Abstract
Objective
The Diabetes Prevention Program (DPP) showed that intensive lifestyle intervention reduced the risk of diabetes by 58%. This paper examines demographic, psychosocial, and behavioral factors related to achieving weight loss and physical activity goals in the DPP lifestyle participants.
Research Methods and Procedures
Lifestyle participants (n = 1079; mean age = 50.6, BMI = 33.9, 68% female, and 46% from minority groups) had goals of 7% weight loss and 150 min/wk of physical activity. Goal achievement was assessed at the end of the 16-session core curriculum (approximately week 24) and the final intervention visit (mean = 3.2 years) as a function of demographic, psychosocial, and behavioral variables.
Results
Forty-nine percent met the weight loss goal and 74% met the activity goal initially, while 37% and 67%, respectively, met these goals long-term. Men and those with lower initial BMI were more likely to meet activity but not weight loss goals. Hispanic, Asian, and Native Americans were more likely to meet the long-term activity goals, and whites were more likely to meet the initial weight loss goal. In multivariate analyses, meeting the long-term weight loss goal and both activity goals increased with age, while psychosocial and depression measures were unrelated to goal achievement. Dietary self-monitoring was positively related to meeting both weight loss and activity goals, and meeting the activity goal was positively related to meeting the weight loss goal. Participants who met initial goals were 1.5 to 3.0 times more likely to meet these goals long-term.
Discussion
Success at meeting the weight loss and activity goals increased with age. Initial success predicted long-term success. Self-monitoring and meeting activity goals were related to achieving and sustaining weight loss.
Keywords: weight loss, physical activity, prevention, diabetes, overweight
Introduction
Type 2 diabetes affects ∼8% of adults in the United States (1). Several recent studies have shown that lifestyle intervention can reduce the risk of developing diabetes in those at high risk (2–4). In the Diabetes Prevention Program (DPP),1 lifestyle intervention was effective in reducing the risk of diabetes by 58% (2). The benefits of lifestyle intervention were observed in both sexes and in all age, BMI, and racial and ethnic groups studied in the DPP.
The DPP lifestyle intervention focused on two of the modifiable risk factors for diabetes, sedentary lifestyle and overweight. All participants in the intensive lifestyle arm of DPP were given the goal of losing 7% of their body weight and achieving at least 150 min/wk of moderate intensity physical activity. The present paper examines demographic, psychosocial, and behavioral factors that were related to success at achieving these two goals. The study extends previous research on predictors of success in lifestyle intervention by using a larger, more diverse study population and examining success at achieving these goals both short-term (approximately week 24) and after a mean of 3.2 years of intervention.
Research Methods and Procedures
The DPP was a randomized clinical trial involving 3234 persons at 27 centers who were at high risk for developing diabetes. These participants were randomly assigned to standard lifestyle recommendations plus placebo or metformin or to intensive lifestyle intervention. The methods (5) and results (2) of the trial have been reported previously. The present manuscript focuses only on the 1079 participants who were randomly assigned to the intensive lifestyle intervention, using the completed DPP database as of July 31, 2001, immediately preceding the announcement of study results.
Participants
Eligibility criteria for DPP included an age of at least 25 years, BMI of 24 kg/m2 or greater (22 kg/m2 or higher in Asians), a fasting plasma glucose of 95 to 125 mg/dL (≤125 mg/dL in Native Americans) and a plasma glucose value of 140 to 199 mg/dL 2 hours after a 75-gram glucose load. All participants provided written informed consent before entering the study.
Intensive Lifestyle Intervention
The rationale and procedures used in the intensive life-style intervention have been described previously (6). This was a goal-based intervention; all participants at all centers were given the goal of losing 7% of their baseline body weight and achieving at least 150 min/wk of physical activity, using activities similar in intensity to brisk walking. These goals were selected because they appeared achievable and likely to reduce the risk of diabetes (6). Participants were assigned an individual case manager who worked with them throughout the trial. Initially, participants met with their case manager 16 times over the first 6 months of the program and completed a core curriculum. The core curriculum, which was the most structured phase of the intervention, introduced basic skills related to nutrition, exercise, and behavior change. Subsequently, participants were expected to be seen in person at least once every 2 months. These follow-up contacts occurred either at an individual session or at group classes; group classes were offered three times per year, with each class lasting 4 to 6 weeks.
The intensive lifestyle intervention stressed brisk walking as the means to achieving the activity goal, although other activities of similar intensity (aerobics, dance, bicycle riding, skating, swimming) could also be applied to the goal. (No more than 75 min/wk of strength training could be applied to the goal.) Participants were encouraged to increase their activity slowly and to exercise at least three times per week for at least 10 minutes per session. Although most participants completed their activity on their own, two supervised exercise classes were offered at all clinics each week. Participants at high risk for adverse events related to underlying coronary artery disease were given an exercise tolerance test before starting the activity intervention.
Physical activity was seen as a potentially important independent approach to preventing diabetes but also as a means to achieving and maintaining the weight loss goal in combination with dietary restriction. A low-fat (<25% fat) intake was recommended; if reducing fat did not produce weight loss to goal, calorie restriction was also recommended. Participants weighing 120 to 174 lb (54 to 78 kg) at baseline were instructed to follow a 1200-kcal/d diet (33 grams fat); participants weighing 175 to 219 lb (79 to 99 kg) were instructed to follow a 1500-kcal/d diet (42 grams fat); those 220 to 249 lb (100 to 113 kg) were instructed to follow an 1800-kcal/d diet (50 grams fat); and those over 250 lb (114 kg) were instructed to follow a 2000-kcal/d diet (55 grams fat).
Outcome Measures
Participants were instructed to self-monitor minutes of physical activity and fat grams consumed every day during the core curriculum and then 1 wk/mo over the remainder of the trial. These self-monitoring records and measures of body weight taken at each intervention visit were used to assess success at achieving the intervention goals. Participants were sometimes missing values for weight, fat grams, and physical activity for a variety of reasons, including a lack of a scale for occasional visits conducted outside the usual clinic or lack of self-monitoring information. These participants were excluded from analyses where these values were required.
Statistical Analyses
Analyses focused on the percentage of participants who were successful at achieving the 150-minute activity goal and the 7% weight loss goal at the end of the core curriculum and at the final postcore intervention visit (before the time of early termination of the study). Χ2 statistics were used to compare goal achievement as a function of age at randomization (<45 years, 45 to 59 years, 60 to 64 years, and 65 years and older), ethnicity, BMI (<30 kg/m2, 30 to 34.9 kg/m2, and ≥35 kg/m2), and sex. Goal achievement was also assessed as a function of the following psychosocial variables: current employment status [employed full-or part-time, retired, other (student/homemakers/seasonally employed)]; income (refused, <$35,000, $35,000 to $75,000, ≥$75,000); number in household (1, 2 to 4, 5 or more); marital status (married or living together, other), and the Beck Depression Inventory Scale score (<11, ≥11) (7). Logistic regression models were used to determine which factors (including demographic, psychosocial, and depression scores) were independently related to goal achievement. Finally, to determine whether adherence to various aspects of the lifestyle intervention was interrelated, we included adherence to self-monitoring (defined by the number of dietary self-monitoring records completed during the first 6 months of the program and over the first 2 years of the program) in the prediction of success at achieving the activity and weight loss goals. For analyses predicting weight loss, we also included self-reported success at meeting the physical activity goal at the same time-point.
Analyses were completed in two ways: first, we computed goal achievement using participants who attended the visit and/or provided self-monitoring records. We then redid all analyses assuming that participants who did not attend visits and/or did not turn in self-monitoring records had not met the goal. This latter approach reduced the actual percentage of participants achieving the goals, but the relationships with demographic variables were basically unchanged. Thus, only the first approach has been presented in the results.
Results
The 1079 participants assigned to the intensive lifestyle intervention had a mean (± SD) age of 50.6 ± 11.3 years, 68% were women, and the mean BMI was 33.9 ± 6.8. As seen in Table 1, 46.3% of the participants were from minority groups. The majority were married or living with a partner (66%), and 73% were employed. Average score on the Beck Depression Inventory was in the normal range, and only 10% reported mild or higher levels (≥11) of depressive symptoms. Of the 1079 participants randomized to lifestyle intervention, 1076 (99.7%) completed at least the first session of the core curriculum, and 1024 (95%) completed the entire 16-session core curriculum. The median time to completion of the core curriculum was 24 weeks. Some participants started the postcore visits without completing the full core curriculum; thus, 1035 participants completed at least one postcore visit with the intervention case manager; the final postcore visit occurred after a median 3.25 years of intervention. Participants attended 23.6 ± 7.1 sessions during year 1 (mean ± SD), 12.5 ± 7.1 sessions in year 2, and a total of 50.3 ± 21.8 sessions over the entire trial. Self-monitoring records of dietary fat intake were completed on 11.3 ± 5.3 weeks (range 0 to 23) during the first 6 months of the program and on 20.4 ± 13.5 weeks (range 0 to 89) over the first 2 years.
Table 1.
Baseline characteristics of the intensive lifestyle intervention group
| Variable | Number | Mean±SD or % |
|---|---|---|
| Age (years) | 1079 | 50.6±11.3 |
| Women | 734 | 68.0% |
| Ethnic Group | ||
| White | 579 | 53.7% |
| African American | 204 | 18.9% |
| Hispanic | 178 | 8.6% |
| Native American | 61 | 5.7% |
| Asian/Pacific Islander | 57 | 5.3% |
| BMI (kg/m2) | 1079 | 33.9±6.8 |
| Employment status | ||
| Full or part time | 785 | 72.8% |
| Retired | 148 | 13.7% |
| Other | 146 | 13.5% |
| Marital status | ||
| Married or living together | 708 | 65.6% |
| Other | 371 | 34.4% |
| Household Income | ||
| <$35,000 | 348 | 32.3% |
| $35,000 to $75,000 | 424 | 39.3% |
| $75,000 | 224 | 20.8% |
| Refused | 83 | 7.7% |
| Number in household | 1079 | 2.9±1.6 |
| 1 | 85 | 17.2% |
| 2 to 4 | 745 | 69.0% |
| 5 or more | 149 | 13.8% |
| Beck Depression Inventory score | 1065 | 4.6±4.5 |
| % with BDI ≥ 11 | 106 | 10.2% |
Physical Activity
Intensive lifestyle participants reported completing an average of 224 ± 141 min/wk of physical activity at the end of the core curriculum (N = 936; 87%) and 227 ± 212 min/wk at the final intervention visit (N = 952; 88%). The goal of ≥150 min/wk of activity was achieved by 74% of participants at the end of the core curriculum and 67% at the final intervention visit. Success at achieving the exercise goal at the end of the core curriculum was strongly related to being successful at the final visit. Participants who achieved the activity goal at the end of the core curriculum were 1.5 times more likely to achieve the goal at the final intervention visit compared with those who did not initially achieve the goal (75% vs. 50%, p < 0.001).
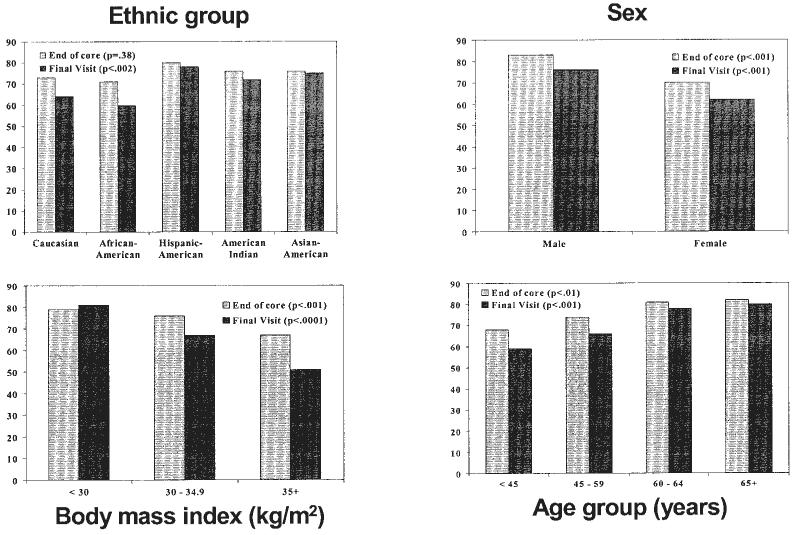
Figure 1 shows the percentage of participants who achieved the activity goal at the end of the core curriculum and at the final intervention visit according to baseline demographic characteristics. In univariate analyses, being male, having lower BMI, and being older were significantly associated with success at achieving the activity goal at both the end of the core curriculum and at the final visit. Ethnicity was significantly related to achieving the activity goal at the final intervention visit, with higher success rates in Hispanic Americans, Asian Americans, and Native Americans. Table 2 shows activity goal attainment as a function of the psychosocial variables we assessed. Retired participants were most likely to meet the exercise goal at both the end of the core curriculum and the final intervention visit. Similarly, income was related to achieving the activity goal at the final visit, with those refusingto report and those with incomes of less than $35,000 most likely to meet the goal. Marital status, number in household, and Beck Depression scores were unrelated to success at achieving the exercise goals at either end of core or the final intervention visit.
Figure 1.
Percentage of participants who achieved the exercise goal (<150 minutes per week) at the end of the core curriculum and at the final intervention visit by ethnic group, sex, baseline BMI, and baseline age.
Table 2.
Percentage of participants who met the physical activity and weight loss goal by psychosocial characteristic
| Exercise of ≥150 minutes* |
Weight loss of ≥7%* |
|||
|---|---|---|---|---|
| End of core curriculum |
Final intervention visit |
End of core curriculum |
Final intervention visit |
|
| Employment status | ||||
| Full or part time | 73% | 64% | 47% | 32% |
| Retired | 84% | 81% | 56% | 56% |
| Other | 73% | 66% | 54% | 45% |
| p = 0.02 | p = 0.0009 | p = 0.08 | p = <0.0001 | |
| (n = 936) | (n = 956) | (n = 1017) | (n = 1023) | |
| Marital Status | ||||
| Married/living together | 75% | 67% | 52% | 36% |
| Other | 73% | 66% | 44% | 39% |
| p = 0.61 | p = 0.82 | p = 0.02 | p = 0.35 | |
| (n = 936) | (n = 956) | (n = 1017) | (n = 1023) | |
| Income | ||||
| <$35,000 | 75% | 71% | 45% | 44% |
| $35,000 to $75,000 | 75% | 64% | 49% | 33% |
| ≥$75,000 | 73% | 63% | 55% | 33% |
| Refused | 75% | 71% | 53% | 34% |
| p = 0.96 | p = 0.04 | p = 0.15 | p = 0.0025 | |
| (n = 936) | (n = 956) | (n = 1017) | (n = 1023) | |
| Number in household | ||||
| 1 | 78% | 65% | 52% | 47% |
| 2 to 4 | 73% | 67% | 49% | 35% |
| 5 or more | 74% | 70% | 49% | 35% |
| p = 0.51 | p = 0.62 | p = 0.81 | p = 0.0078 | |
| (n = 926) | (n = 946) | (n = 1004) | (n = 1010) | |
| Depression | ||||
| 0 to 10 | 75% | 67% | 51% | 37% |
| 11 or more | 67% | 67% | 42% | 37% |
| p = 0.07 | p = 0.99 | p = 0.10 | p = 0.93 | |
| (n = 926) | (n = 946) | (n = 1004) | (n = 1010) | |
Participants without an intervention visit or with missing information on physical activity or weight at the end of the core curriculum or at the end of the intervention are excluded.
In multivariate analyses (Table 3), age, gender, and BMI remained significant predictors of success at achieving the activity goals at both the end of the core curriculum and at the final intervention visit, and ethnicity predicted goal achievement at the final visit. After adjusting for demographic factors (in particular, adjusting for age), the effect of employment status and income were no longer significant. Frequency of monitoring of dietary intake was also related to success at achieving the physical activity goal [odds ratio (OR) = 1.050 per one record increase in self-monitoring, p = 0.003 at the end of the core curriculum and OR = 1.024, p < 0.001 at the final intervention visit], suggesting that adherence to one aspect of the intervention was related to adherence to other aspects.
Table 3.
Logistic regression models predicting success at achieving the physical activity goal at the end of the core curriculum and at the final intervention visit
| At end of core‡ |
At final intervention visit‡ |
|||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% Confidence interval |
p value | OR | 95% Confidence interval |
p value | |||
| Age (per 5 years) | 1.117 | 1.018 | 1.225 | 0.0195 | 1.094 | 1.005 | 1.190 | 0.0381 |
| Sex (men vs. women) | 1.836 | 1.255 | 2.688 | 0.0018 | 1.572 | 1.117 | 2.214 | 0.0096 |
| BMI (per 1 kg/m2) | 0.964 | 0.941 | 0.987 | 0.0021 | 0.937 | 0.916 | 0.959 | <0.0001 |
| Ethnicity (vs. White) | 0.1813† | 0.0332† | ||||||
| Native American | 2.092 | 0.939 | 4.659 | 0.0710 | 1.499 | 0.754 | 2.981 | 0.2484 |
| Asian | 0.959 | 0.480 | 1.914 | 0.9051 | 1.194 | 0.611 | 2.336 | 0.6041 |
| Hispanic | 1.630 | 0.991 | 2.683 | 0.0544 | 1.980 | 1.234 | 3.175 | 0.0046 |
| African American | 1.024 | 0.672 | 1.559 | 0.9130 | 0.872 | 0.591 | 1.287 | 0.4907 |
| Number of self-monitoring fat intake records (per record)* |
1.050 | 1.016 | 1.084 | 0.0032 | 1.024 | 1.012 | 1.036 | <0.0001 |
Models adjusted for all variables listed as well as for: employment status, income, marital status, number living in the household, and Beck depression score, which were not nominally significant at p < 0.05 in the combined model.
Number of self-monitoring fat intake records during the first 6 months of the study (core) or during the first 2 years of the study (final intervention visit).
Overall p value for ethnicity.
Participants with missing information on self monitoring of fat intake or physical activity at the specified time points are excluded.
Weight Loss
At the first intervention session, participants weighed, on average, 94.5 ± 21.0 kg (mean ± SD), with weights ranging from 49.1 to 200.9 kg; the average BMI was 33.9 ± 6.8. Weight loss over the core curriculum (N = 1017; 95%) averaged 6.5 ± 4.7 kg or 6.9 ± 4.5% initial body weight. At the final intervention visit, participants (N = 1023; 95%) had maintained an average weight loss of 4.5 ± 7.6 kg or 4.9 ± 7.4% of initial body weight. The 7% weight loss goal was achieved by 49% of participants at the end of the core and by 37% at the final intervention visit. Early success at achieving the weight loss goal predicted later success. Participants who achieved the weight loss goal at the end of core were 3 times more likely to achieve the goal at study end (56% vs. 18%, p < 0.0001).
Figure 2 shows the percentage of participants who achieved the weight loss goal at both the end of the core curriculum and the final intervention visit in univariate analyses by BMI, age, gender, and ethnicity. Age was significantly related to success at achieving the weight loss goal at both the end of the core curriculum and the final intervention visit. Among those 65 years old or above, 60% met the 7% weight loss goal at end of core, compared with 43% of those under 45 years old. Similarly, at the final visit, 63% of those 65 years and older met the weight loss goal compared with 27% of those <45 years of age. Ethnicity was significantly related to initial weight loss success, with whites more successful than other ethnic groups (57% at goal compared with 30% to 48% at goal, respectively). However, there were only small nonsignificant differences by ethnic group by the final intervention visit. Baseline BMI was unrelated to weight loss success initially, but by the final visit, those with a lower baseline BMI were significantly more likely to have achieved the 7% weight loss goal. Men were more likely than women to achieve the 7% weight loss goal at both the end of core and final visit. In univariate analyses, several of the psychosocial variables were also related to achieving the weight loss goal (Table 2); married individuals were more likely to meet the goal at the end of the core curriculum, and those with lower income, retired people, and those with only one person in the household were more likely to achieve the weight loss goal at the final visit.
Figure 2.
Percentage of participants who achieved the 7% weight loss goal at the end of core curriculum and at the final intervention visit, by ethnic group, sex, baseline BMI, and baseline age.
Adjusting for age removed most of the demographic and psychosocial effects described above. Using logistic regression models (Table 4), the only psychosocial or demographic variable related to initial success at achieving the weight loss goal was ethnicity; age and employment status remained significant at the final intervention visit. Employed (full- or part-time) participants were similar to retired individuals in their likelihood of achieving the weight loss goal at the final intervention visit but significantly less likely than participants who were classified as “not employed” (homemakers, seasonally employed, students; N = 146).
Table 4.
Logistic regression models predicting success at achieving the weight loss goal at the end of the core curriculum and at the final intervention visit
| At end of core‡ |
At final intervention visit‡ |
|||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% Confidence interval |
p value | OR | 95% Confidence interval |
p value | |||
| Age (per 5 years) | 1.052 | 0.970 | 1.141 | 0.2233 | 1.235 | 1.133 | 1.347 | <0.0001 |
| Sex (men vs. women) | 1.056 | 0.770 | 1.447 | 0.7363 | 1.215 | 0.872 | 1.693 | 0.2489 |
| BMI (per 1 kg/m2) | 1.011 | 0.988 | 1.034 | 0.3509 | 1.020 | 0.996 | 1.046 | 0.1063 |
| Ethnicity (vs. White) | 0.0011† | 0.1756† | ||||||
| Native American | 0.637 | 0.319 | 1.272 | 0.2012 | 0.661 | 0.323 | 1.352 | 0.2565 |
| Asian | 0.626 | 0.346 | 1.135 | 0.1230 | 0.924 | 0.490 | 1.741 | 0.8072 |
| Hispanic | 0.834 | 0.552 | 1.259 | 0.3871 | 0.802 | 0.515 | 1.249 | 0.3288 |
| African American | 0.443 | 0.300 | 0.653 | <0.0001 | 0.598 | 0.392 | 0.911 | 0.0167 |
| Employment Status (vs. full/ part time) |
0.2499† | 0.0156† | ||||||
| Retired | 1.161 | 0.716 | 1.882 | 0.5451 | 1.159 | 0.709 | 1.894 | 0.5564 |
| Other | 1.426 | 0.929 | 2.190 | 0.1047 | 1.938 | 1.235 | 3.041 | 0.0040 |
| Meeting exercise goal | 1.899 | 1.374 | 2.627 | 0.0001 | 4.107 | 2.860 | 5.897 | <0.0001 |
| Number of self monitoring fat records (per record)* |
1.083 | 1.050 | 1.116 | <0.0001 | 1.020 | 1.009 | 1.031 | 0.0005 |
Models adjusted for all variables listed as well as for: income, marital status, number living in the household, and Beck depression score, which were not nominally significant at p < 0.05 in the combined model.
Number of self-monitoring fat intake records during the first 6 months of the study (core) or during the first 2 years of the study (final intervention visit).
Overall p value for ethnicity or employment status.
Participants with missing information on weight or self-monitoring of fat intake or physical activity at the specified time points are excluded.
After adjusting for these variables, success at meeting the weight loss goal at the end of the core curriculum and at the final intervention visit was predicted by success at achieving the exercise goal (OR = 1.90, p = 0.0001 for end of core; OR = 4.11, p < 0.0001 at final visit) and the number of times fat grams were self-monitored (OR = 1.08 per one record increase, p < 0.0001 at end of core; OR = 1.02, p = 0.0005 at final visit).
Discussion
The 150 min/wk activity goal was achieved by three-quarters of DPP lifestyle participants at the end of the core curriculum and by two-thirds at the end of the study. The 7% weight loss goal was achieved by ∼49% of participants at the end of the core curriculum and by 37% at study end. In the present paper, we examined the demographic, psychosocial, and behavioral factors that distinguished between those who achieved these goals and those who did not.
Older age was a strong predictor of success at meeting the weight loss goal and the physical activity goal at both the end of the core curriculum and at the final intervention visit. Older individuals were also more likely to complete self-monitoring records and to report a lower percentage of calories from fat than younger individuals (data not shown). Thus, older participants were more likely to adhere to multiple components of the lifestyle intervention. Adjusting for age removed many of the other univariate effects. These findings may explain why older individuals had the greatest reduction in diabetes risk (2) and suggest that older individuals may be particularly good candidates for lifestyle interventions. In other lifestyle interventions focused specifically on the elderly, excellent outcomes have also been observed (8). The success of older individuals may derive from the fact that they have fewer competing demands and/or because they are more aware of the negative health consequences of diabetes and, thus, more motivated to make behavior changes. The converse is also true—younger individuals may have particular difficulty implementing life-style changes while employed and/or caring for children. Further research is needed to understand reasons for the age differences in adherence to lifestyle intervention. Similarly, it is important to develop more effective intervention approaches for younger individuals, perhaps using techniques such as the Internet to increase the convenience of treatment contact (9).
Other demographic variables related to achieving the activity goal in DPP included the following: men and thinner individuals were more likely to achieve the physical activity goal both initially and long-term, and Hispanic Americans and Native Americans were more likely to meet the activity goals. Epidemiological studies have shown that men and thinner individuals are more likely to be physically active (10), but very few studies have examined success at achieving physical activity goals within the context of a weight loss intervention.
Whites were more likely to achieve the weight loss goal at the end of core, but at study end, there were no significant differences in weight loss success among the ethnic groups. There were also no significant effects of gender, initial BMI, any of the socioeconomic variables (income, marital status, number of persons in the household), or depressive symptoms on success at achieving the weight loss goal after adjusting for other demographic factors. Employment status was related to success at achieving the weight loss goal long-term, but this difference is difficult to interpret because it was between employed or retired persons and a small “other” category (N = 146).
Previous studies of predictors of weight loss in lifestyle interventions have been limited by the relatively small sample sizes and homogeneity of the populations studied (11). Moreover, most of these studies have examined the association between baseline characteristics and absolute amount of weight loss, rather than success at achieving a weight loss goal. The most consistent predictor of absolute weight loss in these studies has been initial body weight, with heavier individuals losing more weight (12). Likewise, men have been found to have larger initial weight loss, but this difference often disappears after adjusting for initial body weight (13); gender differences are typically not observed at follow-up. Age, marital status, and employment have not been related to weight loss outcome (12). The failure to find an effect of age on weight loss outcome in these prior studies, compared with the significant effect of age noted in DPP, may be due to differences in sample size and the range of ages of the participants.
Several prior studies have observed smaller weight losses in African Americans than in whites. Kumanyika et al. (14) reported recently that African Americans achieved less weight loss than whites initially but maintained their weight loss better, so that at follow-up weight loss was similar in the two groups. The present study suggests that a similar phenomenon may occur in other minority ethnic groups. In DPP, an effort was made to develop culturally sensitive materials; in addition, the case management approach allowed for tailoring of the intervention to the individual participant. These strategies may have helped to achieve similar long-term weight loss outcomes across the diverse populations studied.
Depressive symptoms were unrelated to success at achieving the activity or weight loss goals in DPP. This may result, in part, from the low levels of depressive symptoms in our participants and the paucity of individuals with clinical depression. Prior behavioral weight loss studies have also failed to show a relationship between baseline depressive symptoms and weight loss, although depression has, in some cases, been related to the risk of dropping out of the program (11,12).
The present analyses suggest important interrelationships among the behaviors prescribed in lifestyle intervention. For example, frequency of dietary self-monitoring was related to success at achieving both the physical activity goal and the weight loss goal. Likewise, success at achieving the activity goal was related to success at achieving the weight loss goal. Thus, there appears to be a clustering of behavior changes, with participants who adhere to one aspect of the lifestyle regimen more likely to adhere to other aspects (15,16). This clustering of behavior changes may help to maximize the initially positive results, but it could also explain the tendency to regain weight over time if participants who stop adhering to one behavior stop adhering to others.
Finally, this study suggests that getting patients off to a good start is critical for long-term success. Both for weight loss and physical activity, success at achieving the goal at end of core was strongly related to the probability of success at study end. This evidence supports the behavioral approach of incorporating frequent contact and more aggressive approaches at the start of treatment programs (17–19).
Strengths of the study include the large sample size, the diversity of the participants, the standardization of the intervention across a large number of clinical sites, and the extended length of treatment intervention. Several limitations of this study should be noted. The physical activity data are based on self-report and, thus, may overestimate physical activity (20). This bias may have been increased by the fact that self-monitoring records were turned in to the lifestyle coaches who used this information as the basis for counseling the participant. The intervention had goals for physical activity and weight loss; changes in dietary intake were not considered as goals but rather as a means to achieve the weight loss goal. Moreover, the number of fat grams recommended per day was individualized based on the participant’s body weight, and calorie levels were prescribed as needed to produce weight loss. For these reasons, and because adherence to dietary monitoring decreased over time, we have not considered dietary data in these analyses.
In summary, the DPP intensive lifestyle intervention was very effective in changing weight and physical activity. Although one might expect that older individuals would have more difficulty changing their behaviors, our results indicate that older participants were particularly successful at achieving both the weight and physical activity goals of DPP and had the greatest reduction in diabetes incidence (2). Other variables including employment, marital status, income, and depressive symptoms were unrelated to achieving either the weight or activity goals. We found that behavior changes tended to cluster, with participants who reported success at achieving one behavioral goal frequently having success at others. Likewise, initial success predicted longer term success; thus, clinicians should aim to have participants achieve the intervention goals by the end of the initial phase of intervention.
Acknowledgments
We thank the participants of the DPP for their commitment and dedication. Funding was provided by the NIH through the National Institute of Diabetes and Digestive and Kidney Diseases, the Office of Research on Minority Health, the National Institute of Child Health and Human Development, the National Institute on Aging, the Indian Health Service, the Centers for Disease Control and Prevention, and the American Diabetes Association. Two pharmaceutical companies, Bristol-Myers Squibb and Parke-Davis, contributed support. The General Clinical Research Center Program, National Center for Research Resources, supported many of the clinical centers. Support to the clinical centers and the Coordinating Center was provided by the National Institute of Diabetes and Digestive and Kidney Diseases through a Cooperative Agreement, except for the Southwestern American Indian Centers, which were supported directly by the National Institute of Diabetes and Digestive and Kidney Diseases and the Indian Health Service. Members of the writing group were: Rena R. Wing (Cochair), Richard F. Hamman (Cochair), George A. Bray, Linda Delahanty, Sharon L. Edelstein, James O. Hill, Edward S. Horton, Mary A. Hoskin, Andrea Kriska, John Lachin, Elizabeth J. Mayer-Davis, Xavier Pi-Sunyer, Judith G. Regensteiner, Beth Venditti, and Judith Wylie-Rosett. A complete list of all Centers, investigators, and staff can be found in reference 2.
The costs of publication of this article were defrayed, in part, by the payment of page charges. This article must, therefore, be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Footnotes
- DPP
- Diabetes Prevention Program
- OR
- odds ratio
References
- 1.Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance: U.S. adults. Diabetes Care. 1998;21:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 2.Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or Metformin. New Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pan XR, Li GW, Hu YH, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. Diabetes Care. 1997;20:537–44. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- 4.Toumilehto JL, Eriksson JG, Valle TT, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. New Engl J Med. 2001;344:1343–92. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]
- 5.Diabetes Prevention Program Research Group Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care. 1999;22:623–34. doi: 10.2337/diacare.22.4.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Diabetes Prevention Program Research Group The Diabetes Prevention Program: description of the lifestyle intervention. Diabetes Care. 2002;25:2165–71. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beck AT, Beck RW. Screening depressed subjects in family practice: a rapid technique. Postgrad Med. 1972;52:81–5. doi: 10.1080/00325481.1972.11713319. [DOI] [PubMed] [Google Scholar]
- 8.Whelton PK, Appel LJ, Espeland MA, et al. Sodium reduction and weight loss in the treatment of hypertension in older persons: a randomized controlled trial of nonpharmacologic interventions in the elderly (TONE) JAMA. 1998;279:839–46. doi: 10.1001/jama.279.11.839. [DOI] [PubMed] [Google Scholar]
- 9.Tate DF, Wing RR, Winett RA. Using Internet technology to deliver a behavioral weight loss program. JAMA. 2001;285:1172–7. doi: 10.1001/jama.285.9.1172. [DOI] [PubMed] [Google Scholar]
- 10.Dishman RK. Determinants of participation in physical activity. In: Bouchard C, Shephard RJ, Stephens T, Sutton JR, McPherson BD, editors. Exercise, Fitness and Health. Human Kinetics; Champaign, IL: 1990. pp. 75–102. [Google Scholar]
- 11.Wadden TA, Foster GD, Wang J, et al. Clinical correlates of short and long-term weight loss. Am J Clin Nutr. 1992;56:274–7S. doi: 10.1093/ajcn/56.1.271S. [DOI] [PubMed] [Google Scholar]
- 12.Wing RR, Phelan S. Strategies to improve outcomes and predictors of success. In: Eckel RH, editor. Obesity: Mechanisms and Clinical Management. Lippincott, Williams, and Wilkins; Philadelphia, PA: 2003. pp. 415–35. [Google Scholar]
- 13.French SA, Jeffery RW, Wing RR. Sex differences among participants in a weight-control program. Addictive Behav. 1994;19:147–58. doi: 10.1016/0306-4603(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 14.Kumanyika S, Espeland MA, Bahnson JL, et al. Ethnic comparison of weight loss in the trial of nonpharmacologic interventions in the elderly. Obes Res. 2002;10:96–106. doi: 10.1038/oby.2002.16. [DOI] [PubMed] [Google Scholar]
- 15.Jakicic J, Wing RR, Winters-Hart C. Relationship of physical activity to eating behaviors and weight loss in women. Med Sci Sports Exerc. 2002;34:1653–9. doi: 10.1097/00005768-200210000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Wadden TA, Letizia KA. Predictors of attrition and weight loss in patients treated by moderate and severe caloric restriction. In: Wadden TA, VanItallie TB, editors. Treatment of the Seriously Obese Patient. The Guilford Press; New York: 1992. pp. 383–410. [Google Scholar]
- 17.Jeffery RW, Wing RR, Mayer RR. Are smaller weight losses or more achievable weight loss goals better in the long term for obese patients? J Consult Clin Psychol. 1998;66:641–5. doi: 10.1037//0022-006x.66.4.641. [DOI] [PubMed] [Google Scholar]
- 18.Wing RR. Behavioral approaches to the treatment of obesity. In: Bray G, Bouchard C, James P, editors. Handbook of Obesity. Marcel Dekker, Inc.; New York: 1998. pp. 855–73. [Google Scholar]
- 19.Wadden TA, Vogt RA, Andersen RE, et al. Exercise in the treatment of obesity: effects of four interventions on body composition, resting energy expenditure, appetite, and mood. J Consult Clin Psychol. 1997;65:269–77. doi: 10.1037//0022-006x.65.2.269. [DOI] [PubMed] [Google Scholar]
- 20.Lichtman SW, Pisarska K, Berman ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327:1893–8. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]