Abstract
Historians have the opportunity of viewing events, people, and their epoch through an aperture in time. With retrospective clarity, change and the forces effecting change can be appropriately categorized, emphasized, and interpreted. Sociologists see change in a forward-focused manner. When we examine our patients today, it is clear our current patients having total joint arthroplasty are different from those in years past. The sociologic influences effecting this change are many and include the revolutionary explosion of, access to, and dissemination of information; increased wealth, life activity expectation, and life expectancy; and an aging workforce. Concurrent with these forces registering change in our patient population is an erosion in respect for professionalism and vertically oriented authoritarian structure throughout society. Our patients are citizens of our modern age. Our public has come to expect miracles in medicine as the norm, yet these miracles are not without inherent risk. The trap implicit in allowing an incompletely informed populace to drive the decisions we make may be bridged by a more complete understanding of who our patients are and what their needs include. This discussion attempts to offer some insight into the forces at play. It focuses on how the changes in society, population, and technology have affected patients’ knowledge and attitude toward medicine and what our response as physicians should be.
Introduction
After nearly 40 years of development, modern-era total joint arthroplasty appears to have reached a virtual apogee. The designs are successful, the technologies are well studied, and our patients do well after surgery. However, a true apogee, from our patients’ perspective, remains before us. Just as techniques used in total joint arthroplasty have evolved, embracing improvement in fixation techniques and bearing surfaces, the patients for whom these devices are designed have changed as well.
We are experiencing in this modern era of total joint arthroplasty demographic and social trends, well underway, which will continue to influence whom we see in our offices. Yogi Berra said, “The future ain’t what it used to be” [1]. Although we have made substantial strides since the introduction of total joint arthroplasty surgery regarding techniques and implant design, these surgeries now often are performed in an increasingly demanding and active patient population, characteristics that likely will influence the outcomes of current designs and the development of future strategies.
In our time, demographic change, education, affluence, availability of information, patient mobility, direct-to-consumerism, patient age, patient activity demands, cost pressures, and physician accountability all converge to present the practitioner with a patient who is more informed and has higher expectations (and sometimes is more demanding) than any prior generation of patients undergoing joint arthroplasty. In the past, it was widely held, when a person reached 50 years of age, he or she had reached the brink of old age. By the time they reached 65 years of age, a person was believed well on the way into elder years of decline. However, if we examine and compare our patient populations with those in years past, it becomes clear there exists a ‘boomer mentality’ that embraces youth and rebukes the traditional stereotypes of aging. I will focus on how the changes in society, population, and technology have affected our patients’ knowledge and attitude toward medicine and what I believe our response as physicians should be.
Demographics are Changing
On October 17, 2006, the United States reached a milestone becoming only the third country in the world to have a population greater than 300 million. It took this country more than 150 years to reach 100 million. We reached 200 million in 1967, and less than 40 years later, we have reached the 300 million mark. In a mere 35 years, we are projected to reach 400 million [20]. Population growth occurs naturally with an excess of births over deaths. However, this \ accounts for only 60% of our current annual growth in the United States [20]. International immigration, legal and illegal, accounts for the additional 40% of US population growth and will effect a profound transformation of the ethnic and social constituencies [20].
For all of medicine and society, it is important we take note of another growth trend in this country, that of the aging of America. Currently, a baby boomer turns 50 every 7.5 seconds [27]. The noted social scientist Peter F. Drucker has said, “The extreme youth culture of the last 40 years was based on demographics. It’s an age-old rule that the population group that is both the biggest and growing the fastest determines the mood” [27]. In the United States, there are 76 million baby boomers, the largest single-age demographic in our population.
In addition to aging and growth trends, patients have realized higher activity levels, improved general access to health care, and improved economic security; they are living longer, are better educated, and, unfortunately, are more obese. The percentage of Americans older than 25 years who finished high school soared dramatically from 55% in 1970 to 85% in 2004 [32]. Increase in educational achievement is reflected in economic status and sense of security in the general population; yet, it is clear the rate of improvement in economic growth is not proportional across all racial and socioeconomic classes [13].
As a percentage of the US population, those older than 65 years have increased from 6.7% of all Americans in 1960 to 12.4% in 2000. The number of Americans older than 65 years is expected to increase some 70 million by 2030 [21].
Additionally, in Americans, the body mass index has increased with age through the sixth decade [11]. This trend is particularly disturbing when we reflect on the fact Americans are experiencing a sharp increase in the prevalence of obesity in our population in general. In fact, the majority of Americans aged 60 to 79 years have a body mass index in the overweight or obese range [14]. These obese patients report higher incidences of activity-limiting osteoarthritis [26] and have an increased risk of having osteoarthritis develop when compared with normal-weight adults [16, 19, 33]. In the knee, the literature showing the relationship between increased body mass index and osteoarthritis is clear [17, 22, 24, 29]; however, this relationship in the hip has been inconsistent, with some studies reporting no relationship [17, 29] and others showing a direct correlation [15, 24, 25]. If we add these two factors alone, an aging populace that is ever more obese, the effect on the number of arthroplasties is profound [8, 14, 26].
Another important demographic with sociologic consequence is the slow disappearance of the multiperson household. With older patients living longer and youth moving out and delaying marriage, the number of one-person households is increasing. With this trend toward social isolation comes a subsequent reliance on the media, underscoring the importance of information conveyance in our society.
The Information Revolution
As orthopaedic surgeons, we are inundated with patients in our offices who present not simply with a chief complaint but desiring a particular operation and sometimes even a particular implant. The information revolution impacts every aspect of our society, including our relationships with our patients. The physician is no longer the sole source of medical information and patients often are equipped with enough snippets of information to stimulate a dialogue expressing their expectations for an outcome and techniques to achieve that outcome. As a result, the doctor-patient relationship has, in a sense, been democratized, with the patient, surgeon, and industry all influencing the decision process.
The information revolution is simply defined as the explosion of not only the acquisition of information but also its dissemination. It is difficult now to remember a world in which the Internet did not have its current level of influence. Underpinned by the Internet, the information revolution encroaches on our human sensibilities, delivering an unending stream of new data at an ever-accelerating pace. This information challenges us to review and react to changes at a far greater pace than any generation in history.
Society Readily Accepts the Amplification
Throughout history, knowledge was spread primarily by proximity. In the modern information era, we are now experiencing exponential growth of information and the combination of information streams. As a single media source reveals a story, it is quickly amplified on traditional and nontraditional media, such as blogs, podcasts, and YouTube, creating a story out of a story.
As our lives become increasingly pressured by the information available to us at work and at leisure, we express this pressure, or time conscientiousness, by multiplying our attention streams. We know this time conscientiousness as multitasking. Our complex modern civilization has adopted a proclivity for productivity and time efficiency, which has become ingrained in our collective psyche. Citizens of this modern age have become accustomed to interaction with their increasingly complex environment. As a result, we expect to direct, engage, and control our environment in ways no other generation has before us.
The connectivity of the modern world has resulted in an economy that works 7 days a week, placing a distinct awareness and premium on time. We buy prewashed jeans and instant coffee and our meals are from the drive-thru of the fast food restaurant. The time we save through these modernizations rarely is redirected toward leisure.
Examine these flashpoints in your own day-to-day life. In a modern elevator, the door close button is simply a placebo placed to placate the individual for whom 5 seconds is an eternity. Sociologists have found increasing wealth and increasing education bring a sense of tension about time. The modern patient undergoing joint arthroplasty brings this tension to our offices.
It is true also that time awareness drives social change. The author and sociologist Mark Halprin remarked, “Our lives are lived with the kind of excitement that our forbearers knew only in battle. They, unlike us, were the prisoners of mundane tasks. They wrote with pens, they did long division, they waited endlessly for things that come to us instantaneously” [18]. They had less than we do and they bowed to necessity, as we do not. Our infatuation with technologic advances has placed an increasing emphasis on speed and precision. Our $15 digital watches measure time in hundredths of a second. A handheld global positioning system (GPS) has replaced the compass and sextant used to discover and map our country.
At the beginning of the last century, in 1901, H.G. Wells published “The New Accelerator” [34], in which his devilish professor character sought to discover a stimulant that would allow humans to move faster, produce more work, heal quicker, and essentially, modulate the dimension of time. The relativity of time, incidentally, was not discovered by Einstein until some 25 years later. Now, in the 21st century, our patients live out this new acceleration at work, in the car, turning on a microwave, and shopping on the Internet. Is it not then understandable that our new patients, these baby boomers and ultimately their children and grandchildren, who are accustomed to choice and control and are infatuated with speed, would not demand their physicians capitulate?
Paradigm Shift
This time consciousness stretches further into the social fabric of our patients’ lives. Maybe it is because our sense of time is absolute that age is becoming relative. Fifty is the new 40, 40 is the new 30, and so on. With this social backdrop, it becomes easier to understand why our patients are now younger, more active, and more demanding. In our offices, they are demanding quicker recovery, return to higher-level sport activity, and earlier discharge from hospitals. Like it or not, we are experiencing a paradigm shift away from the traditional surgeon goals of infection rates, radiolucencies, and survivorship to those goals now imposed by our patients. These patient goals have, in large part, been defined by definitions that we as surgeons have placed in the media. Patients have come to expect, not by review of peer literature, but rather of the popular press, that we are able to provide rapid recovery, improved cosmesis, high functional demands, cutting-edge technology, and one (and only one) operation.
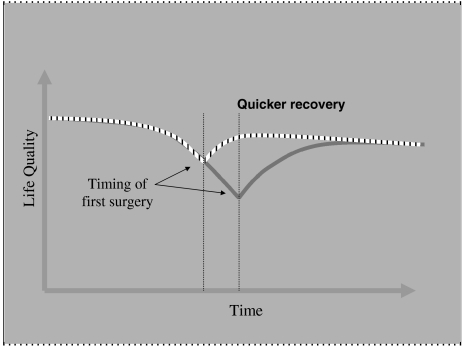
In a modern society pressured by time, quality of life is the new mantra of our patients. The patients’ focus on quality of life is reflected in their approach to surgery. In years past, primarily at the surgeon’s insistence, they would be inclined to delay surgical intervention. Now, however, patients understand the availability of and, in many cases, the reliability of the surgical procedures we perform and they are not willing to sustain a long decline in their functional capacity and quality of life before undergoing surgery (Fig. 1).
Fig. 1.
Surgery can affect life quality positively. The quantitative effect on quality of life is potentially related to the timing of surgical intervention and is represented graphically as the area beneath the curves.
Medicine is Evolving
Chances are most medical residents in training today will never see a case of measles or diagnose chickenpox. Both were leading causes of death 100 years ago [12]. The humility of the patients who survived polio, measles, the Depression, and a global war is disappearing with the new demographic. Indeed, in the United States, most of us remain largely insulated from the ravages of war or the modern plague of HIV/AIDS and our culture reflects this insulation. The contentedness is, in part, a function of our imperial, preeminent economic status in the world. However, on a deeper, more human level, we are comforted by the advances in modern medicine and its impact on disease. Many chronic conditions are amenable to our remedies, rendering scourges of years past to the power of our modern diagnostics and therapeutics. The age-at-death ratios of patients for most diseased conditions have improved with modern medicine. We as a populace are living longer. With notable exceptions, we have pioneered medicine through two epochs of care, that of communicable diseases and, more recently, chronic disease states. It has been suggested we are evolving now into a third epoch of medicine, namely, improving quality and function in the lives of our patients [5–7]. Orthopaedics, and joint arthroplasty in particular, figure highly in this new epoch of medicine.
Epidemiologists easily can measure and report reductions in death rates and disease modification, thereby defining our successes and failures in the first two epochs of modern medical evolution. Unfortunately, the crucial metrics are missing for the third epoch! As it is highly subjective, it remains unquantifiable to all interested parties—surgeons, hospitals, insurance companies, and industry alike. We in medicine hold a vaulted social position because we are perceived by our public as being devoted to the needs of our patients. Although this remains true, our patients’ needs are changing. The concept of life quality is elusive. Lacking a metric to measure our success and wanting to continue to fulfill our societal role, healthcare costs are positioned to spiral as patients demand more intervention and modalities to reach higher and higher quality of life and function while we as physicians scramble to fulfill their demands.
We know healthcare spending is in trouble even without the pressures of the third epoch. As the United States struggles for fiscal clarity from one administration to the next, the federal deficit continues to grow. The United States spends more than it earns by 5% to 6% a year and has so for years [13]. The constraints on future healthcare financing invariably are linked. Gregory Manikiw, Bush’s top economic advisor, recently said, “The benefits now scheduled for future generations under current law are not sustainable. They are empty promises” [13]. Medicare, Medicaid, and Social Security already cost approximately 7% of everything produced by every American every year (by 2030? greater than 15%) [13]. An estimated 48% of the total government’s budget will be allocated to the elderly by 2015 [16]. In other words, the trend of the third epoch in medicine will be faced with a financial reckoning solved only by insightful political realism at a national legislative level, systematic improvements in healthcare delivery and efficiencies, an increased personal financial accountability for care received, or societal checks on this drive for life quality. In a modern society, it is unlikely the latter will occur. If you care to guess who will influence these decisions you need only consider today in the United States, mature Americans, those older than 50 years, account for 35% of the population and hold 77% of the liquid personal assets and 57% of discretionary income [27].
The Current Milieu
Daniel J. Boorstin, the Pulitzer Prize-winning historian, commented, “Planning for the future without a sense of history is like trying to plant cut flowers” [3]. The traditional role of the surgeon and physician has been to deduce, delineate, and control the flow of information and care to their patients. We are operating in a different milieu today in which, at least for now, we compete for these patients between practices and between individual physicians in part because these patients have mobility and information from which to make choices. We have begun to legitimize the shift in control even in our own literature, advocating for patient input into care decisions, or as it is termed ‘patient-centered care.’ The Institute of Medicine’s Committee on Future Quality of Healthcare outlines six areas for improving healthcare delivery in the United States, stating health care should be safe, effective, patient-centered, timely, efficient, and equitably delivered [23]. Without argument, each of us would wish our healthcare system provided such care.
Yet, for orthopaedic patients, providing true patient-centered care relies on the ability for us as surgeons to provide our patients with accurate, evidence-based information and to improve communication. However, currently involving our patients in true patient-centered decision processes is potentially dangerous because we lack evidence-based data to support many of the new technologies and techniques our patients desire.
Thomas Sculco, a pioneer in modern total joint arthroplasty and a scrupulous investigator, recently stated, in a traditional scientific setting, “Earlier designs and materials that demonstrated inferior functional and long-term results have disappeared in a Darwinian fashion” [30]. However, with the rampant influx of new procedures, implant materials, products, and, notably, patients, attributable to the population growth and the increased interest in procedures with recognized improved outcomes from patients previously not pursuing such options, the natural selection process bridges far more concurrent experiments. The individual outcomes are subject to the same Darwinian fate; however, their lineage becomes less transparent.
Peter Senge, senior lecturer at Massachusetts Institute of Technology and founder of the Society for Organizational Learning, said, “Our problems today are the result of yesterday’s solutions” [31]. Successful innovation always makes predecessor technology appear dated, and our patients are now savvy enough to begin to ask about these newer technologies. The optimism for continued advancement of our specialty in the 21st century lies in what we have learned from our prior mistakes and with corollary advances in other fields of science. As we have discovered particle disease and osteolysis as limitations of our current designs, material scientists have continued to improve their understanding of crystallinity, metallurgy, manufacturing tolerances, and simulator modeling.
In the 21st century, just as important as who our patients are and what we manufacture for them is the system in which they are treated. When the Institute of Medicine published its report on medical errors in 1999, we were told we are killing 100,000 patients per year in our hospitals [9]. Updated information technology is seen as a mandatory basis for the future of healthcare systems. These information-based systems will cut down on medical errors. However, the development of these systems initially will place additional demands on us, the physicians, particularly regarding accountability in providing, assessing, assimilating, and responding to the increased amount of information. As the universal availability of information increases concurrent with the rapid growth of human knowledge, physicians and the public will be granted a more comprehensive picture of health. With more information, 21st century patients will increasingly expect a holistic, personal approach to their health care. Information systems will allow for synergies between medical specialties and industrial technologies to prosper, paving the way for novel approaches and modernization (one need only reflect on the sequencing of the human genome accomplished at the end of the last century). Information synergies will save time and money, important to the 21st century patient, and will place an increasing emphasis on individual-specific (not gender, race, or age-specific) care.
Influence of Direct-to-Consumer Marketing
The lifestyle interventions the new demographic, the boomers, seek are now the story of direct-to-consumer (DTC) marketing. Evening newscasts are punctuated by these commercials with directions for additional information at their Web sites. It is an interesting corollary that the information revolution makes DTC possible! We know the people who need those pharmaceuticals and devices advertised in DTC are the same demographic that has the money. Although DTC may drive unit sales temporarily, these campaigns are expensive for the companies. Advocates conclude these commercials provide the public with information. This point remains debatable. However, they do produce product branding and loyalty. This point may be particularly important as we unravel the financial reckoning brought on in part by a quest for increased life quality. A more cynical interpretation of the drive for DTC marketing may resonate in the shift of healthcare financing to the individual.
Robert Booth, in a recent editorial, suggested, just as the advent of anesthesia was the tipping point in the evolution of American surgery, so DTC advertising may be a catalyst for its decline [2]. We are losing the respect of our patients in part because of our failure to communicate properly, to provide patients with fair and balanced education, and to properly counsel our patients in the face of the onslaught of DTC advertisements. Moreover, as we find increasingly savvy ways to advertise our uniqueness to the world through the media, we delegitimize our profession. This devolution of trust by patients of the healthcare system is multifactorial. However, it is likely linked to the pace of change in our society. Harvard Business Professor Juan Enriquez stated, “It is not that people are more evil today than they were in your grandparents’ generation. More likely, this sense of unease as to ‘who can I trust?’ reflects the overwhelming pace and magnitude of change. Nothing seems stable” [13]. Trust in the institution of medicine has suffered the same fate as trust in other major US institutions such as government, declining precipitously [28].
If we examine the influences of DTC advertising on orthopaedic practices today, there is a great deal of interest in the public about a hip implant endorsed by a major professional golfer, knee implants that bend and rotate, surface replacement for young athletes, and gender-specific implants. Critical review of our literature underscores the paucity of evidence-based information to support these media proclamations. We have, unfortunately, come to understand patients do not necessarily care about evidence-based medicine. They often are willing to adopt the vendor message verbatim and consequently are open to our experimentation. This duplicity, however, is understandable when examined from the patient’s perspective. Patients do not yet understand medicine despite the increasing availability of information sources. However, they are, and will continue to be, drawn to ideas that seem simple or simply elegant. Who would not want minimally invasive surgery or computer-enhanced accuracy? Oliver Wendell Holmes once said, “I wouldn’t give a fig for the simplicity on this side of complexity; but I would give my right arm for the simplicity on the far side of complexity” [10]. Despite the increasing sophistication of their information sources, patients are unclear as to which side of the complexity equation we present to them.
Conclusions
Our patients presenting for total joint arthroplasty now are a different lot from patients in years past. Demographic trends are swelling their numbers, influencing and commanding our attention. Disparate and convergent trends of age, obesity, activity level, and life expectancy ensure we will remain challenged to perfect the techniques we practice.
More importantly, potentially, is how we embrace our patients as they gain additional insight into their health options. In a world that relishes the acceleration of information exchange, the precision of computerization, and metric declination, seemingly speeding up and expanding daily, we need to understand why they ask more questions if we are to remain the arbiter of orthopaedic medical knowledge. Daniel J. Boorstin said, “The fog of information can drive out knowledge” [4]. The beacon in the fog should not be The Inquirer or an advertisement in the newspaper, but rather the doctor working diligently with the patient to understand the problems specifically in the context of available solutions.
What, then, is our responsibility and response to the 21st century patient? It is, I believe, to maintain control of validated information sources and of the exchange of information with the patient. We need to be the interpreters and balancers of scientific information to help guide our patients through the maze of medical hyperbole. We need to discuss new treatments and technologies openly and honestly. Additionally, it is important to understand, although what the patient demands from us, their physicians, is changing, our responsibility for their safety and care has not. The current demographics, time pressure, patient mobility, consumerism, and cost pressures are trends. As trends, they too will continue to change. What will remain constant with our new patients will be physician accountability, that is, our responsibility to make decisions, guide patients, and communicate with them in an easily understood manner.
“You can observe a lot just by watchin’.”—Yogi Berra [1]
Acknowledgments
I thank Michelle Mitchell for help with manuscript preparation and express deep appreciation for editorial assistance from Christi Sychterz Terefenko. Finally, thanks to Dr. Tony DiGioia for his insistence that I put my thoughts to paper.
References
- 1.Berra Y, Berra D. The Yogi Book. New York: Workman Publishing; 1998.
- 2.Booth RE Jr. Truth in advertising: the ethical limits of direct-to-consumer marketing. Orthopedics. 2006;29:780–781. [DOI] [PubMed]
- 3.Boorstin DJ. The humane study of law. The Yale Law Journal. 1948;57:960–975. [DOI]
- 4.Boorstin DJ. On computerization of libraries. The New York Times. July 8, 1983.
- 5.Breslow L. From disease prevention to health promotion. JAMA. 1999;281:1030–1033. [DOI] [PubMed]
- 6.Breslow L. Perspectives: the third revolution in health. Annu Rev Public Health. 2004;25:xiii–xviii. [DOI] [PubMed]
- 7.Breslow L. Health measurement in the third era of health. Am J Public Health. 2006;96:17–19. [DOI] [PMC free article] [PubMed]
- 8.Centers for Disease Control and Prevention (CDC). Prevalence of self-reported arthritis or chronic joint symptoms among adults—United States, 2001. MMWR Morb Mortal Wkly Rep. 2001;51:948–950. [PubMed]
- 9.Corrigan J, Kohn LT, Donaldson MS. To Err Is Human: Building a Safer Health Care System. Washington, DC: National Academies Press; 1999. [PubMed]
- 10.Covey SR. The 8th Habit: From Effectiveness to Greatness. New York, NY: Free Press; 2004:103.
- 11.Crowninshield RD, Rosenberg AG, Sporer SM. Changing demographics of patients with total joint replacement. Clin Orthop Relat Res. 2006;443:266–272. [DOI] [PubMed]
- 12.Elliott VS. Live well, live long: medicine turns focus to well-being. Am Med News. 2006:49:18.
- 13.Enriquez J. The Untied States of America. New York, NY: Crown Publisher; 2005:29, 152, 162, 239–266.
- 14.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. [DOI] [PubMed]
- 15.Flugsrud GB, Nordsletten L, Espehaug B, Havelin LI, Engeland A, Meyer HE. The impact of body mass index on later total hip arthroplasty for primary osteoarthritis: a cohort study in 1.2 million persons. Arthritis Rheum. 2006;54:802–807. [DOI] [PubMed]
- 16.Flugsrud GB, Nordletten L, Espehaug B, Havelin LI, Meyer HE. Risk factors for total hip replacement due to primary osteoarthritis: a cohort study in 50,034 persons. Arthritis Rheum. 2002;46:675–682. [DOI] [PubMed]
- 17.Gelber AC, Hochberg MC, Mead LA, Wang NY, Wigley FM, Klag MJ. Body mass index in young men and the risk of subsequent knee and hip osteoarthritis. Am J Med. 1999;107:542–548. [DOI] [PubMed]
- 18.Gleick J. Faster the Acceleration of Just About Everything. Philadelphia, PA: Random House; 2000.
- 19.Hart DJ, Doyle DV, Spector TD. Incidence and risk factors for radiographic knee osteoarthritis in middle-aged women: the Chingford Study. Arthritis Rheum. 1999;42:17–24. [DOI] [PubMed]
- 20.Haub C, Jacobsen L. International migration is reshaping United States, global economy. Available at: http://www.prb.org/presentations/06WorldDataSheet_presentation.ppt. Accessed August 25, 2006.
- 21.Hobs FB, Damon BL. 65+ in the United States: Current Population Reports. Washington, DC: US Census Bureau; April 1996:23–190.
- 22.Holmberg S, Thelin A, Thelin N. Knee osteoarthritis and body mass index: a population-based case-control study. Scand J Rheumatol. 2005;34:59–64. [DOI] [PubMed]
- 23.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the Twenty-first Century. Washington, DC: National Academies Press; 2001. [PubMed]
- 24.Järvholm B, Lewold S, Malchau H, Vingård E. Age, bodyweight, smoking habits and the risk of severe osteoarthritis in the hip and knee in men. Eur J Epidemiol. 2005;20:537–542. [DOI] [PubMed]
- 25.Karlson EW, Mandl LA, Aweh GN, Sangha O, Liang MH, Grodstein F. Total hip replacement due to osteoarthritis: the importance of age, obesity, and other modifiable risk factors. Am J Med. 2003;114:93–98. [DOI] [PubMed]
- 26.Mokdad H, Ford ES, Bowman BA, Dietz WH, Vinicor F, Bales VS, Marks JS. Prevalence of obesity, diabetes, and obesity-related health risk factors, 2001. JAMA. 2003;289:76–79. [DOI] [PubMed]
- 27.Novelli WD. How aging boomers will impact American business. Available at: http://www.aarp.org/about_aarp/aarp_leadership/on_issues/baby_boomers/how_aging_boomers_will_impact_american_business.html. Accessed September 9, 2006.
- 28.Nye JS Jr, King DC, Zelikow PD. Why People Don’t Trust Government. Cambridge, MA: Harvard University Press; 1997.
- 29.Reijman M, Pols HA, Bergink AP, Hazes JM, Belo JN, Lievense AM, Bierma-Zeinstra SM. Body mass index associated with onset and progression of osteoarthritis of the knee but not of the hip: the Rotterdam Study. Ann Rheum Dis. 2007;66:158–162. [DOI] [PMC free article] [PubMed]
- 30.Sculco TP. The economics of new age arthroplasty: can we afford it? Orthopedics. 2006;29:780. 27. [DOI] [PubMed]
- 31.Senge PM. The Fifth Discipline: The Art and Practice of The Learning Organization. New York, NY: Currency Doubleday; 1990:57.
- 32.US Census Bureau. Educational attainment. Current Population Reports. 1970;20, no 207: Table 2; Educational Attainment in the US. 2004: Table 10. Statistical Abstract of the United States. 2006: Table 260. Available at: http://www.census.gov. Accessed August 29, 2006.
- 33.van Saase JL, Vandenbroucke JP, van Romunde LK, Valkenburg HA. Osteoarthritis and obesity in the general population: a relationship calling for an explanation. J Rheumatol. 1988;15:1152–1158. [PubMed]
- 34.Wells HG. The new accelerator. The Strand. December 1901.