Abstract
We modified the posterior approach by preserving the external rotator muscles to enhance joint stability after primary THA. We asked whether this modified posterior approach would have a lower dislocation rate than the conventional posterior approach, with and without a repair of external rotator muscles. We retrospectively divided 557 patients (670 hips) who had undergone primary THA into three groups based on how the external rotator muscles had been treated during surgery: (1) not repaired after sectioning, (2) repaired after sectioning, or (3) not sectioned and preserved. The minimum followup was 1 year. In the group with preserved external rotator muscles, we observed no dislocations; in comparison, the dislocation rates for the repaired rotator group and the no-repair group were 3.9% and 5.3%, respectively. This modified posterior approach, which preserves the short external rotator muscles, seemed effective in preventing early dislocation after primary THA.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
High postoperative dislocation rates (0.5%–9.5%) [7, 9, 16, 21] continue to be a major concern for both surgeons and patients even though the posterior approach for THA has numerous advantages, including low incidence of heterotrophic ossification [2, 11], decreased surgery time [5, 13], and minimal blood loss [5, 13, 15].
In hopes of preventing dislocation, numerous authors have reported the benefits of repairing the short external rotator muscle and capsule [7, 14, 19, 20, 22, 23, 25]. Nonetheless, one study had an exceptionally high dislocation rate of 9.5%, even after the piriformis tendon and both obturator tendons were repaired [21]. Stähelin et al. [17, 18] reported a high failure rate (75%) of repaired external rotators, suggesting the short external rotator muscles repaired during THA are not reliably sufficient to resist the forces that occur during the healing process. Given the conflicting conclusions in the literature, it is not clear if the stability of the merely repaired external rotator muscles are enhanced enough to reduce the dislocation rate.
Therefore, we modified the conventional posterior approach by preserving the external rotator muscles to enhance joint stability after THA and named this surgical approach the external rotator preservation (ERP) procedure.
We asked whether the ERP procedure would reduce the dislocation rate after primary THA compared to the conventional posterior approach, with or without repairing external rotator muscles in terms of dislocation rates, patient variables, prosthesis variables, and surgery variables.
Materials and Methods
We retrospectively reviewed 658 selected patients (769 hips) who underwent primary THA performed by the same surgeon (YSK) between August 1997 and May 2005. After excluding the patients with specific conditions that could possibly affect hip stability after THA, 557 patients (670 hips) remained and were divided into three groups based on how their external rotator muscles were treated during THA (Table 1). All data for this study were retrieved from our institution’s database; we did not see or contact patients specifically for this study.
Table 1.
Patient data
| Variable | The ERP group | The repair group | The no-repair group | p Value |
|---|---|---|---|---|
| Period in which primary THA was performed | August 2003 to May 2005 | May 2000 to July 2003 | August 1997 to April 2000 | |
| Number of patients (number of hips) | 196 (220) | 243 (282) | 118 (168) | |
| Age (years)* | 45.6 ± 14.6 | 47.6 ± 13.8 | 49.2 ± 15.1 | 0.474 |
| Gender (male:female) | 124:72 | 149:94 | 75:43 | 0.493 |
| Weight (kg)* | 64.1 ± 11.9 | 63.7 ± 12.7 | 62.4 ± 12.4 | 0.682 |
| Body mass index (kg/m2)* | 24.9 ± 8.5 | 23.9 ± 8.2 | 24.1 ± 7.9 | 0.648 |
| Preoperative diagnosis (number of hips) | ONFH (182); OA (26); other (12) | ONFH (199); OA (62); other (21) | ONFH (119); OA (42); other (7) | |
| Prosthesis† (number of hips) | Corail (94); Summit (66); VerSys (34); CLS (26) | VerSys (117); AML (65); other (21) | Mallory/Head (63); Omnifit (41); Centralign (22); other (42) |
*Mean ± standard deviation; †AML® Total Hip System (DePuy Orthopaedics, Inc, Indianapolis, IN); Centralign® (Zimmer, Inc, Warsaw, IN); CLS® (Centerpulse™, Bern, Switzerland); Corail® Total Hip System (DePuy); Mallory-Head® Hip System (Biomet Inc, Warsaw, IN); Omnifit® (Stryker Orthopaedics, Kalamazoo, MI); Summit™ Tapered Hip System (DePuy); VerSys® (Zimmer); ERP = external rotator preservation; OA = osteoarthritis; ONFH = osteonecrosis of the femoral head.
Between August 1997 and April 2000, THAs were performed in which the posterior capsule and short external rotator were excised and not repaired in 118 patients (168 hips) (no-repair group). Between May 2000 and July 2003, THAs were performed in which the detached short external rotators were reattached to the posterior border of the greater trochanter with No. 2 Ethibond™ sutures (Ethicon, Inc, Piscataway, NJ) in 243 patients (282 hips) (repair group). Between August 2003 and May 2005, THAs were performed using the modified posterior approach by preserving the external rotator muscles in 196 patients (220 hips) (ERP group). A power analysis (alpha = 0.05, n = 670) was performed to determine if the sample size was appropriate for the analysis (chi-square test) of the dislocation rate of each group, resulting in p = 0.8448. We compared the three groups with respect to dislocation rate, age, gender, weight, body mass index, operation time, postoperative blood loss, cup anteversion, cup inclination, and preoperative and 1-year postoperative Harris hip scores [3]. The minimum followup was 1 year (mean, 1.9 years; range, 1–2.8 years) in the ERP group, 2.9 years (mean, 4.2 years; range, 2.9–6 years) in the repair group, and 6 years (mean, 7.5 years; range, 6–8.8 years) in the no-repair group.
In the ERP group, there were 124 men and 72 women with a mean age of 45.6 ± 14.6 years (range, 17–77 years) at the time of the arthroplasty. The mean body weight was 64.1 ± 11.9 kg (range, 43–89 kg), and the mean body mass index was 24.9 ± 8.5 (range, 12.1–67.5). In the repair group, there were 149 men and 94 women with a mean age of 47.6 ± 13.8 years (range, 21–79 years). The mean body weight was 63.7 ± 12.7 kg (range, 44–90 kg), and the mean body mass index was 23.9 ± 8.2 (range, 12.4–52.4). In the no-repair group, there were 75 men and 43 women with a mean age of 49.2 ± 15.1 years (range, 20–78 years). The mean body weight was 62.4 ± 12.4 kg (range, 42–87 kg), and the mean body mass index was 24.1 ± 7.9 (range, 13.1–55.3). The most common diagnosis in all groups was osteonecrosis of the femoral head: 82.7% in the ERP group, 70.5% in the repair group, and 70.8% in the no-repair group (Table 1). There were no differences in age, gender, weight, and body mass index between the three groups. The preoperative Harris hip scores [3] were higher (p = 0.019) in the ERP group than the repair group, but there was no difference in the preoperative Harris hip scores [3] between the ERP group and the no-repair group (50.1 ± 11.5 in the ERP group, 42.4 ± 12.5 in the repair group, and 46.7 ± 10.8 in the no-repair group).
In the no-repair group, all of the short external rotator muscles were sectioned, and the complete capsulectomy was performed. The short external rotator muscles were not repaired after the implantation of the acetabular and femoral components. In the repair group, all of the short external rotator muscles were detached at the bony insertion site, and the complete capsulectomy was performed. The short external rotator muscles were then reattached at the trochanteric insertion site with the use of No. 2 Ethibond suture after the implantation of the acetabular and femoral components.
In the ERP group, the short external rotator muscles were exposed using the conventional posterior approach. The piriformis, superior gemelli, and obturator internus were preserved, but the inferior gemelli and obturator externus were sectioned at the bony insertion site. By retracting the obturator internus proximally and the quadratus femoris distally, we exposed the posterior joint capsule (Fig. 1). At this point, the obturator internus was retracted proximally with a Hohmann retractor and gently to prevent tearing. The posterior part of the joint capsule was excised to the maximum extent possible, and then the hip was dislocated posteriorly. The neck was cut, about the width of a finger, above the top of the lesser trochanter. While placing the tip of a Hohmann retractor on the anterior wall of the acetabulum, the proximal femur was retracted anteriorly and with 70° to 80° of flexion, 20° of adduction, and 90° of internal rotation. Three additional retractors were positioned: beneath the transverse acetabular ligament, and in the corner of the anterosuperior and posterosuperior acetabulum to perform the complete capsulectomy (Fig. 2). This procedure allowed enough space for easy access of the acetabular reamer and acetabular component (Fig. 3). The preparation of the femur and insertion of instruments and femoral components were performed in a routine manner. After inserting the real components, the hip was examined for its adduction and internal rotation to see if the external rotators were intact and tensed enough. The prostheses used in the three groups were made by different manufacturers (Table 1), but all had a neck taper of 12/14 mm and a 28-mm ball head.
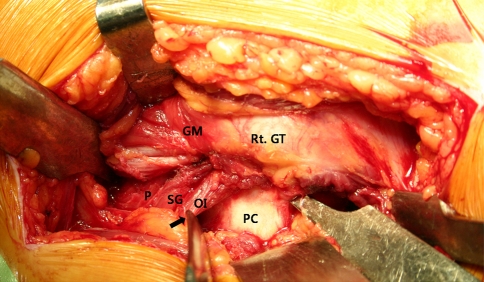
Fig. 1.
The obturator internus (OI), superior gemelli (SG), and piriformis (P) were retracted proximally with a Hohmann retractor (arrow), and the quadratus femoris muscle was retracted inferiorly to expose the posterior capsule (PC). Rt. GT = right greater trochanter; GM = gluteus medius.
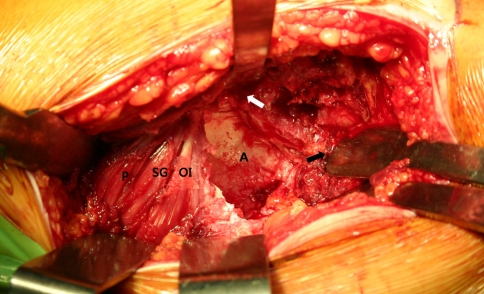
Fig. 2.
The acetabulum (A) is well-exposed after the complete capsulectomy. The tip of a Hohmann retractor is placed on the anterior wall of the acetabulum (white arrow); the proximal femur is retracted anteriorly (black arrow). The obturator internus (OI), superior gemelli (SG), and piriformis (P) are well-preserved.
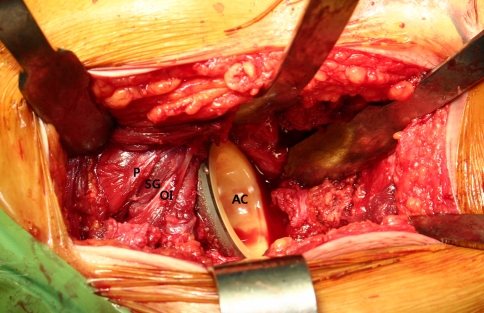
Fig. 3.
The acetabular component (AC) is successfully implanted without damaging the obturator internus (OI), superior gemelli (SG), and piriformis (P).
In the no-repair and repair groups the postoperative regimen was identical. Patients began walking on the first or second postoperative day with the assistance of a physical therapist with training in treating patients who have undergone joint arthroplasty. Patients were advised for the first 12 weeks after surgery to limit flexion to 90° and to avoid internal rotation while the hip was flexing. We instituted 6 weeks of protected weight bearing followed by full weight bearing. The postoperative rehabilitation program for the ERP group was specially designed to fit each patient’s individual needs. Patients were not restricted to a regimented postoperative clinical protocol, and some patients were even permitted to engage in maximum hip flexion of 120° and slight internal rotation while the hip was flexed. If both components were stably fixed to the bone, full weight bearing without any aids was permitted on the second postoperative day.
The dislocation rate within the first year after surgery was determined from the records. Harris hip scores [3] were evaluated preoperatively and at 1 year postoperatively for pain and function.
We (SYK, DHS, SKH) determined the cup position by goniometric measurements of the abduction and version angle. The inclination angle of the acetabular component was measured from the line connecting the acetabular teardrop to the line tangential to the acetabular component opening. Acetabular cup anteversion was determined using Widmer’s method [24]. We determined stem position by goniometric measurements of the angle subtended by the femoral shaft axis and the long axis of the femoral component on anteroposterior radiographs. Femoral component angulations between 3° varus and 3° valgus relative to the femoral shaft axis were considered well-aligned.
We compared the means of all numeric variables (age, weight, body mass index, operation time, postoperative blood loss, cup anteversion, cup inclination, dislocation rate, and preoperative and 1-year postoperative Harris hip scores) of the three different surgical techniques using one-way analysis of variance. The gender distribution and dislocation rate differences among groups were obtained using the chi-square test. In all analyses, differences between the three groups were considered significant at p < 0.05. Analysis was performed using the SPSS WIN 12.0 program (SPSS Inc, Chicago, IL).
Results
The ERP group had the lowest (p = 0.004) postoperative dislocation rate compared to the repair group and the no-repair group. There was no dislocation among 220 hips in the ERP group compared with 11 dislocations (three anterior; eight posterior) among 282 hips in the repair group and nine dislocations (one anterior; eight posterior) among 168 hips in the no-repair group (Table 2).
Table 2.
Comparison of posterior approaches according to the treatment of the external rotators
| Variable | The ERP group (A) | The repair group (B) | The no-repair group (C) | p Value | Duncan |
|---|---|---|---|---|---|
| Surgical factors | |||||
| Operation time (minutes)* | 91.1 ± 8 | 90.1 ± 11.6 | 81.2 ± 14.1 | < 0.001 | A,B > C |
| Postoperative blood loss (mL)* | 718.7 ± 258.6 | 745.8 ± 234 | 736.6 ± 209.1 | 0.465 | |
| Radiographic evaluation | |||||
| Cup anteversion (degrees)* | 11.5 ± 5.7 | 15.3 ± 5.5 | 15 ± 4.9 | < 0.001 | B,C > A |
| Cup inclination (degrees)* | 43.2 ± 3.5 | 42.2 ± 3.6 | 42.5 ± 3.7 | 0.013 | A > B |
| Stem malposition | 3 | 3 | 4 | ||
| Clinical evaluation | |||||
| Preoperative Harris hip scores* | 50.1 ± 11.5 | 42.4 ± 12.5 | 46.7 ± 10.8 | 0.019 | A > B |
| 1-year postoperative Harris hip scores* | 97 ± 2.9 | 94.9 ± 3.4 | 94.2 ± 3.2 | < 0.001 | A > B,C |
| Complications | |||||
| Dislocation rate (%)* | 0/220 (0) | 11/282 (3.9) | 9/168 (5.3) | 0.004 | |
| Infection | 0 | 1 | 0 | ||
| Nerve palsy | 0 | 1 | 2 | ||
*Mean ± standard deviation; ERP = external rotator preservation.
Among the 220 hips of the ERP group, the obturator internus was torn in six hips by the forceful retraction during surgery: five hips with the torn external obturator muscles but intact piriformis and superior gemelli and one hip with the bony avulsion of conjoined tendon at the insertion site of the trochanter.
The mean operative time was 91.1 ± 8 minutes in the ERP group, 90.1 ± 11.6 minutes in the repair group, and 81.2 ± 14.1 minutes in the no-repair group. The operation time was shorter in the no-repair group than in either the ERP group (p < 0.001) or the repair group (p < 0.001); however, there was no difference between the ERP group and the repair group. There was no difference in postoperative blood loss among the three groups.
The least (p < 0.001) mean cup anteversion occurred in the ERP group, followed by the repair group and the no-repair group (11.5° ± 5.7°, 15.3° ± 5.5°, and 15° ± 4.9°, respectively). We observed the greatest (p = 0.013) cup inclination in the ERP group, followed by the repair group and the no-repair group (mean 43.2° ± 3.5°, 42.2° ± 3.6°, 42.5° ± 3.7°, respectively).
The 1-year postoperative Harris hip scores were higher in the ERP group than in either the repair group (p < 0.001) or the no-repair group (p < 0.001) (97 ± 2.9, 94.9 ± 3.4, and 94.2 ± 3.2, respectively). We observed no difference in the postoperative Harris hip scores between the repair group and the no-repair group.
There was no infection or nerve palsy in the ERP group; however, there was one postoperative infection and one sciatic nerve palsy in the repair group and two nerve palsies in the no-repair group.
Discussion
To prevent dislocation after THA with the posterior approach, we had tried to repair the short external rotator muscles for many years. Because merely repairing was not enough to lower the dislocation rate, we developed a modified posterior approach that preserved the short external rotator muscles (ERP procedure). We performed this study to determine whether the ERP procedure could lower the dislocation rate from that of the conventional posterior approach, with or without repair of the short external rotator muscles.
We have noted several limitations to our study. First, our study design was not a concurrent randomized design but a sequential cohort design so it could potentially entail confounding variables such as different types of prostheses and implanting methods. Second, we did not measure pre and postoperative leg-length discrepancy, which could have been an important numeric variable for comparing the dislocation rates of each group; we did not take the soft tissue tension into consideration which could have been caused by the shortening or lengthening of the legs. Third, there was no fixed protocol for the rehabilitation for all groups; the differences in individual activities affecting dislocation rates were not considered.
In several clinical studies, lower dislocation rates (0.5%–2%) were reported when these soft tissues were repaired compared with when they were not repaired [7, 14, 19–23, 25]. The advantages of soft tissue repairs for postoperative stability after THA also were demonstrated in a mechanical study [10]. However, Stähelin et al. [18] recently have reported failures of repaired short external rotator muscles in 15 of 20 hips within 3 months of THA, suggesting the repair of capsular-enhanced short external rotator muscles after THA is not sufficient to allow it to reliably withstand the forces that occur during the process of healing. The early failure of repaired tendons is closely related to high dislocation rates [9, 21].
The results of the ERP procedure in terms of dislocation rate are better than those in the literature, in which the soft tissues were repaired during the conventional posterior approach. However, the dislocation rate of 3.9% in the repair group of our study was higher than the rates in other studies with repaired soft tissue. The Asian lifestyle uses greater flexion, internal rotation, and adduction after surgery for most patients, and perhaps contributed to the somewhat higher rate.
Posterior dislocation is thought by many to be caused by posterior capsulectomy, while skillful repairing of the capsule is believed to lower the dislocation rate [4, 14, 19, 23]. Our data is somewhat contrary to this notion since no dislocation occurred in the ERP group even though complete capsulectomy was performed in all cases. These results suggest the importance of the short external rotator rather than the capsule in preventing the dislocation.
Positioning of the acetabular component is an important risk factor for dislocation [1, 6, 8, 12]. Three of the 11 dislocated hips in the repair group and one of the nine dislocated hips in the no-repair group had anterior dislocations, which we suspect were caused by the large amount of anteversion intended to prevent posterior dislocation. Because the posterior capsulectomy was not completed in the initial stage of the surgical procedure, it was difficult to anteriorly retract the femur; therefore, we could not ensure enough anteversion of the acetabular component in the ERP group. Although the amount of cup anteversion in the ERP group (11.5° ± 5.7°) was less than that in the repair group (15.3° ± 5.5°) and in the no-repair group (15° ± 4.9°), no dislocations occurred in the ERP group. These data suggest if the external rotators can be preserved effectively to prevent posterior dislocation, excessive anteversion is unnecessary. The femoral components of all groups were inserted with a slight anteversion to fit the neck configuration, and the anteversion of the femoral components in each group would not have affected the dislocation.
Because our patients had a relatively low weight and body mass index, and therefore a smaller skeletal structure, the surgery was carried easily. However, in patients with a larger skeletal structure or obesity, it may be more difficult to effectively preserve the structures; for those patients, the procedure can be performed using the extended skin incision of the conventional posterior approach. Even with this modified posterior approach, it is difficult to perform in severely dysplastic, fused, or severely contracted hips, and the ERP procedure may have limited application in patients with primary osteoarthritis, osteonecrosis of the femoral head, or rheumatoid arthritis. In addition, there could be a limitation in implanting the cemented acetabular components accurately because of the difficulty in cement handling, but implanting the cemented femoral stem could be completed without difficulty. The ERP procedure can be performed by surgeons who are well acquainted with the posterior approach, but even for those, five to 10 cases are essential for the learning curve. There was no nerve paralysis in this study. However, there is a possibility of nerve paralysis if excessive Hohmann retraction is applied to this petite incision, which should be kept in mind.
Our data suggest preserving the external rotators reduces the dislocation rate compared to sectioning and repairing the external rotators and capsule. We recommend this approach to surgeons using the posterior approach hoping to reduce the dislocation rate.
Acknowledgments
We thank Katharine O’Moore-Klopf and Eun-Na Choe for providing editorial assistance.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B. Reducing the risk of dislocation after THA: the effect of orientation of the acetabular component. J Bone Joint Surg Br. 2005;87:762–769. [DOI] [PubMed]
- 2.Bischoff R, Dunlap J, Carpenter L, DeMouy E, Barrack R. Heterotopic ossification following uncemented THA: effect of the operative approach. J Arthroplasty. 1994;9:641–644. [DOI] [PubMed]
- 3.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 4.Hedley AK, Hendren DH, Mead LP. A posterior approach to the hip joint with complete posterior capsular and muscular repair. J Arthroplasty. 1990;5(Suppl):S57–S66. [DOI] [PubMed]
- 5.Hovelius L, Hussenius A, Thorling J. Posterior versus lateral approach for hip arthroplasty. Acta Orthop Scand. 1977;48:47–51. [DOI] [PubMed]
- 6.Komeno M, Hasegawa M, Sudo A, Uchida A. Computed tomographic evaluation of component position on dislocation after THA. Orthopedics. 2006;29:1104–1108. [DOI] [PubMed]
- 7.Kwon MS, Kuskowski M, Mulhall KJ, Macaulay W, Brown TE, Saleh KJ. Does surgical approach affect THA dislocation rates?. Clin Orthop Relat Res. 2006;447:34–38. [DOI] [PubMed]
- 8.Masaoka T, Yamamoto K, Shishido T, Katori Y, Mizoue T, Shirasu H, Nunoda D. Study of hip joint dislocation after THA. Int Orthop. 2006;30:26–30. [DOI] [PMC free article] [PubMed]
- 9.Masonis JL, Bourne RB. Surgical approach, abductor function, and THA dislocation. Clin Orthop Relat Res. 2002;405:46–53. [DOI] [PubMed]
- 10.Mihalko WM, Whiteside LA. Hip mechanics after posterior structure repair in THA. Clin Orthop Relat Res. 2004;420:194–198. [DOI] [PubMed]
- 11.Morrey BF, Adams RA, Cabanela ME. Comparison of heterotopic bone after anterolateral, transtrochanteric, and posterior approaches for THA. Clin Orthop Relat Res. 1984;188:160–167. [PubMed]
- 12.Nishii T, Sugano N, Miki H, Koyama T, Takao M, Yoshikawa H. Influence of component positions on dislocation: computed tomographic evaluations in a consecutive series of THA. J Arthroplasty. 2004;19:162–166. [DOI] [PubMed]
- 13.Pätiälä H, Lehto K, Rokkanen P, Paavolainen P. Posterior versus lateral approach for hip arthroplasty. Acta Orthop Scand. 1977;48:47–51. [DOI] [PubMed]
- 14.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res. 1998;355:224–228. [DOI] [PubMed]
- 15.Roberts JM, Fu FH, McClain EJ, Ferguson AB. A comparison of the posterolateral and anterolateral approaches to THA. Clin Orthop Relat Res. 1984;187:205–210. [PubMed]
- 16.Sierra RJ, Raposo JM, Trousdale RT, Cabanela ME. Dislocation of primary THA done through a posterolateral approach in the elderly. Clin Orthop Relat Res. 2005;441:262–267. [DOI] [PubMed]
- 17.Stähelin T, Drittenbass L, Hersche O, Miehlke W, Munzinger U. Failure of capsular enhanced short external rotator repair after total hip replacement. Clin Orthop Relat Res. 2004;420:199–204. [DOI] [PubMed]
- 18.Stähelin T, Vienne P, Hersche O. Failure of reinserted short external rotator muscles after THA. J Arthroplasty. 2002;17:604–607. [DOI] [PubMed]
- 19.Suh KT, Park BG, Choi YJ. A posterior approach to primary THA with soft tissue repair. Clin Orthop Relat Res. 2004;418:162–167. [DOI] [PubMed]
- 20.van Stralen GM, Struben PJ, van Loon CJ. The incidence of dislocation after primary THA using posterior approach with posterior soft-tissue repair. Arch Orthop Trauma Surg. 2003;123:219–222. [DOI] [PubMed]
- 21.Vicar AJ, Coleman CR. A comparison of the anterolateral, transtrochanteric, and posterior surgical approaches in primary THA. Clin Orthop Relat Res. 1984;188:152–159. [PubMed]
- 22.Weeden SH, Paprosky WG, Bowling JW. The early dislocation rate in primary THA following the posterior approach with posterior soft-tissue repair. J Arthroplasty. 2003;18:709–713. [DOI] [PubMed]
- 23.White RE, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res. 2001;393:163–167. [DOI] [PubMed]
- 24.Widmer KH. A simplified method to determine acetabular cup anteversion from plain radiographs. J Arthroplasty. 2004;19:387–390. [DOI] [PubMed]
- 25.Yamaguchi T, Naito M, Asayama I, Kambe T, Fujisawa M, Ishiko T. The effect of posterolateral reconstruction on range of motion and muscle strength in THA. J Arthroplasty. 2003;18:347–351. [DOI] [PubMed]