Abstract
Total knee arthroplasty frequently is required during early adulthood in patients with advanced juvenile rheumatoid arthritis. We queried patients on issues of importance to them, asked whether they were satisfied with surgical outcomes, and ascertained their postoperative status. We retrospectively reviewed 14 adult patients (22 knees) with severe juvenile rheumatoid arthritis who were treated with primary total knee arthroplasty between 1989 and 2001. All patients were evaluated by pain and stiffness visual analog scales, range of motion, the Patient-Specific Index, Hospital for Special Surgery knee score, WOMAC Osteoarthritis Index, EuroQuol in five dimensions, and SF-36 Health Survey. Preoperative scores were assessed by recall. Patients had a minimum followup of 2 years (mean, 8 years; range, 2–13 years). Quality of life improved after TKA as measured by the Patient-Specific Index. Eighteen of 22 patients rated themselves satisfied with the functional outcome of their surgery; all patients were satisfied with pain relief. Final SF-36, EuroQuol in five dimensions, and WOMAC scores were low compared with age-matched population norms. A mean postoperative flexion arc of 77° (range, 30°–130°) was observed. Total knee arthroplasty had a major positive impact on quality of life as reported by patients.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Juvenile rheumatoid arthritis (JRA) is a chronic, inflammatory, disabling condition distinct from its adult counterpart with onset before 16 years and an incidence of approximately 10 per 100,000 population [25]. The knee is the most common joint involved in JRA and is a major factor in diminished function for these patients. Diminished function may be severely limiting to physical, social, and emotional development in childhood, adolescence, and young adult life. In early adult life, full-thickness articular cartilage damage in the lateral component of the knee frequently results in intolerable flexion and valgus deformity of JRA. Arthroplasty of the knee then is indicated to reduce pain and improve function [4, 8, 26].
Implantation of knee prostheses in the third and fourth decades of life in patients who have a long life expectancy raises concerns about the potential need for revision surgery at a young age. Hargreaves et al. [12] reported wound healing problems in 26% of patients with JRA. A search of computerized medical databases located 10 additional studies of outcomes of TKA in patients with JRA [4, 7, 8, 18, 23, 24, 26,29, 32, 33]. Unlike the reports of 55% to 80% improvement in pain after TKA in JRA [8, 23, 24, 26, 32, 33], improvements in functional outcome measures and other instruments have been less positive than generally seen in TKA for osteoarthritis. These studies showed mean Knee Society scores from 82 to 92 and functional scores from 39 to 76 (on a scale of 0–100) at 4 to 6.5 years postoperatively [4, 24, 33], Jergensen’s functional outcomes scores of 68 to 85 (on a scale of 0–100) [7, 8], and Hospital for Special Surgery knee scores of 80 to 84 (on a scale of 0–100) [26, 32]. A marked improvement in ambulation was reported after surgery. Whereas 88% to 100% of patients required walking aids or wheelchairs before surgery, 73% to 100% of patients did not require walking aids at 3.5 to 7 years’ followup [7, 8, 24, 25, 33]. However, these studies did not analyze patient satisfaction or quality of life. It has been our clinical impression that patients with JRA who are profoundly disabled by multiple impairments usually highly value the beneficial effect of TKA performed for appropriate indications despite continuing to experience residual disability.
Clinical measures of health status, focusing on physiologic and physical measurements, reflect clinicians’ perceptions of disease but often correlate poorly with patients’ perceptions of health [38]. Other measures therefore have been designed to have direct relevance to patients’ lives [2, 22, 38], such as patient-specific indices, in which the patient chooses the questionnaire items. Examples of such instruments include the McMaster Toronto Arthritis Questionnaire and the Patient-Specific Index (PASI) [39], which have been previously reviewed and compared with seven other patient-specific instruments [16]. The PASI asks patients to evaluate the severity of a given list of symptoms, degree of difficulty of a given list of activities, and importance of a given list of problems. The final two questions are completely open-ended, permitting patients to identify and rate any two symptoms and any three activities to form the last five patient-generated items, or PASI-pg.
We asked what issues were of importance to adult patients with JRA before and after TKA, as determined by a patient-specific index, the PASI-pg, and whether patients were satisfied with the surgery. We also asked what their postoperative status was, as evaluated radiographically, clinically, and by standardized outcome measures that are widely used in evaluation of TKA.
Materials and Methods
We retrospectively evaluated 14 consecutive patients (22 knees) diagnosed with either severe polyarticular-onset JRA (13 patients; 20 knees) or systemic-onset JRA (both knees of one patient) admitted for elective primary TKA between 1989 and 2001 (Table 1). Indications for surgery included JRA with severe, painful, and disabling arthritis of the knee. Key outcome measures were evaluated after a minimum followup of 2 years (mean, 8 years; range, 2–13 years) and compared with historical controls from the literature. All patients signed a consent form to participate in the study. We obtained prior approval by our research ethics board.
Table 1.
Baseline characteristics of patients with juvenile rheumatoid arthritis who underwent TKA
| Characteristic | Number of patients (%) |
|---|---|
| Number of patients | 14 (22 knees) |
| Mean age at surgery (years) | 33 (range, 15–42) |
| Gender | |
| Female | 12/14 (86%) |
| Male | 2/14 (14%) |
| Mode of juvenile rheumatoid arthritis onset | |
| Pauciarticular | 0/14 (0%) |
| Polyarticular | 13/14 (93%) |
| Systemic | 1/14 (7%) |
| Marital status | |
| Single | 7/14 (50%) |
| Married or common law | 7/14 (50%) |
| Highest level of education | |
| Primary | 1/14 (7%) |
| Secondary | 8/14 (57%) |
| University/college | 5/14 (36%) |
| Employment status | |
| Full-time | 2/14 (14%) |
| Part-time | 1/14 (7%) |
| Not working | 11/14 (79%) |
| Type of prosthesis (% cemented) | |
| Femoral implant | 15/22 (68%) |
| Tibial implant | 19/22 (86%) |
| Patella resurfaced | 15/22 (68%) |
| Mean followup (years) | 8.0 (range, 2–13) |
All surgical procedures were performed by one of the authors (ERB). Exposure was through a midline incision and a medial parapatellar arthrotomy. Because of bone deformity and contracted, inelastic soft tissue, it frequently was difficult to rotate the patella, in which case it initially was subluxated without rotation to gain access to the joint. A quadriceps tendon snip usually was avoided but was performed when necessary. Osteotomy of the anterior tibial tubercle was not performed because of concerns regarding osteoporosis and potential poor fixation. There was typically little or no synovitis. Although the entire skeleton was usually small, a variable deformity consisting of relative overgrowth of the epiphyses with relatively large condyles and a thick, squared-off patella was found, which contributed to the restricted range of motion. Five knees had ankylosis. The soft tissue capsule was restrictive over the large condyle. To optimize range of motion, the excessive anteroposterior diameter of the femoral condyles was reduced by generous bone resection while maintaining the posterior condylar aspect. Anterior femoral bone was removed without notching the metaphysis, and excess posterior bone was resected by choosing the next smaller femoral component when possible. The posterior cruciate ligament could not be made isometric in a reliable manner because of the unusual shape and size of the condyles and because of the flexion and valgus deformities encountered, so it was resected and posterior stabilized implants were used. Flexion and valgus deformities were managed with posterior and lateral soft tissue releases. Lower limb alignment often was difficult to achieve because of concomitant hip and hindfoot deformity. Patellar resurfacing was performed in 15 of 22 knees (Table 2) either to address articular surface damage and poor articulation with the femoral component or to reduce the anteroposterior diameter of the patella and promote flexion. All implants used since 1992 were cemented. Implants included Osteonics® (12 knees; Stryker Orthopaedics, Mahwah, NJ), PFC® (four knees; DePuy Orthopaedics, Inc, a Johnson and Johnson company, Warsaw, IN), Miller-Galante® I (one knee) and II (three knees) (Zimmer, Inc, Warsaw, IN), and Howmedica PCA® (two knees; Stryker Orthopaedics) (Table 2). Substantial soft tissue releases sometimes were necessary, and we addressed soft tissue and bone causes of tightness in the knee to promote range of motion. We used prosthesis systems that included small components when operating on smaller patients.
Table 2.
Cemented and uncemented prostheses used for TKA
| Patient number | Joint side | Femoral component | Patellar resurfacing | Patellar component | Tibial component | Prosthesis* |
|---|---|---|---|---|---|---|
| 2 | Right | Cemented | No | NA | Cemented | PFC |
| 2 | Left | Cemented | No | NA | Cemented | PFC |
| 3 | Right | Cemented | No | NA | Cemented | Miller-Galante II |
| 5 | Right | Uncemented | Yes | Cemented | Cemented | Howmedica PCA |
| 7 | Right | Cemented | Yes | Cemented | Cemented | Osteonics |
| 7 | Left | Cemented | Yes | Cemented | Cemented | Osteonics |
| 13 | Right | Uncemented | No | NA | Cemented | Osteonics |
| 16 | Right | Uncemented | No | NA | Uncemented | Miller-Galante II |
| 16 | Left | Cemented | Yes | Cemented | Cemented | PFC |
| 21 | Left | Uncemented | Yes | Cemented | Cemented | PFC |
| 24 | Right | Cemented | Yes | Cemented | Cemented | Osteonics |
| 27 | Right | Uncemented | Yes | Uncemented | Uncemented | Miller-Galante I |
| 27 | Left | Uncemented | Yes | Cemented | Cemented | Miller-Galante II |
| 28 | Left | Cemented | No | NA | Cemented | Osteonics |
| 28 | Right | Cemented | Yes | Cemented | Cemented | Osteonics |
| 29 | Left | Cemented | Yes | Cemented | Cemented | Osteonics |
| 29 | Right | Cemented | Yes | Cemented | Cemented | Osteonics |
| 32 | Left | Cemented | No | NA | Cemented | Osteonics |
| 33 | Left | Cemented | Yes | Cemented | Cemented | Osteonics |
| 33 | Right | Uncemented | Yes | Uncemented | Uncemented | Howmedica PCA |
| 34 | Left | Cemented | Yes | Cemented | Cemented | Osteonics |
| 34 | Right | Cemented | Yes | Cemented | Cemented | Osteonics |
*Prostheses included Osteonics® (Stryker Orthopaedics, Mahwah, NJ), PFC® (DePuy Orthopaedics, Inc, a Johnson and Johnson company, Warsaw, IN), Miller-Galante® I and II (Zimmer, Inc, Warsaw, IN), and Howmedica PCA® (Stryker Orthopaedics); NA = not applicable.
Patients were asked to return for followup and were evaluated retrospectively by one independent observer (BMJ).
Patient data gathered included patient demographics with age, gender, education level, and employment status, and mode of JRA onset (systemic, polyarticular, pauciarticular) and number of other joints involved. Intraoperative data from the operative record included the prosthesis type, the type of fixation used, soft tissue releases performed, and intraoperative complications. An independent observer (BMJ) interviewed patients and performed a clinical examination at followup. Preoperative pain and stiffness were estimated with a visual analog scale (VAS) by patient recall. Postoperative data included pain and stiffness at followup, postoperative range of motion, and late complications. Objective outcomes were assessed with the Hospital for Special Surgery (HSS) knee score [14] and range of motion of the knees.
Each participant completed a questionnaire, which included the SF-36 Health Survey [34, 35], the EuroQol in five dimensions (EQ-5D) [5, 9], the Meaning of Illness Questionnaire—Self Report [6, 36], and the WOMAC Osteoarthritis Index (Version 3) [3] to evaluate the patients’ subjective outcomes, and the five patient-generated items from the PASI-pg [39], which included two symptoms and three activities, each scored separately [16]. The PASI-pg questionnaire asks open-ended questions for patients to identify and rate any two symptoms and any three activities. Additionally, patients were asked to recall issues that led them to have TKA, and a recall PASI-pg was completed at followup describing preoperative issues of importance to the participants. To evaluate patient satisfaction with the surgery, the questionnaire (Appendix 1) also included items from the Group Health Association of America Consumer Satisfaction Survey adapted for knee pain [31] and the Patient-Doctor Interaction Scale [30].
We (ERB, BMJ) assessed anteroposterior and lateral radiographs of the surgically treated joint(s) with the Knee Society radiographic evaluation form [10] and the Aglietti index for patellar height [1]. Interobserver correlation coefficients were computed for the radiographic analysis (femoral or tibial subsidence, radiolucent lines, overhang, or undersizing) and a mean agreement of 91% with a mean κ value of 0.73 (substantial agreement) were obtained.
Descriptive analyses were completed on demographic information and clinical and radiographic outcomes. Quality of life at followup was measured with the SF-36, EQ-5D, WOMAC, Knee Society score, and PASI-pg scores. WOMAC scores and subscores for pain, stiffness, and function of the patients with JRA were normalized on a scale ranging from 0 to 100. We used the Wilcoxon signed rank test at the α = 0.05 level of significance to compare SF-36 scores of the study population with the normal population of the same age [13, 34, 35]. The PASI-pg patient-generated items were coded into general categories according to the headings of the International Classification of Functioning, Disability and Health [37]. We used ranked statistics to determine the items identified most frequently by patients in the symptoms area of the score and in the activities area of the score; the ranked statistics were used to reduce dependence on absolute numeric scores, which may not have a common meaning in patient-specific measures such as the PASI-pg [16].
Results
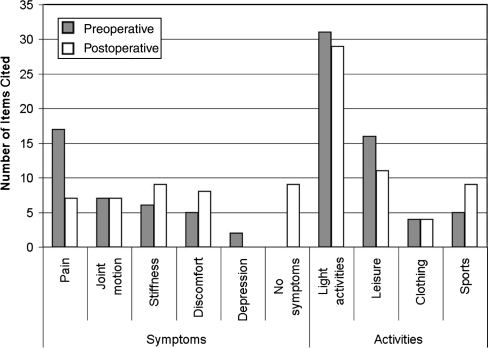
The PASI-pg questionnaire identified changes in items generated by patients with JRA after TKA when compared with preoperative items generated by patient recall, indicating an improvement in quality of life (Fig. 1). The patients identified six symptom areas, including pain, joint motion, stiffness, discomfort, depression, and no reported symptoms, and four activity areas, including light household, leisure, clothing, and sports, as important and relevant to their lives. The issues most frequently cited by the patients when recalling their preoperative status differed from those raised by the patients at postoperative evaluation, showing a shift away from pain and toward greater activity. Pain was selected by 19 of 22 patients with JRA in their recall of preoperative salient issues compared with only eight at followup. Although no patients reported having no symptoms before surgery, nine of 22 reported having no symptoms at followup. Furthermore, the ability to perform sports was selected as important by only five of 22 patients preoperatively but by nine patients at followup, reflecting a shift in the level of activity that could be considered by the patients and representing a clinically important change in quality of life.
Fig. 1.
A comparison is shown of symptoms and activities most frequently identified by patients with JRA in the patient-generated PASI-pg (n = 20) after TKA (Postoperative) and in recall of preoperative issues (Preoperative). Issues were coded into general categories using the headings of the International Classification of Functioning, Disability and Health [37].
Patients’ reported satisfaction with the surgical outcome was high. Regarding the knee, 20 of 22 reported their pain at a level permitting daily activities, and all patients were satisfied with pain relief. Eighteen of 22 rated themselves as satisfied by knee surgery, and 12 to 20 patients were satisfied with their ability to perform heavy activities of daily living (Table 3). Overall, 16 of 22 patients said their needs were addressed.
Table 3.
Satisfaction of patients with pain relief and activities of daily living at a mean followup of 8 years (n = 22 knees)
| Item/Activity | Completely satisfied/satisfied | Neither satisfied nor dissatisfied | Dissatisfied |
|---|---|---|---|
| Pain relief | 22 (100%) | ||
| Ability to perform light activities such as housework | 20 (91%) | 2 (9%) | |
| Ability to perform heavy activities such as gardening or lifting | 12 (55%) | 2 (9%) | 7 (32%) |
| Comfort in walking | 19 (86%) | 3 (14%) | |
| Balance or steadiness on their feet | 17 (77%) | 4 (18%) | 1 (5%) |
| Ability to perform self-care activities such as bathing and dressing | 14 (64%) | 4 (18%) | 4 (18%) |
| Ability to participate in recreational activities | 13 (59%) | 3 (14%) | 5 (23%) |
| Overall, needs were addressed | 16 (73%) | 6 (27%) |
We identified radiolucent lines greater than 2 mm for six knees (Table 4). The tibial components were generally appropriately sized (Table 5). The mean patellar thickness was 16.48 mm (range, 9–23 mm) and the height was 0.49 mm (range, 0.08–0.87 mm). No patient had symptoms suggestive of component loosening. The postoperative mean flexion was 77° (range, 30°–130°). Four knees had flexion contractures at final followup (5°, 10°, 20°, 30°, respectively). Patients indicated their pain and stiffness at followup was low to moderate (Table 6). One patient had a very stiff knee associated with a very limited range of motion. That patient underwent arthroscopy and manipulation 3 weeks postoperatively. No patients had revisions or were scheduled for revision at the time of followup.
Table 4.
Radiolucent lines and radiographic subsidence at final followup (n = 22 knees)
| Radiolucent lines/Radiographic subsidence | No | Yes | Zone | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| Radiolucent lines (> 2 mm) | |||||||||
| Femoral | 21 (95%) | 1 (5%) | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Tibial (mediolateral) | 21 (95%) | 1 (5%) | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Tibial (anteroposterior) | 17 (77%) | 5 (23%) | 4 | 1 | 0 | ||||
| Patellar | 21 (95%) | 1 (5%) | 1 | 0 | 0 | ||||
| Radiographic subsidence (> 3 mm) (for all 3 components) | 22 (100%) | ||||||||
Table 5.
Radiographic observations of tibia at final followup (n = 22 knees)
| Radiographic observation | Finding absent | Finding present | < 2 mm | 2–5 mm | > 5 mm |
|---|---|---|---|---|---|
| Tibia | |||||
| Lateral overhang | 19 (86%) | 3 (14%) | 1 | 1 | 1 |
| Medial overhang | 19 (86%) | 3 (14%) | 1 | 2 | 0 |
| Lateral undersize | 16 (73%) | 6 (27%) | 3 | 3 | 0 |
| Medial undersize | 17 (77%) | 5 (23%) | 2 | 3 | 0 |
Table 6.
Outcome measures for patients with juvenile rheumatoid arthritis at followup
| Outcome measure | Mean score (SD) | Range | Possible range |
|---|---|---|---|
| VAS pain | 1.95 (2.33) | 0–7 | 0 (none)–10 (severe) |
| VAS stiffness | 3.31 (3.04) | 0–8 | 0 (none)–10 (severe) |
| HSS | |||
| Knee score | 81 | 50–95 | 0 (poor)–100 (excellent) |
| Pain subscore | 29 | 25–30 | 10 (severe)–50 (none) |
| Function subscore | 54 | 26–73 | 0 (poor)–100 (excellent) |
| EQ-5D | |||
| Health state score | 0.52 (0.23) | 0.02–0.74 | 0 (poor)–1.0 (excellent) |
| VAS score | 73 (15) | 40–95 | 0 (poor)–100 (excellent) |
| WOMAC | (normalized) | ||
| Total score | 66 | 31–96 | 0 (poor)–100 (excellent) |
| Pain subscore | 80 | 30–100 | 0 (poor)–100 (excellent) |
| Stiffness subscore | 72 | 38–100 | 0 (poor)–100 (excellent) |
| Physical function | 61 | 29–96 | 0 (poor)–100 (excellent) |
| Meaning of Illness Questionnaire | |||
| Factor 1 (impact) | 2.6 (1.4) | 0–4 | 0 (high)–6 (low) |
| Factor 2 (stress and attitude of harm) | 1.3 (1.1) | 0–4 | 0 (high)–6 (none) |
| Factor 3 (degree of stress and change in commitments) | 3.0 (1.4) | 0–5.2 | 0 (negative)–6 (positive) |
| Factor 4 (challenge, positive attitude, motivation, and hope) | 4.1 (1.0) | 2.8–5.6 | 0 (poor)–6 (hopeful) |
SD = standard deviation; VAS = visual analog scale; HSS = Hospital for Special Surgery; EQ-5D = EuroQoL in five dimensions.
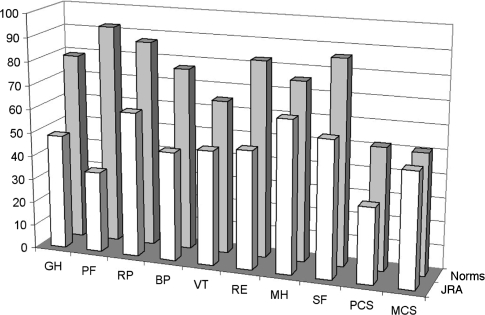
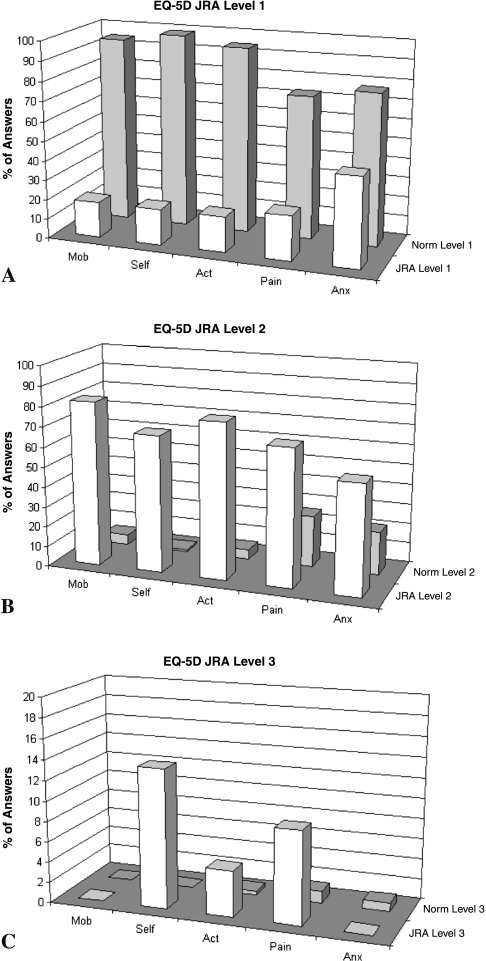
At followup, the HSS knee scores (Table 6) indicated excellent results for nine of 22 patients with JRA, good for nine, fair for three, and poor for one. Followup SF-36 scores for patients with JRA were low with a physical component summary of 32.09 (standard deviation [SD], 9.73) and mental component summary of 48.37 (SD, 12.62) (Fig. 2). Followup EQ-5D scores for patients with JRA were low on the range of possible scores (Table 6), and Level 2 and Level 3 EQ-5D scores, indicating a moderate or extreme problem, respectively, were found in 18 of 22 patients with JRA for mobility, self-care, and usual activities. The patients also had relatively low WOMAC scores at followup (Table 6), with a mean of 66.
Fig. 2.
SF-36 scores for patients with JRA at followup were compared with the population norms for people 25 to 34 years old [13, 34, 35]. GH = global health, p = 0.0019; PF = physical functioning, p = 0.0014; RP = growth physical, p = 0.0014; BP = bodily pain, p = 0.0029; VT = vitality, p = 0.0125; MH = mental health, p = 0.15; SF = social functioning, p = 0.0086; PCS = physical component summary score, p = 0.0014; MCS = mental component summary score, p = 0.15.
Discussion
We asked what the issues of importance were to adult patients with JRA before and after TKA, as determined by a patient-specific index, the PASI-pg, and whether patients were satisfied with the surgery. We also asked what their postoperative status was, as evaluated radiographically, clinically, and by standardized outcome measures that are widely used in evaluation of TKA.
Limitations of the study include the assessment of preoperative scores by patient recall, with Level IV evidence and deficient statistical power. Recall can be affected by current patient status and the perceived need to justify having had the surgery. Recall of pain is controversial. In a prospective study evaluating the accuracy of postoperative recall of preoperative pain related to endometriosis, Redwine [27] reported accurate recall; 6 to 18 months after surgery, more than 80% of patients recalled their preoperative pain level within 1 point on a 5-point scale for 10 of 11 symptoms. Patients who did not undergo reoperation tended to slightly inflate their postoperative assessment of preoperative pain. In knee and hip arthroplasties, a tendency to retrospectively exaggerate preoperative pain has been noted [17, 20]. In a study by Mancuso and Charlson [20], patients who completed a Hip Rating Questionnaire before and several years after THA tended to recall more pain, better walking, and better function than they reported before surgery. In our study, although our pain evaluation at final outcome is likely valid, it is likely that the recall evaluation of preoperative pain is somewhat greater than would have been obtained preoperatively, and thus the very large differential in preoperative and postoperative pain may be somewhat higher than would have been recorded if a prospective assessment had been available. In contrast, our data regarding differences in function likely underestimate the actual improvement observed. This study addresses deficiencies in applying standard outcome measures to this patient group. We show that standard outcome measures do not capture issues of importance to the patient with JRA after TKA. Therefore, we offer a different category of outcome measure, ie, patient-generated outcomes, in addition to standard outcomes, to capture issues of importance. The condition is sufficiently uncommon that no published randomized prospective trials of TKA in patients with JRA exist.
The PASI-pg questionnaire we used suggested symptoms and activities selected by patients shifted in frequency of selection between preoperative and final assessments. Pain was selected as a key issue preoperatively by 19 of 22 patients with JRA, as compared with eight patients at followup. The ability to perform heavier activities such as sports was selected as a key issue by five of 22 patients preoperatively, shifting to nine of 22 at followup, reflecting a shift in the level of activity that would be considered by the patients. We interpret the shift in issues reported by the patients to be indicative of clinical improvement. These issues, which were identified by the patients, were not captured in any other standardized instruments we used.
The majority of patients (18 of 22) were satisfied with the outcome of their surgery, although they had a high mean impact factor score and severe mean stress and attitude of harm score as evaluated by the Meaning of Illness Questionnaire (Table 6). Benefits of TKA in patients with JRA have been documented [4, 7, 8, 26, 29], but our study quantifies satisfaction and quality of life after TKA in different domains of daily life. Palmer et al. [23] reported on eight patients undergoing TKA with a mean followup of 15.5 years, and three of 15 TKAs were rated as unsuccessful. Parvizi et al. [24] reported on 13 patients undergoing TKA with a mean followup of 10.7 years, and Thomas et al. [33] reported on 10 patients undergoing TKA with a mean followup of 6 years, but these studies did not comment on patient satisfaction. Lybäck et al. [18] reported an overall “subjective contentment” of 75% of the patients. In our study, after surgery, all patients rated themselves as satisfied with pain relief, but satisfaction ratings were much lower for self-care activities (bathing and dressing), heavy activities (gardening, lifting), and recreational activities. The differential in preoperative and postoperative VAS pain scores, even if more modest than measured by recall evaluation, is indicative of how important pain is to these patients and their satisfaction with the surgery.
Our data showed a postoperative mean knee flexion arc of 73° (range, 20°–120°), with four knees having a flexion contracture after surgery (mean, 16°). Other authors have reported an improvement in range of motion. Boublik et al. [4] reported a mean flexion arc improvement of 26°, with a mean postoperative flexion arc of 103° (range, 65°–135°); Carmichael and Chaplin [8] reported a mean postoperative flexion arc of 73° (range, 15°–120°), with a mean residual flexion contracture of 17°; Thomas et al. [33] reported a mean flexion arc improvement of 33°, with a mean residual flexion contracture of 7°; and Palmer et al. [23] reported a 43° increase in mean arc of motion (range, 36°–79°). However, Parvizi et al. [24] reported TKA did not increase range of motion in a series of 15 patients younger than 20 years who underwent TKA, and Stuart and Rand [32] reported a modest decrease in knee flexion after TKA in 26 patients (44 knees) younger than 40 years. The range of motion reported in patients with JRA would be considered unsatisfactory for patients with osteoarthritis. However, it appears acceptable to patients with JRA based on their satisfaction report. The improvement in subjective pain scores cannot be directly compared with reported scores because only qualitative descriptions of pain have been published. Boublik et al. [4] stated “dramatic” pain relief was the “single most important contributor to the improved knee score.” Subjective stiffness was cited as one of the three major preoperative symptoms by almost ½ of the patients with JRA in our PASI-pg, but we found no references in the literature for comparison.
Outcome scores for these patients with JRA were lower than those reported for patients with osteoarthritis using standardized measures. Followup SF-36 scores for patients with JRA were considerably worse in all domains compared with the reference 25- to 34-year-old population norm [13, 34, 35], with the exception of the mental health domain (Fig. 2). Patients with JRA had EQ-5D scores that were moderately lower than the reference value of 83 for the population norms for people 30 to 39 years old (SD, 10) [15] (Fig. 3), and 82% of patients with JRA had Level 2 or 3 scores for mobility and self-care (indicating moderate or extreme problems) compared with less than 5% of the normal population [15]. Patients with JRA also had lower WOMAC global scores at followup (66) than patients with osteoarthritis 6 months after TKA (77), despite the fact they had similar pain and stiffness subscores [19]. The principal difference was in the physical function subscore, which includes some general daily activities, such as climbing stairs, going shopping, and heavy domestic duties. It is likely this subscore was low in patients with JRA because of the involvement of other joints of the lower or upper limbs. In addition, our HSS knee score results were considerably inferior to the 90% excellent results reported for posterior-stabilized primary TKA in 137 consecutive cases in a general orthopaedic population [11]. Nevertheless, TKA in this group of patients with advanced JRA provided worthwhile patient-reported benefits, notwithstanding limited postoperative function as determined by traditional outcome measures.
Fig. 3A–C.
EQ-5D scores for patients with JRA at followup were compared with the population norms for people 30 to 39 years old [15]: (A) Level 1, indicating no problem; (B) Level 2, indicating some problem; and (C) Level 3, indicating an extreme problem. Mob = mobility; Self = self-care; Act = usual activities; Pain = pain/discomfort; Anx = anxiety/depression.
The SF-36, EQ-5D, WOMAC, and HSS scores did not reflect what these profoundly disabled patients identified as positive outcomes. This is expected, because severely affected patients with JRA often have associated polyarticular upper and lower limb joint involvement and lifelong soft tissue contractures that impact their scores. Neer et al. [21] referred to the difficulty of evaluating the outcome of an operation in a polyarticular condition (referring to rheumatoid arthritis) stating, “the use of the term unsatisfactory in the rigid clinical rating system does not depict the true value of the procedure.” Because patients generally reported satisfaction despite results in the poor range on generally accepted objective outcome instruments, the question of how to evaluate the impact of an intervention in one joint in a patient with severe multiple joint involvement is problematic. A patient-specific index [28, 39] may better reflect a patient’s perception of quality of life and should describe the effect of a condition on those aspects of life considered by the patient of greatest importance [16, 28], thereby providing a useful additional measure of outcome in certain patient groups, such as severely disabled patients with JRA.
A midterm review of TKA in this uncommon and severely affected group of patients showed a quality of life and ability to perform activities of living acceptable to our patients, and satisfactory pain levels. The PASI-pg captured issues missed by standardized instruments currently in wide use, indicating patients with JRA who have severe polyarticular involvement highly value TKA despite poor results on standard outcome measures. Surgeons treating this group of patients need not be discouraged, in setting indications for TKA, by low postoperative scores in commonly used outcome measures.
Acknowledgments
We thank Dagmar Gross for assistance in the preparation of the manuscript.
Appendix 1. Questionnaire, including Satisfaction Questions



Footnotes
One of the authors (BMJ) received funding from the Vaud Association Against Rheumatism (Ligue Vaudoise contre le Rhumatisme), Lausanne, Switzerland.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
References
- 1.Aglietti P, Baldini A, Buzzi R, Indelli PF. Patella resurfacing in total knee replacement: functional evaluation and complications. Knee Surg Sports Traumatol Arthrosc. 2001;9(suppl 1):S27–S33. [DOI] [PubMed]
- 2.Beaton DE, Tarasuk V, Katz JN, Wright JG, Bombardier C. “Are you better?” A qualitative study of the meaning of recovery. Arthritis Rheum. 2001;45:270–279. [DOI] [PubMed]
- 3.Bellamy N. WOMAC Osteoarthritis Index: User Guide IV. Herston, Queensland, Australia: University of Queensland Press; 2000.
- 4.Boublik M, Tsahakis PJ, Scott RD. Cementless total knee arthroplasty in juvenile onset rheumatoid arthritis. Clin Orthop Relat Res. 1993;286:88–93. [PubMed]
- 5.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. [DOI] [PubMed]
- 6.Browne GB, Byrne C, Roberts J, Streiner D, Fitch M, Corey P, Arpin K. The meaning of illness questionnaire: reliability and validity. Nurs Res. 1988;37:368–373. [DOI] [PubMed]
- 7.Cage DJ, Granberry WM, Tullos HS. Long-term results of total arthroplasty in adolescents with debilitating polyarthropathy. Clin Orthop Relat Res. 1992;283:156–162. [PubMed]
- 8.Carmichael E, Chaplin DM. Total knee arthroplasty in juvenile rheumatoid arthritis: a seven-year follow-up study. Clin Orthop Relat Res. 1986;210:192–200. [PubMed]
- 9.EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. [DOI] [PubMed]
- 10.Ewald FC. The Knee Society total knee arthroplasty roentgenographic evaluation and scoring system. Clin Orthop Relat Res. 1989;248:9–12. [PubMed]
- 11.Groh GI, Parker J, Elliott J, Pearl AJ. Results of total knee arthroplasty using the posterior stabilized condylar prosthesis: a report of 137 consecutive cases. Clin Orthop Relat Res. 1991;269:58–62. [PubMed]
- 12.Hargreaves DG, Hampton RW, McCullough CJ. Total knee arthroplasty in juvenile chronic arthritis. J Orthop Rheumatol. 1996;9:119–122.
- 13.Hopman WM, Towheed T, Anastassiades T, Tenenhouse A, Poliquin S, Berger C, Joseph L, Brown JP, Murray TM, Adachi JD, Hanley DA, Papadimitropoulos E. Canadian normative data for the SF-36 Health Survey. Canadian Multicentre Osteoporosis Study Research Group. CMAJ. 2000;163:265–271. [PMC free article] [PubMed]
- 14.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–765. [PubMed]
- 15.Johnson JA, Pickard AS. Comparison of the EQ-5D and SF-12 health surveys in a general population survey in Alberta, Canada. Med Care. 2000;38:115–121. [DOI] [PubMed]
- 16.Jolles BM, Buchbinder R, Beaton DE. A study compared nine patient-specific indices for musculoskeletal disorders. J Clin Epidemiol. 2005;58:791–801. [DOI] [PubMed]
- 17.Lingard EA, Wright EA, Sledge CB, Kinemax Outcomes Group. Pitfalls of using patient recall to derive preoperative status in outcome studies of total knee arthroplasty. J Bone Joint Surg Am. 2001;83:1149–1156. [DOI] [PubMed]
- 18.Lybäck CO, Belt EA, Hämäläinen MM, Kauppi MJ, Savolainen HA, Lehto MU. Survivorship of AGC knee replacement in juvenile chronic arthritis: 13-year follow-up of 77 knees. J Arthroplasty. 2000;15:166–170. [DOI] [PubMed]
- 19.Mahomed NN, Koo Seen Lin MJ, Levesque J, Lan S, Bogoch ER. Determinants and outcomes of inpatient versus home based rehabilitation following elective hip and knee replacement. J Rheumatol. 2000;27:1753–1758. [PubMed]
- 20.Mancuso CA, Charlson ME. Does recollection error threaten the validity of cross-sectional studies of effectiveness? Med Care. 1995;33(4 suppl):AS77–AS88. [PubMed]
- 21.Neer CS 2nd, Watson KC, Stanton FJ. Recent experience in total shoulder replacement. J Bone Joint Surg Am. 1982;64:319–337. [PubMed]
- 22.Nordeson A, Engström B, Norberg A. Self-reported quality of life for patients with progressive neurological diseases. Qual Life Res. 1998;7:257–266. [DOI] [PubMed]
- 23.Palmer DH, Mulhall KJ, Thompson CA, Severson EP, Santos ER, Saleh KJ. Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 2005;87:1510–1514. [DOI] [PubMed]
- 24.Parvizi J, Lajam CM, Trousdale RT, Shaughnessy WJ, Cabanela ME. Total knee arthroplasty in young patients with juvenile rheumatoid arthritis. J Bone Joint Surg Am. 2003;85:1090–1094. [DOI] [PubMed]
- 25.Peterson LS, Mason T, Nelson AM, O’Fallon WM, Gabriel SE. Juvenile rheumatoid arthritis in Rochester, Minnesota 1960–1993: is the epidemiology changing? Arthritis Rheum. 1996;39:1385–1390. [DOI] [PubMed]
- 26.Ranawat CS, Bryan WJ, Inglis AE. Total knee arthroplasty in juvenile arthritis. Arthritis Rheum. 1983;26:1140–1144. [DOI] [PubMed]
- 27.Redwine DB. Remote recollection of preoperative pain in patients undergoing excision of endometriosis. J Am Assoc Gynecol Laparosc. 1994;1:140–145. [DOI] [PubMed]
- 28.Ruta DA, Garratt AM, Leng M, Russell IT, MacDonald LM. A new approach to the measurement of quality of life: The Patient-Generated Index. Med Care. 1994;32:1109–1126. [DOI] [PubMed]
- 29.Sarokhan AJ, Scott RD, Thomas WH, Sledge CB, Ewald FC, Cloos DW. Total knee arthroplasty in juvenile rheumatoid arthritis. J Bone Joint Surg Am. 1983;65:1071–1080. [PubMed]
- 30.Smith JK, Falvo D, McKillip J, Pitz G. Measuring patient perceptions of the patient-doctor interaction: development of the PDIS. Eval Health Prof. 1984;7:77–94. [DOI] [PubMed]
- 31.Solomon DH, Bates DW, Horsky J, Burdick E, Schaffer JL, Katz JN. Development and validation of a patient satisfaction scale for musculoskeletal care. Arthritis Care Res. 1999;12:96–100. [DOI] [PubMed]
- 32.Stuart MJ, Rand JA. Total knee arthroplasty in young adults who have rheumatoid arthritis. J Bone Joint Surg Am. 1988;70:84–87. [PubMed]
- 33.Thomas A, Rojer D, Imrie S, Goodman SB. Cemented total knee arthroplasty in patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2005;433:140–146. [DOI] [PubMed]
- 34.Ware JE, Kosinski M, Dewey JE. How to Score Version Two of the SF-36 Health Survey. Lincoln RI: QualityMetric Inc; 2001.
- 35.Ware JE, Snow KK, Kosinski M. SF-36 Health Survey: Manual, Interpretation Guide. Lincoln RI: QualityMetric Inc; 2000.
- 36.Weir R, Browne G, Roberts J, Tunks E, Gafni A. The Meaning of Illness Questionnaire: further evidence for its reliability and validity. Pain. 1994;58:377–386. [DOI] [PubMed]
- 37.World Health Organization. International Classification of Functioning, Disability and Health: ICF. Geneva, Switzerland: World Health Organization; 2001.
- 38.Wright JG, Young NL. The patient-specific index: asking patients what they want. J Bone Joint Surg Am. 1997;79:974–983. [DOI] [PubMed]
- 39.Wright JG, Young NL, Waddell JP. The reliability and validity of the self-reported patient-specific index for total hip arthroplasty. J Bone Joint Surg Am. 2000;82:829–837. [DOI] [PubMed]