Abstract
Background. Laparoscopic cholecystectomy is the present treatment of choice for patients with gallbladder stones, despite its being associated with a higher incidence of biliary injuries compared with the open procedure. Injuries occurring during the laparoscopic approach seem to be more complex. A complex biliary injury is a disease that is difficult to diagnose and treat. We considered complex injuries: 1) injuries that involve the confluence; 2) injuries in which repair attempts have failed; 3) any bile duct injury associated with a vascular injury; 4) or any biliary injury in association with portal hypertension or secondary biliary cirrhosis. The present review is an evaluation of our experience in the treatment of these complex biliary injuries and an analysis of the international literature on the management of patients.
Keywords: Associated biliary lesions, complex bile duct injuries, liver transplantation for bile duct injuries
Introduction
At present, laparoscopic cholecystectomy is the treatment of choice for patients with gallbladder stones, although this approach has always been associated with a higher incidence of biliary injuries compared with the open procedure. In the 1990s, the incidence ranged between 0.3% and 1.3%, and at present it has stabilized at around 0.6% 1,2,3. Injuries occurring when the laparoscopic approach has been taken seem to be more complex than those occurring during the open procedure, owing to the more proximal location of the injury in the biliary tree, its frequent association with a vascular injury, and the thermal mechanism usually involved 4,5. Besides, a high percentage of these injuries coexist with biliary fistula, and this conditions the small caliber of the bile duct 6,7,8. This obscure picture can worsen if the surgeon performing the operation does not take the correct decision once the bile duct injury has occurred.
Most bile duct injuries are complex for the non-specialized HPB surgeon 9 (Table I), i.e. surgeons who are specialized in HPB surgery obtain better results in the treatment of this pathology than those who are not. This situation can be avoided if HPB specialists first treat the patient using a multidisciplinary approach, i.e. a collaboration of surgeons, interventional radiologists, and endoscopists 10.
Table I. Bile duct injuries.
|
A complex biliary injury is a disease that is difficult to diagnose and treat. Our aim is therefore to analyze the management of complex bile duct injuries.
Management and treatment
Inadequate management of complex bile duct injuries may result in complications such as biliary peritonitis, leading to systemic sepsis and multiple organ failure in the early stages, or secondary biliary cirrhosis (SBC), leading to the need for liver transplantation in the long-term follow-up 11,12,13,14. Although results published from highly acknowledged centers show more than 90% success in the treatment of these severe injuries, the quality of life of patients at 5 years is severely impaired, both physically and mentally, compared to that of patients who have undergone laparoscopic cholecystectomy and have had no biliary injuries 10.
A. Injuries that involve the hepatic duct confluence
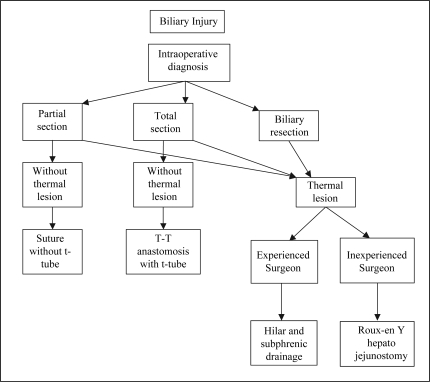
Initial management of injuries that involve the hepatic duct confluence is dependent on the time of diagnosis and the type of lesion. The algorithm we used is illustrated in Figure 115.
Figure 1. .
Algorithm for the management of intraoperative diagnosed biliary injuries.
1. Injuries identified during laparoscopic cholecystectomy
Only 15% to 30% of biliary injuries are diagnosed during the surgical procedure 16. In the current series of bile duct injuries treated at the Hospital Italiano, only 23% of lesions were detected during cholecystectomy and only 21% of these patients had undergone intraoperative cholangiography. The lesion was identified due to the existence of a bile leak or abnormal cholangiogram.
The surgeon should carefully consider his experience and ability to repair any injury that is immediately identifiable during the laparoscopic procedure. Conversion to open laparotomy has to be immediate, and injuries repaired preferably by an experienced HPB surgeon. This will reduce morbidity, shorten the stay in hospital, and decrease hospital costs 17. An inadequate primary repair may increase the incidence of biliary stenosis and introduce complications that will need new therapeutic procedures. Every failure to repair these complex injuries is associated with a loss of biliary tissue, and every attempt to repair the injuries goes up in the biliary tree, destroying duct confluence with the possibility of isolating right and left hepatic ducts 9,18.
When a lesion is identified and the surgeon performing the operation cannot repair it, the hepatic pedicle and subphrenic space have to be adequately drained and the patient referred to a tertiary center. Ligature of the ducts to allow dilatation should be avoided because of the high risk of cholangitis and bile leak with peritonitis for late slippage of the ligature.
Guidelines to be followed by HPB surgeons are given in Table II15,19,20,21. The use of intra-anastomotic stents is controversial 4,22,23, some authors reporting their use when the bile duct caliber is less than 3 or 4 mm 10,24.
Table II. Guidelines for the treatment of bile duct injuries.
|
2. Injuries diagnosed in the postoperative course
Few biliary injuries are identified during laparoscopic cholecystectomy, and instead become symptomatic weeks, months, or years later. When diagnosed in the early postoperative period, the definitive treatment should be performed immediately, i.e. first in stages combining interventional radiology and endoscopic procedures (treatment of abscesses, bilomas, cholangitis), and deferring definitive surgical treatment for 6 to 8 weeks, when local inflammatory phenomena have decreased.
Only when there is cholangitis or biliary fistula do we employ percutaneous transhepatic biliary drainage (PTBD) to stabilize the patient and to improve local conditions. Some schools use PTBD as a routine procedure prior to any surgical approach and, after bilio-enteric continuity is performed, they change the stent for a sylastic softer one, internalizing it in the same procedure 4.
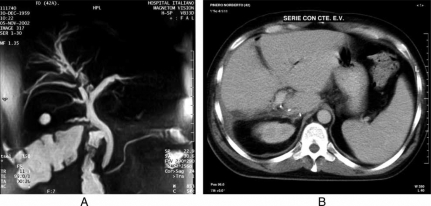
Hilar and subphrenic collections should be ruled out by abdominal ultrasound. A contrast-enhanced computed tomography (CT) sometimes has the capacity to define the injury level as well as vascular injuries and parenchymal atrophy 23.
Biliary anatomy should be thoroughly investigated before any attempt at surgical repair. Nowadays, if there is any doubt we complete the CMRI with a PTC performed when the patient is in the operating room for the definitive surgical procedure 25.
In Stewart and Way's communications, operations to repair bile duct injuries were unsuccessful in 96% of patients when cholangiograms were not obtained preoperatively and in 69% when cholangiographic data were incomplete 9.
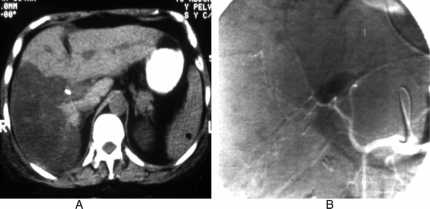
If a vascular injury is suspected either because of some abnormality of the previous studies or because of a bleeding accident during the laparoscopic cholecystectomy, abdominal angiography should be prompted in order to define hepatic artery and portal vein anatomy integrity (Figure 2).
Figure 2. .
Associated vascular injury. A. CT scan with hipodense right liver lobe. B. Angiography with injury of right hepatic artery and right portal branch.
As already mentioned, while some authors defer the definitive surgical treatment until 6 to 8 weeks after the bile injury has occurred 4,11, others do so only if the patient is unstable. They argue that the waiting time increases the complication rate as a result of drainage obstruction or displacement, and that the deferred treatment is difficult to maintain in the outpatient setting. With this strategy, they are able to perform the bile reconstruction within a median of 2 days after admission of the patient, resulting in an average length of stay of 11 days (median 9 days) compared with a 32-day average reported by authors who defer the treatment 26.
In our opinion, a very important advantage of this management is that when taking into account that laparoscopic biliary injuries very often have a thermal mechanism, the 6 or 8 weeks period allows the lesion to progress to the last stage before repair 15,25
As is the case with many other surgeons, we approach the left hepatic duct as described by Hepp and Couinaud in order to obtain normal tissue with good vascularization and to perform a wide anastomosis 25,27,28. Bismuth type E3 lesions are ideal for repair with this technique. When the ducts are isolated in Bismuth type 4 or 5 lesions, the left hepatic duct can be approached using the previously mentioned technique. If the right duct does not have a good exposure, it can be approached by performing a hepatostomy in the gallbladder fossa direction, as described by Jarnagin and Blumgart and by Strasberg et al. 19,29. The same tactics can be used when the lesion is Bismuth type 5 or Strasberg type E5. In these cases, the preoperative placement of a PTBD can be extremely useful not only in providing a biliary map but also in localizing a small right posterior duct during the surgical repair. Sometimes it is necessary to catheterize both ducts in the right side, one for the anterior sector, the other for the posterior.
3. The isolated right posterior hepatic duct injury
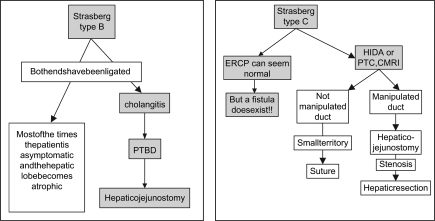
We consider the isolated right posterior hepatic duct injury as a complex lesion because of the difficulty of diagnosis and the many repair failures after treatment. The reason for these failures is the small caliber of the posterior hepatic segmental duct, which, when injured, is isolated high up in the hilum 30. The tactics for diagnosis depend on whether the isolated hepatic duct has been ligated or not (Strasberg type B or C injury). As both ends of the duct have been ligated in Strasberg type B, usually the patient is asymptomatic and the hepatic lobe becomes atrophied without any other sequelae. Although the ERCP can seem normal in type C, the lesion must be suspected because of the existence of a biliary fistula, and because the posterior segment of the right hepatic duct does not appear in the cholangiography. In these circumstances, HIDA scintigraphy or percutaneous transhepatic cholangiography (PTC) can also show the disconnected duct 31 (Figure 3).
Figure 3. .
Management of Strasberg types B and C biliary injuries.
There is some controversy regarding management of the lesion of 2- or 3-mm ducts when these are identified during laparoscopic cholecystectomy. If the duct has not been manipulated, some authors prefer to ligate it without performing anastomosis. In this case, we perform an intraoperative cholangiography of the injured duct, and if the area that this duct drains is large enough, we always carry out a Roux-en-Y hepatojejunostomy no matter how thin the duct is. If a stenosis occurs during the long-term follow-up, dilatation through interventional radiology is our option because bilio-enteric continuity already exists. If this technique fails and the patient is symptomatic, hepatic resection has to be performed 32 (Figure 4).
Figure 4. .
Intrahepatic multiple stenosis in right bile duct. A. CMRI with stenosis. B. CT scan after right hepatectomy.
Indications for liver resection are biliary confluence destruction associated with portal lesion and destruction of right anterior or posterior collectors with severe lobar atrophy. In a series of 77 patients with biliary injuries, Sauvanet et al. used hepatic resection in 15% of cases 33.
In our series, three patients with Strasberg type C and E5 lesions were treated, after failure of hepaticojejunostomy, with balloon dilatation (one of these three patients had an associated vascular injury), but this method failed in all cases and we performed a hepatic resection with good outcome.
B. High stenosis with previous repair attempt failures
Patients in whom several repair attempts have failed are complex cases and a surgical challenge. They should be thoroughly studied to avoid further failure. The work-up must always include an abdominal angiography, because a vascular associated injury can be the reason for failure. Koffron et al. reported that 61% of patients with biliary injuries, and in which primary repair attempts had failed, had associated vascular lesions. The higher the stenosis, the greater the incidence of associated vascular lesions; 71% in Bismuth type 4, 63% in type 3, and 33% in type 2 34.
These repeated failures in biliary repair generally cause a long period of cholestasis due to poor bilio-enteric drainage. Prolonged biliary obstruction can lead to progressive hepatic fibrosis and secondary biliary cirrhosis with portal hypertension. The latter is considered an ominous predictive sign of morbidity and mortality and its diagnosis prior to a therapeutic decision is crucial 19,35,36. In a recent study of biliary stenosis, hepatic histopathologic changes were found in most patients; grade I hepatic fibrosis in 47% of patients, grade II in 34%, and grade III in 11% 37.
If the patient does not have severe portal hypertension and the stenosis is either extrahepatic or limited intrahepatic, the surgical approach is used. We do a wide bilio-enteric anastomosis 1 cm above the stenosis. If the stenosis has an associated lobar atrophy, or if it is too far inside the liver and is associated with cholangitis, we carry out ipsilateral liver hepatectomy and perform a hepatico-jejuno anastomosis with the opposite duct. Hepatic resection was performed in three patients in our series (two right and one left) due to destruction of the hepatic confluence and high-up stenosis inside the liver parenchyma.
Interventional radiology has become a therapeutic option for many patients in whom morbidity and mortality can be increased due to portal hypertension. It is also useful for dilating long thermal intrahepatic stenoses that have progressed high inside the liver and difficult to approach surgically. The sole condition is that bilio-enteric continuity exists 38,39.
Misra et al. treated 51 patients with this approach, 50 (98%) of whom were stent-free at a mean follow-up of 76 months. The success rate of percutaneous management was 58.8%, needing no subsequent intervention 40.
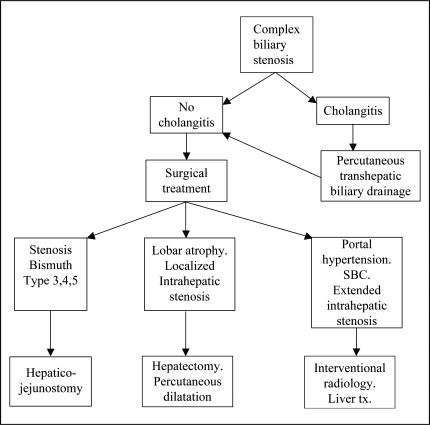
We use the algorithm described in Figure 5 for management of complex biliary stenosis.
Figure 5. .
Algorithm for the management of postoperative diagnosed biliary stenosis.
C. Bile duct injuries associated with vascular lesion
As a result of the close relationship between the common hepatic duct and the right hepatic artery, it is not unusual for this artery to be injured during laparoscopic cholecystectomy if a bile duct injury occurs. In an autopsy study of cholecystectomized patients in whom the open procedure was performed, the incidence of vascular lesions was 7% 41. After laparoscopic cholecystectomies, this incidence can be as high as 12% or 39% 9. In 27 life-threatening complex biliary injuries (Bismuth types III, IV and V), Buell et al. found associated arterial injuries in 26% of cases 42. Arterial lesions of this nature were more frequent when the biliary lesion was more proximal 34,42.
Although hepatic artery ligation can be well tolerated, certain factors condition this tolerance 43,44. Normal portal blood flow and continuity of the liver collateral circulation have to remain intact when the hepatic artery or one of its branches has been ligated. In some circumstances, this arterial ligation is not well tolerated, leading to ischemic infarction of the liver tissue.
The biliary duct is extremely sensitive to arterial blood supply deprivation and cannot tolerate surgical manipulation 45. There are arterial bridges between the left and right hepatic arteries at the level of the hilar plate called hilar plexus. Knowledge of its existence is crucial when a biliary injury is being repaired, since its attrition, as a consequence of excessive dissection, can result in a poor outcome.
When a biliary injury occurs just below the hepatic confluence, and the right hepatic artery is also injured, the blood supply to the right hepatic duct is maintained through the hilar plexus, which is fed from the left hepatic artery 46. Surgeons must identify all arterial branches in the hepatic hilum and, during liver exploration, must not ligate potentially useful collaterals such as a left hepatic branch coming from the left gastric artery or other collateral branches.
Controversy prevails regarding the consequences and implications that the association of a bile duct injury and an arterial injury may have. Alves et al. state that 19 of their 43 patients with biliary injuries had an associated right hepatic arterial lesion. All these patients underwent a Roux-en-Y hepaticojejunostomy. The authors found no differences regarding intraoperative management, blood consumption, postoperative complications, outcome in the long-term follow-up (mean time: 56±23 months) in patients with or without vascular injuries 7.
Koffron et al. reported failure to repair 18 consecutive cases with biliary injuries that were referred to a tertiary center. In 61% of cases they identified associated vascular injuries and concluded that arterial disruption could affect the outcome of primary management of bile duct injuries 34.
Buell et al. found that an associated arterial injury is an independent predictor of mortality (38% with versus 3% without arterial injury p<0.001) 42.
In a comprehensive review, Shallaly et al. advised assessing arterial compromise in all biliary injuries, since management and outcome are influenced by the absence of arterial blood flow 47. The vascular lesion has to be suspected: when a bleeding accident during laparoscopic cholecystectomy occurs, when there is a sudden rise in ALT during early postoperative course, or when there are multiple metallic clips on plain film images of the abdomen. In these cases, an abdominal angiography is always indicated to rule out any arterial or portal venous damage.
We never use Doppler ultrasound in the above-mentioned cases, as other authors have described, owing to the existence of collateral circulation producing false-positive results 34.
If a vascular associated biliary lesion is identified during the intra-operative procedure, the immediate reconstruction of both lesions has to be accomplished, thus preventing possible hepatic necrosis, hepatico-jejunostomy anastomotic fistula, or bile duct stricture in the long-term follow-up 46,48. The technique for arterial reconstruction will depend on the type of lesion. A direct anastomosis can be done if there is no loss of arterial tissue and if the sectioned ends are not attritioned. If the hepatic artery has been resected, an inferior mesenteric artery is the preferred interposition graft to be used.
The approach to be taken if the arterial occlusion is detected later is not clearly stated in the literature. The controversy arises because late arterial reconstruction will not prevent the already existing hepatic necrosis. However, the influence on the hepaticojejunostomy anastomosis remains unknown 46.
If an arterial injury is suspected in the immediate postoperative period, a complete abdominal angiography, including portal vein evaluation, has to be done. It is extremely important to identify the distal arterial end and to find out if there is good retrograde flow through it during the surgical approach.
If the arterial occlusion has an attritioned distal end or has no retrograde flow that prevents reconstruction, but coexists with good portal flow and lobar ischemia is not evident, a hepaticojejunostomy can be performed because many patients have a good evolution. If arterial reconstruction is impossible, however, due to technical reasons and lobar ischemia is evident, hepatic resection is indicated together with hepaticojejunostomy in the remaining duct 49,50,51.
Since the clearing function of the liver with the translocated intestinal bacteria is impaired after ischemia, it is important to maintain these patients with high antibiotic levels in the blood just to avoid septic complications in the ischemic liver parenchyma 52,53.
D. Bile duct injury associated with portal hypertension or secondary biliary cirrhosis
Successive failures of therapeutic procedures or inappropriate treatment of cholestasis and infection may lead to end-stage liver disease within a few years post injury 54,55. In a historical series of bile duct reconstruction, the incidence of portal hypertension and SBC was 8% 56. Johnson et al. stated that the development of hepatic fibrosis confirmed by liver biopsy was associated with a delay in adequate treatment being administered in patients with biliary stenosis 57.
The presence of cirrhosis during bile duct injury repair is considered an ominous sign and the most important risk factor predicting increased morbidity and mortality 58. In Chapman et al.'s series of bile duct injuries, 23 patients had portal hypertension and a high mortality rate during surgical reconstruction (26%). The mortality rate for patients with PH who underwent some surgical procedure was 23% (n=5). In contrast, the mortality rate in patients without portal hypertension, and who underwent some surgical procedure, was only 2% (n=2) 18. The results of biliary reconstruction in patients with cirrhosis are poor. Pellegrini et al. report only 25% of good results in patients with recurrent biliary stenosis associated with biliary cirrhosis 36. SBC by itself has a poor prognosis and a high late mortality rate despite the patency of the hepaticojejunostomy 59.
The time required for the development of SBC after benign biliary stenosis has been reported to be 7.1 years, i.e. 4.6 years in those with common bile duct stones and 0.8 years in patients with malignant biliary obstruction 60. Recent studies describe the time of obstruction, basal ALT level, and time to normalization of ALT level after surgical repair as predictive factors in the development of hepatic fibrosis 37.
At our unit, patients with complex biliary injuries and portal hypertension, and who have bilio-enteric continuity, are treated by interventional radiology. If there is no continuity and the patient has some contraindication for liver transplantation, the bile duct is drained with a TPBD and portal hypertension is treated with a transjugular intrahepatic portosystemic shunt (TIPS) or a mesocaval shunt before bile duct repair. On three occasions, we treated patients with biliary stenosis associated with cavernomatous transformation of the portal vein. These patients had undergone a mesocaval shunt prior to hepaticojejunal anastomosis with a good outcome.
Most of the histologic changes produced in the early obstruction stages are reversible if adequate treatment is performed in good time 61. Unfortunately, many patients arrive at our unit late, after having undergone multiple unsuccessful treatments and with signs and symptoms of end-stage liver disease. To date, there have been few publications about liver transplantation as a treatment for SBC 62,63,64,65.
Our experience was published in 2002 13. In a 10-year period (1988–1998), 8 out of 14 patients with SBC were given transplants. The most evident proof of the severity of the 14 patients who were included in the transplant waiting list with SBC was the mortality rate (28.5%, i.e. 4 patients). One of the patients had an injured right arterial and portal pedicle which led to complete atrophy of that lobe 13.
Intractable ascites, repeated episodes of variceal bleeding, repeated cholangitis, progressive jaundice, pruritus and poor quality of life are all indicators of the need for liver to be replaced 66. The hospital mortality rate of this series was 12.5% (13), which is similar to results reported in the literature 63. The 5-year survival rate of liver transplantation for benign diseases exceeds 80% with excellent quality of life. Up to now, 16 of our patients have been given transplants, with an actuarial 1-year survival rate of 91.7%. However, we lost 4 patients who were on the waiting list.
Biliary injuries produced during laparoscopic cholecystectomy have proved to be more severe and complex. These lesions represent an intricate disease that is difficult to diagnose and treat. Inadequate procedures, multiple interventions performed by inexperienced surgeons, and delayed referrals to specialized centers may result in late complications sometimes requiring liver transplantation as the only possible treatment.
References
- 1.Cuschieri A, Dubois F, Mauriel J, Houser P, Becker H, Bues G. The European experience with laparoscopic cholecystectomy. Am J Surg. 1991;161:385–7. doi: 10.1016/0002-9610(91)90603-b. [DOI] [PubMed] [Google Scholar]
- 2.Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. 1995;180:101–5. [PubMed] [Google Scholar]
- 3.Fletcher DR, Hobbs MST, Tan P. Complications of cholecystectomy bile duct injuries: risks of the laparoscopic approach and prospective effects of operative cholangiography. A population-based study. Ann Surg. 1999;229:449–57. doi: 10.1097/00000658-199904000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lillemoe KD, Melton GB, Cameron JL, Pitt HA, Cambell KA, Talamini MA, et al. Postoperative bile duct strictures: management and outcome in the 1990s. Ann Surg. 2000;232:430–41. doi: 10.1097/00000658-200009000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shah SR, Mirza DF, Afonso R, Mayer AD, McMaster P, Buckels JAC. Changing referral pattern of biliary injuries sustained during laparoscopic cholecystectomy. Br J Surg. 2000;87:890–1. doi: 10.1046/j.1365-2168.2000.01446.x. [DOI] [PubMed] [Google Scholar]
- 6.Mur MM, Gigot JF, Nagorny WS, Harnsen MS, Ilstrup MS, Faumle MB. Long-term result of biliary reconstruction after laparoscopic bile duct injuries. Arch Surg. 1999;134:604–10. doi: 10.1001/archsurg.134.6.604. [DOI] [PubMed] [Google Scholar]
- 7.Alves A, Farges O, Nicolet J, Wadrin T, Sauvanet A, Belghiti J. Incidence and consequence of an hepatic artery injury in patients with post cholecystectomy bile duct strictures. Ann Surg. 2003;238:211–16. doi: 10.1097/01.sla.0000074983.39297.c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chandhary A, Monisegron M, Chandro A, et al. How do bile duct injuries sustained during laparoscopic cholecystectomy differ from those during open cholecystectomy? J Laparoendosc Adv Surg Tech. 2001;11:187–91. doi: 10.1089/109264201750539682. [DOI] [PubMed] [Google Scholar]
- 9.Stewart L, Way L. Bile duct injuries during laparoscopic cholecystectomy. Factors that influence the result of treatment. Arch Surg. 1995;130:1123–9. doi: 10.1001/archsurg.1995.01430100101019. [DOI] [PubMed] [Google Scholar]
- 10.Mercado M, Orozco H, Lopez Martinez LM, Perez del Vllar AP, Tielve M, et al. Survival and quality of life alter bile duct reconstruction for iatrogenic injury. Hepato Pancreato Bil. 2000;2:321–4. [Google Scholar]
- 11.Gouma DJ, Obertop H. Management of bile duct injuries: treatment and long-term results. Dig Surg. 2002;19:117–22. doi: 10.1159/000052024. [DOI] [PubMed] [Google Scholar]
- 12.Loinaz C, Gonzalez EM, Jimenez C, Garcia I, Gomez R, Gonzalez Pinto I, et al. Long-term biliary complications alter liver surgery leading to liver transplantation. World J Surg. 2001;25:1260–3. doi: 10.1007/s00268-001-0106-4. [DOI] [PubMed] [Google Scholar]
- 13.de Santibañes E, Pekolj J, McCormack L, Nefa J, Matera J, Sivori J, et al. Liver transplantation for the sequelae of intra-operative bile duct injury. Hepato Pancreato Bil. 2002;4:34–8. doi: 10.1080/136518202760387993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Melton G, Lillemoe K, Cameron J, et al. Major bile duct injuries associated with laparoscopic cholecystectomy. Effect of surgical repair on quality of life. Ann Surg. 2002;235:888–95. doi: 10.1097/00000658-200206000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pekolj J. Manejo de las complicaciones más frecuentes de la cirugía abdominal. Rev Arg de Cirg 2003. Número extraordinario. [Google Scholar]
- 16.Stewart L, Way L. Bile duct injuries during laparoscopic cholecystectomy. Factors that influence the result of treatment. Arch Surg. 1995;130:1123–9. doi: 10.1001/archsurg.1995.01430100101019. [DOI] [PubMed] [Google Scholar]
- 17.Savader SJ, Lillemoe KD, Prescoth CA, et al. Laparoscopic cholecystectomy-related bile duct injuries: a health and financial disaster. Ann Surg. 1997;225:268–73. doi: 10.1097/00000658-199703000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chapman WC, Haley A, Blumgart LH, Benjamin IS. Postcholecystectomy bile duct strictures. Management and outcome in 130 patients. Arch Surg. 1995;130:412–16. doi: 10.1001/archsurg.1995.01430060035007. [DOI] [PubMed] [Google Scholar]
- 19.Jarnagin WR, Blumgart LH. Operative repair of bile duct injuries involving the hepatic duct confluence. Arch Surg. 1999;134:769–75. doi: 10.1001/archsurg.134.7.769. [DOI] [PubMed] [Google Scholar]
- 20.Mathews JB, Blumgart LH. Zinner M, Schwartz , Ellis H. Appleton and Lange; Norwalk: 1997. Benign biliary strictures, Maingot's abdominal operations; pp. 1803–34. [Google Scholar]
- 21.Smadja C, Blumgart LH. Blumgart LH. Churchill Livingstone; Edinburgh: 1994. The biliary tract and the anatomy of biliary exposure, Surgery of the liver and biliary tract; pp. 11–24. [Google Scholar]
- 22.Tochi A, Costa G, Lepre L, Liotta G, Masón G, Sito A. The long-term outcome of hepaticojejunostomy in the treatment of benign bile duct strictures. Ann Surg. 1996;224:162–7. doi: 10.1097/00000658-199608000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blumgart LH. Hilar and intrahepatic biliary enteric anastomosis. Surg Clin North Am. 1994;74:845–63. [PubMed] [Google Scholar]
- 24.Mercado M, Orozco H, et al. To stent or not to stent bilio enteric anastomosis after iatrogenic injury: a dilemma not answered. Arch Surg. 2001;1:60–3. doi: 10.1001/archsurg.137.1.60. [DOI] [PubMed] [Google Scholar]
- 25.de Santibañes E, Sivori J, Pekolj J, et al. Lesiones de la via biliar secundaria a colecistectomía laparoscópica. Rev Arg de Cirg. 1996;70:208–19. [Google Scholar]
- 26.Wudel LJ, Pinson WC, et al. Bile duct injury following laparoscopic cholecystectomy. Am Surg. 2001;67:557–64. [PubMed] [Google Scholar]
- 27.McDonald M, Fornell M, Nagorney D, et al. Benign biliary strictures: repair and outcome with a contemporary approach. Surgery. 1995;118:582–91. doi: 10.1016/s0039-6060(05)80022-4. [DOI] [PubMed] [Google Scholar]
- 28.Hepp J. Hepaticojejunostomy using the left biliary trunk for iatrogenic biliary lesions: the French connection. World J Surg. 1995;9:507–11. doi: 10.1007/BF01655291. [DOI] [PubMed] [Google Scholar]
- 29.Strasberg SM, Picus DD, Delvin JA. Results of a new strategy for reconstruction of biliary injuries having an isolated right sided component. J Gastrointest Surg. 2001;3:266–74. doi: 10.1016/s1091-255x(01)80047-0. [DOI] [PubMed] [Google Scholar]
- 30.Suhocki PV, Meyers WC. Injury to aberrant bile ducts during cholecystectomy. A common cause of diagnostic error and treatment delay. Am J Roentgenol. 1999;172:955–9. doi: 10.2214/ajr.172.4.10587128. [DOI] [PubMed] [Google Scholar]
- 31.Chapman WC, Abecassis W, Jarnagin W, Mulbihill S, Strasberg S. Bile duct injuries, 12 years after the introduction of laparoscopic cholecystectomy. J Gastrointest Surg. 2003;7:412–16. doi: 10.1016/s1091-255x(02)00162-2. [DOI] [PubMed] [Google Scholar]
- 32.Venishi T, Hirohashi K, Tanaka H, et al. Right hepatic lobectomy for recurrent cholangitis after bile duct and hepatic artery injury during laparoscopic cholecystectomy. Report of a case. Hepatogastroenterology. 1999;46:2296–8. [PubMed] [Google Scholar]
- 33.Sauvanet A, Belghiti J, et al. Major hepatectomy for bile duct injuries after cholecystectomy. Hepato Pancreato Bil. 2000;2:171–5. [Google Scholar]
- 34.Koffron A, Ferrario M, Parson A, Nervicec A, Salker M, Abecassis M. Failed primary managements of iatrogenic biliary injuries: incidence and significance of concomitant hepatic arterial disruption. Surgery. 2001;130:722–31. doi: 10.1067/msy.2001.116682. [DOI] [PubMed] [Google Scholar]
- 35.Rothlin MA, Lopfe M, Schlumpp T, Largiader F. Long-term results of hepatojejunostomy for benign lesions of the bile ducts. Am J Surg. 1998;178:22–6. doi: 10.1016/s0002-9610(97)00229-8. [DOI] [PubMed] [Google Scholar]
- 36.Pellegrini CA, Thomas MJ, Way LW. Recurrent biliary stricture: patterns of recurrence and outcome of surgical therapy. Am J Surg. 1984;147:175–80. doi: 10.1016/0002-9610(84)90054-0. [DOI] [PubMed] [Google Scholar]
- 37.Sanjay Singh Negi, Sakhuja P, Malhotra V, et al. Factors predicting advanced hepatic fibrosis in patients with postcholecystectomy bile duct strictures. Arch Surg. 2004;139:299–303. doi: 10.1001/archsurg.139.3.299. [DOI] [PubMed] [Google Scholar]
- 38.Pitt HA, Kaufman SC, Coleman J, et al. Benign postoperative biliary strictures: operate or dilate? Ann Surg. 1989;210:417–27. doi: 10.1097/00000658-198910000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mueller PR, Van Sonnemberg E, Ferrucci T, Jr, et al. Biliary stricture dilatation: multicenter review of clinical management in 73 patients. Radiology. 1986;160:17–26. doi: 10.1148/radiology.160.1.3715030. [DOI] [PubMed] [Google Scholar]
- 40.Misra S, Melton G, Geschwind JF, Venbrux AC, Cameron JL, Lillemoe K. Percutaneous management of bile duct strictures and injuries associated with laparoscopic cholecystectomy. J Am Coll Surg. 2004;198:218–27. doi: 10.1016/j.jamcollsurg.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 41.Halasz NA. Cholecystectomy and hepatic artery injury. Arch Lung. 1991;126:137–8. doi: 10.1001/archsurg.1991.01410260021002. [DOI] [PubMed] [Google Scholar]
- 42.Buell JF, Cronin DC, Funaki B, Koffron A, Yoshida A, Lo A, et al. Devastating and fatal complications associated with combined vascular and bile duct injuries during cholecystectomy. Arch Surg. 2002;137:703–10. doi: 10.1001/archsurg.137.6.703. [DOI] [PubMed] [Google Scholar]
- 43.Bengmark S, Rosengreen K. Arteriographic studies of the collateral circulation to the liver after ligation of the hepatic artery in man. Am J Surg. 1970;119:620–4. doi: 10.1016/0002-9610(70)90228-x. [DOI] [PubMed] [Google Scholar]
- 44.Brittain RS, Marchioro TL, Hermann G, Wadell WR, Starzl TE. Accidental hepatic artery ligation in humans. Am J Surg. 1964;107:822–32. doi: 10.1016/0002-9610(64)90169-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heinrich S, Seifert H, Krähenbühl L, Fellbaunn C, Lorenz M. Right hemihepatectomy for bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 2003;17:1494–5. doi: 10.1007/s00464-002-4278-2. [DOI] [PubMed] [Google Scholar]
- 46.Gupta N, Solomon H, Fairchild R, Kaminski D L. Management and outcome of patients with combined bile duct an hepatic artery injuries. Arch Surg. 1998;133:176–181. doi: 10.1001/archsurg.133.2.176. [DOI] [PubMed] [Google Scholar]
- 47.Shallaly GEI, Cuschieri A. Nature, aetiology and outcome of bile duct injuries after laparoscopic cholecystectomy. HPB Surg. 2000;2:3–12. [Google Scholar]
- 48.Bachellier P, Nakano H, Weber JC, Lemarque P, Oussoultzojlou E, Candon Ch, Wolf P, Jaeck D. Surgical repair after bile duct an vascular injuries during laparoscopic cholecystectomy: When and How? World J Surg. 2001;25:1335–1345. doi: 10.1007/s00268-001-0120-6. 2001. [DOI] [PubMed] [Google Scholar]
- 49.Schmidt SC, Langrehr JM, Raakow R, Klupp J, Steinmuller T, Nehaus P. Right hepatic lobectomy for recurrent cholangitis after combined bile duct and right hepatic artery injury during laparoscopic cholecystectomy: a report of two cases. Langenbeck‘s Arch Surg. 2002;387:183–187. doi: 10.1007/s00423-002-0300-3. [DOI] [PubMed] [Google Scholar]
- 50.Lichtenstein S, Moorman D, Malatesta JQ, Martin MF. The role of hepatic resection in the management of bile duct injuries following laparoscopic cholecystectomy. The American Surgeon. 2000;66:372–377. [PubMed] [Google Scholar]
- 51.Nishio H, Kamiya J, Nagino M, Vesaka K, Kanai M, Sano T, et al. Right hepatic lobectomy for bile duct injury associated with major vascular occlusion after laparoscopic cholecystectomy. J Hepatobiliary Pancreat Surg. 1999;6:427–430. doi: 10.1007/s005340050145. [DOI] [PubMed] [Google Scholar]
- 52.Wells C, Maddans MA, Simmons R L. Proposed mechanisms for the translocation of intestinal bacteria. Rev Infect Dis. 1988;10:958–963. doi: 10.1093/clinids/10.5.958. [DOI] [PubMed] [Google Scholar]
- 53.Schatlen WE. The role of intestinal bacteria in liver necrosis following experimental excision of the hepatic arterial supply. Surgery. 1954;36:256–269. [PubMed] [Google Scholar]
- 54.Mirza DF, Narsimham KL, Ferraz Neto B, Mayer AD, Mc Master P, Buckels JAC. Bile duct injury following laparoscopic cholecystectomy: referral pattern and management. Br J Surg. 1997;84:786–790. [PubMed] [Google Scholar]
- 55.Topal B, Aerts R, Pennincky F. The outcome of major biliary tract injury with leakage in laparoscopic cholecystectomy. Surg Endoscop. 1999;13:53–56. doi: 10.1007/s004649900897. [DOI] [PubMed] [Google Scholar]
- 56.Braasch JW, Bolton JS, Rossi R. A technique of biliary tract reconstruction with complete follow–up in 44 consecutive cases. Ann Surg. 1981;194:635–638. doi: 10.1097/00000658-198111000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Johnson SR, Koehler A, Pennington LK, Hauto DW. Long–term results of surgical repair of bile duct injuries following laparoscopic cholecystectomy. Surgery. 2000;128:668–677. doi: 10.1067/msy.2000.108422. [DOI] [PubMed] [Google Scholar]
- 58.Rothlin MA, Loppe M, Schlumpf R, Largiader F. Long–term results of hepaticojejunostomy for benign lesion of bile ducts. Am J Surg. 1998;175:22–26. doi: 10.1016/s0002-9610(97)00229-8. [DOI] [PubMed] [Google Scholar]
- 59.Rauti M, Podlech P, Jaschlse W, Manegold BC, Trede M, Chir B. Management of bile duct injuries and strictures following cholecystectomy. World J Surg. 1993;17:553–562. doi: 10.1007/BF01655124. [DOI] [PubMed] [Google Scholar]
- 60.Scobie BA, Summerskil WH. Hepatic cirrhosis secondary to obstruction of the biliary system. Am J Diag Dis. 1965;10:135–146. doi: 10.1007/BF02236664. [DOI] [PubMed] [Google Scholar]
- 61.Zimmermann H, Reichen J, Zimmermann A, Sagesser H, Therrisch B, Hoflin F. Reversibility of secondary biliary fibrosis by biliodigestive anastomosis in the rat. Gastroenterology. 1992;103:579–589. doi: 10.1016/0016-5085(92)90850-x. [DOI] [PubMed] [Google Scholar]
- 62.Madariaga JR, Dodson T, Selby R, Todo S, Iwatsuki S, Starzl TE. Corrective treatment and anatomic considerations for laparoscopic cholecystectomy injuries. J Am Coll Surg. 1994;179:321–324. [PMC free article] [PubMed] [Google Scholar]
- 63.Nordin A, Halme L, Makisalo H, Isoniemi K, Hockeusted T. Management and outcome of major bile duct injuries after laparoscopi cholecystectomy: from therapeutic endoscopy to liver transplantation. Liver Transplantation. 2002;8:1036–1043. doi: 10.1053/jlts.2002.35557. [DOI] [PubMed] [Google Scholar]
- 64.Bacha E, Stieler AC, Galloway JR, Hunter JG. Non–biliary complication of laparoscopic cholecystectomy. Lancet. 1994;344:896–897. [PubMed] [Google Scholar]
- 65.Robertson AJ, Rela M, Karani J, Steger AC, Benjamin IS, Heaton ND. Laparoscopic cholecystectomy injury: An anusual indication for liver transplantation. Transpl Int. 1998;11:449–451. doi: 10.1007/s001470050173. [DOI] [PubMed] [Google Scholar]
- 66.Bismuth H, Samuel D. Indications et resultants de la transplantation hepatique. EMC 7080.A. 9–1990. [Google Scholar]