Abstract
PURPOSE
The purpose of this study is to examine gender differences in associations between body mass index (BMI) and affective disorders.
METHODS
We used logistic regression to examine the effects of BMI and gender on DSM-IV mood and anxiety disorders in a sample of 40,790 adults.
RESULTS
Obesity (BMI ≥ 30.0) was associated with increased risk for any mood disorder, major depressive disorder, and dysthymic disorder, in both men and women (odds ratios [ORs], 1.35–1.88). Risk of bipolar I and II disorders was elevated in obese women (ORs, 1.70–2.41) but not men. Overweight (BMI = 25.0–29.9) predicted increased risk for any mood disorder and bipolar I disorder in women but not men (ORs, 1.16–1.44). Obesity was associated with increased odds of any anxiety disorder and specific phobia in men and women (ORs, 1.35–1.79). Obese women were additionally at increased risk for social phobia. Overweight predicted increased risk of social phobia and specific phobia for women but not men (ORs, 1.27–1.37).
CONCLUSIONS
Obese individuals of both genders are at increased risk for a range of mood and anxiety disorders, but women who are even moderately overweight experience increased risks for some disorders as well.
Keywords: Overweight, Obesity, Mood disorders, Anxiety disorders, Sex/gender, Risk
Introduction
Health risks associated with overweight and obesity are well documented. Diabetes, cardiovascular disease, arthritis, and certain cancers are more prevalent among overweight and obese individuals than among those of normal weight (1–3), and risks for these disorders increase with body mass (2, 4, 5). Recent evidence suggests increased prevalence of mood and anxiety disorders among individuals who are overweight or obese compared to those with weight in the normal range (6). Among those seeking weight loss treatment, rates of depressive and bipolar disorders are elevated (7–9). Conversely, rates of overweight and obesity are elevated among individuals seeking treatment for psychiatric disorders, particularly mood disorders (8, 10–12).
Epidemiological studies are the gold standard for establishing comorbidity rates because they are not confounded by treatment seeking status, and they allow for investigation of demographic variables that may influence relationships. Few epidemiological studies examining the relationship between body mass index (BMI) and psychopathology exist. Most find that the risk of major depression significantly increases with BMI even when controlling for demographic characteristics and other risk factors (6, 13). Obesity also appears to be associated with increased odds of anxiety disorders (6).
Rates of overweight and obesity differ for men and women. Men are more likely to be overweight (14), but women are more likely to be obese (15). In the population as a whole, women are more likely than men to experience mood or anxiety disorders (16). Relationships between psychiatric disorders and BMI also appear to differ for men and women. In an epidemiological sample divided into obese (BMI ≥ 30) and non-obese (BMI < 30) categories, obesity was associated with elevated risk for mood and anxiety disorders in women and men (6). When overweight and obesity are categorized separately, both have been associated with greater likelihood of reporting symptoms of depression or anxiety in women (17, 18), but one study found that these relationships did not hold for men (18), and another found they applied to overweight but not obese men (17). Women but not men who report a lifetime history of major depression or bipolar disorder have elevated odds of obesity (19). Adolescent and young adult females classified as obese are more likely to report anxiety disorders than their normal weight counterparts, a relationship not observed in males (20).
Some recent studies suggest that overweight may actually be associated with better mental health among men. Overweight and obese men are less likely to attempt or commit suicide compared to underweight or normal weight men (21, 22). In contrast, increased BMI is associated with higher rates of suicidal ideation among women (23).
The purpose of this study was to clarify and corroborate findings of previous studies suggesting interactions between BMI and gender in predicting risk for mood and anxiety disorders using a large, recently collected, representative sample of the United States population. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) (24) is the largest psychiatric epidemiology study conducted to date. The National Institute on Alcohol and Alcoholism (NIAAA) collected NESARC data from a representative sample of the U.S. population in 2001 and 2002. The primary goals of NESARC were to determine the prevalence of alcohol use and alcohol use disorders and to examine associated physical and emotional disabilities. Self-reported height and weight were obtained from respondents, and a range of mood and anxiety disorders were diagnosed based on DSM-IV criteria. The NESARC sample therefore appeared to be ideally suited to the task of examining associations between BMI and psychopathology, and the large size of the sample allowed for categorization of respondents into normal weight, overweight, and obese groups and for analysis of interactions between BMI and gender.
Methods
NESARC Sample
Non-institutionalized civilians aged 18 and over were the target population of NESARC, and participants were drawn from all fifty states and the District of Columbia. African American and Hispanic individuals were over-sampled to each constitute approximately 20 percent of the total sample. Young adults, aged 18 to 24, were also over-sampled at a 2.25:1 ratio. The sample was later weighted based on characteristics of the sampling methods, to account for the selection of one person from each household and for over-sampling, and to adjust for non-response at the household level. Weights allow the data to be adjusted during analysis to represent the U.S. population on demographic variables including age, sex, race, ethnicity, and region of residence based on the 2000 Decennial Census results.
Potential NESARC respondents were informed in writing about the nature of the survey, the statistical uses of survey data, the voluntary nature of participation, and Federal laws protecting confidentiality of identifiable survey information. Respondents who consented to participate after receiving this information were interviewed in person by interviewers from the U.S. Census Bureau, who entered responses directly into laptop computers. A total of 43,093 respondents were interviewed, and the response rate was 81%. The research protocol, including informed-consent procedures, received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget.
Assessment of Body Mass Index and DSM-IV Psychiatric Disorders
Body mass index (BMI) was computed from self-reported weight in kilograms divided by self-reported height in meters squared and was available for 41,654 respondents. Respondents were classified into three groups based on established guidelines (25). Those with BMI values of 18.5 to 24.9 were in the normal weight category, respondents with a BMI of 25 to 29.9 were classified as overweight, and respondents with a BMI of 30 or greater were classified as obese. Individuals classified as underweight (BMI < 18.5) were excluded from the current analyses because underweight is associated with other psychopathology already known to increase the risk for mood and anxiety disorders (26, 27), leaving data for 40,790 respondents. Although self-reports of height and weight tend to underestimate BMI somewhat (28), they are highly correlated with direct physical measurement (29).
Lifetime and past-year DSM-IV mood and anxiety disorders were assessed using the NIAAA Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV). Mood disorders evaluated included major depressive disorder, dysthymic disorder, bipolar I disorder, and bipolar II disorder. Individuals with a lifetime diagnosis of bipolar I or bipolar II disorder were not also diagnosed with lifetime major depressive disorder. Individuals with a lifetime diagnosis of major depressive disorder, bipolar I, or bipolar II disorder who experienced an episode of major depression (or manic or hypomanic episode for bipolar I and II disorders respectively) in the past year were considered to have a past-year diagnosis of their lifetime disorder. Anxiety disorders assessed were generalized anxiety disorder, panic disorder without agoraphobia, panic disorder with agoraphobia, agoraphobia without history of panic disorder, social phobia, and specific phobia. The AUDADIS-IV has fair to good reliability and validity for assessing DSM-IV mood and anxiety disorders (24, 30). Mood or anxiety disorders that were substance-induced or due to a general medical condition or bereavement were not included in our analyses.
Statistical Analysis
Respondents were divided into six categories based on BMI and gender (normal weight men, normal weight women, overweight men, overweight women, obese men, and obese women). Chi-square analysis examined omnibus differences among the six groups on categorical variables, and simple regression analysis was used for continuous variables.
Logistic regression examined the relationship of BMI and mood and anxiety disorders within each gender separately, after controlling for demographic characteristics (age, race/ethnicity, education, marital status, income, region of country, and urban vs. rural residence). In addition, separate logistic regression analyses assessed effects of interactions between gender and BMI on mood and anxiety disorders.
All analyses were conducted using SUDAAN (31), a software package that adjusts for complex sampling methodology, including weighting, using Taylor series linearization.
Results
Demographic Characteristics
Table 1 shows demographic characteristics of the sample stratified by BMI category and gender. All demographic features differed significantly across the six categories. Subsequent analyses therefore controlled for all these demographic features.
Table 1.
Demographic characteristics by body mass index (BMI) category and sex
| Normal Weight | Overweight | Obese | Statistic | ||||
|---|---|---|---|---|---|---|---|
| BMI 18.50–24.99 | BMI ≥ 25.00–29.99 | BMI ≥ 30.00 | |||||
| Male | Female | Male | Female | Male | Female | ||
| N | 5957 | 10246 | 7822 | 6784 | 4215 | 5766 | |
| Agea* | 41.99 (0.30) | 44.14 (0.27) | 45.68 (0.27) | 48.21 (0.33) | 45.13 (0.27) | 47.57 (0.30) | F(5, 65) = 75.90, p <.001 |
| Race-ethnicity* | χ2 (20) = 105.10, p<.001 | ||||||
| African American | 9.86 (0.76) | 7.66 (0.76) | 9.15 (0.58) | 13.26 (0.90) | 12.07 (0.87) | 19.52 (1.11) | |
| American Indian | 1.91 (0.26) | 1.92 (0.23) | 1.94 (0.21) | 2.01 (0.26) | 2.64 (0.37) | 2.77 (0.35) | |
| Asian | 7.36 (1.16) | 5.95 (0.74 | 3.43 (0.44) | 3.09 (0.46) | 1.68 (0.34) | 1.76 (0.33) | |
| Hispanic/Latino | 11.67 (1.19) | 9.63 (1.02) | 12.48 (1.37) | 13.28 (1.69) | 12.20 (1.56) | 11.70 (1.36) | |
| White | 69.20 (2.02) | 74.84 (1.63) | 73.01 (1.55) | 68.37 (1.86) | 71.42 (1.73) | 64.24 (1.70) | |
| Education* | χ2 (10) = 97.48, p <.001 | ||||||
| Less than high school | 16.08 (0.67) | 11.97 (0.50) | 14.97 (0.68) | 17.25 (0.92) | 16.64 (0.93) | 20.05 (0.85) | |
| High school graduate | 27.40 (0.88) | 27.65 (0.73) | 28.16 (0.90) | 30.25 (0.74) | 31.41 (0.93) | 33.41 (0.85) | |
| Some college or higher | 56.51 (1.05) | 60.38 (0.81) | 56.87 (0.94) | 52.50 (0.96) | 51.95 (1.10) | 46.54 (0.95) | |
| Marital status* | χ2 (15) = 196.42, p <.001 | ||||||
| Married/living with partner | 54.48 (0.84) | 58.95 (0.74) | 69.80 (0.62) | 62.00 (0.83) | 70.58 (0.97) | 56.90 (0.82) | |
| Widowed | 2.80 (0.25) | 9.20 (0.32) | 2.52 (0.17) | 11.31 (0.43) | 1.55 (0.18) | 11.22 (0.47) | |
| Divorced/separated | 8.88 (0.38) | 11.48 (0.37) | 9.59 (0.36) | 12.16 (0.44) | 9.87 (0.48) | 14.74 (0.51) | |
| Single (never married) | 33.84 (0.90) | 20.36 (0.68) | 18.09 (0.57) | 14.53 (0.63) | 18.01 (0.86) | 17.13 (0.59) | |
| Income* | χ2 (15) = 168.13, p <.001 | ||||||
| $10,000 per year or less | 9.53 (0.46) | 11.41 (0.45) | 5.85 (0.35) | 11.13 (0.49) | 5.79 (0.44) | 12.82 (0.57) | |
| $10,001–$25,000 | 20.40 (0.74) | 20.13 (0.55) | 17.21 (0.59) | 24.65 (0.65) | 17.24 (0.75) | 25.71 (0.70) | |
| $25,000–$50,000 | 31.90 (0.84) | 28.39 (0.63) | 31.75 (0.73) | 30.29 (0.61) | 33.27 (1.01) | 32.66 (0.83) | |
| Over $50,000 | 38.18 (1.08) | 40.06 (1.02) | 45.18 (0.99) | 33.93 (0.98) | 43.69 (1.25) | 28.81 (0.91) | |
| Region of country* | χ2 (15) = 29.66, p <.050 | ||||||
| Northeast | 18.79 (3.71) | 20.20 (3.61) | 21.03 (3.47) | 20.34 (3.58) | 17.90 (2.84) | 18.11 (3.06) | |
| Midwest | 22.10 (3.30) | 22.58 (3.39) | 22.95 (3.13) | 22.47 (3.24) | 25.67 (3.13) | 24.65 (3.24) | |
| South | 34.22 (3.47) | 33.92 (3.43) | 34.53 (3.26) | 35.96 (3.38) | 36.73 (3.10) | 37.37 (3.15) | |
| West | 24.89 (4.18) | 23.30 (3.76) | 31.49 (3.42) | 21.24 (3.62) | 19.70 (3.10) | 19.86 (3.18) | |
| Urban vs. Rural* | χ2 (5) = 35.20, p <.001 | ||||||
| Urban | 82.54 (1.65) | 81.74 (1.62) | 80.00 (1.67) | 80.04 (1.75) | 76.66 (1.82) | 78.20 (1.77) | |
| Rural | 17.46 (1.65) | 18.26 (1.62) | 20.00 (1.67) | 19.96 (1.75) | 23.34 (1.82) | 21.80 (1.77) | |
Values represent percentages (unless otherwise noted) and numbers in parentheses are standard errors.
Values represent means.
Indicates significant group differences.
Prevalence of DSM-IV Mood and Anxiety Disorders
Figure 1 and Figure 2 depict lifetime and past-year prevalence of mood and anxiety disorders, adjusted to reflect population demographics, for each gender in the three BMI categories. Women, particularly obese women, tended to have higher rates of mood disorders, both over the lifetime and in the year preceding the interview, than men. Prevalence of anxiety disorders was associated with BMI in both genders, but overall, women had greater increases in prevalence rates with increasing BMI compared to men.
Figure 1. Prevalence of lifetime and past-year mood disorders by BMI and gender.
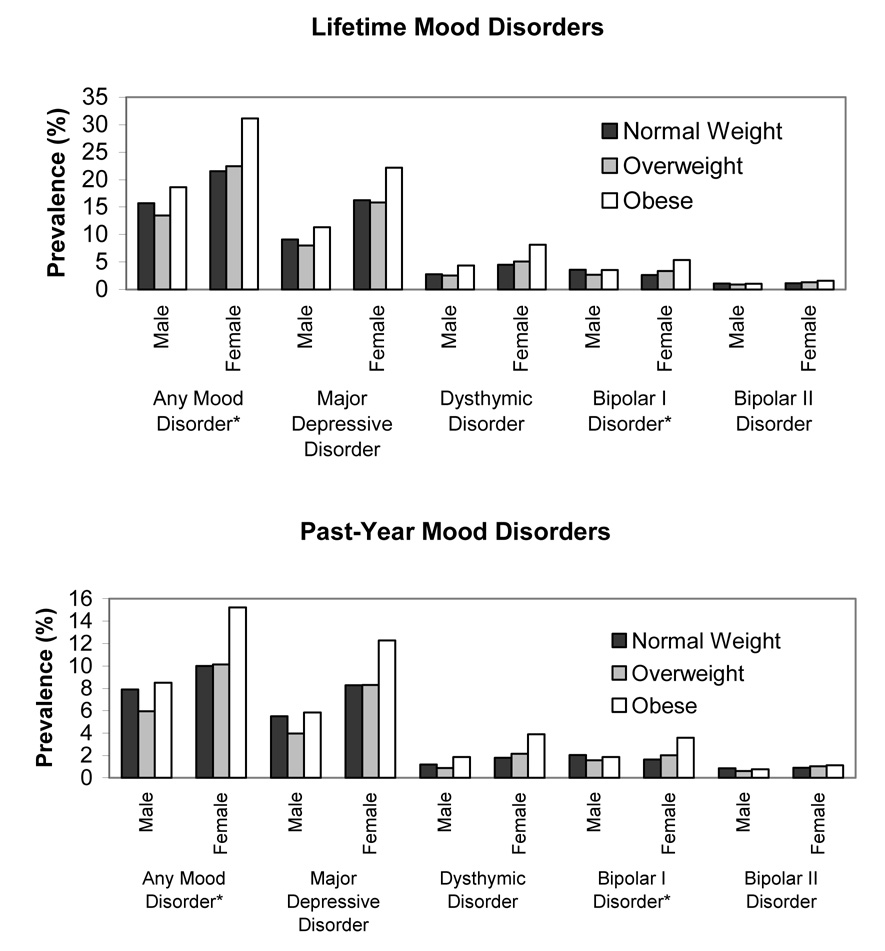
*Indicates a significant effect of the interaction between gender and BMI.
Figure 2. Prevalence of lifetime and past-year anxiety disorders by BMI and gender.
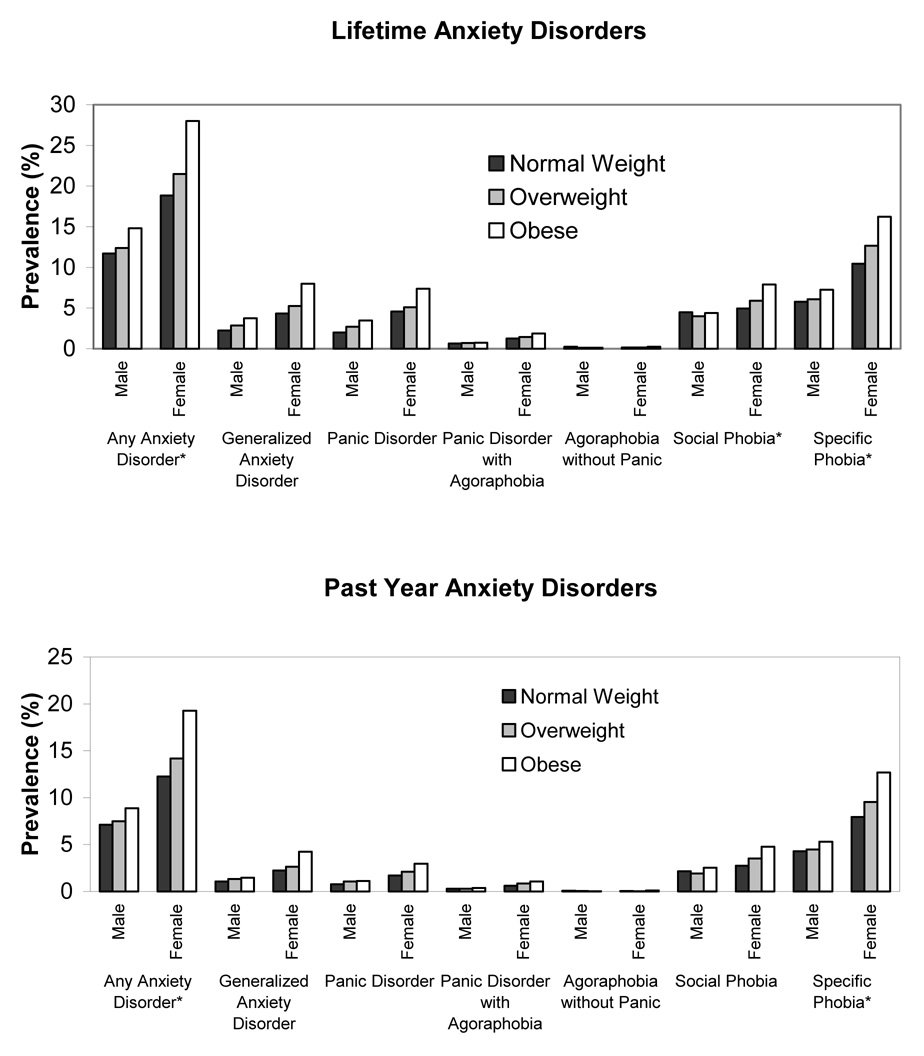
*Indicates a significant effect of the interaction between gender and BMI.
Relationships Between DSM-IV Mood Disorders and BMI by Gender
Table 2 shows odds ratios (OR) and 95% confidence intervals (CI) resulting from the logistic regression analyses with mood disorders as the dependent variables. Controlling for demographic characteristics, the analyses indicated a significant gender by BMI interaction effect on the likelihood of any lifetime or past-year mood disorder. Overweight and obese women had a greater likelihood of any lifetime mood disorder than normal weight women, while only obese but not overweight men had increased odds of any lifetime mood disorder compared to normal weight men. The odds of any past-year mood disorder were significantly elevated for both men and women in the obese category compared to their normal weight counterparts. This interaction was also significant in that the OR was higher for obese women than for obese men. Obese women and men were more likely to have lifetime and past-year major depressive disorder and dysthymic disorder compared to their normal weight counterparts. Overweight and obese women had increased odds of lifetime and past-year bipolar I disorder; there was no significant relationship between BMI and bipolar I disorder in men. The interaction between BMI and gender was significant for lifetime and past-year bipolar I disorder. Risk of lifetime bipolar II disorder was elevated for obese women. No other significant associations between BMI category and bipolar II disorder were observed, and there was no significant BMI by gender interaction effect.
Table 2.
Odds ratios (ORs) of DSM-IV mood disorders by body mass index (BMI) category for males and females
| Male | Male Only | Female | Female Only | Interaction | |||
|---|---|---|---|---|---|---|---|
| Overweight | Obese | F (df=2) | Overweight | Obese | F (df=2) | F (df=2) | |
| BMI=25.00–29.99 | BMI ≥ 30.00 | BMI=25.00–29.99 | BMI ≥ 30.00 | ||||
| Any mood disorder | |||||||
| Lifetime, OR | 0.94 | 1.39 | 18.15, p<.001 | 1.16 | 1.79 | 77.23, p <.001 | 6.47, p <.005 |
| (95% C.I.) | (0.83–1.07) | (1.21–1.60)* | (1.05–1.28)* | (1.63–1.97)* | |||
| Past Year, OR | 0.90 | 1.33 | 9.56, p <.001 | 1.13 | 1.75 | 36.17, p <.001 | 3.62, p <.050 |
| (95% C.I.) | (0.76–1.07) | (1.10–1.59)* | (0.98–1.31) | (1.52–2.01)* | |||
| Major depressive disorder | |||||||
| Lifetime, OR | 0.91 | 1.35 | 11.86, p <.001 | 1.04 | 1.58 | 43.93, p <.001 | 1.83, p =.168 |
| (95% C.I.) | (0.78–1.07) | (1.14–1.59)* | (0.93–1.17) | (1.43–1.75)* | |||
| Past Year, OR | 0.85 | 1.31 | 7.34, p =.001 | 1.02 | 1.49 | 13.07, p <.001 | 0.85, p =.430 |
| (95% C.I.) | (0.68–1.06) | (1.03–1.67)* | (0.85–1.22) | (1.25–1.76)* | |||
| Dysthymic disorder | |||||||
| Lifetime, OR | 1.02 | 1.77 | 11.51, p <.001 | 1.17 | 1.88 | 31.76, p <.001 | 0.70, p =.500 |
| (95% C.I.) | (0.79–1.31) | (1.35–2.34)* | (0.98–1.40) | (1.60–2.20)* | |||
| Past Year, OR | 0.87 | 1.85 | 7.05, p <.005 | 1.22 | 2.10 | 18.32, p <.001 | 1.31, p =.276 |
| (95% C.I.) | (0.59–1.29) | (1.24–2.76)* | (0.90–1.65) | (1.62–2.73)* | |||
| Bipolar I disorder | |||||||
| Lifetime, OR | 0.91 | 1.20 | 2.21, p =.118 | 1.44 | 2.24 | 28.24, p <.001 | 8.75, p <.001 |
| (95% C.I.) | (0.71–1.17) | (0.93–1.55) | (1.11–1.86)* | (1.80–2.78)* | |||
| Past Year, OR | 0.97 | 1.15 | 0.55, p =.578 | 1.41 | 2.41 | 16.47, p <.001 | 6.16, p <.005 |
| (95% C.I.) | (0.70–1.30) | (0.80–1.64) | (1.04–1.82)* | (1.84–3.17)* | |||
| Bipolar II disorder | |||||||
| Lifetime, OR | 1.10 | 1.46 | 2.74, p =.072 | 1.44 | 1.70 | 4.98, p <.010 | 0.65, p =.527 |
| (95% C.I.) | (0.71–1.70) | (1.06–2.01) | (1.00–2.08)* | (1.20–2.39)* | |||
| Past Year, OR | 1.03 | 1.34 | 0.61, p =.548 | 1.48 | 1.56 | 2.71, p =.074 | 0.75, p =.477 |
| (95% C.I.) | (0.61–1.74) | (0.76–2.35) | (0.97–2.26) | (1.03–2.37) | |||
Wald F values report effect of BMI on likelihood of mood disorder within sex and the interaction of BMI and sex on likelihood of mood disorder. Odds ratios (ORs) obtained using normal weight as reference group. Normal weight and male gender are comparators for interactions. Analyses control for age, level of education, race/ethnicity, income, marital status, region of country, and urban vs. rural residence.
Indicates that Wald F is significant, and OR is significantly different from 1.00 within that gender.
Relationships Between DSM-IV Anxiety Disorders and BMI by Gender
Table 3 shows ORs and 95% CIs resulting from the logistic regression analyses with anxiety disorders as the dependent variables. After controlling for demographic characteristics, significant interaction effects between gender and BMI category were observed for any lifetime and past-year anxiety disorder, for lifetime social phobia, and for lifetime and past-year specific phobia.
Table 3.
Odds ratios (ORs) of DSM-IV anxiety disorders by body mass index (BMI) category for males and females
| Male | Male Only | Female | Female Only | Interaction | |||
|---|---|---|---|---|---|---|---|
| Overweight | Obese | F (df=2) | Overweight | Obese | F (df=2) | F (df=2) | |
| BMI=25.00–29.99 | BMI ≥ 30.00 | BMI=25.00–29.99 | BMI ≥ 30.00 | ||||
| Any anxiety disorder | |||||||
| Lifetime, OR | 1.10 | 1.35 | 10.57, p<.001 | 1.24 | 1.76 | 56.41, p <.001 | 6.23, p <.005 |
| (95% C.I.) | (0.96–1.25) | (1.18–1.53)* | (1.12–1.38)* | (1.58–1.96)* | |||
| Past Year, OR | 1.14 | 1.36 | 7.06, p <.005 | 1.26 | 1.79 | 42.17, p <.001 | 4.02, p <.050 |
| (95% C.I.) | (0.99–1.33) | (1.16–1.61)* | (1.11–1.43)* | (1.58–2.03)* | |||
| Generalized anxiety disorder | |||||||
| Lifetime, OR | 1.35 | 1.77 | 6.88, p <.005 | 1.29 | 2.00 | 30.04, p <.001 | 0.51, p =.604 |
| (95% C.I.) | (1.02–1.80)* | (1.30–2.40)* | (1.08–1.54)* | (1.67–2.39)* | |||
| Past Year, OR | 1.44 | 1.53 | 2.31, p =.107 | 1.27 | 2.02 | 13.40, p <.001 | 1.20, p =.309 |
| (95% C.I.) | (0.96–2.16) | (1.00–2.34) | (0.97–1.67) | (1.53–2.65)* | |||
| Panic disorder without agoraphobia | |||||||
| Lifetime, OR | 1.37 | 1.81 | 6.69, p <.005 | 1.17 | 1.72 | 17.66, p <.001 | 0.76, p =.474 |
| (95% C.I.) | (1.06–1.78)* | (1.30–2.50)* | (0.95–1.44) | (1.42–2.07)* | |||
| Past Year, OR | 1.54 | 1.64 | 2.42, p =.097 | 1.35 | 1.84 | 7.65, p =.001 | 0.60, p =.552 |
| (95% C.I.) | (1.01–2.34) | (0.96–2.79) | (1.00–1.81) | (1.35–2.52)* | |||
| Panic disorder with agoraphobia | |||||||
| Lifetime, OR | 1.28 | 1.30 | 0.49, p =.614 | 1.18 | 1.52 | 2.89, p =.063 | 0.36, p =.700 |
| (95% C.I.) | (0.75–2.19) | (0.70–2.42) | (0.86–1.63) | (1.07–2.16) | |||
| Past Year, OR | 1.21 | 1.69 | 0.81, p =.450 | 1.51 | 1.84 | 3.26, p <.050 | 0.27, p =.761 |
| (95% C.I.) | (0.61–2.42) | (0.74–3.84) | (0.95–2.39) | (1.12–3.01)* | |||
| Agoraphobia without panic disorder | |||||||
| Lifetime, OR | 0.48 | 0.55 | 0.85, p =.431 | 1.03 | 1.51 | 0.54, p =.585 | 0.90, p =.412 |
| (95% C.I.) | (0.15–1.55) | (0.14–2.20) | (0.38–2.79) | (0.65–3.53) | |||
| Past Year, OR | 0.57 | 0.47 | 0.28, p =.753 | 0.58 | 1.47 | 1.08, p <.345 | 0.50, p =.612 |
| (95% C.I.) | (0.09–3.65) | (0.05–4.69) | (0.10–3.33) | (0.36–5.96) | |||
| Social phobia | |||||||
| Lifetime, OR | 0.93 | 1.02 | 0.33, p =.723 | 1.27 | 1.70 | 16.12, p <.001 | 6.64, p <.005 |
| (95% C.I.) | (0.73–1.19) | (0.80–1.30) | (1.07–1.52)* | (1.41–2.06)* | |||
| Past Year, OR | 0.98 | 1.28 | 1.83, p =.169 | 1.37 | 1.81 | 12.11, p <.001 | 2.37, p =.101 |
| (95% C.I.) | (0.72–1.33) | (0.92–1.78) | (1.05–1.77)* | (1.42–2.30)* | |||
| Specific phobia | |||||||
| Lifetime, OR | 1.12 | 1.33 | 5.71, p <.010 | 1.30 | 1.74 | 38.33, p <.001 | 4.43, p <.050 |
| (95% C.I.) | (0.94–1.32) | (1.12–1.59)* | (1.16–1.47)* | (1.53–1.97)* | |||
| Past Year, OR | 1.12 | 1.32 | 3.39, p <.050 | 1.29 | 1.76 | 30.96, p <.001 | 3.21, p <.050 |
| (95% C.I.) | (0.92–1.35) | (1.07–1.64)* | (1.12–1.49)* | (1.53–2.03)* | |||
Wald F values report effect of BMI on likelihood of mood disorder within sex and the interaction of BMI and sex on likelihood of mood disorder. Odds ratios (ORs) obtained using normal weight as reference group. Normal weight and male gender are comparators for interactions. Analyses control for age, level of education, race/ethnicity, income, marital status, region of country, and urban vs. rural residence.
Indicates that Wald F is significant, and OR is significantly different from 1.00 within that gender.
Among women, both overweight and obesity were associated with greater likelihood of any lifetime or past-year anxiety disorder, but only obesity was associated with greater odds of any lifetime or past-year anxiety disorder among men. The likelihood of lifetime and past-year social phobia was also elevated for overweight and obese women relative to normal weight women with increasing odds for these anxiety disorders as BMI increased. There was no significant increase in the odds of social phobia with increasing BMI among men. Odds of lifetime and past-year specific phobia were higher in overweight and obese women, and in obese but not overweight men, relative to those in the normal weight category.
Odds of lifetime generalized anxiety disorder increased with BMI in both men and women. Panic disorder without agoraphobia was associated with overweight in men and obesity in both genders; the interaction between BMI and gender was not significant. Panic disorder with agoraphobia and agoraphobia without panic disorder were not associated with BMI in either gender.
Discussion
This study found that obesity was associated with many DSM-IV mood and anxiety disorders in both genders and that gender interacted with BMI to increase risk of certain disorders. Women who were either overweight or obese had increased odds of any lifetime mood disorder and of lifetime and past-year bipolar II disorder, whereas overweight men were not at elevated risk for any lifetime or past-year mood disorder. Similar interactions between gender and BMI were noted to affect the risk for anxiety disorders, with overweight women more often evidencing anxiety disorders, especially social and specific phobias, than their normal weight counterparts. For obese persons of either gender, odds of almost all mood and anxiety disorders were elevated.
Being overweight or obese could contribute to depression or anxiety, and could do so differently in men and women. For example, weight-related stigma and discrimination are more severe for women than for men (32, 33). Women who are overweight, even moderately so, are more likely to be dissatisfied with their weight and to experience social disadvantages compared to normal weight women (34, 35). Forty-four percent of men in the NESARC sample were overweight, and only 33% were in the normal weight category, making overweight the “normal” condition for men. In contrast, 30% of women were overweight, and 57% were of normal weight. Overweight may thus be more deviant for women than men. The specific finding that overweight and obese women, but not men, are at increased risk for social phobia is consistent with these observations. Overweight and obese women may fear social situations more than their male counterparts because they anticipate being negatively evaluated based on weight, more so than men.
Conversely, mood and anxiety disorders could lead to weight gain. Women are more likely than men to eat in response to negative emotions (36), a coping strategy that could contribute to weight gain. Atypical depression, a condition more frequently observed in women (37, 38) is associated with increased appetite, increased sleep (which could reduce activity levels) and weight gain (39). An episode of major depression may thus be more likely to contribute to weight gain in women compared to men. Although NESARC did not include a specific diagnostic category of atypical depression, the specific symptoms of increased appetite and increased sleep were assessed. Among respondents with a diagnosis of any lifetime mood disorder, women were more likely than men to endorse increased appetite (34% vs. 23%, χ2(1)=96.50, p<.001) and increased sleep (47% vs. 42%, χ2(1)=21.03, p<.001). Although overweight women were not at significantly increased risk for major depressive disorder than normal weight women, their likelihood of experiencing a lifetime episode of major depression was increased (OR [CI] = 1.12 [1.01–1.24]). Among NESARC respondents meeting DSM-IV criteria for bipolar I disorder, men were more likely to report only manic episodes; 74.15% of women and 56.7% of men had experienced an episode of major depression. It therefore appears that elevated risk for bipolar I disorder in overweight women could be driven largely by their higher rates of depressive episodes‥
Another plausible connection between mood and anxiety disorders and weight gain may be use of psychoactive medications, including selective serotonin reuptake inhibitors, lithium, and atypical antipsychotics and anticonvulsants, that are frequently associated with weight gain (40–43). Although NESARC respondents were asked if a doctor had ever prescribed medication for symptoms of each mood and anxiety disorder assessed, specific medications were not recorded, and respondents were not asked to provide a time frame for or duration of medication use. Medication use could have contributed to the observed associations, but this database does not allow for accurate assessment of relationships between medication use and weight gain.
The results of this study replicate findings from smaller studies showing gender differences in relationships between BMI and mood and anxiety disorders. Some limitations of this study should be noted. The design is cross-sectional, precluding determination of the direction of causality between elevated BMI and psychiatric disorders. Further research exploring the casual pathways between the observed relationships is needed.
A second limitation is use of self-reported height and weight to calculate BMI, which may result in underestimates (28, 44, 45). However, the proportions of respondents in each category were consistent with those observed in an epidemiological sample from the same year using objective measurements (46), so any potential underestimation appears to have been equally distributed across BMI and gender categories. The fact that all NESARC interviews were conducted in person rather than by telephone as has been done in some epidemiological studies (17, 19) may have enhanced the accuracy of self-reports.
Finally, other psychiatric conditions that could have impacted the observed relationships were not evaluated. For instance, eating disorders were not assessed by NESARC, and binge eating disorder, which is slightly more prevalent in women (47), could have contributed to both weight gain and mood and anxiety symptoms (48). Psychotic disorders were not formally evaluated in NESARC, but only a small proportion of respondents in the entire sample (<1%) endorsed a history of a psychotic disorder, with similar rates in men and women (χ2(1)=.32, p=.57), so unreported use of antipsychotic medications associated with weight gain is unlikely to have influenced our results significantly.
The greatest strength of this study is its use of a large epidemiologic sample carefully evaluated and diagnosed using DSM-IV criteria for mood and anxiety disorders. The sample was randomly selected, the response rate was high, and groups traditionally underrepresented in studies of physical and mental health risk factors were over-sampled to ensure adequate representation. The size of the sample also allowed for examination of separate overweight and obese BMI categories, facilitating identification of gender-based risk patterns that might not have emerged had broader categories (e.g., obese vs. not obese or overweight vs. normal weight) been used.
In summary, results of this study indicate that overweight and obesity are associated with mood and anxiety disorders, and the association emerges at the level of overweight for women, while associations between psychiatric conditions usually do not emerge until the level of obesity for men. Targeting obese individuals and overweight women for mood and anxiety disorder screening could aid in identifying and treating these conditions. Since pharmacological treatments for mood and anxiety disorders are often associated with weight gain, special treatment considerations may be indicated in this population already subject to increased weight-related health risks.
Among individuals seeking weight loss treatment, many are likely to meet criteria for current or lifetime mood or anxiety disorders, but few have sought psychiatric treatment (49). This study’s findings highlight the need to consider the effect of mood and anxiety disorders when designing weight loss interventions. Overweight and obese individuals may carry psychological burdens that interfere with their ability to adhere to diet and exercise programs, and understanding the relationship between mood and anxiety disorders and elevated BMI may be crucial to improving these health interventions.
Acknowledgments
Preparation of this report was supported in part by NIH grants R01-MH60417, R01-MH60417-Supp, R01-DA13444, R01-DA018883, R01-DA14618, R01-DA016855, P50-AA03510, and P50-DA09241. We thank NIAAA and the U.S. Census Bureau field representatives who administered the NESARC interview.
ABBREVIATIONS
- BMI
Body Mass Index
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders, 4th Edition
- NESARC
National Epidemiologic Survey on Alcohol and Related Conditions
- OR
Odds Ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Brown CD, Higgins M, Donato KA, Rohde FC, Garrison R, Obarzanek E, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605–619. doi: 10.1038/oby.2000.79. [DOI] [PubMed] [Google Scholar]
- 2.McTigue K, Larson JC, Valoski A, Burke G, Kotchen J, Lewis CE, et al. Mortality and cardiac and vascular outcomes in extremely obese women. J Am Med Assoc. 2006;296:79–86. doi: 10.1001/jama.296.1.79. [DOI] [PubMed] [Google Scholar]
- 3.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with overweight and obesity. J Am Med Assoc. 1999;282:1523–1529. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Graubard BI, DF W, Gail MH. Excess deaths associated with underweight, overweight, and obesity. J Am Med Assoc. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 5.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. J Am Med Assoc. 2003;289:187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 6.Simon GE, Von Korff M, Saunders K, Miglioretti DL, Crane PK, van Belle G, et al. Association between obesity and psychiatric disorders in the US adult population. Arch Gen Psychiatry. 2006;63:824–830. doi: 10.1001/archpsyc.63.7.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alciati A, D'Ambrosio A, Foschi D, Corsi F, Mellado C, Angst J. Bipolar spectrum disorders in severely obese patients seeking surgical treatment. J Affect Disord. 2007;101:131–138. doi: 10.1016/j.jad.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 8.McElroy SL, Kotwal R, Malhorta S, Nelson EB, Keck PE, Nemeroff CB. Are mood disorders and obesity related? A review for the mental health professional. J Clin Psychiatry. 2004;65:634–651. doi: 10.4088/jcp.v65n0507. [DOI] [PubMed] [Google Scholar]
- 9.Wadden TA, Butryn ML, Sarwer DB, Fabricatore AN, Crerand CE, Lipschutz PE, et al. Comparison of psychosocial status in treatment-seeking women with class III vs. class I–II obesity. Surg Obes Relat Dis. 2006;2:138–145. doi: 10.1016/j.soard.2006.03.016. [DOI] [PubMed] [Google Scholar]
- 10.Jones LE, Carney CP. Increased risk for metabolic syndrome in persons seeking care for mental disorders. Ann Clin Psychiatry. 2006;18:149–155. doi: 10.1080/10401230600801085. [DOI] [PubMed] [Google Scholar]
- 11.Kloiber S, Ising M, Reppermund S, Horstmann S, Dose T, Majer M, et al. Overweight and obesity affect treatment response in major depression. Biol Psychiatry. 2007;62:321–326. doi: 10.1016/j.biopsych.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 12.Fagiolini A, Frank E, Scott JA, Turkin S, Kupfer DJ. Metabolic syndrome in bipolar disorder: findings from the Bipolar Disorder Center for Pennsylvanians. Bipolar Disord. 2005;7:424–430. doi: 10.1111/j.1399-5618.2005.00234.x. [DOI] [PubMed] [Google Scholar]
- 13.Onyike CU, Crum RM, Lee HB, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 14.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegel KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. J Am Med Assoc. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 15.Poulose BK, Holzman MD, Zhu Y, Smalley W, Richards WO, Wright JK, et al. National variations in morbid obesity and bariatric surgery use. J Am Coll Surg. 2005;201:77–84. doi: 10.1016/j.jamcollsurg.2005.03.022. [DOI] [PubMed] [Google Scholar]
- 16.Wiessman MM, Bland R, Joyce PR, Newman S, Wells JE, Wittche H-U. Sex differences in rates of depression: Cross-national perspectives. J Affect Disord. 1993;29:77–84. doi: 10.1016/0165-0327(93)90025-f. [DOI] [PubMed] [Google Scholar]
- 17.Heo M, Pietrobelli A, Fontaine KR, Sirey JA, Faith MS. Depressive mood and obesity in US adults: Comparison and moderation by sex, age, race. Int J Obes. 2006;30:513–519. doi: 10.1038/sj.ijo.0803122. [DOI] [PubMed] [Google Scholar]
- 18.Jorm AF, Korten AE, Christensen H, Jacomb PA, Rodgers B, Parslow RA. Association of obesity with anxiety, depression, and emotional well-being: A community survey. Aust N Z J Public Health. 2003;27:434–440. doi: 10.1111/j.1467-842x.2003.tb00423.x. [DOI] [PubMed] [Google Scholar]
- 19.McIntyre RS, Konarksi JZ, Wilkins K, Socyznska JK, Kennedy SH. Obesity in bipolar disorder and major depressive disorder: Results from a national community health survey on mental health and well-being. Can J Psychiatry. 2006;51:274–280. doi: 10.1177/070674370605100502. [DOI] [PubMed] [Google Scholar]
- 20.Lamertz CM, Jacobi C, Yassouridis A, Arnold K, Henkel AW. Are obese adolescents and young adults at higher risk for mental disorders? A community survey. Obes Res. 2002;10:1152–1160. doi: 10.1038/oby.2002.156. [DOI] [PubMed] [Google Scholar]
- 21.Magnusson PKE, Rasmussen F, Lawlor DA, Tynelius P, Gunnell D. Association of body mass index with suicide mortality: A prospective cohort study of more than one million men. Am J Epidemiol. 2006;163:1–8. doi: 10.1093/aje/kwj002. [DOI] [PubMed] [Google Scholar]
- 22.Mukamal KJ, Kawachi I, Miller M, Rimm EB. Body mass index and risk of suicide among men. Arch Intern Med. 2007;167:468–475. doi: 10.1001/archinte.167.5.468. [DOI] [PubMed] [Google Scholar]
- 23.Carpenter K, Hasin D, Allison D, Faith M. Relationship between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: Results from a general population study. Am J Public Health. 2000;90:251–257. doi: 10.2105/ajph.90.2.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grant BF, Moore TC, Kaplan K. Bethesda, MD: Natl Inst Alcohol Abuse Alcohol; Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) 2003
- 25.National Heart, Lung, Blood Institute in cooperation with the National Institute of Diabetes and Digestive and Kidney. Washington, DC: Natl Inst Health; Diseases.: Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. 1998
- 26.Bulik CM, Sullivan PF, Tozzi F, Furberg H, Lichtenstein P, Pedersen NL. Prevalence, heritability, and prospective risk factors for anorexia nervosa. Arch Gen Psychiatry. 2006;63:305–312. doi: 10.1001/archpsyc.63.3.305. [DOI] [PubMed] [Google Scholar]
- 27.Wade TD, Bulik CM, Neale M, Kendler KS. Anorexia nervosa and major depression: Shared genetic and environmental risk factors. Am J Psychiatry. 2000;157:469–471. doi: 10.1176/appi.ajp.157.3.469. [DOI] [PubMed] [Google Scholar]
- 28.Roberts RJ. Can self-reported data accurately describe the prevalence of overweight? Public Health. 1995;109:275–284. doi: 10.1016/s0033-3506(95)80205-3. [DOI] [PubMed] [Google Scholar]
- 29.Cash TF, Counts B, Hangen J, Huffine CE. How much do you weigh? Determinant of validity of self-reported body weight. Percept Mot Skills. 1989;69:248–250. [Google Scholar]
- 30.Grant BF, Hasin DS. Rockville, MD: Natl Inst Alcohol Abuse Alcohol; The Alcohol Use Disorders and Associated Disabilities Interview Schedule. 1991
- 31.Institute RT: Software for Survey Data Analysis (SUDAAN) Version 8.1. Research Triangle Park, NC: Research Triangle Institute; 2003. [Google Scholar]
- 32.Chen EY, Brown M. Obesity stigma in sexual relationships. Obes Res. 2005;13:1393–1397. doi: 10.1038/oby.2005.168. [DOI] [PubMed] [Google Scholar]
- 33.Maranto CL, Stenoien AF. Weight discrimination: A multidisciplinary analysis. Empl Respons Rights J. 2000;12:9–24. [Google Scholar]
- 34.Gortmacker SL, Must A, Perrin JM, Sobol AM, Dietz WH. Social and economic consequences of overweight in adolescence and young adulthood. N Engl J Med. 1993;30:1008–1012. doi: 10.1056/NEJM199309303291406. [DOI] [PubMed] [Google Scholar]
- 35.Pingitore R, Spring B, Garfield D. Gender differences in body satisfaction. Obes Res. 1997;5:402–409. doi: 10.1002/j.1550-8528.1997.tb00662.x. [DOI] [PubMed] [Google Scholar]
- 36.Larsen JK, Strien T, Eisinga R, Engels RCME. Gender differences in the association between alexithymia and emotional eating in obese individuals. J Psychosom Res. 2006;60:237–243. doi: 10.1016/j.jpsychores.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 37.Frank E, Carpenter LL, Kupfer DJ. Sex differences in recurrent depression: Are there any that are significant? Am J Psychiatry. 1988;145:41–45. doi: 10.1176/ajp.145.1.41. [DOI] [PubMed] [Google Scholar]
- 38.Young MA, Scheftner WA, Fawcett J, Klerman GL. Gender differences in the clinical features of unipolar depressive disorder. J Nerv Ment Dis. 1990;178:200–203. doi: 10.1097/00005053-199003000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Hasler G, Pine DS, Gamma A, Milos G, Ajdacic V, Eich D, et al. The associations between psychopathology and being overweight: A 20-year prospective study. Psychol Med. 2004;34:1047–1057. doi: 10.1017/s0033291703001697. [DOI] [PubMed] [Google Scholar]
- 40.Taylor V, MacQueen G. Associations between bipolar disorder and metabolic syndrome: A review. J Clin Psychiatry. 2006;67:1034–1041. doi: 10.4088/jcp.v67n0704. [DOI] [PubMed] [Google Scholar]
- 41.Aronne LJ, Segal KR. Weight gain in the treatment of mood disorders. J Clin Psychiatry. 2003;64:22–29. [PubMed] [Google Scholar]
- 42.Dannon PN, Iancu I, Cohen A, Lowengrub K, Grunhaus L, Kotler M. Three year naturalistic outcome study of panic disorder patients treated with paroxetine. BMC Psychiatry. 2004;4:1–6. doi: 10.1186/1471-244X-4-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Keck PE, McElroy SL. Bipolar disorder, obesity, and pharmacotherapy-associated weight gain. J Clin Psychiatry. 2003;64:1426–1435. doi: 10.4088/jcp.v64n1205. [DOI] [PubMed] [Google Scholar]
- 44.Flood V, Webb K, Lazarus R, Pang G. Use of self-report to monitor overweight and obesity in populations: some issues for consideration. Aust N Z J Public Health. 2000;24:96–99. doi: 10.1111/j.1467-842x.2000.tb00733.x. [DOI] [PubMed] [Google Scholar]
- 45.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 46.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 47.Smith DE, Marcus MD, Lewis CE, Fitzgibbon M, Schreiner P. Prevalence of binge eating disorder, obesity, and depression in a biracial cohort of young adults. Ann Behav Med. 1998;20:227–232. doi: 10.1007/BF02884965. [DOI] [PubMed] [Google Scholar]
- 48.Linde JA, Jeffery RW, Levy RL, Sherwood NE, Utter J, Pronk NP, et al. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. Int J Eat Disord. 2004;28:418–425. doi: 10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- 49.Ravaldi C, Barboni E, Lai M, Rotella CM, Vannacci A, Ricca V. Obesity and mood disorders: The complex problem of insight. J Clin Psychiatry. 2005;66:265. doi: 10.4088/jcp.v66n0217a. [DOI] [PubMed] [Google Scholar]


