Abstract
Purpose
To identify factors that impact asthma morbidity in rural school-aged children.
Design
Exploratory analysis of baseline data collected in a longitudinal intervention study.
Setting
Four rural school districts that served small towns and unincorporated areas..
Sample
Children in grades 2 to 5 who had current asthma and who spoke English or Spanish. There were 183 children (108 boys, 75 girls) with an average age of 8.78, and who were Hispanic (46%), White (31%), or African American (22%).
Methods
Associations between asthma risk factors (gender, ethnicity/race, socioeconomic status [SES], asthma severity), asthma resources (access to care, health insurance), family asthma management, and asthma morbidity (absenteeism, emergency department [ED] visits, hospitalizations) were analyzed.
Findings
Children with more severe asthma had higher absenteeism, more hospitalizations, and their parents performed more asthma management behaviors. Families who had difficulty accessing care had more hospitalizations and ED visits, and were more likely to be poor. More boys, more Hispanic and African American children, and more children from poorer families were hospitalized for asthma than were middle-class and non-Hispanic White children.
Conclusions
Asthma is a chronic condition that is fairly easy for some families to manage, while other families are having higher asthma morbidity that needs to be addressed through targeted interventions.
Keywords: Asthma, children, rural
Asthma is the most common chronic illness of childhood with more than 4 million children (6%) under 18 years having current asthma.1 Asthma is characterized by a pattern of episodic bronchial hyperresponsiveness (BHR) that is reversible with medication intervention.2 The pathophysiological basis of asthma is chronic airway inflammation that causes mucosal swelling, subsequent narrowing of the airway as edema accumulates, and increased irritability of the bronchial smooth muscles.3,4 The seasonal and highly individualized pattern of BHR is mainly attributed to allergenic provocateurs, yet many persons with asthma have symptoms in the absence of allergens. In fact, viral infections (e.g. colds, flu) are the most common cause of asthma exacerbations in school-aged children.5 In addition vigorous physical activity, strong smells, and air pollution are common intrinsic triggers of asthma exacerbations.6
Asthma in Rural Areas
There are conflicting findings regarding the impact of living in rural areas on childhood asthma. In some studies comparing urban dwellers with rural dwellers, rural dwellers were found to have lower asthma prevalence,7,8 fewer days with asthma symptoms,7 and fewer allergic triggers.8 In contrast, Ernest and Cormier found that 5% of rural children in Canada who lived in farm environments had asthma, while rural children who did not live in farm environments had a much higher asthma prevalence rate at 9%.9 The rural environment has a rich mixture of allergens from seasonal crops, abundant wildflower and weed growth, dust and animal dander in barns and silos, air pollution (e.g., ozone, methane gas from manure), and noxious odors from landfills which are frequently located in rural areas.9-12 Nevertheless, asthma remains a major health concern for children who live in rural areas. The purpose of the present study was to identify factors that impacted asthma morbidity in rural school-aged children.
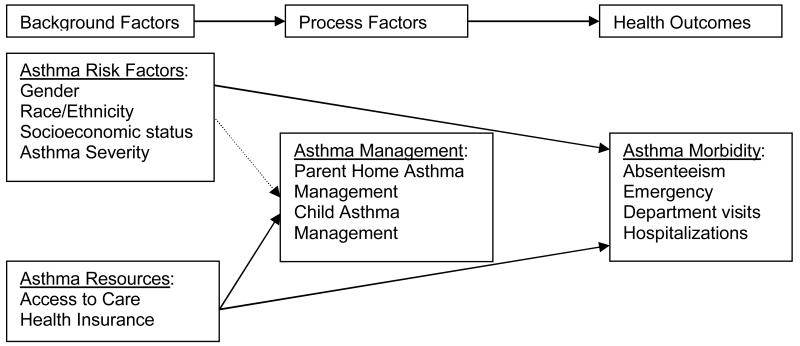
Asthma Health Model
Asthma morbidity is reflected in days ill with asthma and health care utilization including hospitalization and emergency department (ED) visits. Bruhn's theoretical model of asthma management posits that background, process, and outcome factors constantly interact to influence asthma management.13 The author adapted the model to guide assessment of factors that influence parents' and children's asthma management and test the effectiveness of the intervention in improving asthma management and health outcomes. Because clinical nurse specialists (CNS) work with families with various backgrounds and differing degrees of resources the CNS needs to consider the impact of these factors on children's asthma morbidity and to individualize care accordingly.
Background Factors
Background factors include asthma risk factors and family resources. Asthma risk factors have the potential to increase health disparities experienced by rural dwellers. Asthma risk factors include the child's gender, race/ethnicity, socioeconomic status [SES], and asthma severity that can complicate the management of asthma. Childhood asthma affects more boys than girls (1.57:1), more ethnic minorities than Whites, and more poor than middle-class children.1,14,15 Asthma severity is probably the most important factor influencing the daily work of managing asthma. Asthma severity describes the child's clinical condition in terms of both the underlying disease state and the current level of symptom control.16 Asthma severity is determined by symptom frequency, airflow reduction, activity limitations, and medications (type and quantity) needed to improve or control symptoms.17 The National Asthma Education and Prevention Program developed guidelines for asthma management that are titrated according to the child's asthma severity.3,17
Asthma resources include health insurance that covers the child, medications, and access to care. Access to care is integral to initiating self-management behaviors. Access to care includes the availability of health care providers, affordability, a perception of the appropriateness of the care provided, and the belief that the provider makes a genuine effort to understand the family's concerns.18 There are fewer health care providers in rural areas and so families must travel some distance to obtain care.19 More rural Americans work in low-benefit jobs that do not provide insurance or sick care benefits than do urban Americans and health insurance is a critical factor in “timely access to health care.”20,p19, 21 Rural families tend to delay seeking health care when symptoms first arise and as the health condition worsens, they will then seek care at urban urgent care centers.22 Health care visits for both preventive care and chronic illness management are negatively impacted by lack of health insurance and reduced access to care.19
Process Factors
The process of family asthma management includes preventive and treatment strategies. Preventive activities focus on environmental management to control asthma triggers and use of preventive medications to lessen BHR.3,23 While medication therapy is integral to good asthma management, it causes great parental concern regarding side effects and fears of over-treating episodes.24
Early treatment of asthma symptoms is encouraged to limit the severity and duration of asthma episodes.3,17 Allergens are a primary trigger for asthma episodes. In studies comparing rural and urban populations, rural children were less likely to be sensitive to domestic pet dander (e.g., cats, dogs) but were more sensitive to farm animals (e.g., horse, cow, pig, storage mites) than were urban children.9 The rural environment can pose significant health risks for children with asthma including pesticide spraying of crops, waste/dump sites located in rural rather than urban areas, bacterial endotoxins from farm animals, and air pollution (ozone, indoor carbon monoxide, methane gases).10,11
Health Outcomes
While many health outcomes are of concern to families and health care providers, asthma morbidity was the focus in this study. Asthma morbidity includes school absenteeism, hospitalizations and emergency department (ED) visits for asthma. Asthma morbidity carries a heavy price tag in terms of health care expenditures, use of health care resources, disruptions in family routines, loss of wages, loss of learning time, and even death.25,26 Children with asthma miss an average of 7.6 school days annually, in comparison to healthy peers who miss 2.5 days.26 However, even when attending school, children with asthma symptoms are easily fatigued and have poor concentration, which can impair learning.27 To summarize, living in a rural environment contributes to the potential for increased asthma episodes due to agricultural processes (e.g. pollinating crops, spraying of pesticides, harvesting crops),9,12 the distance to and the lack of health care providers,19 and the low-benefits occupations that are common among rural dwellers.20
Methods
This is an exploratory analysis of the baseline data collected in a longitudinal intervention study. The research questions guiding this study were:
What are the associations between asthma management, asthma risk factors (child's asthma severity, race/ethnicity, gender, and family SES), asthma resources (access to care, health insurance), and asthma morbidity (school absenteeism, ED visits, and hospitalizations)?
Are there significant differences between asthma risk factors for ED visits, hospitalizations, and absenteeism?
Which factors (asthma management, asthma risk factors, asthma resources) significantly predict health care utilization (ED visits, hospitalizations)?
Sample
Four rural school districts participated in this study. These school districts served small towns (e.g. populations 380 – 1,200) and the surrounding areas. Sample criteria include (a) children in grades 2 to 5 who had a diagnosis of asthma, (b) who had experienced asthma in the past 12 months (current asthma), and (c) who spoke English or Spanish. Children were excluded if they had a co-morbidity that would impair their participation in an educational intervention.
There were 183 children in this sample; 108 boys and 75 girls with a mean age of 8.78 years (s.d. = 1.24). The sample was predominately tri-ethnic with 46% Hispanic, 31% White, 22% African American. The mothers' mean age was 36.58 years (s.d. = 9.37). The mothers' education levels ranged from less than high school (7 - 11 years: 15.6%), to high school graduates (42%), and post-high school education (42.4%).
Procedures
The study was approved by the Institutional Review Board of a large southwestern university. School personnel who worked in the school nurse offices reviewed medical history records of children in grades 2 to 5 to identify those children with a medical diagnosis of asthma. Letters were mailed to their parents to invite their participation in this study about asthma management. Response postcards were enclosed with the letters so that parents who were interested in hearing more about the study could grant permission to the school personnel to give the families' names, telephone numbers, and addresses to the researchers. This screening process ensured that confidentiality of school records was maintained.
Informed consent
A meeting was scheduled at a time and place convenient to the family, usually in their homes, during which the study purpose and procedures were explained, and questions were answered. Parents signed consent forms and children signed assent forms indicating their agreement to participate in the study.
Data collection
Data for this study were collected after the informed consent and assents were completed. One parent and their child who had asthma completed their own survey booklet. The survey booklet directions and items were read to the children. Parents completed their booklets independently, except in the instance of a blind parent for whom a graduate research assistant read the items.
Instruments
Parents completed a demographic page that included the child's age, gender, ethnicity and race, grade in school, health insurance, and parents' marital status, educational levels, and occupations. The parents' education and occupation data were used to derive the family SES variable using the Hollingshead Four-Factor Index.28
Asthma history
Parents completed an asthma history questionnaire that was developed for this study based on a review of literature and clinical asthma guidelines.3 The history questions included asthma medications, asthma triggers, asthma morbidity (i.e., ED visits and hospitalizations for asthma) in the past year, and health insurance.
School absenteeism
School attendance (i.e., days enrolled in school) and absences were obtained with parent permission from the child's school records. This data was transformed by dividing the days absent by days enrolled and multiplying by 100 to obtain an absenteeism rate.
Asthma severity
Asthma severity describes the child's clinical condition in terms of current level of asthma control. Severity of Chronic Asthma (SCA) is a 3-item scale that corresponds to clinical guidelines for determining asthma severity and yields a continuous score.3 Parents are asked to reflect on the past month and rate how frequently their child had asthma symptoms every week, how often the child's activity was limited every week, and how often their sleep was disturbed by asthma in the past month using a 4-point ordinal scale that ranges from “0-2 times a week” to “daily.” The SCA was tested in a sample of 94 school age children who had asthma and adequate to good item-to-total correlations (0.64 – 0.81) were found.16
Access to care
Access to care is a multidimensional construct that includes a range of factors that affect whether families can reach and make use of health care resources. Parents answered the 9-item Parent Barriers to Managing Asthma scale by rating how difficult each factor was in their efforts to obtain care for their child. A 10th item was added to the scale for this rural population and asked the parent how hard it was to travel a distance for care. The 5-point response format ranged from 1 for “not hard at all” to 5 for “extremely hard.” Internal consistency (α =.79) of the scale is good.18
Family asthma management
Family asthma management involves parents' work to manage their child's asthma and the child's self-management work. Parents' asthma management was assessed by the parent's responses to the 16-item Management Behavior Survey.29 Items are scored on a 5-point scale from 1 for “never” to 5 for “always.” The tool was designed to measure asthma symptom prevention and treatment activities performed by parents for their child's asthma. Internal consistency (α =.82) was good.34 Children's asthma self-management was assessed by the child's responses to the 17-item Asthma Behavior Inventory.30 Items are scored on a 5-point scale from 1 for “never” to 5 for “always.” The tool measures children's self-reported asthma treatment and preventive behaviors. Internal consistency (α = .71) was adequate with a school-age sample.30
Data Analysis
Data were entered into an SPSS file and assessed for missing data. Frequencies of demographic data and study variables were run. For the first research question (RQ1), associations among the variables were assessed by running Pearson's product moment correlation for the continuous variables and running point-biserial correlation procedures when one of the variables was dichotomous.31 For RQ2, ANOVA and chi-square were run to identify differences in asthma morbidity by the asthma risk factors. Finally for RQ3, logistical regression was run to identify what factors predicted hospitalization and ED visits for asthma. The asthma management and access to care scales are all reported as means of the summed scale items.
Results
Descriptive statistics are listed in Table 1 with means and standard deviations for continuous variables and frequencies with percentages for nominal or qualitative variables. School absenteeism was high at 4.8% or an average of 7.1 school days. In addition, 28% of the participants had visited the ED for an acute asthma episode in the previous 12 months and 13% had also had a hospitalization for asthma. It is noteworthy that 11% of this community-based sample had no health insurance.
Table 1. Descriptive statistics.
| Variable/Instrument | Mean (SD) | N | (%) |
|---|---|---|---|
| Asthma Risk Factors | |||
|
|
|||
| Asthma Severity | 4.17 (1.49) | ||
| Socioeconomic Status | 33.72 (12.05) | ||
| Boys (%) | 108 | (59%) | |
| Girls (%) | 75 | (41%) | |
| Hispanic | 84 | (46%) | |
| African American | 41 | (22%) | |
| Non-Hispanic White | 56 | (31%) | |
| Asthma Resource | |||
|
|
|||
| Access to Care | 1.43 (.54) | ||
| Health insurance (no) | 20 | (11%) | |
| Family Asthma Management | |||
|
|
|||
| Parent | 2.64 (.78) | ||
| Child | 2.9 (.58) | ||
| Asthma Morbidity | |||
|
|
|||
| School Absenteeism (%) | 4.8 (4.42) | ||
| Hospitalizations (yes) | 24 | (13%) | |
| ED Visits (yes) | 52 | (28%) |
Associations between the asthma management, asthma risk factors, asthma resources, and asthma morbidity are reported in Table 2. The correlations are weak among the factors but most are in the expected direction. For example, asthma severity is significantly associated with parent asthma management, absenteeism, and hospitalization, but not with ED visits. Children with more severe asthma had higher absenteeism, more hospitalizations, and their parents performed more asthma management behaviors. Access to care had significant associations with hospitalization and ED visits, and was inversely associated with SES. Such that when access to care was rated poorly (higher score), the children had more hospitalizations and ED visits, and were more likely to be from poorer (lower SES scores) families.
Table 2. Correlations among study variables.
| Variables | AS | SES | G | R/E | AC | Ins | PM | CM | Abs | H | ED |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Asthma Risk Factors and Resources | |||||||||||
|
|
|||||||||||
| Asthma Severity (AS) | 1.0 | ||||||||||
| Socioeconomic Status (SES) | -.13 | 1.0 | |||||||||
| Gender (G) | .07 | -.15 | 1.0 | ||||||||
| Race/Ethnicity (R/E) | .16* | -.46** | .12 | 1.0 | |||||||
| Access to Care (AC) | -.01 | -.15* | .05 | .10 | 1.0 | ||||||
| Health Insurance (Ins)§ | -.10 | -.15* | -.08 | -.20** | -.09 | 1.0 | |||||
| Asthma Management | |||||||||||
|
|
|||||||||||
| Parent (PM) | .25** | -.11 | .15 | .23** | -.06 | -.19* | 1.0 | ||||
| Child (CM) | .06 | -.01 | -.12 | .08 | -.09 | -.09 | -.15 | 1.0 | |||
| Asthma Morbidity | |||||||||||
|
|
|||||||||||
| School Absenteeism (Abs) | .30** | -.17* | .19* | .08 | -.03 | -.08 | .25** | -.09 | 1.0 | ||
| Hospitalizations (H)§ | .22** | -.19** | .19** | .18* | .20** | -.17* | .10 | .18* | .06 | 1.0 | |
| Emergency Department Visits (ED)§ | .12 | -.15 | .01 | .12 | .23** | -.05 | .00 | .16* | .13 | .55** | 1.0 |
= p < .05.
= p < .01.
= dichotomous variables for which point-biserial correlation were run.
Parents' and children's asthma management, while not statistically significant, were inversely associated. It is interesting to note that while parents' asthma management was significantly associated with absenteeism, it was not associated with ED visits or hospitalizations. In contrast, the children's asthma management was not significantly associated with absenteeism but it was significantly associated with both hospitalization and ED visits.
The results of ANOVA and chi-square procedures run to examine differences in asthma morbidity (hospitalization, ED visits, absenteeism) by asthma risk factors are reported in Table 3. There were no differences in terms of gender, race or ethnic group, or asthma severity between those children who visited the ED for asthma care and those who did not visit the ED. However, significantly more children from poorer families were seen in the ED for asthma care than were children from middle class families. In contrast, there were significant differences by gender, race or ethnic group, and SES group among those children who were hospitalized for asthma. Specifically more boys (18.5%) than girls (5%), more Hispanic (17.9%) and African American (17%) than non-Hispanic White (3.6%) children, and more children from poorer (22%) than middle-class (6.4%) families were hospitalized for asthma. Children with persistent asthma had higher absenteeism than did those children with mild intermittent asthma (5.79% versus 3.56%). In addition, boys had higher absenteeism than did girls (5.45% versus 3.77%, respectively).
Table 3. Asthma Risk Factors and Children's Asthma Morbidity.
| Absenteeism | Hospitalizations | Emergency Department Visits | |||||||
|---|---|---|---|---|---|---|---|---|---|
| F | df | p | X2 | df | p | X2 | df | p | |
| Asthma Severity | 10.41 | (1,155) | .002 | 2.39 | (1) | .12 | .82 | (1) | .37 |
| SES (poor/middle class) | 2.27 | (1/148) | .13 | 9.45 | (1) | .002 | 5.98 | (1) | .014 |
| Gender | 5.50 | (1,155) | .02 | 6.75 | (1) | .009 | .01 | (1) | .92 |
| Race/Ethnicity | .93 | (2,152) | .40 | 6.63 | (2) | .036 | 4.70 | (2) | .10 |
Notes: F = F statistic (ANOVA), X2 = chi square statistic, df = degrees of freedom, p = significance
Finally, logistical regression were run to determine if asthma risk factors, resources, or asthma management predicted which children would be visit the ED or be hospitalized for asthma. Only a few of the variables were found to significantly predict or differentiate between children who were hospitalized for asthma and those who were not hospitalized. Specifically, boys and uninsured children were more likely to be hospitalized. In addition, having visited the ED for asthma was the strongest predictor for subsequent hospitalizations for asthma. In contrast, the only variable that significantly predicted that a child would visit the ED for asthma was having previously been hospitalized for asthma.
Implications
Consistent with other studies, the children in this study had high levels of absenteeism with boys and children who had persistent asthma symptoms having higher levels of absenteeism. In turn, the parents' asthma management activities were increased in the presence of increasing absenteeism. Since school-aged children cannot be left at home unattended, parents either miss work to stay home and care for the child or they must arrange alternate child care with a family member, trusted neighbor, or babysitter. High absenteeism can be a burden on families. First, there is the loss of income experienced in many families who work in jobs that do not have sick leave benefits – a common occurrence among rural dwellers.20 However, even when the parents work in jobs with benefits, some parents of children who have high absenteeism have expended all available compensatory benefits (i.e., sick leave, vacation time). Second, all families have additional out-of-pocket expenses related to health care visits, loss of income, and incidental asthma management. Based on 2004 dollars the estimated cost for asthma was $16.1 billion of which $4.6 billion were accounted for as indirect costs covered by families.32 Finally, there is the underlying worry about whether or not the child needs to be seen by a health care provider.25,26 This last point is a significant one for rural families because of the distance they need to travel to reach a provider and in poorer families the need to arrange for transportation to take the child to a provider.22
In terms of health care utilization, national surveys indicate that among 5- to 14-year old children who have current asthma, 8.1% were seen in the ED for asthma care in the previous 12 months and 2% were hospitalized for asthma.33 In the present study of rural children who have current asthma, 28% were seen in the ED for asthma care and 13% were hospitalized for asthma in the previous 12 months. The only risk factor found to contribute to ED visits was SES: More children from poorer families (38%) visited the ED for asthma care than did middle class children (21%). While this finding is consistent with other studies that have found higher utilization of ED services for health care among poor families, it may also be a reflection of the lack of local acute care services in rural areas.14,20 When faced with an asthma exacerbation, families who already have fewer resources may be choosing to travel to the closest full-service source of care as a ‘preemptive strike’ in case the exacerbation is difficult to resolve.34
The children who were hospitalized for asthma were more likely to be male, poor, or a member of an ethnic minority group. The coupling of ethnic minority status and lower SES and increased health care utilization is found in most studies of childhood asthma.15,34 While many studies report more males are hospitalized than females, this is not a consistent finding.34,35 The factors that were found to predict hospitalization in this study were being male, lacking health insurance, and being seen in the ED for asthma care. The finding that 11% of these families had no health insurance may have compounded the high rates of health care utilization. The lack of health insurance in a group that has a chronic health problem is a serious issue because this affects both acute care and preventive or primary care management of asthma. Many families who do not have health insurance need assistance in working through the complicated paperwork for obtaining coverage. In the present study, the research team provided these families with packets of information about the Children's Health Insurance Program and telephone numbers to agencies that assist families in the process.
These findings can lend support to the CNS who wants to develop and initiate an asthma management program. In this study, the children who had been hospitalized or seen in the ED for asthma reported performing more asthma self-management. This finding may reflect the learning or increased awareness that can occur in these direct care encounters. Exploratory analyses like those reported here can serve as the impetus for developing asthma self-management education that takes advantage of learning opportunities in brief patient encounters. The efficacy and effectiveness of such educational interventions need to be tested.
While it is not clear what aspects about being male contributed to increased risk for hospitalization among the boys in this sample, this finding may highlight the need for individualized education to address child- and family-needs. There is nothing in the literature about gender-based differences in asthma management, but parents will talk about the greater difficulty in managing asthma in boys when compared with girls. It is possible that this may reflect biases or assumptions about boys, but it may also be possible that different strategies are needed to facilitate asthma management in boys when compared with girls. The increased hospitalization in this sample, points out a need for research to determine what factors contribute to this increased hospitalization and develop interventions for addressing the modifiable factors.
The findings presented here are limited by the volunteer nature of the sample. It is possible that families who were more concerned about children's asthma were more likely to participate in study designed to improve children's asthma self-management. Generalizability of findings is limited to rural school districts similar to those that participated in this study.
Conclusion
Asthma is a chronic condition with variable onset and duration in the face of a variety of provocateurs. However, these symptomatic episodes can be reduced or controlled with the use of preventive medications, environmental controls, and prompt treatment of exacerbations.3,17 While asthma is fairly easy for some families to manage, other families are having higher asthma morbidity that needs to be addressed through targeted interventions. The CNS can conduct studies like the one presented here to determine what factors contribute to high asthma morbidity in their community. The results can be used as the basis for developing interventions or programs to meet the needs of their at-risk families.
Figure 1.
Asthma Health Model
Table 4. Logistical Regression of Predictors of Hospitalization and Emergency Department (ED) Visits for Asthma.
| β | SE | Wald | df | p | |
|---|---|---|---|---|---|
| Hospitalization for Asthma | |||||
|
|
|||||
| Constant | .17 | .39 | .19 | 1 | - |
| ED Visits | -4.36 | .89 | 24.26 | 1 | <.001 |
| Gender | -2.01 | .74 | 7.31 | 1 | .007 |
| Health insurance | 1.95 | .98 | 3.98 | 1 | .046 |
| ED Visits for Asthma | |||||
|
|
|||||
| Constant | 2.30 | .74 | 9.64 | 1 | .002 |
|
| |||||
| Hospitalization | -3.84 | .77 | 24.82 | 1 | <.001 |
Notes: β = , SE = , df = degrees of freedom, p = significance,
References
- 1.Bloom B, Dey AN. Summary Health Statistics for U.S. Children: National Health Interview Survey, 2004. National Center for Health Statistics. Vital Health Stat. 2006;10(227) [PubMed] [Google Scholar]
- 2.Silverman M. Introduction. In: Silverman M, editor. Childhood asthma and other wheezing disorders. 2nd. London: Arnold; 2002. pp. 1–6. [Google Scholar]
- 3.Pediatric asthma: Promoting best practice, guide for managing asthma in children. Milwaukee, WI: American Academy of Allergy Asthma & Immunology; 2004. pp. 8–10. [Google Scholar]
- 4.Janson S. National asthma education and prevention program, expert panel report II: Overview and application to primary care. Lippincott's Primary Care Practitioner. 1998;2:578–588. [PubMed] [Google Scholar]
- 5.Friedlander SL, Busse WW. The role of rhinovirus in asthma exacerbations. J Allergy Clin Immunol. 2005;116:267–273. doi: 10.1016/j.jaci.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Charpin D, Ramadour M, Lanteaume A, Vervloet D. Triggers in instrinsic asthma in the EGEA study. J Asthma. 2003;40:87–91. doi: 10.1081/jas-120017211. [DOI] [PubMed] [Google Scholar]
- 7.Iversen L, Hannaford PC, Price DB, Godden DJ. Is living in a rural area good for your respiratory health? Results from a cross-sectional study in Scotland. Chest. 2005;128:2059–2067. doi: 10.1378/chest.128.4.2059. [DOI] [PubMed] [Google Scholar]
- 8.Riedler J, Eder W, Oberfeld G, Schreuer M. Australian children living on a farm have less hay fever, asthma and allergenic sensitization. Clin Exp Allergy. 2000;30:194–200. doi: 10.1046/j.1365-2222.2000.00799.x. [DOI] [PubMed] [Google Scholar]
- 9.Ernst P, Cormier Y. Relative scarcity of asthma and atopy among rural adolescents raised on a farm. Am J Respir Crit Care Med. 2000;161:1563–1566. doi: 10.1164/ajrccm.161.5.9908119. [DOI] [PubMed] [Google Scholar]
- 10.Flores G, Fuentes-Afflick E, Barbot O, et al. The health of Latino children: Urgent priorities, unanswered questions, and a research agenda. JAMA. 2002;288:82–90. doi: 10.1001/jama.288.1.82. [DOI] [PubMed] [Google Scholar]
- 11.Resto M, Huss K, Winkelstein M, et al. Asthma education in rural communities. Clin Excell Nurse Pract. 2001;5:168–174. doi: 10.1054/xc.2001.23124. [DOI] [PubMed] [Google Scholar]
- 12.Yawn B. Asthma and the rural environment. Rural Clinician Q. 2001;11(3):1. [Google Scholar]
- 13.Bruhn JG. The application of theory in childhood asthma self-help programs. J Allergy Clin Immunol. 1983;72:561–577. doi: 10.1016/0091-6749(83)90483-9. [DOI] [PubMed] [Google Scholar]
- 14.Amre DK, Infante-Rivard C, Gautrin D, Malo JL. Socioeconomic status and utilization of health care services among asthmatic children. J Asthma. 2002;39:625–631. doi: 10.1081/jas-120014927. [DOI] [PubMed] [Google Scholar]
- 15.Higgins PS, Wakefield D, Cloutier MM. Risk factors for asthma and asthma severity in nonurban children in Connecticut. Chest. 2005;128:3846–3853. doi: 10.1378/chest.128.6.3846. [DOI] [PubMed] [Google Scholar]
- 16.Horner SD, Kieckhefer GM, Fouladi RT. Measuring Asthma Severity: Instrument Refinement. J Asthma. 2006;43:533–538. doi: 10.1080/02770900600857192. [DOI] [PubMed] [Google Scholar]
- 17.U.S. Department of Health and Human Services. National Asthma Education and Prevention Program, Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. NIH Publication no. 07-4051. 2007. [Google Scholar]
- 18.Bursch B, Schwankovsky L, Gilbert J, Zeiger R. Construction and validation of four childhood asthma self-management scales: Parent barriers, child and parent self-efficacy, and parent belief in treatment efficacy. J Asthma. 1999;36:115–128. doi: 10.3109/02770909909065155. [DOI] [PubMed] [Google Scholar]
- 19.Crago S, Coors L, Lapidus JA, et al. Prehospital treatment of acute asthma in a rural state. Ann Allergy Asthma Immunol. 1998;81:322–325. doi: 10.1016/S1081-1206(10)63123-7. [DOI] [PubMed] [Google Scholar]
- 20.Bolin J, Gamm L. Access to quality health services in rural areas – insurance. In: Gamm LD, Hutchison LL, Dabney BJ, Dorsey AM, editors. Rural Healthy People 2010: A companion document to Healthy People 2010. Vol. 1. College Station, Texas: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. pp. 19–24. [Google Scholar]
- 21.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: The compounding effects of race/ethnicity and rurality on health. Am J Public Health. 2004;94:1695–1703. doi: 10.2105/ajph.94.10.1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Horner SD, Ambrogne-Smith J, Coleman MA, et al. Traveling for care: Factors influencing health care access for rural dwellers. Public Health Nurs. 1994;11:145–149. doi: 10.1111/j.1525-1446.1994.tb00393.x. [DOI] [PubMed] [Google Scholar]
- 23.Platts-Mills TAE, Vaughan JW, Carter MC, Woodfolk JA. The role of intervention in established allergy: Avoidance of indoor allergens in the treatment of chronic allergic disease. J Allergy Clin Immunol. 2000;106:787–804. doi: 10.1067/mai.2000.110548. [DOI] [PubMed] [Google Scholar]
- 24.DePaola LM, Roberts MC, Blaiss MS, Frick PJ, McNeal RE. Mothers' and children's perceptions of asthma medication. Children's Health Care. 1997;26:265–283. [Google Scholar]
- 25.Mannino DM, Homa DM, Akinbami LJ, Moorman MS, Gwynn C, Redd SC. Surveillance for asthma: United States, 1980-1999. MMWR. 2002;51(SS01):1–13. [PubMed] [Google Scholar]
- 26.Hanson JE, Lapidus J, Zuniga J, Murphy S. Childhood asthma in low-income Hispanic and non-Hispanic White families in a rural state: The impact-on-family scale. Children's Health Care. 2000;29:65–67. [Google Scholar]
- 27.Welch MJ, Kemp JP, Meltzer EO, Orgel HA, Ostrom NK. Asthma in the schools. Immunol Allergy Clin N Am. 1991;11:173–181. [Google Scholar]
- 28.Hollingshead AB. Four factor index of social status. New Haven, CT: Yale; 1975. [Google Scholar]
- 29.Mesters I, Meertens R, Crebolder H, Parcel G. Development of a health education program for parents of preschool children with asthma. Health Educ Res. 1993;8:53–68. doi: 10.1093/her/8.1.53. [DOI] [PubMed] [Google Scholar]
- 30.Kieckhefer GM. Testing self-perception of health theory to predict health promotion and illness management behavior in children with asthma. J Pediatr Nurs. 1987;2:381–391. [PubMed] [Google Scholar]
- 31.Field A. Discovering statistics using SPSS. 2nd. London: Sage; 2005. [Google Scholar]
- 32.American Lung Association. Trends in asthma morbidity and mortality. 2005. [Google Scholar]
- 33.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma – United States, 1980-2004. MMWR. 2007;56(SS08):1–60. [PubMed] [Google Scholar]
- 34.Stignone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006;97:244–250. doi: 10.1016/S1081-1206(10)60021-X. [DOI] [PubMed] [Google Scholar]
- 35.Wallace JC, Denk CE, Kruse LK. Pediatric hospitalizations for asthma: Use of a linked file to separate person-level risk and readmission. Prev Chronic Dis. 2004 [serial online] April (cited 1/18/08) [PMC free article] [PubMed] [Google Scholar]