Abstract
The goal of the Bernese periacetabular osteotomy is to correct the deficient acetabular coverage in hips with developmental dysplasia to prevent secondary osteoarthrosis. We determined the 20-year survivorship of symptomatic patients treated with this procedure, determined the clinical and radiographic outcomes of the surviving hips, and identified factors predicting poor outcome. We retrospectively evaluated the first 63 patients (75 hips) who underwent periacetabular osteotomy at the institution where this technique was developed. The mean age of the patients at surgery was 29 years (range, 13–56 years), and preoperatively 24% presented with advanced grades of osteoarthritis. Four patients (five hips) were lost to followup and one patient (two hips) died. The remaining 58 patients (68 hips) were followed for a minimum of 19 years (mean, 20.4 years; range, 19–23 years) and 41 hips (60%) were preserved at last followup. The overall mean Merle d’Aubigné and Postel score decreased in comparison to the 10-year value and was similar to the preoperative score. We observed no major changes in any of the radiographic parameters during the 20-year postoperative period except the osteoarthritis score. We identified six factors predicting poor outcome: age at surgery, preoperative Merle d’Aubigné and Postel score, positive anterior impingement test, limp, osteoarthrosis grade, and the postoperative extrusion index. Periacetabular osteotomy is an effective technique for treating symptomatic developmental dysplasia of the hip and can maintain the natural hip at least 19 years in selected patients.
Level of Evidence: Level III, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Dysplasia of the hip is a frequent cause of secondary osteoarthritis (OA) [29, 31, 32]. Although THA is the preferred treatment for older patients who are not expected to outlive the implant or in whom only few revisions are anticipated, arthroplasty becomes a less desirable solution in younger, more active patients in whom the cause of OA can be mechanically corrected. The goal of contemporary joint-preserving hip surgery is to correct these anatomic abnormalities ideally to prevent or at least retard the development of secondary OA.
In 1984, the Bernese periacetabular osteotomy (PAO) for treatment of developmental dysplasia of the hip (DDH) in adolescents and adults was introduced by one of the senior authors (RG) [10]. We have performed this procedure more than 1100 times at our institution and its use has spread worldwide. The Bernese PAO reportedly has favorable short-term and 10-year results [6, 8, 21, 30, 33, 40, 41, 47, 57], but the longer-term outcomes are unknown.
We raised the following questions: (1) what is the 20-year cumulative survivorship of hips that undergo the Bernese PAO?; (2) will the clinical scores and (3) the radiographic measures be maintained with time?; (4) do any demographic (age, gender, body mass index), clinical (hip pain, range of motion [ROM], walking ability, pain provocation tests), radiographic (osteoarthrosis, morphologic features of the femoral head, acetabular coverage and orientation), or surgery-related factors (concomitant intertrochanteric osteotomy [IO] or previous surgeries) predict a poor outcome? Finally, we compared our outcomes with the natural history and with the results of other osteotomies.
Material and Methods
Based on a survival analysis on the first 63 patients (75 hips) who underwent PAO, we performed a retrospective case-control study with comparison of the result to published results of survivorship of hips with a natural course and hips with other pelvic osteotomies. All patients underwent surgery by one of the authors (RG) between April 1984 and December 1987. They are the first consecutive patients undergoing Bernese PAOs. The indication for surgery was a symptomatic hip dysplasia with hip pain in all patients. Fifty-five hips (73%) had additional restricted ambulation. Five patients (six hips or 8%) presented with an underlying neurologic disorder with dysplasia (meningomyelocele, cerebral palsy) including two patients with paraparesis (three hips or 4%). Two patients (two hips or 3%) had a proximal femoral focal deficiency, and posttraumatic acetabular deficiency was present in two patients (two hips or 3%). Twelve patients (19%) had bilateral procedures and 13 patients (16 hips [21%]) had a concomitant IO (Table 1). Concomitant IOs used were abduction IO in 13 (6%) hips, adduction IO in two (3%) hips, and an extension IO in one (1%) hip. In seven of the 13, abduction IOs were performed as re-osteotomy after a previous adduction osteotomy. Twenty-two patients (23 hips [31%]) had a previous surgical attempt to achieve sufficient acetabular coverage, including IO in nine (12%) hips, combined Salter and IO in four (6%) hips, combined triple and IO in three (4%) hips, triple osteotomy combined with another osteotomy in three (4%) hips, combined shelfplasty and IO in two (3%) hips, combined Chiari and IO in one (1%) hip, and one Chiari osteotomy in one (1%) hip. The early preliminary and the minimum 10-year followups of the same patients were reported [10, 47].
Table 1.
Demographic data of the patient series
| Parameter | Value |
|---|---|
| Number of patients (hips) | 63 (75) |
| Percentage of bilateral hips | 16 |
| Age at surgery (years) | 29.3 ± 11.6 (13–56) |
| Gender (percent male of all hips) | 23 |
| Side (percent right of all hips) | 49 |
| Weight (kg) | 61 ± 11.4 (41–86) |
| Height (cm) | 166 ± 8.6 (149–186) |
| Body mass index (kg/m2) | 22.1 ± 3.1 (15.8–28.2) |
| Operation time (hours) | 3.5 ± 0.73 (2.0–5.0) |
| Blood loss (L) | 2.0 ± 0.86 (0.8–4.5) |
| Red blood cell concentrates (units) | 3.8 ± 1.93 (1–11) |
| Concomitant intertrochanteric osteotomy (percent) | 21 |
| Previous surgery to attempt sufficient coverage (percent) | 31 |
| Sphericity index [48] (percent) | 79 ± 9.1 (53–95) |
| Severin classification [44] (percent) | |
| Class 1 | — |
| Class 2 | 1 |
| Class 3 | 50 |
| Class 4 | 44 |
| Class 5 | 5 |
| Class 6 | — |
| Preoperative osteoarthritis score according to Tönnis [55] (percent) | |
| Grade 0 | 43 |
| Grade 1 | 33 |
| Grade 2 | 21 |
| Grade 3 | 3 |
Values of continuous parameters are expressed as mean ± standard deviation with range in parentheses.
Using our patient records, we identified all patients of the series who had known conversion to a THA and the date of conversion. Contacting the remaining patients by phone, again the date of THA was recorded, allowing for calculation of the cumulative survivorship. We clinically and radiographically evaluated the patients with surviving joints at the outpatient clinic. These results for the survivor and the nonsurvivor groups were compared with the preoperative and 10-year followup status and the initial data were tested for predictive factors.
At followup, five patients (seven hips [9%]) were not available. One patient with bilateral osteotomies died during the observation period 6 years postoperatively from a cause unrelated to the osteotomy. Four patients (five hips [7%]) were lost to followup; two had an uneventful postoperative course with followup of 1.2 and 1.8 years, respectively; three hips with a followup of 10.6, 11.3, and 11.5 years had good to excellent clinical results (Merle d’Aubigné and Postel scores ranging from 16 to 18) without severe radiographic signs of OA (OA Grade 2 or greater according to Tönnis [55]) or conversion to a THA at final followup. The minimum followup of the remaining 58 patients (68 hips [91%]) was 19 years (mean, 20.4 ± 1.1 years; range, 19–23 years). This study was approved by the local Institutional Review Board.
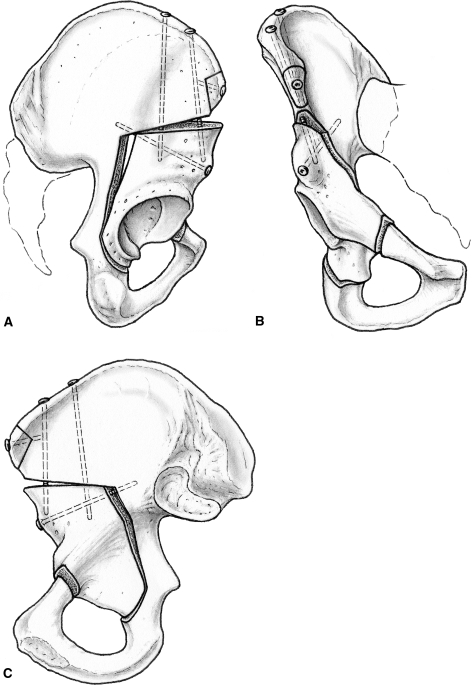
The details of the operative technique have been described [10, 45]. In short, the technique is performed through a modified Smith-Petersen approach, and four periacetabular osteotomies and a controlled fracture are performed to completely mobilize the acetabulum from the innominate bone (Fig. 1). It allows extensive potential for acetabular reorientation with three rotational degrees of freedom, including medial and lateral displacement of the fragment. The posterior column of the true pelvis remains intact maintaining stability through an intact continuity of the pelvic ring allowing for minimal internal fixation of the fragment and aftercare with early partial weightbearing and immediate mobilization without the need for external fixation.
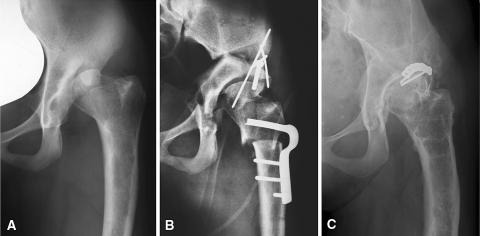
Fig. 1A–C.
The Bernese periacetabular osteotomy is performed through a modified Smith-Petersen approach, including an osteotomy of the anterior superior iliac spine to dissect the inguinal ligament and the adjacent muscles. (A) With four periacetabular osteotomies and a controlled fracture, the acetabulum is completely mobilized from the innominate bone. (B) For fixation of the reoriented fragment, three cortical screws are used. (C) The posterior column of the true pelvis remains intact maintaining stability through an intact continuity of the pelvic ring.
One of the authors (SDS) assessed the 58 patients at last followup with the Merle d’Aubigné and Postel score [27]. The Merle d’Aubigné and Postel score was graded as poor below 12, fair from 12 to 14, good from 15 to 17, and excellent with 18 points [27]. The anterior impingement and apprehension tests were assessed indicating a possible labral lesion anterosuperior or posteroinferior [18, 46, 52]. Additionally, the full goniometric ROM and gait were analyzed. All parameters were documented preoperatively and at 10 and 20 years postoperatively.
Routine radiographic evaluations consisted of preoperative and postoperative anteroposterior (AP) pelvic radiographs and a false profile view [24]. We performed an additional AP abduction view to simulate postoperative joint congruency preoperatively. At each followup, an AP pelvic radiograph and a lateral crosstable radiograph of the proximal femur were obtained [9]. To describe the morphologic features of the acetabulum and femoral head, a series of 11 standard radiographic parameters (Table 2) were assessed and computerized by one observer (SDS) with the help of previously developed and validated computer software (Hip2Norm; University of Bern, Bern, Switzerland) [51, 53, 65]. Osteoarthritis was graded according to Tönnis [55]. To detect the reliability and reproducibility of the Tönnis grading system, 50 pelvic radiographs (100 hips) were randomly chosen from the image database of this patient cohort. The Tönnis classification of OA was applied to all blinded hips by two independent observers (SDS, MT) on two separate occasions at least 1 month apart. Femoral head sphericity was assessed on AP radiographs with the sphericity index defined as the ratio of the minor axis to the major axis of the circle or ellipse drawn to best fit the femoral articular surface. Interobserver agreement and intraobserver agreement of the Tönnis classification were calculated with the kappa value [23]. Kappa was interpreted as poor below 0.20, fair from 0.21 to 0.40, moderate from 0.41 to 0.60, good from 0.61 to 0.80, and very good from 0.81 to 1.0 [23]. The intraobserver variability of the Tönnis classification was good for both observers (kappa, 0.73 for Observer 1; kappa, 0.76 for Observer 2). A good interobserver variability also was detected (kappa, 0.74 for both measurements).
Table 2.
Preoperative and postoperative radiographic status of all patients
| Parameter | Preoperative value | Postoperative value | p Value |
|---|---|---|---|
| Lateral center edge angle [60] (degrees) | 6 ± 9.0 (−24–25) | 34 ± 12.3 (10–55) | < 0.001 |
| Anterior center edge angle [24] (degrees) | 4 ± 13.8 (−20–24) | 26 ± 13.1 (12–50) | < 0.001 |
| Acetabular index [56] (degrees) | 26 ± 10.6 (12–50) | 6 ± 10.7 (−15–18) | < 0.001 |
| Extrusion index [31] (percent) | 37 ± 11.8 (7–81) | 10 ± 9.9 (−13–37) | < 0.001 |
| ACM angle [16] (degrees)+ | 46 ± 9.7 (31–70) | 45 ± 5.6 (34–60) | 0.846 |
| Crossover sign [42] (percent positive) | 36 | 17 | 0.007 |
| Posterior wall sign [42] (percent positive) | 92 | 70 | < 0.001 |
| Shenton’s line intact (percent intact) | 39 | 62 | 0.004 |
| Caudocranial coverage (percent) | 64 ± 15.1 (12–100) | 88 ± 15.8 (63–100) | < 0.001 |
| Anterior coverage (percent) | 15 ± 7.4 (0–31) | 18 ± 10.0 (1–56) | 0.041 |
| Posterior coverage (percent) | 35 ± 11.0 (8–63) | 45 ± 14.4 (8–72) | < 0.001 |
n = 75 hips; there were no changes in radiographic parameters during the 20-year postoperative period; values of continuous parameters are expressed as mean ± standard deviation with range in parentheses; +The ACM angle is a measure of acetabular depth described by Idelberger and Frank [16].
Several demographic (age, gender, body mass index), clinical (hip pain, ROM, walking ability, pain provocation tests [Table 3]), radiographic (osteoarthrosis, femoral head morphology, acetabular coverage and orientation [Table 2]), or surgery-related (concomitant IO, previous surgery) parameters were tested for prediction of poor outcome.
Table 3.
Clinical results of the surviving hips
| Parameter | Preoperative | 10-year Followup | 20-year Followup |
|---|---|---|---|
| Merle d’Aubigné & Postel score [27] | 15.2 ± 1.6 (9–18) | 16.7 ± 1.4 (13–18)* | 15.8 ± 2.1 (10–18)† |
| Limp (percent of all patients) | 66 | 34* | 41* |
| Anterior impingement test [52] | |||
| (percent of all hips) | 20 | 24 | 38* |
| Apprehension test [52] | |||
| (percent of all hips) | 7 | 7 | 7 |
| Range of motion | |||
| Flexion | 117 ± 13.0 (90–130) | 100 ± 11.2 (80–130)* | 93 ± 11.5 (60–110)* |
| Extension | 1 ± 7.8 (−20–20) | 3 ± 4.9 (0–15) | 3 ± 4.5 (0–10) |
| Internal rotation | 41 ± 13.5 (20–70) | 32 ± 15.4 (0–60)* | 18 ± 11.2 (0–40)* |
| External rotation | 35 ± 14.9 (0–70) | 17 ± 12.4 (0–40)* | 14 ± 11.1 (0–40)*,† |
| Abduction | 38 ± 9.2 (20–60) | 33 ± 9.3 (20–50)* | 29 ± 6.6 (15–40)* |
| Adduction | 30 ± 7.9 (10–50) | 27 ± 6.6 (15–40) | 25 ± 5.2 (20–30) |
Values of continuous parameters are expressed as mean ± standard deviation with range in parentheses; *significant difference compared with the preoperative status; †significant difference between 10- and 20-year results.
We tested normal distribution of all continuous parameters with the Kolmogorov-Smirnov test. Because none were normally distributed, we used only nonparametric tests. The cumulative survivorship was performed according to Kaplan and Meier [19] with the end point defined as conversion to THA or fusion of the hip. To detect differences between preoperative and postoperative radiographic values, we used the Wilcoxon signed rank test for continuous data and Fisher’s exact test for binominal data. To compare clinical and radiographic parameters preoperative and at 10- and 20-year followups, the Friedman test was applied. The Cox proportional hazards model was used to detect factors predicting poor outcome and to calculate the corresponding hazard ratios [7]. When a predictive factor with a nonnominal scale was found, differences in terms of the survivorship between the two groups were calculated using the log-rank test. When a survival analysis regarding preoperative OA grades was performed, the only Grade 3 OA according to Tönnis [55] (that was not lost-to-follow-up) was treated as Grade 2 OA.
Results
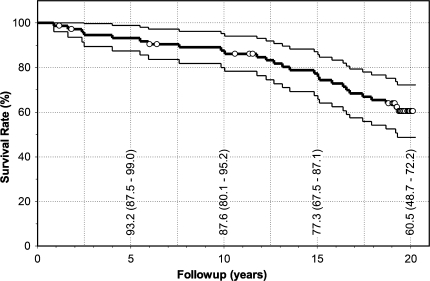
Forty-one hips (60%) were preserved at 20 years, which corresponds to a cumulative Kaplan-Meier survivorship of 60.5% (range, 48.7%–72.2%; 95% confidence interval) (Figs. 2, 3). Twenty-six hips (38%) were converted to a THA and one (1%) had fusion at a mean of 11.7 ± 5.9 years (range, 0.9–19.3 years) after the index operation (Fig. 4).
Fig. 2.
The Kaplan-Meier survival analysis is shown with the conversion to a THA or hip fusion as the end points. Values are expressed as cumulative survivorship with 95% confidence interval in parentheses for each 5-year interval. Circles indicate censored data.
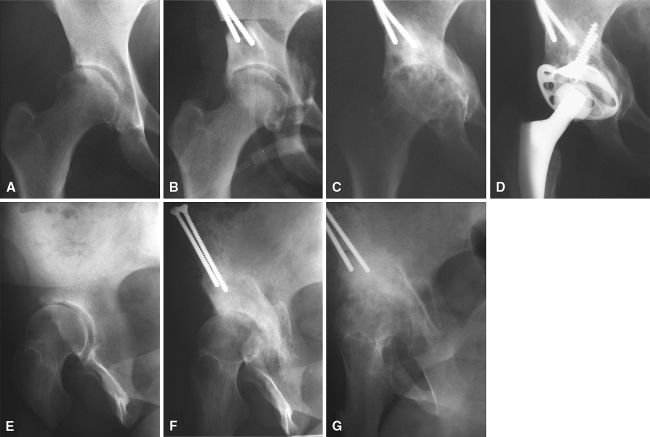
Fig. 3A–G.
Radiographs are shown of a 26-year-old woman with a dysplastic right hip with (A) an LCE angle of 16° and an AI of 12° without any signs of osteoarthritis (Tönnis osteoarthritis Grade 0 [55]). Initially she presented with limping and a negative impingement test. The mean Merle d’Aubigné and Postel score was 15. (B) The postoperative LCE angle was 32° and the AI −2°. At the (C) 10-year and the (D) 20-year followups, no osteoarthitic changes were seen. At last followup, the mean Merle d’Aubigné and Postel was 17, limping disappeared, and the impingement test remained negative. (E) In the corresponding false-profile [24] views, (F) the preoperative ACE angle of 39° increased to 45° postoperatively and (G) no osteoarthritic changes were seen at the 10-year followup. LCE = lateral center edge angle; AI = acetabular index; ACE = anterior center edge angle.
Fig. 4A–G.
Radiographs are shown of a 46-year-old women with a (A) dysplastic right hip with cranial acetabular retroversion, an LCE angle of 8°, an AI of 24°, and preoperative osteoarthritis grade of 1 according to Tönnis [55]. Initially she presented without limping and a negative impingement test. The mean Merle d’Aubigné and Postel score was 16 as a result of a decrease in pain status. (B) With the PAO, good coverage could be achieved with a postoperative relatively highly anteverted acetabular fragment and a resultant prominent posterior wall with an LCE angle of 30° and an AI angle of 4°. (C) The osteoarthritis showed marked progression after 5 years with end-stage osteoarthritis (Tönnis Grade 3), and (D) 10 years after the PAO, a THA with an acetabular reinforcement ring was performed. In the corresponding false-profile [24] views, the (E) preoperative ACE angle of 2° increased to (F) 25° postoperatively and showed (G) early deterioration with end-stage osteoarthritis at the 10-year followup. LCE = lateral center edge angle; AI = acetabular index; ACE = anterior center edge angle.
At 20 years, the mean Merle d’Aubigné and Postel score of all patients decreased (p = 0.004) in comparison to the 10-year value and was similar to (p = 0.095) the preoperative score, mainly related to an re-increase of the pain status. The 41 surviving hips (60%) had a mean Merle d’Aubigné and Postel score of 15.8 ± 2.1 (Table 3) at last followup. Of these, eight hips (20%) were graded as excellent, 25 (61%) as good, six (15%) as fair, and two (5%) as poor. The mean Merle d’Aubigné and Postel score increased (p < 0.001) from the preoperative status in comparison to the scores at 10 years (Table 3). Flexion (p < 0.001), internal (p < 0.001) and external rotation (p < 0.001), and abduction (p = 0.005) in the survivor group were decreased compared with the preoperative status (Table 3). The prevalence of limping decreased (p = 0.023) at the 20-year followup compared with the preoperative status. The prevalence of the anterior impingement test was significantly increased (p = 0.044) at last followup compared with the preoperative status. The prevalence of the apprehension test was not significantly different (p = 1.000) at the 20-year followup compared with the preoperative status (Table 3).
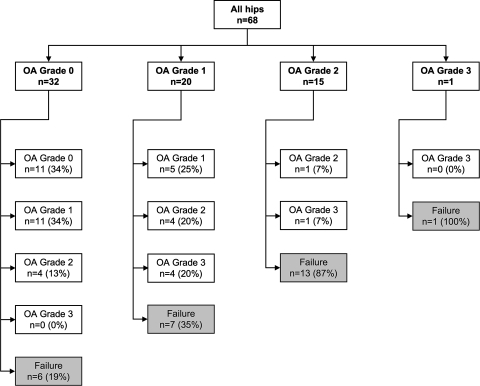
We observed no major changes in any of the radiographic parameters during the 20-year postoperative period except the OA score. In comparison to the preoperative radiographic values, there was an increase of the postoperative lateral center edge angle (LCE), the anterior center edge angle (ACE), the caudocranial/anterior and posterior coverage, and the intactness of Shenton’s line (Table 2). In contrast, the acetabular index (AI), the extrusion index, the crossover, and the posterior wall signs decreased (Table 2). We observed no differences for the ACM angle (p = 0.846). We observed no progression (p = 0.052) of the OA grade in the survivor group from a preoperative mean of 0.4 ± 0.6 (range, 0–2) to 0.6 ± 0.6 (0–2) during the first 10 years. However, the grade increased (p < 0.001) to 1.1 ± 1.0 (range, 0–3) at 20 years. We found decreased (p < 0.001) survivorship with increasing preoperative grade of OA (Fig. 5). Hips with OA scores of 0 or 1 preoperatively (n = 52) had a survivorship of 75%, whereas those with a preoperative OA score of 2 or 3 (n = 16) had a survivorship of 13% (Fig. 5).
Fig. 5.
This flowchart shows the distribution of osteoarthritis (OA) progression and the failure rate depending on the preoperative osteoarthritis score of all 68 evaluated hips.
We identified six factors predicting poor outcome: (1) increased age at surgery, (2) lower preoperative Merle d’Aubigné and Postel score, (3) positive preoperative anterior impingement test, (4) preoperative limp, (5) preoperative increased OA score (Tönnis), and (6) postoperative increased extrusion index (Table 4). Four of these predictive factors had a nonnominal scale. Worse 20-year outcome occurred in patients 30 years and older at the time of surgery (p < 0.001), patients with preoperative Merle d’Aubigné and Postel scores of 14 or less (p < 0.001), those with a preoperative OA grade of 2 (p < 0.001), and those with a postoperative extrusion index of 20% or more (p = 0.004).
Table 4.
Cox regression analysis with THA or hip fusion as end points
| Parameter | Hazard ratio | p Value |
|---|---|---|
| Demographic | ||
| Age (per year older) | 1.08 (1.04–1.11) | <0.001 |
| Clinical | ||
| Merle d’Aubigné and Postel score [27] (per point lower) | 1.31 (1.16–1.48) | <0.001 |
| Positive preoperative anterior impingement test [52] | 6.17 (2.68–14.21) | <0.001 |
| Preoperative limp | 2.87 (1.34–6.17) | 0.007 |
| Radiographic | ||
| Preoperative grade of osteoarthritis [55] (per grade higher)* | 3.39 (2.04–5.63) | <0.001 |
| Postoperative extrusion index [31] (per percent less) | 1.11 (1.06–1.16) | <0.001 |
Values are expressed as mean, with 95% confidence interval in parentheses; * = for Grades 0 to 2. (The only Grade 3 was treated as Grade 2 OA according to Tönnis [55]).
Discussion
Dysplasia of the hip frequently leads to early asymptomatic and symptomatic hip degeneration. The goal of contemporary joint-preserving hip surgery is to correct the anatomic abnormalities leading to early degeneration ideally to prevent or at least retard the development of secondary OA. The goal of the Bernese PAO is to specifically correct deficient acetabular coverage in hips with developmental dysplasia to prevent secondary osteoarthrosis. We raised the following questions: (1) what is the 20-year cumulative survivorship of hips that had the Bernese PAO?; (2) will the clinical scores and (3) the radiographic measures be maintained with time?; (4) do any demographic (age, gender, body mass index), clinical (hip pain, ROM, walking ability, pain provocation tests), radiographic (osteoarthrosis, femoral head morphology, acetabular coverage and orientation), or surgery-related factors (concomitant intertrochanteric osteotomy [IO] or previous surgeries) predict a poor outcome? Finally, we compared our outcomes with the natural history and with the results of other osteotomies.
In additional to the lack of a control group, there are three other limitations to our study. First, clinical parameters of all patients were assessed by different observers at each followup. This is unavoidable for a longitudinal study design spanning more than 20 years. In the literature, substantial interobserver agreement and intraobserver agreement have been reported for the Merle d’Aubigné and Postel score [20], limp [4], and ROM, particularly flexion [14], internal [14, 62] and external [14] rotation, and abduction [14, 26]. Most of these parameters differed between the preoperative and 20-year followup status and therefore we believe these limitations do not influence the results of this study to a large extent. We identified no publication about the reliability and correlation with morphologic findings intraoperatively or in MRIs of the anterior impingement test. This should be considered when comparing the rates of positive anterior impingement tests at the different followups or interpreting the anterior impingement test as a predictive factor. Second, this series of patients reflects the learning curve and the first experiences of a new surgical technique that could be associated with a higher rate of complications [40, 47]. Third, there was considerable heterogeneity in terms of indications, varying degrees of dysplasia [44], OA grade, high number of previous operations, and additional underlying diseases. Although these variations likely reduced the overall 20-year survivorship results, these variations allow an analysis of factors predicting long-term survival.
The surgical technique underwent some minor modifications since the first case in April 1984 (Fig. 6). The supraacetabular osteotomy is now placed more cranially from the anterior-inferior to the anterior-superior iliac spine to preserve vascularity of the acetabular fragment [2] and to improve the hold of the Schanz screw for reorientation (Fig. 1). In addition, since the introduction of the femoroacetabular impingement concept, more emphasis was put on avoiding anterior and lateral overcorrection or retroversion, which could be associated with an unfavorable outcome [34]. For approximately 10 years now, an additional arthrotomy is performed routinely allowing for treatment of labral cysts, observation of range of internal rotation and flexion, and for correction of an aspherical portion of the femoral head-neck offset by osteochondroplasty to improve impingement-free ROM. Therefore, we believe the outcomes with the current technique (including the modifications) would be superior to those in our current study.
Fig. 6A–C.
The first Bernese PAO was performed in 1984 in a 13-year-old girl with a (A) subluxated femoral head articulating in a very shallow and retroverted acetabulum after proximal femoral focal deficiency. (B) The PAO was performed with a concomitant valgus intertrochanteric osteotomy. Three years later, progressive posterior subluxation in flexion resulting from a deficient posterior coverage made a posterior shelfplasty necessary. (C) Twenty-three years later, she presented with a good clinical result (Merle d’Aubigné and Postel score, 15).
We identified six factors predicting poor outcome (Table 4). One was demographic, three were clinical, and two were radiographic factors. A substantial number of these factors were associated with an already advanced stage of joint degeneration at the time of surgery as could be proven for other types of acetabular reorientation procedures: the preoperative OA score [21, 28, 30, 36, 43, 58], a decreased preoperative Merle d’Aubigné and Postel score [58], a preoperative limp, and a positive anterior impingement test indicating a labral lesion [18, 46, 52]. In addition, advanced age [64] was a risk factor for early conversion to THA. The only one of these parameters positively influenced by surgery was the postoperative extrusion index. An undercorrected hip with an extrusion index greater than 20% is prone to develop end-stage OA during the postoperative course. An aspherical femoral head could not be correlated with failure according to these data [30]. Compared with the 10-year result of the same patient series reported earlier [47], the Merle d’Aubigné and Postel score, preoperative positive anterior impingement test and limp, and postoperative extrusion index were new predictive factors. We could not confirm a diminished ACE or an acetabular index less than 0 or greater than 10° predicted poor outcome.
A comparison with the current literature on this topic is difficult. We considered these comparisons in three ways: with the natural course of dysplastic hips, with other acetabular reorientation techniques, and with alternative surgical treatments.
Describing the natural history of hips with dysplasia, Hartofilakidis et al. [12] reported all referred dysplastic hips with a subluxation (ie, broken Shenton’s line) would undergo a THA by the age of 45. These authors would not, of course, be able to comment on asymptomatic patients with subluxation or those who were not symptomatic enough to warrant a referral; many of these patients might undergo THA at a later age or not at all. Others [59] suggest an “inevitability of disabling coxarthrosis” in patients with recognized subluxation. In our study cohort, 54% of all hips with preoperative subluxation (Severin Grade 4 and higher) did not have additional surgery at a mean age of 41 years with a mean Merle d’Aubigné score of 16 points. Murphy et al. [31] reported that all hips with an LCE angle less than 16° or an acetabular index greater than 15° ultimately would develop end-stage OA. In our symptomatic patient cohort, 54% with these radiographic characteristics had no additional surgery at the latest followup (mean age, 44 years). Given more than half of our patients with subluxation did not have additional surgery, we suggest the PAO provides outcomes superior to the natural history in symptomatic patients.
Comparing our results with those of other acetabular reorientation procedures, various studies are available with different followups, treatment in much younger patients before closure of the triradiate cartilage [3, 54], or strong inclusion or exclusion criteria (Table 5). We found two studies for other periacetabular osteotomies with a followup of 20 years [43, 50]. Schramm et al. [43] reported a slightly higher survivorship of 68% for the first 22 cases of spherical periacetabular osteotomy over two decades. However, their patients had a distinctly higher percentage of hips with no signs of preoperative osteoarthritis (77%). Takatori et al. [50] reported a 100% survivorship of dysplastic hips after a rotational acetabular osteotomy at 15 to 22 years followup. However, their study was comprised of a highly selected patient population with a low number of patients (n = 15), no consecutive patient series, exclusively young patients (age younger than 29 years), no preoperative advanced stages of OA, no previous surgeries, and no concomitant femoral osteotomies. Furthermore, the high rate of patients lost to followup (32%) might bias survivorship. Comparing our results with those of other pelvic osteotomies (eg, Chiari, Salter, or triple osteotomy), higher survival rates are reported for a similar followup but in a considerably younger patient group [3, 54, 61] with followup rates of only 60% [61]. Our findings do confirm a worse outcome with increasing age at surgery [61] and with preoperative signs of OA [61]. Additionally, in all of the cited studies [3, 54, 61] the patients had no previous surgical attempts to achieve better acetabular coverage or the series were selected with exclusion of patients with reoperation [3] or neuromuscular disorders [61].
Table 5.
Selected middle and long-term followups
| Authors | Year | Technique | Followup (years) | Number (hips) | Age (years) | Survival rate (percent)* |
|---|---|---|---|---|---|---|
| Current study | 2007 | Bernese | 20.4 (19–23) | 75 | 29.3 (13–56) | 60.5 |
| Kralj et al. [21] | 2005 | Bernese | 12 (7–15) | 26 | 33.5 | 85 |
| Siebenrock et al. [47] | 1999 | Bernese | 11.3 (10–14) | 75 | 29.3 (13–56) | 82 |
| Trumble et al. [57] | 1999 | Bernese | 4.3 (2–10) | 123 | 32.9 (14–54) | 94 |
| Clohisy et al. [6] | 2005 | Bernese | 4.2 | 16 | 17.6 (13.0–31.8) | 100 |
| Hsieh et al. [15] | 2003 | Modified Bernese | 4.2 (2–5) | 46 | 31 (18–58) | 100 |
| Pogliacomi et al. [41] | 2005 | Bernese | 4 (1.5–8) | 36 | 35 (15–55) | 94 |
| Peters et al. [40] | 2006 | Bernese | 3.8 (2.5–7.3) | 83 | 28 (15–47) | 96 |
| Naito et al. [35] | 2005 | Modified Bernese | 3.8 (2–8.3) | 128 | 35.2 (16–59) | 98 |
| Dagher et al. [8] | 2003 | Bernese | 3.5 (2–6) | 64 | 31 (14–59) | 91 |
| Murphy et al. [30] | 2002 | Bernese | Minimum 2 years | 52 | 35.1 (15.8–55.1) | 89† |
| Murphy et al. [33] | 1999 | Bernese | (3–7) | 94 | 29 | 98 |
| Thomas et al. [54] | 2007 | Salter | 43 (40–48) | 77 | 2.8 (1.5–4.7) | 69 |
| Böhm and Brzuske [3] | 2002 | Salter | 31 (26–35) | 73 | 4.1 (1.3–8.8) | 93 |
| Windhager et al. [61] | 1991 | Chiari | 25 (20–34) | 236 | 14.1 (2.6–51.3) | 91 |
| Schramm et al. [43] | 2003 | Spherical | 23.9 (22–29.3) | 22 | 24.4 ± 9.7 | 68 |
| Takatori et al. [50] | 2001 | Rotational | 19.8 (15–22) | 15 | 24.3 (20–28) | 100 |
| Ohashi et al. [39] | 2000 | Chiari | 17 (4–37) | 86 | 18.2 (6–48) | 94 |
| Lack et al. [22] | 1991 | Chiari | 16 (10–21) | 100 | 38 (30–59) | 80 |
| van Hellemondt et al. [58] | 2005 | Triple | 15 (13–20) | 51 | 28 (15–46) | 88 |
| Calvert et al. [5] | 1987 | Chiari | 14 (10–19) | 52 | 19.8 (3–41) | 94 |
| Nakamura et al. [36] | 1998 | Rotational | 13 (10–23) | 145 | 28 (11–52) | 95 |
| Yanagimoto et al. [63] | 2005 | Chiari | 13 (10–20) | 74 | 32 (6–64) | 97 |
| Takatori et al. [49] | 2000 | Rotational | 13 (10–18) | 28 | 33 (19–40) | 96 |
| Miller et al. [28] | 2005 | Dial | 12.6 (5.6–20.2) | 44 | 18.9 (8–31) | 86 |
| Guille et al. [11] | 1992 | Triple | 12 (10–16) | 11 | 14 (10–16) | 91 |
| Nozawa et al. [38] | 2002 | Rotational | 11.4 (10–14.5) | 50 | 31.8 (13–53) | 98 |
| Yasunaga et al. [64] | 2004 | Rotational | 10.5 (8–14.5) | 61 | 35 (13–58) | 100 |
| Ninomiya et al. [37] | 1989 | Rotational | 7.8 (4–16.6) | 41 | 21.5 (10–40) | 100 |
| Hasegawa et al. [13] | 2002 | Rotational | 7.5 (5–10) | 132 | 36.5 (15–59) | 100 |
*Conversion to a THA or hip fusion as the end points; †osteoarthritis Grade 3 according to Tönnis [55] as additional end point.
Good results have been reported with isolated femoral varus ostetotomies [17] or for patients treated with open or closed reduction [1, 25]; however, the patients reported in these series do not represent those in our series.
Despite the fact that our series represents the learning curve of a technically demanding procedure in an inhomogeneous patient group with various previous surgical attempts to achieve sufficient coverage and several concomitant IO, we believe the 20-year results of the first 75 hips are promising. Based on the predictive factors we identified, we suggest the ideal patient for this surgical procedure is young (younger than 30 years) with no or slight preoperative OA (OA score 0 or 1) and no severe hip pain. A positive anterior impingement test suggests an anterior labral lesion and therefore a worse prognosis. A major surgical difficulty is to find the correct balance between undercorrection and overcorrection of the acetabular fragment and to restore correct anteversion. Undercorrection should be avoided because a postoperative extrusion index less than 20% predicts worse outcome. However, overcorrection with acetabular retroversion may cause subsequent painful femoroacetabular impingement [34], which also predicts a worse outcome. We believe these long-term results show PAO is an effective technique for treating symptomatic DDH in selected patients and can maintain the natural hip for at least 19 years in most patients.
Footnotes
One or more of the authors (SDS, MT, KAS) have received funding from the National Center for Competence in Research “Co-Me” of the Swiss National Science Foundation.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Angliss R, Fujii G, Pickvance E, Wainwright AM, Benson MK. Surgical treatment of late developmental displacement of the hip: results after 33 years. J Bone Joint Surg Br. 2005;87:384–394. [DOI] [PubMed]
- 2.Beck M, Leunig M, Ellis T, Sledge JB, Ganz R. The acetabular blood supply: implications for periacetabular osteotomies. Surg Radiol Anat. 2003;25:361–367. [DOI] [PubMed]
- 3.Böhm P, Brzuske A. Salter innominate osteotomy for the treatment of developmental dysplasia of the hip in children: results of seventy-three consecutive osteotomies after twenty-six to thirty-five years of follow-up. J Bone Joint Surg Am. 2002;84:178–186. [DOI] [PubMed]
- 4.Briggs KK, Kocher MS, Rodkey WG, Steadman JR. Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. J Bone Joint Surg Am. 2006;88:698–705. [DOI] [PubMed]
- 5.Calvert PT, August AC, Albert JS, Kemp HB, Catterall A. The Chiari pelvic osteotomy: a review of the long-term results. J Bone Joint Surg Br. 1987;69:551–555. [DOI] [PubMed]
- 6.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–259. [DOI] [PubMed]
- 7.Cox DR. Regression models and life tables. J R Stat Soc [Ser B]. 1972;34:187–220.
- 8.Dagher F, Ghanem I, Abiad R, Haykal G, Kharrat K, Phares A. [Bernese periacetabular osteotomy for the treatment of the degenerative dysplastic hip][in French]. Rev Chir Orthop Reparatrice Appar Mot. 2003;89:125–133. [PubMed]
- 9.Eijer H, Leunig M, Mohamed N, Ganz R. Cross-table lateral radiographs for screening of anterior femoral head-neck offset in patients with femoro-acetabular impingement. Hip Int. 2001;11:37–41.
- 10.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias: technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed]
- 11.Guille JT, Forlin E, Kumar SJ, MacEwen GD. Triple osteotomy of the innominate bone in treatment of developmental dysplasia of the hip. J Pediatr Orthop. 1992;12:718–721. [DOI] [PubMed]
- 12.Hartofilakidis G, Karachalios T, Stamos KG. Epidemiology, demographics, and natural history of congenital hip disease in adults. Orthopedics. 2000;23:823–827. [DOI] [PubMed]
- 13.Hasegawa Y, Iwase T, Kitamura S, Yamauchi Ki K, Sakano S, Iwata H. Eccentric rotational acetabular osteotomy for acetabular dysplasia: follow-up of one hundred and thirty-two hips for five to ten years. J Bone Joint Surg Am. 2002;84:404–410. [PubMed]
- 14.Holm I, Bolstad B, Lutken T, Ervik A, Rokkum M, Steen H. Reliability of goniometric measurements and visual estimates of hip ROM in patients with osteoarthrosis. Physiother Res Int. 2000;5:241–248. [DOI] [PubMed]
- 15.Hsieh PH, Shih CH, Lee PC, Yang WE, Lee ZL. A modified periacetabular osteotomy with use of the transtrochanteric exposure. J Bone Joint Surg Am. 2003;85:244–250. [DOI] [PubMed]
- 16.Idelberger K, Frank A. [A new method for determination of the angle of the pelvic acetabulum in child and in adult.] Z Orthop Ihre Grenzgeb. 1952;82:571–577. [PubMed]
- 17.Ito H, Matsuno T, Minami A. Intertrochanteric varus osteotomy for osteoarthritis in patients with hip dysplasia: 6 to 28 years followup. Clin Orthop Relat Res. 2005;433:124–128. [DOI] [PubMed]
- 18.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262–271. [DOI] [PubMed]
- 19.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. [DOI]
- 20.Kirmit L, Karatosun V, Unver B, Bakirhan S, Sen A, Gocen Z. The reliability of hip scoring systems for total hip arthroplasty candidates: assessment by physical therapists. Clin Rehabil. 2005;19:659–661. [DOI] [PubMed]
- 21.Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7–15-year follow-up of 26 hips. Acta Orthop. 2005;76:833–840. [DOI] [PubMed]
- 22.Lack W, Windhager R, Kutschera HP, Engel A. Chiari pelvic osteotomy for osteoarthritis secondary to hip dysplasia: indications and long-term results. J Bone Joint Surg Br. 1991;73:229–234. [DOI] [PubMed]
- 23.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [DOI] [PubMed]
- 24.Lequesne M, de Séze S. Le faux profil du bassin. Nouvelle incidence radiographique pour l’étude de la hanche. Son utilitè dans les dysplasies et les differentes coxopathies. Rev Rhum Mal Osteoartic. 1961;28:643–652. [PubMed]
- 25.Malvitz TA, Weinstein SL. Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am. 1994;76:1777–1792. [DOI] [PubMed]
- 26.McWhirk LB, Glanzman AM. Within-session inter-rater reliability of goniometric measures in patients with spastic cerebral palsy. Pediatr Phys Ther. 2006;18:262–265. [DOI] [PubMed]
- 27.Merle d’Aubigné R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed]
- 28.Miller NH, Krishnan SG, Kamaric E, Noble PC. Long-term results of the dial osteotomy in the treatment of high-grade acetabular dysplasia. Clin Orthop Relat Res. 2005;433:115–123. [DOI] [PubMed]
- 29.Millis MB, Poss R, Murphy SB. Osteotomies of the hip in the prevention and treatment of osteoarthritis. Instr Course Lect. 1992;41:145–154. [PubMed]
- 30.Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Relat Res. 2002;405:168–174. [DOI] [PubMed]
- 31.Murphy SB, Ganz R, Muller ME. The prognosis in untreated dysplasia of the hip: a study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995;77:985–989. [DOI] [PubMed]
- 32.Murphy SB, Kijewski PK, Millis MB, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Relat Res. 1990;261:214–223. [PubMed]
- 33.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98. [DOI] [PubMed]
- 34.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. [DOI] [PubMed]
- 35.Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005;433:129–135. [DOI] [PubMed]
- 36.Nakamura S, Ninomiya S, Takatori Y, Morimoto S, Umeyama T. Long-term outcome of rotational acetabular osteotomy: 145 hips followed for 10–23 years. Acta Orthop Scand. 1998;69:259–265. [DOI] [PubMed]
- 37.Ninomiya S. Rotational acetabular osteotomy for the severely dysplastic hip in the adolescent and adult. Clin Orthop Relat Res. 1989;247:127–137. [PubMed]
- 38.Nozawa M, Shitoto K, Matsuda K, Maezawa K, Kurosawa H. Rotational acetabular osteotomy for acetabular dysplasia: a follow-up for more than ten years. J Bone Joint Surg Br. 2002;84:59–65. [DOI] [PubMed]
- 39.Ohashi H, Hirohashi K, Yamano Y. Factors influencing the outcome of Chiari pelvic osteotomy: a long-term follow-up. J Bone Joint Surg Br. 2000;82:517–525. [DOI] [PubMed]
- 40.Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006;88:1920–1926. [DOI] [PubMed]
- 41.Pogliacomi F, Stark A, Wallensten R. Periacetabular osteotomy: good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthop. 2005;76:67–74. [DOI] [PubMed]
- 42.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. [DOI] [PubMed]
- 43.Schramm M, Hohmann D, Radespiel-Troger M, Pitto RP. Treatment of the dysplastic acetabulum with Wagner spherical osteotomy: a study of patients followed for a minimum of twenty years. J Bone Joint Surg Am. 2003;85:808–814. [DOI] [PubMed]
- 44.Severin E. Contribution to the knowledge of congenital dislocation of the hip joint: late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand. 1941;84:1–142.
- 45.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed]
- 46.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion: treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. [DOI] [PubMed]
- 47.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. [DOI] [PubMed]
- 48.Steppacher SD, Tannast M, Werlen S, Siebenrock KA. Femoral head morphology differs between hips with deficient and excessive acetabular coverage. Clin Orthop Relat Res. 2008;466:782–790. [DOI] [PMC free article] [PubMed]
- 49.Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I. Long-term results of rotational acetabular osteotomy in young patients with advanced osteoarthrosis of the hip. J Orthop Sci. 2000;5:336–341. [DOI] [PubMed]
- 50.Takatori Y, Ninomiya S, Nakamura S, Morimoto S, Moro T, Nagai I. Long-term results of rotational acetabular osteotomy in patients with slight narrowing of the joint space on preoperative radiographic findings. J Orthop Sci. 2001;6:137–140. [DOI] [PubMed]
- 51.Tannast M, Mistry S, Steppacher S, Zheng G, Langlotz F, Siebenrock KA. Computer-assisted correction of radiographic parameters on pelvic xrays with Hip2Norm: reliable, validated. In: Langlotz F, Davies BL, Grützner PA, eds. Computer Assisted Orthopaedic Surgery. Berlin, Germany: ProBusiness; 2007:88–91.
- 52.Tannast M, Siebenrock KA, Anderson SE. Femoroacetabular impingement: radiographic diagnosis: what the radiologist should know. AJR Am J Roentgenol. 2007;188:1540–1552. [DOI] [PubMed]
- 53.Tannast M, Zheng G, Anderegg C, Burckhardt K, Langlotz F, Ganz R, Siebenrock KA. Tilt and rotation correction of acetabular version on pelvic radiographs. Clin Orthop Relat Res. 2005;438:182–190. [DOI] [PubMed]
- 54.Thomas SR, Wedge JH, Salter RB. Outcome at forty-five years after open reduction and innominate osteotomy for late-presenting developmental dislocation of the hip. J Bone Joint Surg Am. 2007;89:2341–2350. [DOI] [PubMed]
- 55.Tönnis D. General radiography of the hip joint. In: Tönnis D, ed. Congenital Dysplasia, Dislocation of the Hip. New York, NY: Springer; 1987:100–142.
- 56.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed]
- 57.Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy: minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res. 1999;363:54–63. [DOI] [PubMed]
- 58.van Hellemondt GG, Sonneveld H, Schreuder MH, Kooijman MA, de Kleuver M. Triple osteotomy of the pelvis for acetabular dysplasia: results at a mean follow-up of 15 years. J Bone Joint Surg Br. 2005;87:911–915. [DOI] [PubMed]
- 59.Wedge JH, Wasylenko MJ. The natural history of congenital dislocation of the hip: a critical review. Clin Orthop Relat Res. 1978;137:154–162. [PubMed]
- 60.Wiberg G. The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand. 1939;83:7–38.
- 61.Windhager R, Pongracz N, Schönecker W, Kotz R. Chiari osteotomy for congenital dislocation and subluxation of the hip: results after 20 to 34 years follow-up. J Bone Joint Surg Br. 1991;73:890–895. [DOI] [PubMed]
- 62.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. [DOI] [PubMed]
- 63.Yanagimoto S, Hotta H, Izumida R, Sakamaki T. Long-term results of Chiari pelvic osteotomy in patients with developmental dysplasia of the hip: indications for Chiari pelvic osteotomy according to disease stage and femoral head shape. J Orthop Sci. 2005;10:557–563. [DOI] [PubMed]
- 64.Yasunaga Y, Ochi M, Shimogaki K, Yamamoto S, Iwamori H. Rotational acetabular osteotomy for hip dysplasia: 61 hips followed for 8–15 years. Acta Orthop Scand. 2004;75:10–15. [DOI] [PubMed]
- 65.Zheng G, Tannast M, Anderegg C, Siebenrock KA, Langlotz F. Hip(2)Norm: an object-oriented cross-platform program for 3D analysis of hip joint morphology using 2D pelvic radiographs. Comput Methods Programs Biomed. 2007;87:36–45. [DOI] [PubMed]