Abstract
Wear curves from individual patients often show unexplained irregular wear curves or impossible values (negative wear). We postulated errors of two-dimensional wear measurements are mainly the result of radiographic projection differences. We tested a new method that makes two-dimensional wear measurements less sensitive for radiograph projection differences of cemented THAs. The measurement errors that occur when radiographically projecting a three-dimensional THA were modeled. Based on the model, we developed a method to reduce the errors, thus approximating three-dimensional linear wear values, which are less sensitive for projection differences. An error analysis was performed by virtually simulating 144 wear measurements under varying conditions with and without application of the correction: the mean absolute error was reduced from 1.8 mm (range, 0–4.51 mm) to 0.11 mm (range, 0–0.27 mm). For clinical validation, radiostereometric analysis was performed on 47 patients to determine the true wear at 1, 2, and 5 years. Subsequently, wear was measured on conventional radiographs with and without the correction: the overall occurrence of errors greater than 0.2 mm was reduced from 35% to 15%. Wear measurements are less sensitive to differences in two-dimensional projection of the THA when using the correction method.
Introduction
Wear is an important factor in failure of THAs [4, 8, 9, 15, 17, 18, 26]. Manual measurement methods using pencils, plastic templates of circles, and calipers on films are being abandoned in favor of more accurate digital measurement techniques that are becoming the standard for two-dimensional (2-D) wear measurements. Although the precision of these techniques has improved substantially, reported mean errors are still as much as 0.5 mm [3, 7, 8, 10, 14, 19, 23, 24, 27, 28]. A potential source of errors in 2-D wear measurements in a clinical setting are the differences between the 2-D projection of the THA on the immediate postoperative and followup radiographs. The irregular wear patterns, and the occurrence of impossible values such as negative wear, that are seen in individual wear curves may be the result of this. (A more open projection of the cup will result in a smaller distance between the center of the metal ring and the center of the femoral head; if the second radiograph is such that the acetabular cup is now projected more closed, thus with a metal ring that seems narrower, the projected distance between the center of the metal ring and the center of the femoral head will become larger, implying negative wear.) This jeopardizes the applicability of measurements for a patient, and a method to eliminate this source of error therefore is desirable.
We previously developed a geometric framework to model wear measurement errors resulting from projection differences of a THA [29]. Based on this model, we developed an algorithm that adjusted the raw 2-D measurements to more accurate values. This adjustment was accomplished by mathematically reversing the causal chain leading to the 2-D measurement error and then converting the measurement value to approximate the true linear wear, as was described in an earlier publication [29]. This approximation is obtained by using the differences in projection between the radiographs (for example, more pelvic tilting on either radiograph) to extract additional information on the wear pattern. In other words, the source of errors (differences in projection) is used to create more accurate linear wear estimates. This correction method was tested in a laboratory setting and yielded promising preliminary results [29]: in a zero-wear situation, measurement errors of 0.2 mm were found when projection differences in acetabular anteversion were as small as 5°. When the correction method was used, projection differences needed to exceed 20° to result in the same measurement error [29].
Although the results showed a clear improvement in validity of measurement values in that specific specimen in a no-wear situation in a laboratory setting, it remains unclear how the correction method would perform in different individuals in a clinical setting. It also is not clear how the correction method is affected if the assumption of the model (knowledge of the true plane of wear) is not met. This assumption can never be met in clinical practice. The correction method thus needs to be robust; it should still be accurate even if the model assumption is not ideally met. Otherwise, the correction could cause additional errors instead of eliminating them.
The first aim of this study was to subject the correction method to a sensitivity analysis. The second aim was to determine the accuracy of wear measurements with and without application of the correction method.
Materials and Methods
The study design consisted of two components. First, a virtual simulation of wear measurements was performed to quantify the errors (mean absolute error in millimeters of wear measured) that occur when model assumptions were not met. Second, a clinical series with available radiostereometic analysis (RSA) wear measurements was used to determine the efficacy of the correction method in a clinical setting (mean absolute error in millimeters of wear measured). We simulated 144 wear measurements with and without application of the correction method (Appendix 1) by computer analysis under varying conditions; the projection difference of the cup between the reference and followup radiograph varied from 10° to 30°, absolute cup anteversion varied from 0° to 70°, whereas the true amount of linear wear was set at 2.0 mm. The model on which the correction method is based assumes the true plane of wear is known. We simulated failures to meet this assumption by introducing errors of the assumed true plane of wear from –30° to +30°. In other words, if the wear would be assumed to occur in the plane of the radiograph, the true direction of wear was simulated to be at an angle between −30° (posteriorly) and +30° (anteriorly) relative to the radiograph.
The computer calculated how the center of the femoral head would be projected on film relative to the metal ring on the reference and followup radiographs. The raw 2-D linear wear was calculated as the projected shift of the femoral head relative to the metal ring. The difference between the raw 2-D linear wear and the true wear (2.0 mm) was recorded. Then, the correction was applied (Appendix 1) and the resulting difference between the approximated three-dimensional (3-D) linear wear and the true linear wear was recorded. (All reported results are thus calculated and not measured.)
For clinical validation of the correction method, we included all eligible patients who were to receive a primary all-polyethylene THA and who could be given one of the especially manufactured (tantalum-marked) prostheses. We obtained a cohort of 47 patients (32 women) who received a ScanHip® Classic II system with Opticup® (Biomet, Brigend, UK) from September 1995 to October 1998 in the University Hospital of Lund, Lund, Sweden. For this type of prosthesis, the distance between the center of the 28-mm femoral head and the center of the metal ring is approximately 2 mm. For most other types of prostheses, this value is between 2 and 7 mm. The greater this distance, the greater is the expected gain of the correction algorithm.
The mean age (± standard deviation) of the patients was 67 (± 12) years. Their mean body weight (± standard deviation) was 78 (± 13) kg. Twenty-four arthroplasties were performed on the left side. All patients were analyzed with RSA, the gold standard for in vivo wear measurements. Radiostereometric analysis is a method in which change of position of bony or artificial (prosthetic) structures in relation to each other can be measured very accurately. A stereoradiographic approach provides a computer with the necessary data to calculate the relative displacement of interest [5, 13, 22, 25, 30].
The ultrahigh molecular weight polyethylene (UHMWPE) cups (ranging from 46 to 56 mm) had been marked with seven to nine tantalum markers by the manufacturer. Radiostereometric analysis examinations were performed by a uniplanar technique [16, 25] with the patient in the supine position. The two radiograph sources, at an angle of 40° relative to each other, were fixed (mounted to the ceiling). We used a Type 41 calibration cage (Tilly Medical, Lund, Sweden) and the computer software UmRSA® Version 5.0 (RSA Biomedical, Umeå, Sweden). The reference examination was performed within 1 week of the operation and the followups at 1, 2, and 5 years postoperatively. Conventional hip radiographs were taken on the same day as the RSA examinations. The RSA wear measurements were made by digitally tracing the motion of the tantalum markers and calculation of the resultant 3-D vector of the head migration into the cup.
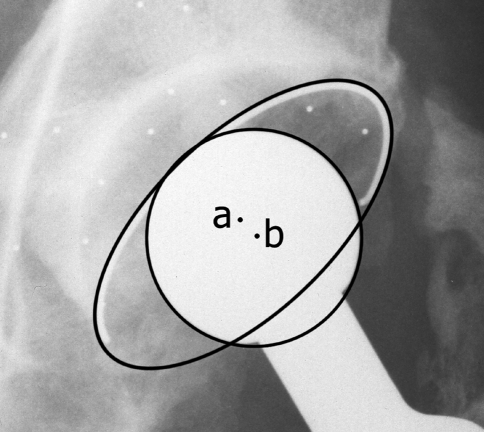
All raw measurements (thus without correction) were performed on 150 dpi digitized radiographs using the noncommercially available software application, Hip, developed in the Orthopaedic Biomechanics Laboratory, University Medical Center Radboud, Nijmegen, The Netherlands. The observer was blinded from the 3-D RSA measurement results. The center of the metal contrast wire of the cup and the center of the prosthetic femoral head were used as reference points for the wear measurements (Fig. 1). The center of the metal ring was determined by digital placement of 10 points on the outer outline of the metal contrast wire. Using these points, an ellipse was fitted by the computer and its center calculated. Ten points on the edge of the femoral head were used to fit an ellipse on the femoral head and calculate its center. Then, the location of the center of the femoral head relative to the center of the metal ring of the acetabular cup was calculated. Wear was detected as a shift of the location of the femoral head relative to the metal ring. The linear wear is corrected for magnification with the known diameter of the femoral head.
Fig. 1.
The raw 2-D measurement method in this study uses the change in distance between two reference points to determine linear wear. The center of the metal ring (a) and the center of the femoral head (b) are used as reference points.
We recorded the difference between the raw 2-D linear wear and the true 3-D linear wear as determined by RSA. Then, the correction was applied and the resulting corrected estimate was compared with the true 3-D linear wear as determined by RSA.
Mean absolute errors and ranges of errors, incidence of errors of a predetermined magnitude, and Pearson correlation coefficients were calculated using SPSS Version 12.0 (SPSS Inc, Chicago, IL). Alpha was set at 0.05 when testing for statistical significance.
Results
The raw measurements had a mean absolute error of 1.8 mm (range, 0–4.51 mm). This was reduced to a mean absolute error of 0.10 mm (range, 0–0.27 mm) by applying the correction (Table 1). The largest error with correction was 0.27 mm and occurred when an extreme failure of meeting the model assumptions was introduced; the assumed plane of wear was at an angle of 30° with the true plane of wear. Negative wear values were found in 25% of the raw measurements, whereas none were found after correction.
Table 1.
Error analysis by virtual simulation
| Difference in opening angle between radiographs | Anteversion | Error (mm) | |
|---|---|---|---|
| No error correction applied | Error correction applied | ||
| 10° | 0° and 10° | 0.18 (0.15–0.27) | 0.10 (0–0.27) |
| 10° and 20° | 0.45* | 0.10 (0–0.27) | |
| 20° and 30° | 0.74* | 0.10 (0–0.27) | |
| 30° and 40° | 1.00* | 0.10 (0–0.27) | |
| 40° and 50° | 1.23* | 0.10 (0–0.27) | |
| 50° and 60° | 1.43* | 0.10 (0–0.27) | |
| 60° and 70° | 1.58* | 0.10 (0–0.27) | |
| Mean | 0.94 | 0.10 | |
| 20° | 0° and 20° | 0.60* | 0.10 (0–0.27) |
| 10° and 30° | 1.19* | 0.10 (0–0.27) | |
| 20° and 40° | 1.74* | 0.10 (0–0.27) | |
| 30° and 50° | 2.23* | 0.10 (0–0.27) | |
| 40° and 60° | 2.66* | 0.10 (0–0.27) | |
| 50° and 70° | 3.01* | 0.10 (0–0.27) | |
| Mean | 1.91 | 0.10 | |
| 30° | 0° and 30° | 1.34* | 0.10 (0–0.27) |
| 10° and 40° | 2.19* | 0.10 (0–0.27) | |
| 20° and 50° | 2.97* | 0.10 (0–0.27) | |
| 30° and 60° | 3.66* | 0.10 (0–0.27) | |
| 40° and 70° | 4.24* | 0.10 (0–0.27) | |
| Mean | 2.88 | 0.10 | |
| Overall mean | 1.80 | 0.10 | |
Each given error is a mean of the absolute errors at 0°, 10°, 20°, and 30° out-of-plane wear, thus indicating the degree of failure to meet the model assumption of using the correct plane of wear; *all values were equal in this series.
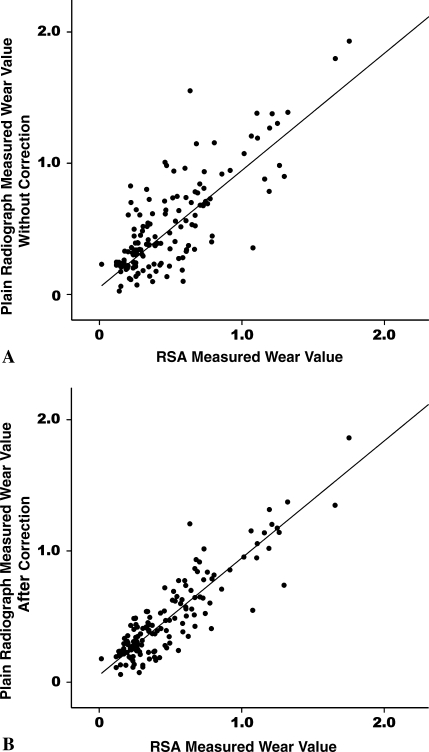
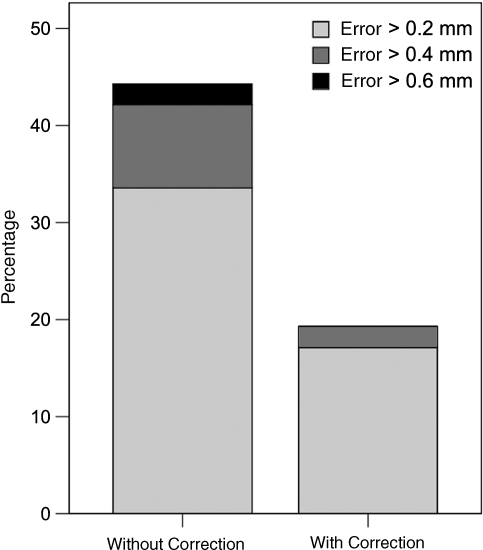
Raw wear values correlated with (r = 0.83; r2 = 0.71) RSA values (Fig. 2A). This was enhanced to a correlation coefficient of 0.92 (r2 = 0.85) when applying the correction method (Fig. 2B). Errors greater than 0.6 mm appeared in 2% of the raw measurements and were eliminated completely by the correction method. Errors greater than 0.4 mm were present in 9% of the raw measurements, which was reduced to 2% by applying the correction. An error greater than 0.2 mm was found in 34% of the raw measurements, whereas this was reduced to 17% by application of the correction (Fig. 3). The mean absolute error was 0.2 mm for the raw values, which was reduced to 0.1 mm with application of the correction method.
Fig. 2A–B.
(A) The true wear values are plotted against the wear values as measured using plain radiographs without application of the correction method. (B) The true wear values are plotted against the wear values as measured using plain radiographs after application of the correction method. The data cloud is now closer to the diagonal as a consequence of better correlation between these values in comparison with the uncorrected values in (A).
Fig. 3.
The magnitude of wear measurement errors is clearly diminished by application of the correction method. It eliminates errors in the highest category (> 0.6 mm) but also lowers the prevalence of errors of lesser magnitude.
Discussion
Most existing 3-D wear measurement techniques are expensive or time-consuming or demand the use of additional (lateral) radiographs, dedicated software, or implantation of reference objects near the THA. We have developed a new method that combines the advantages of conventional 2-D wear measurements with the advantages of 3-D measurements; the obtained wear values are more valid and are virtually identical with varying projections of the THA, whereas no additional equipment or radiographs are needed. The method was effective in virtual and clinical settings. A correlation coefficient of 0.92 (r2 = 0.85) was found between RSA measured values and the values obtained when applying the correction method. This compares favorably or at least comparably to the results of true 3-D methods. The correlation coefficient comparing the values for wear derived with the PolyWare™ (Draftware Developers, Inc, Vevay, IN) radiographic technique with the values derived with a coordinate measuring machine is 0.78, while the correlation coefficient comparing the values derived with the Martell Hip Analysis Suite (The University of Chicago Orthopaedic Research Institute, Chicago, IL) radiographic technique with those derived with a coordinate measuring machine is 0.80 [12].
Some limitations and assumptions concerning the study have to be mentioned. Although the method uses a reversal algorithm to convert 2-D measurements into approximations of the 3-D linear wear, the method cannot be said to be a truly 3-D method because it does not provide the user with separate wear values over three perpendicularly oriented axes of direction. Therefore, the method does not provide the user with a separate estimate of out-of-plane wear, which would enable the user to quantify volumetric wear. However, the reversal algorithm (and thus the correction method) provides the user with measurement values that possess characteristics of 3-D wear values: an overall linear wear value that approximates the 3-D linear wear value and values that are not as sensitive to radiographic projection differences as conventional 2-D wear measurement values.
A second limitation is the fact that our results do not apply to metal-backed prostheses. We focused on wear measurements of cemented THAs for two reasons. The circumferential metal ring of all-polyethylene cups enables accurate measurement of projection differences of the THA [1], which is a basic step in the correction method. Second, the expected gain in validity is highest in measurements on all-polyethylene cups. The reason for this is the center of the metal ring and the center of the femoral head do not coincide but are approximately 2 to 7 mm (depending on the type of cup) apart in a zero-wear situation. The greater this distance, the greater is the expected gain from using the correction method. We used a THA prosthesis type with only a small distance (2 mm) between the reference points, which means the results, when using other types of THA prostheses, in (possible) future replicate studies might be even better.
When applying the correction method in this study, we presumed the second radiograph was the plane in which true wear occurred. This is partially arbitrary because we cannot really know the true plane of wear, but it does have a theoretical advantage: the link between opening angle and 2-D projected distance of reference points is the most accurate in the first postoperative radiograph (because no wear has yet occurred). Correction of the opening angle (and therefore the projected distance) is sure to be exact on the first radiograph, whereas a correction on other radiographs can slightly overcorrect or undercorrect. Because this error is not expected to be very large, an alternative method to choose the reference plane such as the average of the opening angles is also defendable, and perhaps even preferable, when more than two followup radiographs are available; the consideration of more radiographs might be expected to produce a better estimate of the true plane of wear. Nonetheless, the error analysis in this study has clarified the fact that exact knowledge of the true plane of wear is not necessary; even when assuming a wrong plane of wear, it is beneficial to apply the correction method.
We did not assume wear always occurs in a pure cranial or craniomedial direction because the direction of wear is craniolateral in a substantial fraction of our patients. This necessitates a step by which the correction is only applied on the vectoral component perpendicular to the major axis of the elliptic projection of the metal ring (as described in Appendix 1). Not following these guidelines might result in overcorrection of the measurement values.
We could not distinguish between wear and creep in our study. The latter certainly can be a relevant source of additional penetration of the femoral head into the polyethylene. It is believed to mostly add to penetration rates in the first year after implantation and has been the specific subject of study in several papers [2, 11, 21]. Although our correction method, similar to other methods, cannot directly distinguish creep from wear, it does offer the possibility of estimating the amount of creep in individual cases because it makes reliable individual wear curves possible.
Several studies report the implications of using 2-D versus 3-D wear measurements. It is commonly accepted 2-D measurements on average (thus on a group level) underestimate the 3-D wear value (mean differences varying from 0.07 to 0.46 mm) [6, 12, 20, 28]. In addition, wear curves of individual patients measured with 2-D techniques can be unstable, as illustrated in an earlier publication [29]. That report provided the theoretical foundation for the correction method and showed promising preliminary results in a cadaver study. The current study suggests application of this method will not result in large errors, even under extreme conditions, by performing an extensive error analysis. Translated to clinical practice, this also implies the influence of variability in position of the patient on measurement values is substantially reduced. The RSA validation performed in this study has shown its superior performance in a clinical setting in comparison with raw (ie, uncorrected) measurements. Future clinical studies will have to be conducted to quantify the efficacy of this method in different clinical settings (eg, in different types of prostheses). However, on the basis of our results, we would recommend implementation of the correction method in 2-D orthopaedic software packages.
Appendix 1
The correction method uses the underlying mechanism of differences in 2-D projected distances with varying positions of two objects in space to construct a 3-D linear wear approximation [17]. The following formula is used for correction of the raw wear measurement assuming the second radiograph to be the true plane of wear:
 |
where v1 is the distance between the two reference points on the first (direct postoperative) radiograph, v2 is the distance between the reference points on the second radiograph, α is the opening angle of the cup on the first radiograph, and β is the opening angle of the cup on the second radiograph used for the wear measurement. The opening angles are calculated with the following formula: opening angle = arcsine (minor axis/major axis).
This formula should be applied to the vectoral component of wear occurring perpendicular to the long axis of the projected metal contrast wire. The component of wear occurring parallel to this axis should not be changed. The total linear wear is then calculated by taking the square root of the sums of the quadratic values of the adjusted vector perpendicular to the major axis and the unadjusted vector parallel to the major axis of the ellipse.
Footnotes
One or more authors (BT) have received funding from Biomet NL (Dordrecht, The Netherlands).
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Ackland MK, Bourne WB, Uhthoff HK. Anteversion of the acetabular cup: measurement of angle after total hip replacement. J Bone Joint Surg Br. 1986;68:409–413. [DOI] [PubMed]
- 2.Atkinson JR, Cicek RZ. Silane crosslinked polyethylene for prosthetic applications. II. Creep and wear behaviour and a preliminary moulding test. Biomaterials. 1984;5:326–335. [DOI] [PubMed]
- 3.Bankston AB, Cates H, Ritter MA, Keating EM, Faris PM. Polyethylene wear in total hip arthroplasty. Clin Orthop Relat Res. 1995;317:7–13. [PubMed]
- 4.Barrack RL, Castro FP Jr, Szuszczewicz ES, Schmalzried TP. Analysis of retrieved uncemented porous-coated acetabular components in patients with and without pelvic osteolysis. Orthopedics. 2002;25:1373–1378; discussion 1378. [DOI] [PubMed]
- 5.Bragdon CR, Estok DM, Malchau H, Karrholm J, Yuan X, Bourne R, Veldhoven J, Harris WH. Comparison of two digital radiostereometric analysis methods in the determination of femoral head penetration in a total hip replacement phantom. J Orthop Res. 2004;22:659–664. [DOI] [PubMed]
- 6.Devane PA, Bourne RB, Rorabeck CH, Hardie RM, Horne JG. Measurement of polyethylene wear in metal-backed acetabular cups. I. Three-dimensional technique. Clin Orthop Relat Res. 1995;319:303–316. [PubMed]
- 7.Devane PA, Horne JG. Assessment of polyethylene wear in total hip replacement. Clin Orthop Relat Res. 1999;369:59–72. [DOI] [PubMed]
- 8.Dowd JE, Sychterz CJ, Young AM, Engh CA. Characterization of long-term femoral-head-penetration rates: association with and prediction of osteolysis. J Bone Joint Surg Am. 2000;82:1102–1107. [DOI] [PubMed]
- 9.Dumbleton JH, Manley MT, Edidin AA. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17:649–661. [DOI] [PubMed]
- 10.Hardinge K, Porter ML, Jones PR, Hukins DW, Taylor CJ. Measurement of hip prostheses using image analysis: the Maxima hip technique. J Bone Joint Surg Br. 1991;73:724–728. [DOI] [PubMed]
- 11.Huber J, Walter A, Plitz W, Refior HJ. [Effect of the manufacturing process on creep and wear properties of UHMWPE (ultra-high molecular weight polyethylene)] (in German). Biomed Tech (Berl). 1995;40:88–92. [DOI] [PubMed]
- 12.Hui AJ, McCalden RW, Martell JM, MacDonald SJ, Bourne RB, Rorabeck CH. Validation of two and three-dimensional radiographic techniques for measuring polyethylene wear after total hip arthroplasty. J Bone Joint Surg Am. 2003;85:505–511. [DOI] [PubMed]
- 13.Ilchmann T. Radiographic assessment of cup migration and wear after hip replacement. Acta Orthop Scand Suppl. 1997;276:1–26. [DOI] [PubMed]
- 14.Jones PR, Taylor CJ, Hukins DW, Porter ML, Hardinge K. Prosthetic hip failure: retrospective radiograph image analysis of the acetabular cup. J Biomed Eng. 1989;11:253–257. [DOI] [PubMed]
- 15.Kadoya Y, Kobayashi A, Ohashi H. Wear and osteolysis in total joint replacements. Acta Orthop Scand Suppl. 1998;278:1–16. [PubMed]
- 16.Karrholm J, Herberts P, Hultmark P, Malchau H, Nivbrant B, Thanner J. Radiostereometry of hip prostheses: review of methodology and clinical results. Clin Orthop Relat Res. 1997;344:94–110. [PubMed]
- 17.Looney RJ, Boyd A, Totterman S, Seo GS, Tamez-Pena J, Campbell D, Novotny L, Olcott C, Martell J, Hayes FA, O’Keefe RJ, Schwarz EM. Volumetric computerized tomography as a measurement of periprosthetic acetabular osteolysis and its correlation with wear. Arthritis Res. 2002;4:59–63. [DOI] [PMC free article] [PubMed]
- 18.Maloney WJ, Schmalzried T, Harris WH. Analysis of long-term cemented total hip arthroplasty retrievals. Clin Orthop Relat Res. 2002;405:70–78. [DOI] [PubMed]
- 19.Martell JM, Berdia S. Determination of polyethylene wear in total hip replacements with use of digital radiographs. J Bone Joint Surg Am. 1997;79:1635–1641. [DOI] [PubMed]
- 20.Martell JM, Berkson E, Berger R, Jacobs J. Comparison of two and three-dimensional computerized polyethylene wear analysis after total hip arthroplasty. J Bone Joint Surg Am. 2003;85:1111–1117. [DOI] [PubMed]
- 21.McDonald MD, Bloebaum RD. Distinguishing wear and creep in clinically retrieved polyethylene inserts. J Biomed Mater Res. 1995;29:1–7. [DOI] [PubMed]
- 22.Ostgaard SE, Gottlieb L, Toksvig-Larsen S, Lebech A, Talbot A, Lund B. Roentgen stereophotogrammetric analysis using computer-based image-analysis. J Biomech. 1997;30:993–995. [DOI] [PubMed]
- 23.Pedersen DR, Brown TD, Hillis SL, Callaghan JJ. Prediction of long-term polyethylene wear in total hip arthroplasty, based on early wear measurements made using digital image analysis. J Orthop Res. 1998;16:557–563. [DOI] [PubMed]
- 24.Phillips NJ, Stockley I, Wilkinson JM. Direct plain radiographic methods versus EBRA-digital for measuring implant migration after total hip arthroplasty. J Arthroplasty. 2002;17:917–925. [DOI] [PubMed]
- 25.Selvik G. Roentgen stereophotogrammetry: a method for the study of the kinematics of the skeletal system. Acta Orthop Scand Suppl. 1989;232:1–51. [PubMed]
- 26.Sethi RK, Neavyn MJ, Rubash HE, Shanbhag AS. Macrophage response to cross-linked and conventional UHMWPE. Biomaterials. 2003;24:2561–2573. [DOI] [PubMed]
- 27.Shaver SM, Brown TD, Hillis SL, Callaghan JJ. Digital edge-detection measurement of polyethylene wear after total hip arthroplasty. J Bone Joint Surg Am. 1997;79:690–700. [DOI] [PubMed]
- 28.Sychterz CJ, Yang AM, McAuley JP, Engh CA. Two-dimensional versus three-dimensional radiographic measurements of polyethylene wear. Clin Orthop Relat Res. 1999;365:117–123. [DOI] [PubMed]
- 29.The B, Mol L, Diercks RL, Ooijen PM, Verdonschot N. Correction of error in two-dimensional wear measurements of cemented hip arthroplasties. Clin Orthop Relat Res. 2006;442:180–186. [DOI] [PubMed]
- 30.Valstar ER, Vrooman HA, Toksvig-Larsen S, Ryd L, Nelissen RG. Digital automated RSA compared to manually operated RSA. J Biomech. 2000;33:1593–1599. [DOI] [PubMed]