Abstract
Objective
Correlating histology with endometriosis characteristics.
Design
Secondary data analysis.
Setting
Government Research Hospital.
Patients
Women with chronic pelvic pain and endometriosis.
Intervention
Laparoscopic excision of lesions.
Main Outcome Measures(s)
Histologic examination for endometriosis.
Materials and Methods
Between 1999 and 2004, 133 women underwent laparoscopic surgery, during which lesion characteristics and surgical impression of the lesions were recorded. All biopsied were sent for histological examination, and surgical and histological findings were compared.
Results
357 of 544 lesions felt to be endometriosis by the surgeon had positive histology. Mixed color lesions most commonly contained endometriosis (76%), with the percent of positive lesions being similar between single color groups. 58% (164/283) of subtle (red or white) lesions were positive for endometriosis. Thirty women had only red or white lesions, and 18 (60%) had at least one lesion positive for endometriosis. Lesions were most commonly located in the cul-de-sac (64%), utero-sacral ligaments (68%), and ovarian fossa (70%).
Conclusion(s)
Wide, deep, mixed color lesions in the cul-de-sac, ovarian fossa or the utero-sacral ligaments had the highest frequency of endometriosis. Over half of subtle lesions had endometriosis. These results should be considered when diagnosing endometriosis.
Keywords: endometriosis, lesion characteristics, lesion color, prediction of endometriosis, laparoscopy, surgical diagnosis
The 2005 ESHRE guidelines on endometriosis state that laparoscopic visualization of suspicious lesions is the “gold standard” for the definitive diagnosis of endometriosis (1). The typical appearance of endometriosis is described as a superficial “powder-burn” or “gunshot” lesion that is black, dark-brown, or blue, but subtle lesions which are red or clear, small, cysts with hemorrhage or white areas of fibrosis may also be endometriosis (1). We have previously found that white and mixed color lesions had a higher percentage of histology confirmed endometriosis than black lesions (2). Nisolle and Donnez (3) attributed the color of the endometriosis lesions to changes as the lesions age, starting as a red lesion, then progressing to black and finally to white (2, 4-7). Thus endometriosis is not limited to a single color and may be confirmed more frequently in a multi-colored lesion. At present, it is unclear as to which color is most frequently associated with endometriosis.
Considering additional lesion characteristics, such as lesion location and size, may improve the ability to predict endometriosis. Locations reported to have a high rate of endometriosis include the cul-de-sac, ovarian fossa, and the uterosacral ligaments (2, 5). In addition, wide and deep lesions have been more strongly correlated with positive histology (2, 5). Other methods to diagnose endometriosis prior to surgery, such as detailed history/physical, MRI or ultrasound (1, 8-12), have shown poor correlation between pre-surgical prediction and post-surgical findings. To date, surgical findings continue to provide the most accurate and reliable means of diagnosing endometriosis (1).
Defining the characteristics of endometriosis lesions and validating these findings with biopsy results has been one of our long-term objectives. Since reporting our analysis of lesion characteristics in a group of 77 women (2), we have operated on 56 additional subjects. Here we report the findings of the entire cohort of women undergoing surgery from 1999 to 2004.
Methods
Women between the ages of 18 and 45 were enrolled from 1999 to 2004 in a National Institutes of Health research protocol evaluating the use of raloxifene for the treatment of endometriosis. All women were healthy with the exception of pelvic pain that had lasted at least 3 months; none had received hormonal or surgical treatment during the 6 months study entry. Subjects used a reliable non-hormonal form of contraception, and pregnant women or those attempting to become pregnant were excluded. Patients were excluded if their pelvic pain was due to an infectious, gastrointestinal, musculoskeletal, neurologic, or psychiatric cause. The Institutional Review Board from the National Institute of Child Health and Human Development approved this study.
All participants underwent laparoscopy, during which lesions suspicious for endometriosis were excised using the contact neodymium:yttrium-aluminum-garnet laser (Surgical Laser Technologies, The Oaks, PA). Some lesions, such as adhesions, paratubal cysts or other peritoneal surface lesions which were not believed to be endometriosis were removed. Normal appearing peritoneum was not biopsied. All excised lesions were sent for pathologic diagnosis regardless of the surgeon's impression of the lesion; no lesions were ablated. Peritoneal defects were excised in-toto and endometriomas were removed by stripping the cyst wall from the ovary or peritoneal structures. The appendix was removed if it was chronically inflamed or appeared to contain endometriosis. If an implant was deep in the recto-vaginal septum, obliterated the cul-de-sac, appeared to be transmural to the bowel wall or ureter, or was adherent to a blood vessel, it was not resected since removal of these lesions represented unreasonable risks.
At the time of surgical excision, the following information was collected on all lesions. The surgeon's impression of the type of lesion (endometriotic lesion vs. non-endometriotic lesion) was recorded. Lesion location was listed in categories which included the bladder peritoneum, colon/appendix, cul-de-sac, ovarian fossa, ovary, sidewall, utero-sacral ligament, and uterus/fallopian tube. Width was recorded as the average of 2 measured diameters and placed in categories of <5mm, 5−10mm, 11−20mm, and >20mm. If more than one implant was noted within 5mm of another one, a single distance across both lesions was measured. Depth was based on one measurement and was then categorized as <2mm, 2−4mm, 5−10mm, and >10mm. Color categories included red (red or clear), white, black (black, brown, blue, yellow), and mixed (any two of the color categories). The stage of the disease was assigned using the standards described in the revised American Fertility Society classification system (13).
Once excised, all lesions were sent for histologic examination. A pathologist reviewed hematoxlin and eosin stained slides from formalin-fixed, paraffin-embedded specimens for evidence of endometriosis. If no endometriosis was seen on the initial slide, the examination was repeated using samples from three different levels of the paraffin block and CD10 staining was done to aid in identifying glands and stroma (14). Both endometrial glands and stroma were present for the lesion to be labeled as containing endometriosis.
Univariate and bivariate results were calculated using Stata 8.2 (Stata Corporation, College Station, TX). T-tests and χ2 testing were done as appropriate. Using the surgeon's impression as a test for disease, positive predictive value (PPV), negative predictive value (NPV), sensitivity and specificity were calculated. A p value of < 0.05 was considered statistically significant.
Results
The mean age of women undergoing surgery was 31.5 ± 7.2 years. Seventy-nine percent reported their race as white, 16% as black, and 4% as other race. Twenty-one percent (23 of 133) of women had no evidence of endometriosis at the time of surgery in spite of having clinical symptoms that were highly suggestive for the disease. Of the remaining 110 women, 11 (10%) had lesions which appeared to be endometriosis, but lacked histologic confirmation. Eight of these women had Stage I disease, two women had Stage II disease, and one woman who was believed to have stage IV endometriosis had 4 biopsies that were negative for endometriosis.
A total of 611 lesions were excised from the remaining 110 women. Surgeons impression and histologic diagnosis were available on 603 of these lesions. Five hundred and forty four lesions were thought be endometriosis and 59 lesions were judged to be non-endometriotic. Of the 544 “endometriosis” lesions, 350 or 65.0% met the pathology criteria for endometriosis (true positive results). In the remaining 194 lesions, endometriosis could not be confirmed with histology (false positive results). Of the 59 lesions thought to be negative, 52 or 88% had no evidence of endometriosis (true negative results). However, seven lesions (11.9%) in this group had histology confirmed endometriosis in spite of the surgeon's impression (false negative results). Of these seven lesions, four were found on the uterus or fallopian tubes, one was in the ovarian fossa, and 2 were removed from the ovary.
The PPV of using only an experienced surgeon's impression to identify histologically positive lesions was 64.0%, and the NPV was 88%. The sensitivity and specificity of using this method was 98 and 21%, respectively.
One hundred and fifty of these lesions were black (28%), 161 (30%) were red, 123 (23%) were white, and 104 (19%) were of mixed color. Overall, single color lesions had similar frequencies of biopsy-confirmed endometriosis (62%, 57%, and 59%, respectively), and only lesions with multiple colors had a significantly higher percentage of positive biopsies (76%) (p = 0.015) (Figure 1). When lesion width was greater than 10mm (59% for width <10mm vs. 82% for width >10mm) or depth was greater than 5mm there was a higher frequency of biopsy confirmed endometriosis (41% vs. 78% for < 5 vs >5mm, respectively) (Figure 2). A higher percentage of lesions were positive for endometriosis when they were found in the cul-de-sac (77%), utero-sacral ligaments (77%), and ovarian fossa (76%) (p < 0.05 for all groups) (Table 1).
Figure 1.
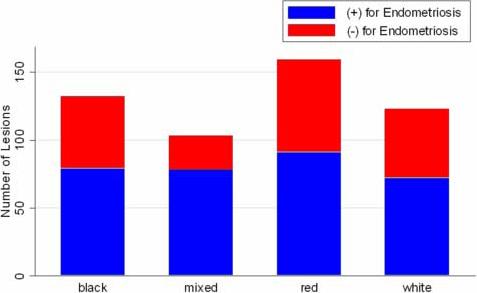
Distribution of Lesions by Color Group
Figure 2.
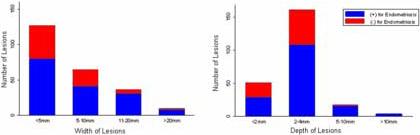
Distribution of Lesions by Width and Depth
Table 1.
Location of Lesions by Surgeon's Impression and Histology
| Location | Presumed Positive Lesions N (%) | Presumed Positive Lesions with (+) Histology N (%) | Presumed Negative Lesions N (%) | Presumed Negative Lesions with (+) Histology N (%) |
|---|---|---|---|---|
| Ovarian fossa | 132 (24) | 96 (73) | 6 (9) | 1 (17) |
| Cul-de-sac | 133 (24) | 92 (69) | 10 (16) | 0 |
| Utero-sacral Ligament | 76 (14) | 52 (68) | 1 (2) | 0 |
| Bladder/Peritoneum | 73 (13) | 40 (55) | 4 (6) | 0 |
| Ovary | 53 (10) | 31 (58) | 17 (27) | 2 (12) |
| Uterus/Fallopian Tube | 29 (5) | 15 (52) | 16 (25) | 4 (25) |
| Sidewall | 32 (6) | 16 (50) | 4 (6) | 0 |
| Colon/Appendix | 9 (2) | 6 (67) | 5 (8) | 1 (20) |
| Round/Broad Ligament | 5 (1) | 2 (40) | 0 | 0 |
| Total | 542* | 350 (65)** | 63 + | 8 (12.7)++ |
7 lesions missing location data;
6 lesions missing location data;
30 lesions missing location data;
1 lesions missing location data
Over half (283 of 544) of all lesions were red or white (subtle) lesions. Of these subtle lesions, 58% (164 of 283) contained histologic evidence of endometriosis compared to 68% (254 of 536) of black or multi-colored lesions. In 30 women, the only lesions identified were either red or white; positive histology was found in 18 (60%) of these women. Even when we restricted the definition of subtle lesions to subtle color (red or white lesions), small size (a width less than 10mm and a depth less than 5mm), and atypical location (other than the cul-de-sac, ovarian fossa, or uterosacral ligaments), 20 of these 54 (37%) lesions (18 of 42 red and 2 of 12 white ones, respectively) were histology confirmed as endometriosis. Of five subjects who only had this type of lesion, 2 women (40%) had lesions which contained positive histology for endometriosis.
Discussion
Our results indicate that at least 75% of lesions that have a mixture of colors, have a depth greater than 5 mm or a width greater than 10 mm, and that were located in the cul-de-sac, in the ovarian fossa, or on the utero-sacral ligament contain histological evidence for endometriosis. In addition, we found that most endometriosis lesions were subtle in color rather than the traditionally described black, powder-burned appearance (1, 2). Furthermore, all single color lesions contained biopsy-confirmed endometriosis at about 60%. Therefore, no single color had a high association with endometriosis, and any lesion containing a single color should be considered equally suspicious for containing endometriosis.
Overall, subtle lesions were nearly as likely to contain endometriosis as those that were black or had mixed color (58% vs. 68%, respectively). Of those women (n=30) who only had subtle lesions, 60% (n=18) were confirmed to have endometriosis on biopsy. Had the diagnosis of endometriosis been based solely on the appearance of these lesions, 16% of our subjects would have been excluded. When the definition of a subtle lesion excluded large, deep lesions that were located in the cul-de-sac, ovarian fossa or on the utero-sacral ligament, 20 of 54 (37%) lesions contained histologically confirmed endometriosis and a similar proportion of women who only had this type of lesion (2 of 5) were found to have biopsy proven endometriosis. Thus, when subtle lesions are found, it may be beneficial to confirm the diagnosis of endometriosis by biopsy.
We were able to corroborate the diagnosis of endometriosis with positive histology in most subjects because we performed multiple biopsies on each woman with surgical findings. However, 11 (8%) women did not have any biopsy containing endometriosis despite having clinical symptoms highly suggestive of the disease. It is possible that these women were misclassified as being disease free as their endometriosis lesions may have been missed during surgery despite our systematic approach to identification and excision of lesions.
Despite attempting to include only women with chronic pelvic pain associated with endometriosis, 20% of women had no evidence of any endometriosis lesions at laparoscopy. Other etiologies for chronic pain, such as pelvic adhesions or evidence of previous pelvic infections (2), could not be eliminated by our screening procedures. The ability to diagnose endometriosis by noninvasive means might have prevented these women from undergoing this procedure, and would be enhanced with the development of more sensitive screening tests and better serologic markers (1, 9, 15, 16)
This study has significant strengths. A large number of women were enrolled from whom a large number of samples were obtained. Also, while the primary study objective of the clinical trail was not to describe lesion characteristics, it was a secondary objective, thus allowing for prospective data collection.
The study design may have caused limitations in our analysis. First, the goal of the clinical trial was to evaluate the effects of raloxifene for chronic pain associated with endometriosis. Therefore, patients were selected as those who were likely to have endometriosis and were not representative of reproductive aged women. Because of these strict entry criteria, these findings may not apply to the general population. Second, the study was not specifically designed to characterize the color and location of endometriosis lesions; non-endometriotic lesions were not routinely excised and may not have been fully characterized. A third, expected limitation is that as our surgical experience increased, our ability to identify endometriosis correctly improved, as others have also reported (6) . However, this illustrates the importance of each surgeon comparing her or his surgical findings with histologic reports.
In conclusion, the lesions most likely to be positive for endometriosis were those greater than 10 mm in width and greater than 5 mm in depth, mixed in color, and located in the cul-de-sac, ovarian fossa, or on the utero-sacral ligaments. However, even surgeons knowledgeable and experienced in the characteristics of endometriosis lesions were only able to correctly identify lesions with confirmed endometriosis 64% of the time. The diagnosis of endometriosis is highly dependent on the surgeon's ability to recognize lesions, both “typical” and “subtle” lesions. “Subtle” lesions frequently contained endometriosis and, at times, were the only positive lesions found in the pelvis. This study suggests that the lesion characteristics such as color do not reliably identify lesions with endometriosis.
Acknowledgements
We would like to thank the Reproductive Endocrinology Staff and Fellows, Alicia Armstrong, MD, Mark Leondires MD, William Catherino, MD, PhD, Rose Christian, MD, John Fratterelli, MD, Rob Gustofson, MD, Rhonda Hearns-Stokes, MD, Andy Levi, MD, Cindy Murdock, MD, Adrienne Neithardt, MD, Jason Parker, MD, and Mark Payson, MD for their support in the operating room; Research staff, Heidi Godoy, MD, Nadine Idress, MD, Nancy Kim, Vanessa Lopez, Sheila Mahoney, CNM, Kelly Morrissey, Katherine Plumb, Clariss Potlog-Nahari, MD, Stacey Spechler, and Victoria Shanmugan, MD for their help with specimens and data entry; Clinical Center nurses, Janice Wilson, RN, Carolyn Zimmer, RN and Donna Hardwick, RN for assistance with study visits.
Financial Support: This research was supported by the Intramural Research Program of the Reproductive Biology and Medicine Branch of the NICHD and the Clinical Center of the National Institutes of Health Presented at the American Society of Reproductive Medicine, Annual Meeting, Montreal, Canada, October 15−19, 2005.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Capsule: Endometriosis presents in different sizes, colors, and locations. We have characterized the presentation of endometriosis as an aid to making a surgical diagnosis.
References
- 1.Kennedy S, Bergqvist A, Chapron C, D'Hooghe T, Dunselman G, Greb R, et al. ESHRE guideline for the diagnosis and treatment of endometriosis. Hum Reprod. 2005;20:2698–704. doi: 10.1093/humrep/dei135. [DOI] [PubMed] [Google Scholar]
- 2.Stratton P, Winkel CA, Sinaii N, Merino MJ, Zimmer C, Nieman LK. Location, color, size, depth, and volume may predict endometriosis in lesions resected at surgery. Fertil Steril. 2002;78:743–9. doi: 10.1016/s0015-0282(02)03337-x. [DOI] [PubMed] [Google Scholar]
- 3.Nisolle M, Donnez J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil Steril. 1997;68:585–96. doi: 10.1016/s0015-0282(97)00191-x. [DOI] [PubMed] [Google Scholar]
- 4.Martin DC. Endometriosis: correlation between histologic and visual findings at laparoscopy. Am J Obstet Gynecol. 2003;188:1663. doi: 10.1067/mob.2003.426. author reply −4. [DOI] [PubMed] [Google Scholar]
- 5.Walter AJ, Hentz JG, Magtibay PM, Cornella JL, Magrina JF. Endometriosis: correlation between histologic and visual findings at laparoscopy. Am J Obstet Gynecol. 2001;184:1407–11. doi: 10.1067/mob.2001.115747. discussion 11−3. [DOI] [PubMed] [Google Scholar]
- 6.Stripling MC, Martin DC, Chatman DL, Zwaag RV, Poston WM. Subtle appearance of pelvic endometriosis. Fertil Steril. 1988;49:427–31. doi: 10.1016/s0015-0282(16)59767-2. [DOI] [PubMed] [Google Scholar]
- 7.Wykes CB, Clark TJ, Khan KS. Accuracy of laparoscopy in the diagnosis of endometriosis: a systematic quantitative review. Br J Obstet Gynaecol. 2004;111:1204–12. doi: 10.1111/j.1471-0528.2004.00433.x. [DOI] [PubMed] [Google Scholar]
- 8.Wolfler MM, Nagele F, Kolbus A, Seidl S, Schneider B, Huber JC, et al. A predictive model for endometriosis. Hum Reprod. 2005;20:1702–8. doi: 10.1093/humrep/deh796. [DOI] [PubMed] [Google Scholar]
- 9.Stratton P, Winkel C, Premkumar A, Chow C, Wilson J, Hearns-Stokes R, et al. Diagnostic accuracy of laparoscopy, magnetic resonance imaging, and histopathologic examination for the detection of endometriosis. Fertil Steril. 2003;79:1078–85. doi: 10.1016/s0015-0282(03)00155-9. [DOI] [PubMed] [Google Scholar]
- 10.Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004;160:784–96. doi: 10.1093/aje/kwh275. [DOI] [PubMed] [Google Scholar]
- 11.Missmer SA, Cramer DW. The epidemiology of endometriosis. Obstet Gynecol Clin North Am. 2003;30:1–19, vii. doi: 10.1016/s0889-8545(02)00050-5. [DOI] [PubMed] [Google Scholar]
- 12.Kinkel K, Frei KA, Balleyguier C, Chapron C. Diagnosis of endometriosis with imaging: a review. Eur Radiol. 2006;16:285–98. doi: 10.1007/s00330-005-2882-y. [DOI] [PubMed] [Google Scholar]
- 13.Revised American Society for Reproductive Medicine classification of endometriosis: 1996. Fertil Steril. 1997;67:817–21. doi: 10.1016/s0015-0282(97)81391-x. [DOI] [PubMed] [Google Scholar]
- 14.Potlog-Nahari C, Feldman AL, Stratton P, Koziol DE, Segars J, Merino MJ, et al. CD10 immunohistochemical staining enhances the histological detection of endometriosis. Fertil Steril. 2004;82:86–92. doi: 10.1016/j.fertnstert.2003.11.059. [DOI] [PubMed] [Google Scholar]
- 15.Calhaz-Jorge C, Mol BW, Nunes J, Costa AP. Clinical predictive factors for endometriosis in a Portuguese infertile population. Hum Reprod. 2004;19:2126–31. doi: 10.1093/humrep/deh374. [DOI] [PubMed] [Google Scholar]
- 16.Chapron C, Barakat H, Fritel X, Dubuisson JB, Breart G, Fauconnier A. Presurgical diagnosis of posterior deep infiltrating endometriosis based on a standardized questionnaire. Hum Reprod. 2005;20:507–13. doi: 10.1093/humrep/deh627. [DOI] [PubMed] [Google Scholar]


