Abstract
Femoroacetabular impingement may occur in patients with so-called acetabular retroversion, which is seen as the crossover sign on standard radiographs. We noticed when a crossover sign was present the ischial spine commonly projected into the pelvic cavity on an anteroposterior pelvic radiograph. To confirm this finding, we reviewed the anteroposterior pelvic radiographs of 1010 patients. Nonstandardized radiographs were excluded, leaving 149 radiographs (298 hips) for analysis. The crossover sign and the prominence of the ischial spine into the pelvis were recorded and measured. Interobserver and intraobserver variabilities were assessed. The presence of a prominent ischial spine projecting into the pelvis as diagnostic of acetabular retroversion had a sensitivity of 91% (95% confidence interval, 0.85%–0.95%), a specificity of 98% (0.94%–1.00%), a positive predictive value of 98% (0.94%–1.00%), and a negative predictive value of 92% (0.87%–0.96%). Greater prominence of the ischial spine was associated with a longer acetabular roof to crossover sign distance. The high correlation between the prominence of the ischial spine and the crossover sign shows retroversion is not just a periacetabular phenomenon. The affected inferior hemipelvis is retroverted entirely. Retroversion is not caused by a hypoplastic posterior wall or a prominence of the anterior wall only and this finding may influence management of acetabular disorders.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
In the middle 1960s and 1970s, Murray [11] and Stulberg et al. [15] described the association between abnormal hip anatomy and its possible etiologic role in the development of hip osteoarthritis (OA). These anomalies, so-called pistol grip or head tilt deformities, were recognized then, but the mechanism leading to OA was not described until two decades later [4, 8]. It now is recognized this anatomic abnormality likely results in cartilage degeneration [6] secondary to femoroacetabular impingement [16, 18]. Among the subtle anatomic abnormalities that have been linked to femoroacetabular impingement is that of acetabular retroversion and that of femoral head-neck offset discrepancies [6, 12, 13]. The former occurs when the acetabular opening is situated in a more posterolateral direction in the sagittal plane when compared with the normal anatomic anterolateral opening and the latter occurs most commonly when an aspheric extension of the femoral head occurs over the neck, most commonly over the anterolateral femoral head neck junction. These two anomalies escaped diagnosis for many years, mainly because of difficulty in observation on standard radiographs of the hip.
Even though the human hip has been studied radiographically for more than a century, it was not until the last decade that a radiographic sign, the crossover sign (COS), was described to identify retroversion from the standard anteroposterior (AP) radiograph [13]. The anterior and posterior walls in a normal hip meet at the lateral projection of the acetabular roof. When the anterior wall and posterior walls meet caudal to the roof, a crossover of the walls occurs and indicates the presence of acetabular retroversion (Fig. 1). In these hips, the normal anterolateral opening of the acetabulum faces more posterolaterally in the sagittal plane. In normal hips, the anteversion progresses in a spiral fashion from caudal to cranial. In retroverted sockets, despite seemingly normal anteversion caudally, there is less progression to anteversion at the center of the acetabulum, and then cranially there is negative acetabular version or what now is called cranial retroversion. The relationship between COS and retroversion was described by Jamali et al. [7] who confirmed COS indicates sectorial retroversion of the acetabulum and mostly affects the cranial portion but also can affect the entire acetabulum. They used a modified radiographic method to estimate radiographic anteversion. They defined cranial, central, and caudal anteversion on radiographs and correlated these with anatomic measurements made on the same bony pelvises. Central anteversion less than 10° correlated with a negative cranial anteversion, or in other words, retroversion. Central anteversion greater than 20° was associated with a positive value for cranial anteversion, and only one hip in their study was retroverted. The radiographic COS then was correlated with the anatomic measurements and found sensitive for detecting cranial retroversion less than 4°.
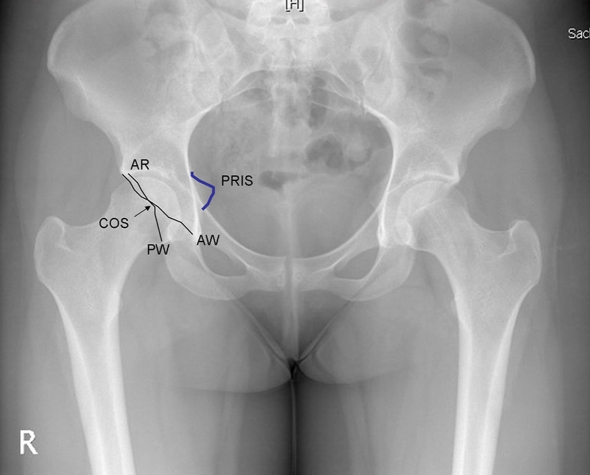
Fig. 1.
A standard AP radiograph of a patient with femoroacetabular impingement shows bilateral retroverted acetabula as evidenced by the COS, and prominence of the ischial spine on both sides (positive PRIS sign). In a normal hip, the ischial spine is almost never visible in the pelvic brim and most commonly lies lateral to the iliopectineal line. AR, acetabular roof; PW, posterior wall; AW, anterior wall.
Interpreting the AP pelvic radiographs, however, is difficult, as is perceiving the three-dimensional structure of the acetabulum in one view. Interpretation becomes even more difficult when these measurements depend on radiographic technique and quality. Quality is important, especially if the observer is not used to reviewing AP pelvic radiographs and the anterior and the posterior borders are not readily visible. An alternative method is needed.
The ischial spine is a pointed process that extends from the posterior border of the superior aspect of the ischium at the level of the lower border of the acetabulum. It gives attachment to the sacrospinous ligament. It is easily seen on standard AP radiographs as a triangular-shaped radiopaque structure that points medially from the pelvic brim toward the pelvic inlet. In clinical practice, we noticed this process often is more prominent in patients with acetabular retroversion and often is hidden behind the acetabulum in patients with normally anteverted acetabula.
To confirm the relationship between COS and the prominence of the ischial spine (PRIS) we posed the following objectives: (1) to ascertain whether the presence of the PRIS within the pelvic cavity correlates with the presence of a COS, indicative of retroversion, (2) to determine whether a longer PRIS is associated with a longer acetabular roof to COS distance, and (3) to assess the interobserver and intraobserver correlations between the COS and the PRIS.
Materials and Methods
We (FK, SSM) reviewed digitized AP pelvic radiographs of 1010 patients who sought treatment for a painful hip. Of these patients, 554 hips had a periacetabular osteotomy initially between 1986 and 2001, and 456 hips had initially a surgical hip dislocation for femoroacetabular impingement between 1996 and 2002. Radiographs that did not meet standardized criteria as described by Siebenrock et al. [14] were excluded. Briefly, the coccyx should point directly over the symphysis pubis, documenting absence of rotation. The distance between the sacrococcygeal joint is on average 47 mm in women and 32 mm in men, denoting a neutrally rotated pelvis. This corresponds to approximately 0 to 2 cm of distance between the symphysis and tip of the coccyx (Fig. 1). For this study, we included only radiographs in which the tip of the coccyx to the symphysis was between 0 to 20 mm to include the differences across gender and to include radiographs with neutral tilt only, as COS is highly dependent on this measurement. These criteria were introduced into clinical practice in 2000. Radiographs in which exposure of the film did not clearly show the outline of the acetabulum, particularly the anterior and posterior walls, the ischial spine, the sclerosis of the acetabular roof (sourcil), and the lateral edge of the acetabulum, were excluded [14]. This included hips that did not allow adequate view of bony landmarks because of a gonadal shield, gas in the pelvic outlet, or open triradiate cartilage or incomplete ossification of the acetabulum. Also, hips with previous fractures or surgery to the pelvis and grossly deformed hips as a result of high dislocation, avascular necrosis, or OA were excluded, as these tend to abnormally tilt or rotate the pelvis because of muscle contractures. Eight hundred sixty-one preoperative radiographs did not meet these criteria and were excluded.
This left 149 of the 1010 (14.7%) preoperative pelvic radiographs (298 hips) that met our criteria. One hundred twelve of the hips (37.6%) had not undergone any type of surgery, 113 (38%) had evidence of hip disease and had undergone a periacetabular osteotomy, and 73 (24.4%) had evidence of hip disease and had undergone a surgical hip dislocation (Table 1). One of us performed all the measurements (FK) after common agreement was attained regarding how retroversion would be measured and how the PRIS would be assessed. All measurements were made on both hips for each patient.
Table 1.
Comparison between procedure type and radiographic diagnosis
| Type of Procedure | Dysplasia | Normal | Perthes | Retroversion | Total |
|---|---|---|---|---|---|
| No surgery | 30 | 36 | 46 | 112 | |
| Surgical hip dislocation | 1 | 24 | 48 | 73 | |
| Periacetabular osteotomy | 93 | 2 | 3 | 15 | 113 |
| Total | 125 | 64 | 3 | 105 | 298 |
By purely radiographic criteria, 125 (41.9%) of 298 hips were classified as having anterolateral undercoverage, 106 (35.5%) had a retroverted acetabulum, 64 (21.5%) had a normal acetabulum, and three (1%) had post-Perthes deformity. The radiographic diagnosis was compared with the hip procedure (Table 1). Thirty hips that had not yet been surgically treated were dysplastic, 36 were normal, and 46 were retroverted. Approximately  of hips operated on for femoroacetabular impingement had a retroverted acetabulum, 80% of the hips that had a periacetabular osteotomy had classic dysplasia, and 15% had a retroverted acetabulum.
of hips operated on for femoroacetabular impingement had a retroverted acetabulum, 80% of the hips that had a periacetabular osteotomy had classic dysplasia, and 15% had a retroverted acetabulum.
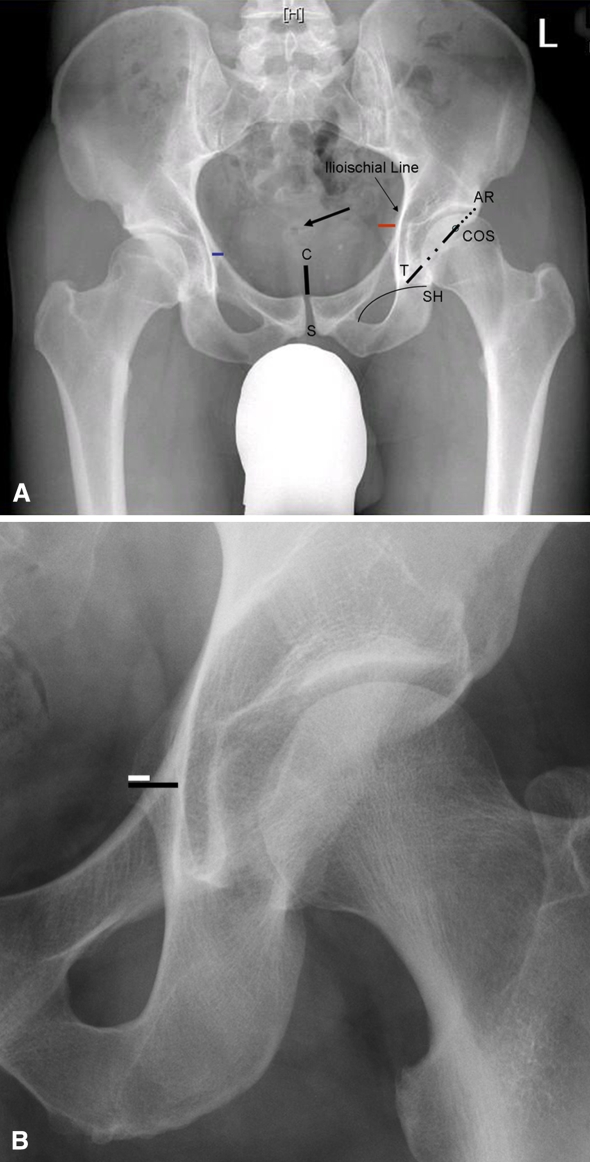
Several measurements were obtained from each radiograph (Fig. 2). We first measured the diameter of each femoral head and the acetabular length, as our radiographs were not standardized for magnification, and these measurements were used to calculate other parameters as described below. The PRIS was measured as the distance from the medial wall of the acetabulum to the tip of the ischial spine. Two measurements were performed. The first one measured the amount of ischial spine that was seen medially extending into the pelvic inlet (PRIS 1), and the second measured only the total width of the ischial spine even if its radiopaque shadow was situated behind the pelvic brim (PRIS 2). The anterior and posterior walls were observed and the occurrence of the COS as described by Reynolds et al. [13] was recorded for each hip. The point of the crossover between the anterior and posterior walls then was measured to the lateral edge of the acetabular roof to obtain a crossover to lateral roof distance. The large acetabular length and femoral head diameters were the result of the magnification factor on older radiographs. Because this magnification factor could affect the results of the length of the COS, we obtained the percentage of retroverted acetabulum by dividing crossover to lateral acetabular roof by the acetabular length.
Fig. 2A–B.
(A) A pelvic radiograph shows the measurements obtained: symphysis (S) to coccyx (C) distance (black continuous line); sacrococcygeal joint (black arrow); COS, where the anterior and posterior walls cross (open circle); length of acetabulum (dotted black line and noncontinuous black line) from the lateral acetabular roof (AR) to the point that intersects the teardrop (T) with Shenton’s line (SH); PRIS 1 (blue line), the amount of ischial spine that was seen medially extending into the pelvic inlet (left side); and PRIS 2 (right side; red line), the distance from the ilioischial line to the tip of the ischial spine, even if its radiopaque shadow was situated behind the pelvic brim as shown. (B) A closer view of PRIS 1 (white line) and PRIS 2 (black line) is shown.
To assess the interobserver and intraobserver variabilities of the PRIS sign, 26 of the 149 pelvis radiographs were selected randomly and assessed by two of us (RJS, FK) on two occasions at least 1 week apart.
Sensitivity, specificity, positive and negative predictive value, and 95% confidence intervals (95% CIs) were calculated for the presence or absence of PRIS as an indicator of retroversion. The association between the COS and PRIS was calculated with the Spearman correlation to see if a more distal COS correlated with a longer PRIS 2. The interobserver and intraobserver agreements were assessed using random effects analysis of variance. Analyses were performed with SPSS 11.0 for Windows (SPSS Inc, Chicago, IL).
Results
The measurements obtained from the radiographs are shown in Table 2. The presence or absence of PRIS 1 was correlated (p < 0.001) with the presence or absence of COS for all hips. Using a positive COS as the gold standard for measurement of retroversion, the presence of PRIS 1 as diagnostic of acetabular retroversion showed a sensitivity of 91% (95% CI, 0.85%–0.95%), a specificity of 98% (95% CI, 0.94%–1.00%), a positive predictive value of 98% (95% CI, 0.94%–1.00%), and a negative predictive value of 92% (95% CI, 0.87%–0.96%).
Table 2.
Radiographic measurements obtained from anteroposterior pelvic radiographs
| Radiographic measurement | Value | Range |
|---|---|---|
| Femoral head diameter (mm) | 66 | 47–94 |
| Acetabular length (mm) | 80 | 56–107 |
| Crossover sign length (mm) | 21 | 4–46 |
| Percentage of retroverted acetabulum | 25 | 5–63 |
| Prominence of ischial spine 1 (mm) | 6.7 | 1–18.5 |
| Prominence of ischial spine 2 (mm) | 14 | 4–27 |
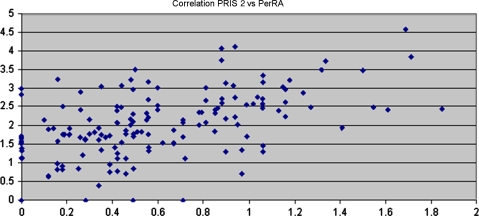
We found a correlation (Spearman R = 0.6; p < 0.001) between PRIS 2 and percentage of retroversion (Fig. 3), indicating, as the length of the PRIS increases, so does the distance from the acetabular roof to the crossover point. This correlation also was present when this was assessed in subgroups of surgical intervention and radiographic diagnosis.
Fig. 3.
A scatterplot shows the correlation between the length of PRIS 1 and the distance between the acetabular roof and the crossover point described as percentage of retroverted acetabulum (PerRA).
The measurements were reproducible and reliable among observers (Table 3).
Table 3.
Interobserver and Intraobserver reliability for radiographic measurements obtained on two different occasions
| Radiographic measurement | Interrater | Intrarater |
|---|---|---|
| Symphysis/coccyx distance | 0.58 | 0.76 |
| Femoral head diameter | 0.94 | 0.97 |
| Acetabular length | 0.91 | 0.95 |
| Crossover sign | 0.65 | 0.83 |
| Prominence of ischial spine 1 | 0.91 | 0.92 |
| Prominence of ischial spine 2 | 0.77 | 0.87 |
Discussion
Femoroacetabular impingement has been described as a mechanism that can lead to osteoarthritis [16, 18]. It occasionally is seen in patients with retroversion of the acetabulum [13]. Retroversion of the acetabulum can be seen on AP pelvic radiographs as the COS, which has been validated as a measurement for retroversion [7]. In clinical practice, we noticed, when a COS was seen, the ischial spine also was seen as a prominence in the pelvic cavity. These findings prompted our review of radiographs to determine the correlation between COS and PRIS. The findings of this study showed a high correlation between the COS and the PRIS. The PRIS is easily visible on the AP radiograph as a projection in the pelvic cavity and is not easily confused, making it a reliable radiographic landmark for retroversion.
A major limitation to this study was the number of radiographs that were excluded because of lack of standardization. Because interpretation of the AP pelvic radiograph is very sensitive to the position of the pelvis at the time of exposure [14], we adhered to strict criteria to include radiographs in the study. Only 15% of the initial radiographs were deemed adequate for the study. Most of the excluded radiographs were not well centered or rotated, which was seen frequently in radiographs taken in earlier years when there was no standardization, or were sometimes of poor quality and the anterior and posterior walls were not visible in their entirety or the symphysis was covered by a gonadal shield. The number of radiographs that were included was small in relation to those that were available, but the source of measurement error would have been too high to accurately validate the PRIS sign as indicative of retroversion. Another limitation of this study was the fact that the radiographs were not adjusted for the magnification factor. However, we used the percentage of retroverted acetabulum, which is the percentage of the ratio between the acetabular diameter and the length of the COS, as a measurement to adjust for magnification. Furthermore, 35% of patients in this series had radiographic acetabular retroversion, which is not surprising, as we were reviewing radiographs of a very select group of patients with hip disorders. The incidence of acetabular retroversion is believed to be one in three to one in six in patients with hip dysplasia [9, 10]. Ezoe et al. [3] also described retroversion in 20% of patients with OA, 18% with developmental dysplasia, and 42% with Legg-Calvé-Perthes disease. Retroversion is more likely to be present in patients with hip disorders than in healthy subjects (6%) [5]. This may limit the applicability of our study to the general population, but this does not change the fact that the COS has a high correlation with the PRIS. Finally, the study was limited by the fact that the observers could not be blinded to the diagnoses. Therefore if a positive PRIS sign was seen, an unconscious effort could have been made by the observer to see a COS. The good correlation between the length of the ischial spine and the length of the COS shows that these measurements are highly dependent on each other.
In conjunction with the COS, the PRIS sign should be used to detect patients with early symptomatic femoroacetabular impingement and also can be used to detect hips at risk when the condition is bilateral and only one side is symptomatic. The PRIS can be used in the pediatric population, for example, because the acetabular walls are not ossified, so their contours are not visible on an AP radiograph. The PRIS can detect acetabular retroversion in this situation and can aid in preoperative planning of osteotomies. Also, in the case of pelvic triple osteotomies that do not leave the posterior column and ischial spine intact, the PRIS sign may aid intraoperatively to prevent iatrogenic acetabular retroversion, a complication that has been reported after poorly performed osteotomies in children and adults [2].
As PRIS increases in size, so does the distance from the roof to the COS, which indicates retroversion is not only a periacetabular phenomenon (a deficiency or absence of the posterior wall of the acetabulum or a prominence of the anterior wall) but also could represent a malrotation, possibly congenital, of the whole hemipelvis. Tönnis and Heinecke [17] alluded to this in their study. They concluded differences in the degree of anteversion of the acetabulum and femur were likely a result of congenital conditions caused by various intrauterine rotational positions of the fetal limbs. In the majority of cases, rotational discrepancies regress spontaneously after birth, but in approximately 15% of cases they do not, resulting in either an increase or decrease in normal version. In some cases, this abnormal version can lead to femoroacetabular impingement and through this mechanism cause OA [1, 4].
We found excellent sensitivity and positive predictive value of the PRIS as a radiographic marker of acetabular retroversion. The PRIS is easily recognized on the AP pelvic radiograph even for the general physician with little training in orthopaedic surgery. The high correlation between PRIS and COS shows patients with these signs actually may have retroversion of the distal hemipelvis and not only a hypoplastic posterior wall or a prominence of the anterior wall. The PRIS sign can be used as a secondary measure for diagnosis and management of patients with acetabular disorders.
Acknowledgments
We thank Burkhardt Seifert, Department of Biostatistics, ISPM, University of Zürich, Switzerland.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed]
- 2.Dora C, Mascard E, Mladenov K, Seringe R. Retroversion of the acetabular dome after Salter and triple pelvic osteotomy for congenital dislocation of the hip. J Pediatr Orthop B. 2002;11:34–40. [DOI] [PubMed]
- 3.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. [DOI] [PubMed]
- 4.Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed]
- 5.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269. [DOI] [PubMed]
- 6.Goodman D, Feighan J, Smith A, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis: relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79:1489–1497. [DOI] [PubMed]
- 7.Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the “cross-over-sign.” J Orthop Res. 2007;25:758–765. [DOI] [PubMed]
- 8.Leunig M, Casillas MM, Hamlet M, Hersche O, Nötzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. [DOI] [PubMed]
- 9.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. [DOI] [PubMed]
- 10.Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004;418:48–53. [DOI] [PubMed]
- 11.Murray RO. The aetiology of primary osteoarthritis of the hip. Br J Radiol. 1965;38:810–824. [DOI] [PubMed]
- 12.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. [DOI] [PubMed]
- 13.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain.J Bone Joint Surg Br. 1999;81:281–288. [DOI] [PubMed]
- 14.Siebenrock KA, Karlbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. [DOI] [PubMed]
- 15.Stulberg SD, Cordell LD, Harris WH, Ramsey PL, MacEwen GD. Unrecognized childhood hip disease: a major cause of idiopathic osteoarthritis of the hip. In: Amstutz HC, ed. The Hip: Proceedings of the Third Open Scientific Meeting of the Hip Society. St Louis, MO: CV Mosby; 1975:212–228.
- 16.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. [DOI] [PubMed]
- 17.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed]
- 18.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–518. [DOI] [PubMed]