoroscopic and arthrographic evaluation of carpal instability. AJR Am J Roentgenol. 1985;144:1259–1262. [DOI] [PubMed]
- 4.Cautilli GP, Wehbé MA. Scapho-lunate distance and cortical ring sign. J Hand Surg Am. 1991;16:501–503. [DOI] [PubMed]
- 5.Cole RJ, Bindra RR, Evanoff BA, Gilula LA, Yamaguchi K, Gelberman RH. Radiographic evaluation of osseous displacement following intra-articular fractures of the distal radius: reliability of plain radiography versus computed tomography. J Hand Surg Am. 1997;22:792–800. [DOI] [PubMed]
- 6.Forward DP, Lindau TR, Melsom DS. Intercarpal ligament injuries associated with fractures of the distal part of the radius. J Bone Joint Surg Am. 2007;89:2334–2340. [DOI] [PubMed]
- 7.Frykman G. Fracture of the distal radius including sequelae: shoulder-hand-finger syndrome, disturbance in the distal radio-ulnar joint and impairment of nerve function: a clinical and experimental study. Acta Orthop Scand. 1967;Suppl 108:3+. [DOI] [PubMed]
- 8.Garcia-Elias M, An KN, Amadio PC, Cooney WP, Linscheid RL. Reliability of carpal angle determinations. J Hand Surg Am. 1989;14:1017–1021. [DOI] [PubMed]
- 9.Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357–365. [DOI] [PubMed]
- 10.Gilula LA, Hardy DC, Totty WG, Reinus WR. Fluoroscopic identification of torn intercarpal ligaments after injection of contrast material. AJR Am J Roentgenol. 1987;149:761–764. [DOI] [PubMed]
- 11.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed]
- 12.Kindynis P, Resnick D, Kang HS, Haller J, Sartoris DJ. Demonstration of the scapholunate space with radiography. Radiology. 1990;175:278–280. [DOI] [PubMed]
- 13.Laulan J, Bismuth JP. Intracarpal ligamentous lesions associated with fractures of the distal radius: outcome at one year: a prospective study of 95 cases. Acta Orthop Belg. 1999;65:418–423. [PubMed]
- 14.Linscheid RL, Dobyns JH, Beabout JW, Bryan RS. Traumatic instability of the wrist: diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 1972;54:1612–1632. [PubMed]
- 15.Meade TD, Schneider LH, Cherry K. Radiographic analysis of selective ligament sectioning at the carpal scaphoid: a cadaver study. J Hand Surg Am. 1990;15:855–862. [DOI] [PubMed]
- 16.Mehta JA, Bain GI, Heptinstall RJ. Anatomical reduction of intra-articular fractures of the distal radius: an arthroscopically-assisted approach. J Bone Joint Surg Br. 2000;82:79–86. [DOI] [PubMed]
- 17.Metz CE. Basic principles of ROC analysis. Semin Nucl Med. 1978;8:283–298. [DOI] [PubMed]
- 18.Metz VM, Wunderbaldinger P, Gilula LA. Update on imaging techniques of the wrist and hand. Clin Plast Surg. 1996;23:369–384. [PubMed]
- 19.Mitsuyasu H, Patterson RM, Shah MA, Buford WL, Iwamoto Y, Viegas SF. The role of the dorsal intercarpal ligament in dynamic and static scapholunate instability. J Hand Surg Am. 2004;29:279–288. [DOI] [PubMed]
- 20.Moneim MS. The tangential posteroanterior radiograph to demonstrate scapholunate dissociation. J Bone Joint Surg Am. 1981;63:1324–1326. [PubMed]
- 21.Nielsen PT, Hedeboe J. Posttraumatic scapholunate dissociation detected by wrist cineradiography. J Hand Surg Am. 1984;9:135–138. [DOI] [PubMed]
- 22.O’Meeghan CJ, Stuart W, Mamo V, Stanley JK, Trail IA. The natural history of an untreated isolated scapholunate interosseus ligament injury. J Hand Surg Br. 2003;28:307–310. [DOI] [PubMed]
- 23.Peicha G, Seibert F, Fellinger M, Grechenig W. Midterm results of arthroscopic treatment of scapholunate ligament lesions associated with intra-articular distal radius fractures. Knee Surg Sports Traumatol Arthrosc. 1999;7:327–333. [DOI] [PubMed]
- 24.Protas JM, Jackson WT. Evaluating carpal instabilities with fluoroscopy. AJR Am J Roentgenol. 1980;135:137–140. [DOI] [PubMed]
- 25.Richards RS, Bennett JD, Roth JH, Milne K Jr. Arthroscopic diagnosis of intra-articular soft tissue injuries associated with distal radial fractures. J Hand Surg Am. 1997;22:772–776. [DOI] [PubMed]
- 26.Schimmerl-Metz SM, Metz VM, Totterman SM, Mann FA, Gilula LA. Radiologic measurement of the scapholunate joint: implications of biologic variation in scapholunate joint morphology. J Hand Surg Am. 1999;24:1237–1244. [DOI] [PubMed]
- 27.Short WH, Werner FW, Green JK, Masaoka S. Biomechanical evaluation of ligamentous stabilizers of the scaphoid and lunate. J Hand Surg Am. 2002;27:991–1002. [DOI] [PMC free article] [PubMed]
- 28.Short WH, Werner FW, Green JK, Masaoka S. Biomechanical evaluation of the ligamentous stabilizers of the scaphoid and lunate: Part II. J Hand Surg Am. 2005;30:24–34. [DOI] [PubMed]
- 29.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. [DOI] [PubMed]
- 30.Tang JB, Shi D, Gu YQ, Zhang QG. Can cast immobilization successfully treat scapholunate dissociation associated with distal radius fractures? J Hand Surg Am. 1996;21:583–590. [DOI] [PubMed]
- 31.Vitello W, Gordon DA. Obvious radiographic scapholunate dissociation: X-ray the other wrist. Am J Orthop. 2005;34:347–351. [PubMed]
- 32.Watson H, Ottoni L, Pitts EC, Handal AG. Rotary subluxation of the scaphoid: a spectrum of instability. J Hand Surg Br. 1993;18:62–64. [DOI] [PubMed]
- 33.Watson HK, Ballet FL. The SLAC wrist: scapholunate advanced collapse pattern of degenerative arthritis. J Hand Surg Am. 1984;9:358–365. [DOI] [PubMed]
- 34.Watson HK, Weinzweig J, Zeppieri J. The natural progression of scaphoid instability. Hand Clin. 1997;13:39–49. [PubMed]
- 35.Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am. 1997;22:344–349. [DOI] [PubMed]
- 36.Whipple TL. The role of arthroscopy in the treatment of scapholunate instability. Hand Clin. 1995;11:37–40. [PubMed]
- 37.Wiesler ER, Poehling GG. Arthroscopy of the wrist: operation room setup and technique. In: McGinty J, Burkhart SS, Jackson RW, Johnson DH, Richmond JC, eds. Operative Arthroscopy. 3rd ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2003:729–736.