Abstract
We believe a better way is needed to accurately describe the spectrum of associated injuries that commonly occur in conjunction with a radial head fracture. A review of our institution’s experience with 333 radial head fractures from 1997 to 2002 documented 88 (26%) associated injuries. Based on this clinical experience, our goal was to develop an accurate and comprehensive description of associated injuries. A shorthand suffix method first recognizes the type of radial head fracture with the traditional Mason classification, followed by abbreviations designating the articular injuries, coronoid (c) and olecranon (o), and the ligamentous injuries, lateral collateral ligament (l), medial collateral ligament (m), and distal radioulnar joint (d). The proposed system offers a logical and reproducible (98%) extension of the current Mason fracture classification to document the presence of additional articular and ligamentous injuries. This provides an opportunity to standardize the communication of fracture type with further details of other injuries that ultimately can help with better understanding of treatment outcome based on the precise injury complex.
Introduction
Classification of fractures is useful for several reasons. First, a classification may describe the anatomic characteristics of a fracture or injury; second, it may provide insight regarding the mechanism of injury; third, treatment options may be considered based on the specific classification; fourth, the prognosis may be correlated to the classification of the injury; and fifth, communication of management and outcomes can be standardized through classification systems. The effectiveness of these goals is predicated on the thoroughness by which the injury is described.
Despite the recognized consequences of associated lesions on treatment and outcome, no classification systems or descriptions include this dimension of the injury. Because associated injuries are so important to determine treatment or provide input to suggest prognosis, we developed a system of supplementing the accepted Mason classification [22] to account for the additional complicating injury.
Our objective, therefore, was to offer a means to describe the associated fracture or ligament disruption. This should provide the clinician with an expanded standardized tool to better describe the full extent of the injury. This tool provides classification modifiers after the clinician has made the appropriate diagnosis of the associated injuries. Our intent is simply to more accurately describe and communicate these associated injuries and thus provide a standard for reporting injury, management, and outcome.
Materials and Methods
We recently conducted a retrospective assessment of 372 radial head fractures in patients treated at our institution from 1997 to 2002, 333 of which had occurred in adults [41]. From this group, 118 (35%) had associated fractures or ligamentous injuries of the elbow, wrist, or shoulder. Of these 118 injuries with associated injury, 88 (26%) occurred in the elbow region (Table 1). A detailed assessment of these 88 cases provides the basis of our proposed modification to the Mason classification system. The frequency and type of associated ligamentous and osseous injuries at the elbow and the distal radioulnar joint were tabulated. A simple intuitive method was developed to account for these additional injuries. To determine the ease with which this supplementary material could be communicated, we shared the system with experienced surgeons and surgeons in training. The associated injuries were illustrated in nine representative examples and all scored the accuracy with which the system was applied in these nine cases.
Table 1.
Associated injury involving the elbow in 88 patients by injury type
| Associated injury | Mason fracture type | ||
|---|---|---|---|
| I | II | III | |
| Lateral collateral ligament | 7 | 6 | 22 |
| Medial collateral ligament | 0 | 3 | 2 |
| Medial collateral ligament + lateral collateral ligament | 2 | 4 | 14 |
| Elbow dislocation | 8 | 8 | 29 |
| Fractures at elbow* | 16 | 20 | 42 |
| Distal radioulnar joint | 1 | 1 | 8 |
| Number of patients† | 17 (8%) | 23 (50%) | 48 (75%) |
| Total fractures | 223 | 46 | 64 |
* Excludes the radial head fracture; †multiple injuries in some patients.
Our experience documented 45 elbow dislocations concurrent with 14 coronoid fractures. Eighty-five of the 88 injuries (97%) involved the coronoid, olecranon, medial and/or lateral collateral ligaments, and the distal radioulnar joint. The remaining 3% consisted of fractures of the capitellum and medial epicondyle.
The Mason classification was used to describe the radial head fracture. This classification describes a Type I injury as undisplaced and Type II as a single fragment involving less than 33% of the head and displaced more than 2 mm or a radial neck fracture with greater than 30° angulation. Type III is a comminuted radial head fracture.
Using an approach similar to that adopted by the AO to describe variations in fracture type, we attached a suffix to the radial head fracture type to describe the associated lesions present (Table 2). The suffix denotes the articular injury (c = coronoid, o = olecranon), followed by the ligamentous injury (l = lateral collateral ligament, m = medial collateral ligament, d = distal radioulnar joint).
Table 2.
Comprehensive classification of radial head fracture with description of associated injuries*
| Radial head fracture (Mason) type | Associated injury suffixes | |
|---|---|---|
| I–III | Articular injuries | c = coronoid fracture |
| o = olecranon fracture | ||
| Ligamentous injuries | m = medial collateral ligament | |
| l = lateral collateral ligament | ||
| d = distal radioulnar disruption | ||
* The suffixes are used in the order shown (for examples, see Figs. 1 and 2).
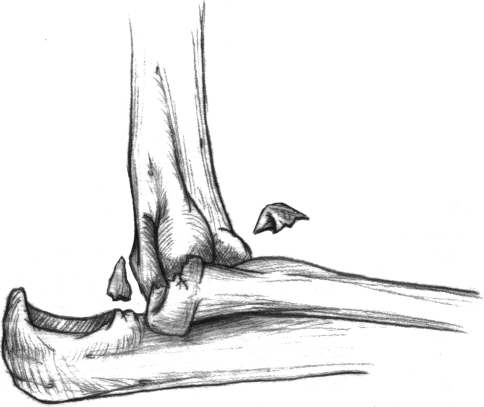
Thus, a comminuted fracture of the radial head, a Mason Type III fracture, with an elbow dislocation but without other injury is termed Type III lm (Fig. 1). This describes the medial and lateral collateral ligament injury that occurs with the dislocation and designates the comminuted radial head fracture. Similarly, the designation of a Type II radial head fracture with a coronoid fracture and dislocation is termed Type II clm (Fig. 2). Although at first glance this may seem awkward, the system is simple and allows designation of most (97%) of these associated injuries documented from the review of the larger sample of 333 fractures. The capitellar fracture is so rare that it is not included in the proposed system.
Fig. 1.
The diagram illustrates an elbow injury consisting of a Mason Type III radial head fracture and dislocation, which is termed Type III lm, indicating injury to the medial (m) and lateral (l) collateral ligaments with a comminuted radial head fracture (III).
Fig. 2.
A diagram illustrates a Mason Type II fracture with dislocation and coronoid fracture described as a Type II clm injury.
The next step was to attain some sense of the ease with which this modification may be applied to the Mason system. Nine radial head fractures with associated disorders were presented using a written description and graphic illustration to 18 board-certified surgeons and to nine orthopaedic residents in the fourth and fifth years of training. There were 22 associated injuries complicating the nine radial head fractures. The complete injury was clearly illustrated for each radial head fracture. The surgeons were asked to describe the associated injuries using the shorthand descriptive methodology described. After one 10-minute description of the system, the ease of which the system could be learned and applied was documented.
We consulted with a statistician experienced in validating clinical measurement instruments. After review of this methodology, it was concluded this study was similar to simply grading an objective multiple-choice test. Therefore, it did not have features that required interobserver or intraobserver validation.
Results
Eleven of 18 board-certified surgeons and six of nine residents scored a perfect 22 of 22. Nine missed accurately categorizing one lesion and one surgeon incorrectly described two injury patterns. Overall, there were 594 (22 × 27) possibilities for accurate description. Of these 594, 583 (98%) of the associated injuries were recognized correctly by the residents and established surgeons after one discussion and exposure to the proposed system.
Discussion
A review of the literature reveals the first classification of radial head fractures was described by Speed [38] in 1924 who made a distinction between complete and incomplete fractures of the head and neck. All subsequent classification systems have focused on the fracture type with virtually no mention of associated trauma [5, 14, 16, 22]. Mason [22] did suggest treatment options according to fracture type: Type I was to be treated nonoperatively; Type II might be treated nonoperatively or the radial head could be resected, depending on fragment size; and the radial head should be resected in Type III fractures [22].
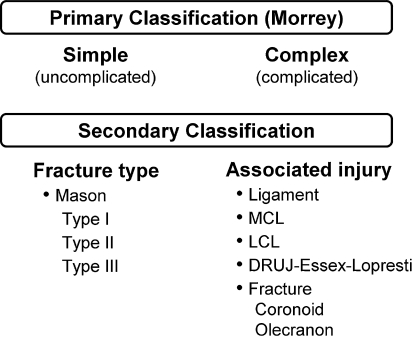
Associated lesions are recognized [16] to influence treatment of the radial head fracture [11, 12, 34, 40]. Outcome not only depends on the fracture type but also on associated lesions to the elbow and wrist [6, 12, 33, 35, 39]. Although not included in the Mason classification [22], Johnston [17] recognized implications of the fracture dislocation, which subsequently was termed a Type IV fracture. Hotchkiss [14] suggested changes to the Mason classification emphasizing consideration of treatment options to specific types of fracture, essentially leaving the Mason classification unchanged as Table 3 shows Hotchkiss’ classification. Although mentioned, associated lesions were not specifically considered in this scheme. Morrey [25, 26] emphasized the importance of the associated injuries recommended an additional consideration by dividing all radial head fractures into simple and complex depending on the presence or absence of associated lesions (Fig. 3). This distinction was offered to better reflect the increasing awareness of the biomechanical function of the radial head [9, 30] the results of resection [28], effectiveness of prosthetic replacement [3] and the prognostic impact of other fractures and ligament injuries [3, 39]. Details of how the spectrum of additional injuries is described were not proposed.
Table 3.
Hotchkiss [14] expansion of the Mason classification [22] of radial head fractures emphasizing the need for and type of intervention by fracture type*
| Fracture type | Fracture description | Type of intervention |
|---|---|---|
| I | Non/minimally displaced head or neck fracture < 2 mm displacement or marginal | No mechanical block |
| Nonoperative management | ||
| II | Displaced fracture (> 2 mm) of the head or neck (angulated) | Possible mechanical block |
| Open reduction with internal fixation | ||
| III | Severely comminuted fracture of the head and neck | Not reconstructible |
| Excision for movement |
* No recognition for associated injury is provided; Adapted and published with permission from: Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1–10.
Fig. 3.
The diagram depicts the evolution of the current classification system. The broad designation of complicated or uncomplicated is expanded to recognize the ligamentous and articular injuries that potentially may complicate any of the Mason I to III types of radial head fractures. MCL = medial collateral ligament; LCL = lateral collateral ligament; DRUJ = distal radioulnar joint.
Neither the Mason [22] nor the Hotchkiss [14] classification addresses decision making in the context of concurrent injury. It is accepted a concurrent ligament injury with a badly comminuted radial head is the ideal indication of prosthetic replacement [8, 12, 13, 30, 37]. Data exist to suggest a comminuted radial head fracture with an associated medial collateral ligament lesion should be addressed by open reduction and internal fixation or, if this is not possible, by prosthetic replacement of the radial head [7, 8, 18, 21, 24, 27]. If there are no additional injuries, resection still is considered appropriate management by some [2, 15, 19, 42]. Describing this injury either with or without the ligament injury is essential to understand the basis of the treatment rendered.
Our proposal does not suggest how to make the diagnosis of associated injury or how the injury complex should be treated. The literature already provides this information, relying principally on MRI and computed tomography reconstruction to delineate soft tissue and articular injuries, respectively [4, 10, 20, 23, 31]. However, once the full extent of the injury is diagnosed, the present proposal offers a logical and systematic process of describing the broad spectrum of articular and ligamentous disease in conjunction with the accepted Mason classification of the type of radial head fracture. The proposed description makes no attempt to offer insights to treatment. The preferred management of the various combinations of osseous and ligamentous injuries is now emerging and being documented in the literature [1–3, 8, 11, 12, 14, 24, 25, 29, 30, 32, 34–36, 40]. Our interpretation of the current thinking regarding management of radial head fractures with associated injuries is summarized as follows.
Whenever possible, the radial head should be preserved or replaced if there is an associated ligamentous or articular injury involving the elbow or the distal radioulnar joint. When possible, open reduction and internal fixation is preferable over prosthetic replacement. Prosthetic replacement is recommended when the radial head cannot be reliably fixed. Fractures of the radial head must be addressed and its function preserved with fractures involving greater than 50% of the coronoid. However, the intent of this article is not to describe the complex array of fractures or their treatment. The intent is to provide a descriptive basis of the abnormalities once the extent of the injury is known. In so doing, treatment and outcome can be described more accurately in a standardized fashion based on the full extent of the injury.
In addition, the proposed system excluded 3% of associated injuries. To address these 3% would require a degree of complexity not justified by the enhanced complexity of the proposed system. Finally, for the sake of clarity and simplicity, we did not include a method to describe whether and how the additional injuries were or could be treated. The proposed system can be extended easily to reflect such information; however, we think it would add to the complexity of the communication and concept and thus it is not included in this manuscript.
The proposed method of injury description was designed to be intuitive, thus minimizing the need for formal memorization because 98% of associated injuries were correctly documented with one orientation session. Furthermore, the system is comprehensive but not all-inclusive: it accurately accounts for 85 of the 88 (97%) radial head fractures and associated elbow injuries in our series. If injuries are described in the manner proposed, it provides a basis for evaluation, treatment, and communication. Therefore, we believe this proposal offers a valuable basis and foundation for future treatment recommendations.
Acknowledgments
We acknowledge William S. Harmsen, MS, from the Mayo Clinic, Department of Statistics, Department of Health Science, for assistance in the evaluation of the data collected in this study.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Andrews JR, Heggland EJ, Fleisig GS, Zheng N. Relationship of ulnar collateral ligament strain to amount of medial olecranon osteotomy. Am J Sports Med. 2001;29:716–721. [DOI] [PubMed]
- 2.Boulas HJ, Morrey BF. Biomechanical evaluation of the elbow following radial head fracture: comparison of open reduction and internal fixation vs. excision, silastic replacement, and non-operative management. Chir Main. 1998;17:314–320. [DOI] [PubMed]
- 3.Broberg MA, Morrey BF. Results of treatment of fracture-dislocations of the elbow. Clin Orthop Relat Res. 1987;216:109–119. [PubMed]
- 4.Carrino JA, Morrison WB, Zou KH, Steffen RT, Snearly WN, Murray PM. Lateral ulnar collateral ligament of the elbow: optimization of evaluation with two-dimensional MR imaging. Radiology. 2001;218:118–125. [DOI] [PubMed]
- 5.Cutler C. Fractures of the head and neck of the radius. Ann Surg. 1926;8:267–268. [DOI] [PMC free article] [PubMed]
- 6.Edwards GS Jr, Jupiter JB. Radial head fractures with acute distal radioulnar dislocation: Essex-Lopresti revisited. Clin Orthop Relat Res. 1988;234:61–69. [PubMed]
- 7.Esser RD, Davis S, Taavao T. Fractures of the radial head treated by internal fixation: late results in 26 cases. J Orthop Trauma. 1995;9:318–323. [DOI] [PubMed]
- 8.Furry KL, Clinkscales CM. Comminuted fractures of the radial head: arthroplasty versus internal fixation. Clin Orthop Relat Res. 1998;353:40–52. [DOI] [PubMed]
- 9.Geel CW, Palmer AK. Radial head fractures and their effect on the distal radioulnar joint: a rationale for treatment. Clin Orthop Relat Res. 1992;275:79–84. [PubMed]
- 10.Haapamaki VV, Kiuru MJ, Koskinen SK. Multidetector computed tomography diagnosis of adult elbow fractures. Acta Radiol. 2004;45:65–70. [DOI] [PubMed]
- 11.Hammacher ER, van der Werken C. Radial head fractures: operative or conservative treatment? The Greek temple model. Acta Orthop Belg. 1996;62(suppl 1):112–115. [PubMed]
- 12.Harrington IJ, Sekyi-Otu A, Barrington TW, Evans DC, Tuli V. The functional outcome with metallic radial head implants in the treatment of unstable elbow fractures: a long-term review. J Trauma. 2001;50:46–52. [DOI] [PubMed]
- 13.Holmenschlager F, Halm JP, Winckler S. Les fractures fraîches de la tête radiale: résultants de la prothèse à cupule flottant de Judet. Rev Chir Orthop Reparatrice Appar Mot. 2002;88:387–397. [PubMed]
- 14.Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1–10. [DOI] [PubMed]
- 15.Janssen RP, Vegter J. Resection of the radial head after Mason type-III fractures of the elbow: follow-up at 16 to 30 years. J Bone Joint Surg Br. 1998;80:231–233. [DOI] [PubMed]
- 16.Johanson O. Capsular and ligamentous injuries of the elbow. Acta Chir Scand. 1962;287(suppl):21–29. [PubMed]
- 17.Johnston GW. A follow-up of one-hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med J. 1962;31:51–56. [PMC free article] [PubMed]
- 18.Kanlic E, Perry CR. Indications and technique of open reduction and internal fixation of radial head fractures. Orthopedics. 1992;15:837–842. [DOI] [PubMed]
- 19.Khalfayan EE, Culp RW, Alexander AH. Mason type II radial head fractures: operative versus nonoperative treatment. J Orthop Trauma. 1992;6:283–289. [DOI] [PubMed]
- 20.Kijowski R, Tuite M, Sanford M. Magnetic resonance imaging of the elbow. Part II: abnormalities of the ligaments, tendons and nerves. Skeletal Radiol. 2005;34:1–18. [DOI] [PubMed]
- 21.King GJ, Evans DC, Kellam JF. Open reduction and internal fixation of radial head fractures. J Orthop Trauma. 1991;5:21–28. [DOI] [PubMed]
- 22.Mason ML. Some observations on fractures of the head of the radius with a review of one hundred cases. Br J Surg. 1954;42:123–132. [DOI] [PubMed]
- 23.Miller TT, Adler RS, Friedman L. Sonography of injury of the ulnar collateral ligament of the elbow: initial experience. Skeletal Radiol. 2004;33:386–391. [DOI] [PubMed]
- 24.Moro JK, Werier J, MacDermid JC, Patterson SD, King GJ. Arthroplasty with a metal radial head for unreconstructible fractures of the radial head. J Bone Joint Surg Am. 2001;83:1201–1211. [DOI] [PubMed]
- 25.Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect. 1995;44:175–185. [PubMed]
- 26.Morrey BF. Fractures of the distal humerus: role of elbow replacement. Orthop Clin North Am. 2000;31:145–154. [DOI] [PubMed]
- 27.Morrey BF. Radial head fracture. In: Morrey BF, ed. The Elbow and Its Disorders. Philadelphia PA: WB Saunders; 2000:341–364.
- 28.Morrey BF, Chao EY, Hui FC. Biomechanical study of the elbow following excision of the radial head. J Bone Joint Surg Am. 1979;61:63–68. [PubMed]
- 29.Morrey BF, Tanaka S, An KN. Valgus stability of the elbow: a definition of primary and secondary constraints. Clin Orthop Relat Res. 1991;265:187–195. [PubMed]
- 30.Popovic N, Gillet P, Rodriguez A, Lemaire R. Fracture of the radial head with associated elbow dislocation: results of treatment using a floating radial head prosthesis. J Orthop Trauma. 2000;14:171–177. [DOI] [PubMed]
- 31.Potter HG, Ho ST, Altchek DW. Magnetic resonance imaging of the elbow. Semin Musculoskelet Radiol. 2004;8:5–16. [DOI] [PubMed]
- 32.Rettig AC, Sherrill C, Snead DS, Mendler JC, Mieling P. Nonoperative treatment of ulnar collateral ligament injuries in throwing athletes. Am J Sports Med. 2001;29:15–17. [DOI] [PubMed]
- 33.Ring D, Jupiter JB, Simpson NS. Monteggia fractures in adults. J Bone Joint Surg Am. 1998;80:1733–1744. [DOI] [PubMed]
- 34.Ring D, Jupiter JB, Zilberfarb J. Posterior dislocation of the elbow with fractures of the radial head and coronoid. J Bone Joint Surg Am. 2002;84:547–551. [DOI] [PubMed]
- 35.Ring D, Quintero J, Jupiter JB. Open reduction and internal fixation of fractures of the radial head. J Bone Joint Surg Am. 2002;84:1811–1815. [DOI] [PubMed]
- 36.Rohrbough JT, Altchek DW, Hyman J, Williams RJ 3rd, Botts JD. Medial collateral ligament reconstruction of the elbow using the docking technique. Am J Sports Med. 2002;30:541–548. [DOI] [PubMed]
- 37.Smets S, Govaers K, Jansen N, Van Riet R, Schaap M, Van Glabbeek F. The floating radial head prosthesis for comminuted radial head fractures: a multicentric study. Acta Orthop Belg. 2000;66:353–358. [PubMed]
- 38.Speed K. Traumatic lesions of the head of the radius: relation to elbow joint dysfunction. Surg Clin North Am. 1924;4:651–656.
- 39.Trousdale RT, Amadio PC, Cooney WP, Morrey BF. Radio-ulnar dissociation: a review of twenty cases. J Bone Joint Surg Am. 1992;74:1486–1497. [PubMed]
- 40.Van Glabbeek F, van Riet R, Verstreken J. Current concepts in the treatment of radial head fractures in the adult: a clinical and biomechanical approach. Acta Orthop Belg. 2001;67:430–441. [PubMed]
- 41.van Riet RP, Morrey BF, O’Driscoll SW, Van Glabbeek F. Associated injuries complicating radial head fractures: a demographic study. Clin Orthop Relat Res. 2005;441:351–355. [DOI] [PubMed]
- 42.Wallenböck E, Pötsch F. Resection of the radial head: an alternative to use of a prosthesis? J Trauma. 1997;43:959–961. [DOI] [PubMed]