Abstract
Vascular injuries around the hip are uncommon with hip arthroplasty. However, given the close proximity of the external iliac and femoral vessels to the hip, iatrogenic injury may occur. We describe a case of superficial femoral artery injury occurring during revision THA using an extended trochanteric osteotomy, bulk allograft, and cerclage wires. We review the available literature on vascular injury in hip arthroplasty and illustrate the great care necessary when placing cerclage wires and the importance of prompt recognition of these potentially devastating complications.
Introduction
Arterial injury with THA is rare but does occur owing to the close proximity of the external iliac and femoral vessels to the hip. The incidence of vascular injury is between 0.16% and 0.25% [3, 7]. Mehta and Finn [6] described a case in which the femoral artery was occluded after a cerclage wire was placed at the level of the midshaft of the femur. Tethering of the fascia surrounding the vessels resulted in an obstruction of blood flow. We had a similar case in a revision THA in which strut allografts and cerclage wires were used after an extended trochanteric osteotomy. In our patient, the distal-most cerclage wire located at the junction of the middle to distal shaft of the femur surrounded and occluded the superficial femoral artery resulting in obstruction of arterial flow. We describe this patient, review the literature, and show the importance of surgical technique to prevent vascular injury. In addition, we illustrate the care necessary when placing cerclage wires and the importance of prompt recognition of these complications.
Case Report
A 48-year-old man with a history of Perthes disease and an osteotomy during childhood presented for evaluation of a painful left hip. Ten years earlier, he had a primary arthroplasty, which consisted of a cemented acetabular component and femoral stem. Secondary to the retained hardware and the femoral deformity, an extended trochanteric osteotomy was performed. The preoperative neurovascular examination showed full motor and sensory function with palpable dorsalis pedis and posterior tibial pulses. The patient’s medical history was otherwise normal. Preoperative anteroposterior radiographs of the pelvis showed a well-fixed cemented acetabular component and a loose subsided cemented femoral stem with a healed trochanteric osteotomy (Fig. 1).
Fig. 1.
A preoperative anteroposterior radiograph of the pelvis shows a well-fixed cemented acetabular component and a loose subsided cemented femoral stem with a healed trochanteric osteotomy.
We performed the revision using the patient’s previous lateral incision and used an extended trochanteric osteotomy to facilitate exposure and aid cement removal. The proximal femur had thin cortices and multiple nondisplaced fractures with contained defects. The stem and the cement were removed without difficulties or additional bone loss. In addition, a transverse diaphyseal osteotomy was needed to accommodate varus remodeling of the femur and to allow placement of the long stem revision component.
Strut allografts with morselized cancellous bone then were placed medially and posterolaterally spanning the proximal and distal fragments of the transverse osteotomy. These were fixed to the femur with multiple cerclage Luque wires. The wires were placed in a subperiosteal fashion with the assistance of a standard wire passer and passed after the strut grafts had been positioned. We encountered no difficulties when passing the cerclage wires and the remainder of the procedure was completed without complications. The patient was extubated at the end of the procedure and transferred to the recovery room in stable condition.
In the recovery room, the patient had diminished sensation on the dorsal and plantar aspect of his foot and was unable to perform dorsiflexion or plantar flexion. His vascular examination showed palpable pulses with a somewhat cool foot. At this point, the patient was returned to the operating room for a suspected sciatic nerve injury. Exploration of the sciatic nerve from the greater sciatic notch to the knee found the nerve free and without signs of contusion, compression, or laceration. After completion of the exploration, perfusion to the limb came into question, as there were signs of impaired circulation: distal pulses no longer were palpable and we were unable to obtain Doppler signals. An emergency vascular surgery consultation was obtained and an intraoperative arteriogram revealed complete obstruction of the superficial femoral artery at the level of the distal-most cerclage wire with impaired distal runoff (Fig. 2). The vascular surgeon performed a thrombectomy and placed an endovascular stent, which relieved compression of the superficial femoral artery (Fig. 3). Once perfusion was restored to the limb, the offending cerclage wire was removed without complications (Fig. 4). After the procedure, the patient had palpable pulses and a well-perfused foot.
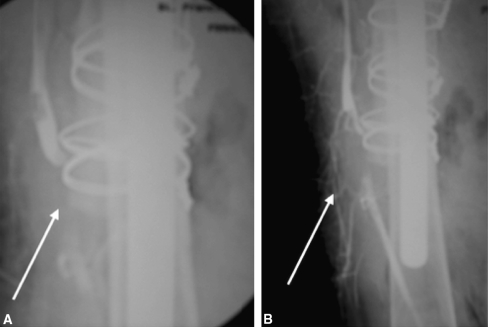
Fig. 2A–B.
Intraoperative arteriograms of the left lower extremity show (A) the superficial femoral artery obstruction before removal of the thrombus (arrow) and (B) the occlusion of the artery at the distal-most cerclage wire after thrombus removal (arrow).
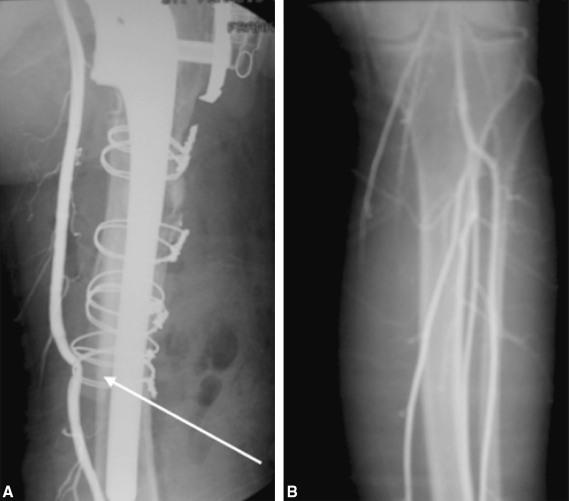
Fig. 3A–B.
An intraoperative angiogram shows (A) the cerclage wire before removal around the femoral artery (arrow). (B) After endovascular stent placement the occlusion of the superficial femoral artery is now relieved and normal distal runoff has been restored.
Fig. 4.

An anteroposterior femoral radiograph taken 2 months postoperatively shows the endovascular stent (arrow) and its proximity to the medially placed strut allograft.
The patient was monitored in the intensive care unit to follow his neurovascular status and to watch for signs of compartment syndrome. As the patient showed elevated creatine kinase levels, he also was monitored for the sequelae of rhabdomyolysis.
The patient’s neurovascular status returned to normal once perfusion was restored to the limb and he had no additional neurovascular problems while hospitalized. The remaining postoperative course was unremarkable, and at the 2-year followup, the patient was functioning well, was pain free, and had no neurovascular impairment.
Discussion
Vascular injury after hip arthroplasty is a rare but potentially catastrophic complication. Nachbur et al. [7] reported 15 patients with vascular injury and identified an overall incidence of 0.25% during an 8-year period. Numerous mechanisms of injury have been identified. The most common include direct trauma from retractor placement; thrombotic occlusion from atherosclerotic plaque rupture or heat polymerization, migration, or implantation of a threaded cup; acetabular protrusion with removal of the cup and/or cement; acetabular reaming; and adjunctive acetabular screw fixation [2, 4, 5, 7, 8]. Sharma et al. [9] performed a questionnaire study among the members of the British Hip Society and reported on 26 vascular injuries. Fourteen of the 26 cases occurred during revision surgery and 86% occurred either immediately or within 48 hours of surgery. Shoenfeld et al. [10] retrospectively reviewed five patients from their experience and 63 from the literature to further define vascular injury during hip arthroplasty. Thirty-nine percent of these injuries occurred in revisions and 43% required emergent surgery. Of those that required emergency surgery, 67% were in the revision group, with the most common presentations being excessive bleeding and ischemia. The most commonly injured vessels were the external iliac artery (36), common femoral artery (17), and the external iliac vein (six). In addition, there was an overall 7% mortality rate and a 15% incidence of limb loss. Delayed presentation of arterial injury after THA also has been reported with false aneurysm occurrence in the femoral artery [8].
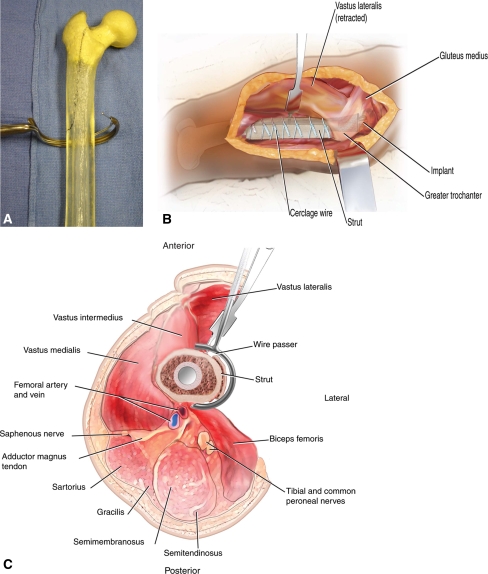
Based on the literature, most of the vascular injuries occurring during hip arthroplasty are in the region of the acetabulum and the proximal femur. Our report and another [6] describe cases of vascular injury related to cerclage wire placement at the middle to distal third of the femur. Both occurred during revision surgery, which has been identified as a risk factor for vascular injury [1]. In addition, both occurred in the middle femur, where the femoral artery courses close to the femur as it prepares to enter Hunter’s canal. With the growing popularity of using an extended trochanteric osteotomy to remove a well-fixed cementless femoral stem or to facilitate cement removal, the importance of passing cerclage wires in this region cannot be overemphasized. Our case shows the great care necessary when passing cerclage wires around the femur, particularly in the middle shaft to distal third of the femur near Hunter’s canal. When using strut allografts, one must be even more diligent when passing cerclage wires, as the bulk of these grafts can change the contour of the femur and thus place the surrounding soft tissues at risk. In this situation, it is best to place the cerclage wires first around the femur and then pass them around the strut grafts to protect the nearby neurovascular structure (Fig. 5).
Fig. 5A–C.
Great care is necessary when passing cerclage wires around the femur, particularly when using strut allografts. The cerclage wires should be placed around the femur first and then passed around the strut grafts to protect the nearby neurovascular structure. (A) A photograph shows the wire passer used in our case. (B) A lateral view shows the cerclage wires around the strut graft. Care should be taken at the distal extent of the wound where the neurovascular bundle is closest to the femur. (C) A cross section shows the proximity of the wire passer to the neurovascular bundle after strut application.
This report was written retrospectively several years after the injury to our patient occurred and some of the specific details involving the case were not readily available. The way in which the initial injury was evaluated may not be agreed upon by all. However, our case shows the importance of an early postoperative neurovascular check to recognize any form of neurovascular injury. In our patient, even though the predominant finding appeared to be a neurologic deficit, it ultimately allowed us to identify the vascular injury and treat it emergently to restore blood flow to the limb. If recognized early and dealt with appropriately, vascular injury after hip arthroplasty can be associated with acceptable outcomes [3]. However, if the diagnosis is delayed, the potential for disastrous complications, such as loss of the limb or even death, is real [4]. Therefore, the most important treatment for a vascular injury after hip arthroplasty is prevention. This starts with a thorough preoperative examination to detect any degree of arterial or neurologic insufficiency in the lower extremity and then requires a high index of suspicion postoperatively so that a prompt diagnosis can be made and treated appropriately.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bergqvist D, Carlsson AS, Ericsson BF. Vascular complications after total hip arthroplasty. Acta Orthop Scand. 1983;54:157–163. [DOI] [PubMed]
- 2.Darmanis S, Pavlakis D, Papanikolaou A, Apergis E. Neurovascular injury during primary total hip arthroplasty caused by a threaded acetabulum cup. J Arthroplasty. 2004;19:520–524. [DOI] [PubMed]
- 3.Feugier P, Fessy MH, Carret JP, Fischer LP, Bejui J, Chevalier JM. [Total hip arthroplasty: risk factors and prevention of iatrogenic complications] [in French]. Ann Chir. 1999;53:127–135. [PubMed]
- 4.Keating EM, Ritter MA, Faris PM. Structures at risk from medially placed acetabular screws. J Bone Joint Surg Am. 1990;72:509–511. [PubMed]
- 5.Mallory TH, Jaffe SL, Eberle RW. False aneurysm of the common femoral artery after total hip arthroplasty: a case report. Clin Orthop Relat Res. 1997;338:105–108. [DOI] [PubMed]
- 6.Mehta V, Finn HA. Femoral artery and vein injury after cerclage wiring of the femur: a case report. J Arthroplasty. 2005;20:811–814. [DOI] [PubMed]
- 7.Nachbur B, Meyer RP, Verkkala K, Zürcher R. The mechanisms of severe arterial injury in surgery of the hip joint. Clin Orthop Relat Res. 1979;141:122–133. [PubMed]
- 8.Proschek D, Proschek P, Hochmuth K, Blazer JO, Mack MG, Vogl TJ. False aneurysm of the left femoral artery and thrombosis of the left femoral vein after total hip arthroplasty. Arch Orthop Trauma Surg. 2006:126:493–497. [DOI] [PubMed]
- 9.Sharma DK, Kumar N, Mishra V, Howell FR. Vascular injuries in total hip replacement arthroplasty: a review of the problem. Am J Orthop. 2003;32:487–491. [PubMed]
- 10.Shoenfeld NA, Stuchin SA, Pearl R, Haveson S. The management of vascular injuries associated with total hip arthroplasty. J Vasc Surg. 1990;11:549–555. [DOI] [PubMed]