Abstract
Perceptions of the difficulty and outcome of unicompartmental knee arthroplasty revision (rev-UKA) vary. We analyzed differences in the complexity, cost, and survival of rev-UKAs compared with revision TKAs (rev-TKA). One hundred eighty knee arthroplasty revisions (68 rev-UKAs/112 rev-TKAs), defined as a minimum of tibial or femoral component revision, were identified from a community joint registry of 7587 knee implants performed between 1991 and 2005. Four of 68 rev-UKAs (5.9%) were revised a second time, whereas seven of 112 rev-TKAs (6.3%) were rerevised. Rev-TKA was predictably more complex than rev-UKA based on the proxies of operative time, use of modular augmentation and stems, and polyethylene liner thickness. Thirty-nine of 68 rev-UKAs (57%) had no form of augmentation and were revised as primary TKAs. There were more rev-TKAs than rev-UKAs with an implant cost greater than $5200 (42% versus 12%) and hospital charges greater than $33,000 (48% versus 25%). We found no difference in survival between the groups. Although rev-UKAs had less surgical complexity and bone loss at the time of revision compared with rev-TKAs, we were unable to show improved survival of rev-UKAs compared with rev-TKAs. Rev-UKAs were associated with lower implant costs and hospital charges compared with rev-TKAs.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Since its introduction, UKA has been an alternative to TKA or high tibial osteotomy for management of isolated unicompartmental knee arthritis. The proposed advantages of UKA include preservation of femoral and tibial bone stock, a less invasive surgery, improved knee range of motion [2] and kinematics, and shorter postoperative lengths of hospitalization [22]. Although early midterm studies cited a high rate of satisfactory results after UKA [12], long-term survivorship and outcome continue to be a concern [9, 13, 20]. Although these concerns are not without foundation, they have been addressed with advancements in prosthetic component design, instrumentation and surgical technique, and appropriate patient selection [5, 7, 27]. Some reports have cited reliable UKA survivorship of greater than 90% for more than 10 years after implantation [1, 11, 19, 21, 26]. When compared with TKA as an index arthroplasty procedure, however, the cumulative revision rate for UKA tends to be higher [8, 9, 15, 17, 20].
Early investigations of UKA revision (rev-UKA) reported technical difficulties associated with the procedure, including substantial bone loss with grafting [20], the need for stemmed revision components, or even the need for custom implants [3]. More recent reports concerning contemporary rev-UKA have been more favorable, noting a technically straightforward approach in terms of revision joint replacement surgery [4, 6, 14, 16, 18, 23, 24].
Although the typical recommendation for UKA failure is revision to TKA, little information is available regarding rev-UKA survival or the survival of rev-UKA compared with rev-TKA. Also, numerous reports of rev-UKA and rev-TKA mostly have been limited to one surgeon, academic, or institutional experience. Infrequently have such reports been gathered from series reflective of the community experience, which may be more representative of the overall efficacy of a surgical procedure.
We hypothesized, in comparison with rev-TKA, rev-UKA would be (1) less complex as reflected by lower use of modular stems and augments and shorter operative time, (2) less expensive as reflected in implant costs, total hospital charges, and higher percentage of patients discharged home, and (3) more durable as reflected in improved implant survival.
Materials and Methods
Between September 1, 1991, and December 31, 2005, 7587 knee arthroplasties were performed in a community-based arthroplasty registry established in the HealthEast hospital system in St Paul, MN. Details of the registry data entry and collection methods and application of statistical analyses have been reported [10]. The registry is based on the case load of 44 orthopaedic surgeons working in 5 hospitals. During this same period, 183 patients had 183 revision knee surgeries involving, at minimum, revision of the tibial or femoral component. Three of the 180 surgeries were excluded from the analysis because the revision involved rev-UKA to another UKA prosthesis, leaving 180 cases (68 rev-UKAs, 112 rev-TKAs) available for analysis. Thirty-four surgeons performed these 180 primary arthroplasties and an identical number performed the revision procedures. Of the 180 revisions, 115 (64%) were performed by the same surgeon who performed the index arthroplasty. Institutional review board approval was obtained for the study. We found no differences in patient gender, age, or diagnosis at the time of the index revision arthroplasty for the two groups (Table 1). The most common indication for knee arthroplasty, either UKA or TKA, was osteoarthritis.
Table 1.
Patient demographics
| Demographic | Rev-UKA (n = 68) | Rev-TKA (n = 112) | Chi square p value |
|---|---|---|---|
| Gender | |||
| Male | 25 (37%) | 51 (45%) | 0.25 |
| Female | 43 (63%) | 61 (55%) | |
| Age | |||
| < 65 years | 36 (53%) | 71 (63%) | 0.17 |
| ≥ 65 years | 32 (47%) | 41 (37%) | |
| Primary diagnosis | |||
| Osteoarthritis | 62 (91%) | 109 (97%) | 0.07 |
| All others | 6 (9%) | 3 (3%) |
Rev-UKA = unicompartmental knee arthroplasty revision; rev-TKA = TKA revision.
There were clear differences in the indications for primary rev-UKA and rev-TKA (Table 2). Progressive adjacent compartment arthritis was the principal factor leading to rev-UKA (48%), whereas the leading indication for rev-TKA was aseptic loosening (45%). Infection was a more common revision indication for the rev-TKA group (13%) than for the rev-UKA group (2%).
Table 2.
Indication for revision arthroplasty
| Reason for revision | Rev-UKA (n = 68) | Rev-TKA (n = 112) | Chi square p value |
|---|---|---|---|
| Progression of arthritis | 33 (48%) | 1 (1%) | < 0.001 |
| All other reasons | 35 (52%) | 111 (99%) | |
| Aseptic loosening | 16 (24%) | 50 (45%) | 0.004 |
| All other reasons | 52 (76%) | 62 (55%) | |
| Wear/osteolysis | 14 (21%) | 20 (18%) | 0.65 |
| All other reasons | 54 (79%) | 92 (82%) | |
| Infection | 1 (2%) | 14 (13%) | 0.009 |
| All other reasons | 67 (98%) | 98 (87%) |
Rev-UKA = unicompartmental knee arthroplasty revision; rev-TKA = TKA revision.
Data maintained in the registry allowed for identification and subsequent analysis of several variables, including patient factors (date of primary and revision surgery, gender, age, diagnosis at the time of the index procedure, discharge disposition), indication for revision surgery, operative time, components necessary for revision (patellar resurfacing, tibial polyethylene insert thickness, number of wedges, number of stems), and implant costs and hospital charges.
Univariate analyses were performed using Pearson’s chi square for categorical variables (patellar resurfacing, metal augmentation, stems, diagnosis at index procedure, indication for revision surgery, discharge disposition, and gender) and Student’s t test for continuous variables (polyethylene insert thickness, operative time, time to revision, implant costs and hospital charges, and age). Cumulative revision rates (CRRs) were calculated using the Kaplan-Meier method. The log-rank test was used to compare survival between rev-UKA and rev-TKA groups. Hazard ratios were calculated using the Cox proportional-hazards model.
Results
Rev-UKA was predictably less complex and resulted in less bone loss , as reflected by lower use of modular metal stems and augments and greater use of thinner polyethylene inserts than rev-TKA (Table 3). The mean polyethylene liner thickness for the tibial insert was greater (p < 0.001) for the rev-TKA group (15.5 mm; range, 8–30 mm) than for the rev-UKA group (12.8 mm; range, 8–25 mm). More (p < 0.001) rev-TKAs (39 of 112 or 35%) had more than one femoral or tibial metal augment than did rev-UKAs (none of 68 or 0%). More (p < 0.001) rev-TKAs had two stemmed components than did rev-UKAs (42 of 112 or 39% versus one of 68 or 1%, respectively). Thirty-nine of 68 rev-UKAs (57%) did not have metal augments, stemmed components, or bone graft at the time of revision surgery and therefore were revised as primary TKAs. Lower complexity also was reflected by lower (p < 0.001) operative time for rev-UKAs (mean = 105 minutes; SD = 44 minutes) compared with rev-TKAs (mean = 152 minutes; SD = 54 minutes).
Table 3.
Revision components
| Component | Rev-UKA (n = 68) | Rev-TKA (n = 112) | p value* |
|---|---|---|---|
| Polyethylene liner thickness (mm)† | 8–25 (12.8) | 8–30 (15.5) | < 0.001 |
| Wedges | |||
| 0 | 52 (77%) | 56 (50%) | < 0.001 |
| 1 | 16 (23%) | 17 (15%) | |
| > 1 | 0 (0%) | 39 (35%) | |
| Stems | |||
| 0 | 50 (74%) | 34 (30%) | < 0.001 |
| 1 | 17 (25%) | 34 (30%) | |
| 2 | 1 (1%) | 44 (39%) |
* Student’s t test for comparison of polyethylene liner thickness and Pearson’s chi square test for comparisons of wedges and stems; †values expressed as means, with ranges in parentheses; rev-UKA = unicompartmental knee arthroplasty revision; rev-TKA = TKA revision.
Lower implant costs (p < 0.001) and hospital charges (p = 0.002) were found for rev-UKAs. No differences (p = 0.92) were found for length of patient hospitalization after rev-UKAs and rev-TKAs (Table 4). Likewise, discharge disposition was similar (p = 0.384), with 70.6% of patients having rev-UKAs and 64.3% of patients having rev-TKAs discharged home.
Table 4.
Hospitalization and related costs
| Variable | Rev-UKA (n = 68) | Rev-TKA (n = 112) | Chi square p value |
|---|---|---|---|
| Length of hospitalization | |||
| < 5 days | 42 (62%) | 70 (63%) | 0.92 |
| ≥ 5 days | 26 (38%) | 42 (37%) | |
| Cost of hospitalization | |||
| < $33,000 | 51 (75%) | 58 (52%) | 0.002 |
| ≥ $33,000 | 17 (25%) | 54 (48%) | |
| Cost of revision implant | |||
| < $5200 | 60 (88%) | 65 (58%) | < 0.001 |
| ≥ $5200 | 8 (12%) | 47 (42%) |
Rev-UKA = unicompartmental knee arthroplasty revision; rev-TKA = TKA revision.
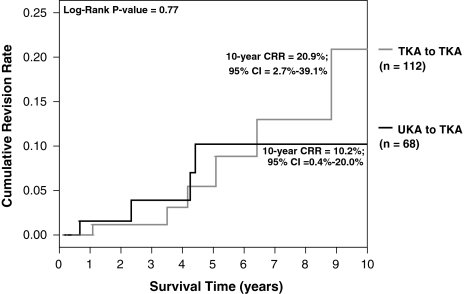
The secondary cumulative revision rates were similar (p = 0.55) for rev-UKA and rev-TKA groups (Fig. 1). Four of the 68 rev-UKAs (4.4%) were revised for a second time; seven of the 112 rev-TKAs (6.3%) were rerevised. Rev-UKAs did not differ from rev-TKAs in the likelihood of undergoing a second revision (hazard ratio = 0.48; confidence interval, 0.13–1.80).
Fig. 1.
The graph shows the secondary cumulative revision rate (CRR) by primary revision type. CI = confidence interval.
Discussion
When a UKA fails, revision to TKA generally is recommended [17]. Numerous studies have cited consistent modes of UKA failure, including progressive adjacent compartment arthritis, aseptic femoral or tibial component loosening, and polyethylene wear [3, 4, 6, 9, 16, 17, 24, 25]. We sought to determine how rev-UKAs perform in a community registry population in comparison to rev-TKAs. In particular, we were interested in the relative complexity, cost, and survival of these two revision procedures.
Limitations of this study include the relatively small population and those inherent to any registry population, where a small percentage of patients (estimated at 6% in the HealthEast Joint Registry [10]) may seek revision surgery elsewhere and where revision itself is the end point measured. We cannot comment, therefore, on impending revisions, poor radiographic or clinical results in either group, or patients who may have deferred additional surgery secondary to medical comorbidities. The use of metal augments and stems and operative time were used as proxies for bone loss and complexity of the surgical procedure, although many other factors that add to surgical complexity are not part of the registry database. Similarly, because numerous surgeons performed the revision surgeries, indications for the procedure and surgical techniques undoubtedly varied. However, such results may be more generalizable to the community population and to the general orthopaedist than those seen in specialized centers.
Early investigations reported technical difficulty during rev-UKAs, citing substantial bone loss requiring grafting, the need for stemmed revision components, or the need for custom implants [20]. More recently, rev-UKA has been described as less technically demanding than rev-TKA [4, 6, 14, 16, 18, 23, 24], perhaps as a result of improvements in prosthetic design [16, 23]. The results of our study provide additional evidence that rev-TKA is technically more complex than rev-UKA, using the proxy of need for metal augmentation and stems and operative time. Rev-TKA had increased requirements for metal wedge augments and stemmed femoral or tibial components when compared with rev-UKA and required greater operative time. Also, the mean polyethylene insert thickness was greater for a rev-TKA than for a rev-UKA. In our study, 57% of the rev-UKAs were performed without having metal wedges, stemmed components, or supplemental bone graft, thus allowing the revision surgery to be performed essentially as a primary TKA. These findings provide evidence attesting to the relative bone-sparing nature of modern UKA as an index arthroplasty, with decreased technical requirements at the time of revision surgery when compared with rev-TKA. Previously reported revision requirements at the time of rev-UKA are provided for comparison (Table 5).
Table 5.
Revision requirements at time of rev-UKA
| Study | % rev-UKA performed as primary TKA | Bone graft | Cement ± screw augmentation | Stems | Wedges |
|---|---|---|---|---|---|
| Barrett and Scott [3] | 55% (16/29) | 10% | 17% | 7% femur | 3% |
| 14% femur/tibia | |||||
| Padgett et al. [20] | 24% (5/21) | 14% | 43% | NR | 5% |
| Levine et al. [16] | 48% (15/31) | 23% | NR | 6% femur | 19% |
| 3% tibia | |||||
| McAuley et al. [18] | 31% (10/32) | 31% | NR | 0% femur | 25% |
| 44% tibia | |||||
| Springer et al. [24] | 32% (7/22) | 27% femur | NR | 0% femur | 23% |
| 45% tibia | 9% tibia | ||||
| Saldanha et al. [23] | 78% (28/36) | 6% femur | 6% tibia | 17% | 6% |
| Current study | 57% (39/68) | NR | 0% | 26% | 23% |
Rev-UKA = unicompartmental knee arthroplasty revision; NR = not reported.
As anticipated, we found differences between the rev-UKA and rev-TKA groups in terms of implant costs and hospital charges. More patients who had rev-TKAs had implant costs greater than $5200 and hospital charges greater than $33,000 compared with patients who had rev-UKAs. As there was no difference found in length of hospitalization between the groups or in discharge disposition, the difference in hospital charges undoubtedly reflects the higher surgical/perioperative costs associated with the costlier implants and longer operating time.
In our registry, the CRR is higher for primary UKA compared with TKA, indicating a decreased overall survivorship for UKA compared with TKA, a finding consistent with those reported previously [8, 9, 15, 17, 20]. In contrast, no difference was found in the secondary CRR between the rev-UKA and rev-TKA groups. Despite the fact that rev-TKA was technically more challenging compared with rev-UKA in terms of the requirement for stems and metal augmentation at the time of revision surgery and the greater operative time, the secondary survival of rev-UKAs and rev-TKAs was similar. This may reflect the morbidity associated with the rev-TKA and a tendency for the patient to autoprotect the multiply operated prosthetic knee or defer additional surgery, the limitations inherent to a registry if additional revision operations were performed outside the registry capture area, or the relatively small numbers of rerevisions performed in both groups.
In our community registry, rev-UKA is a reliable and relatively economical procedure when performed by the community orthopaedic surgeon. A substantial proportion may be revised to primary TKA designs without the need for stems or metal augmentation, but survival in this population was no better than in the rev-TKA population.
Acknowledgments
We thank the many surgeons responsible for the success of the HealthEast Joint Registry.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
References
- 1.Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg Am. 2002;84:2235–2239. [PubMed]
- 2.Bae DK, Guhl JF, Keane SP. Unicompartmental knee arthroplasty for single compartment disease: clinical experience with an average four-year follow-up study. Clin Orthop Relat Res. 1983;176:233–238. [PubMed]
- 3.Barrett WP, Scott RD. Revision of failed unicondylar unicompartmental knee arthroplasty. J Bone Joint Surg Am. 1987;69:1328–1335. [PubMed]
- 4.Bohm I, Landsiedl F. Revision surgery after failed unicompartmental knee arthroplasty: a study of 35 cases. J Arthroplasty. 2000;15:982–989. [DOI] [PubMed]
- 5.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following unicompartmental or bicompartmental knee arthroplasty: a meta-analysis. J Arthroplasty. 1995;10:141–150. [DOI] [PubMed]
- 6.Chakrabarty G, Newman JH, Ackroyd CE. Revision of unicompartmental arthroplasty of the knee: clinical and technical considerations. J Arthroplasty. 1998;13:191–196. [DOI] [PubMed]
- 7.Chesnut WJ. Preoperative diagnostic protocol to predict candidates for unicompartmental arthroplasty. Clin Orthop Relat Res. 1991;273:146–150. [PubMed]
- 8.Deshmukh RV, Scott RD. Unicompartmental knee arthroplasty: long-term results. Clin Orthop Relat Res. 2001;392:272–278. [DOI] [PubMed]
- 9.Gioe TJ, Killeen KK, Hoeffel DP, Bert JM, Comfort TK, Scheltema K, Mehle S, Grimm K. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003;416:111–119. [DOI] [PubMed]
- 10.Gioe TJ, Killeen KK, Mehle S, Grimm K. Implementation and application of a community total joint registry: a twelve-year history. J Bone Joint Surg Am. 2006;88:1399–1404. [DOI] [PubMed]
- 11.Heck DA, Marmor L, Gibson A, Rougraff BT. Unicompartmental knee arthroplasty: a multicenter investigation with long-term follow-up evaluation. Clin Orthop Relat Res. 1993;286:154–159. [PubMed]
- 12.Inglis GS. Unicompartmental arthroplasty of the knee: a follow-up of 3 to 9 years. J Bone Joint Surg Br. 1984;66:682–684. [DOI] [PubMed]
- 13.Insall J, Walker P. Unicondylar knee replacement. Clin Orthop Relat Res. 1976;120:83–85. [PubMed]
- 14.Johnson S, Jones P, Newman JH. The survivorship and results of total knee replacements converted from unicompartmental knee replacements. Knee. 2007;14:154–157. [DOI] [PubMed]
- 15.Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128–135. [DOI] [PubMed]
- 16.Levine WN, Ozuna RM, Scott RD, Thornhill TS. Conversion of failed modern unicompartmental arthroplasty to total knee arthroplasty. J Arthroplasty. 1996;11:797–801. [DOI] [PubMed]
- 17.Lewold S, Robertsson O, Knutson K, Lidgren L. Revision of unicompartmental knee arthroplasty: outcome in 1,135 cases from the Swedish Knee Arthroplasty study. Acta Orthop Scand. 1998;69:469–474. [DOI] [PubMed]
- 18.McAuley JP, Engh GA, Ammeen DJ. Revision of failed unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2001;392:279–282. [DOI] [PubMed]
- 19.Naudie D, Guerin J, Parker DA, Bourne RB, Rorabeck CH. Medial unicompartmental knee arthroplasty with the Miller-Galante prosthesis. J Bone Joint Surg Am. 2004;86:1931–1935. [DOI] [PubMed]
- 20.Padgett DE, Stern SH, Insall JN. Revision total knee arthroplasty for failed unicompartmental replacement. J Bone Joint Surg Am. 1991;73:186–190. [PubMed]
- 21.Rajasekhar C, Das S, Smith A. Unicompartmental knee arthroplasty: 2- to 12-year results in a community hospital. J Bone Joint Surg Br. 2004;86:983–985. [DOI] [PubMed]
- 22.Robertsson O, Borgquist L, Knutson K, Lewold S, Lidgren L. Use of unicompartmental instead of tricompartmental prostheses for unicompartmental arthrosis in the knee is a cost-effective alternative: 15,437 primary tricompartmental prostheses were compared with 10,624 primary medial or lateral unicompartmental prostheses. Acta Orthop Scand. 1999;70:170–175. [DOI] [PubMed]
- 23.Saldanha KA, Keys GW, Svard UC, White SH, Rao C. Revision of Oxford medial unicompartmental knee arthroplasty to total knee arthroplasty: results of a multicentre study. Knee. 2007;14:275–279. [DOI] [PubMed]
- 24.Springer BD, Scott RD, Thornhill TS. Conversion of failed unicompartmental knee arthroplasty to TKA. Clin Orthop Relat Res. 2006;446:214–220. [DOI] [PubMed]
- 25.Squire MW, Callaghan JJ, Goetz DD, Sullivan PM, Johnston RC. Unicompartmental knee replacement: a minimum 15 year followup study. Clin Orthop Relat Res. 1999;367:61–72. [DOI] [PubMed]
- 26.Svard UC, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of an independent series. J Bone Joint Surg Br. 2001;83:191–194. [DOI] [PubMed]
- 27.Tabor OB Jr, Tabor OB, Bernard M, Wan JY. Unicompartmental knee arthroplasty: long-term success in middle-age and obese patients. J Surg Orthop Adv. 2005;14:59–63. [PubMed]