Abstract
The indications for intramedullary nailing have expanded to include most tibial shaft fractures. Nail design has improved since their first introduction, but distal locking remains a difficult part of the procedure, resulting in radiation exposure to the patient and the surgeon and increased operation time. To address these issues, we describe an alternative surgical technique using a newly designed distal targeting device that consists of a proximally mounted aiming arm, and we report the preliminary data from its use in all tibial shaft fractures amenable to surgery for a 2–year period. Sixty-three tibial shaft fractures were treated with this method. The mean duration of the distal locking was 6.5 minutes, and in all successful cases, radiation exposure for distal locking was two shots (one shot before targeting and another for the confirmation of proper screw insertion). Radiation exposure was on average 0.85 seconds (range, 0.4–1.2 seconds) and 1.4 mGy (range, 0.8–1.9 mGy). There were no major intraoperative complications related to the technique. The method has certain advantages and can reduce radiation exposure and operation time. Nonetheless, familiarity with the instrumentation is a prerequisite for accurate distal locking.
Level of Evidence: Level IV Therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Currently, tibial shaft fractures not amenable to nonoperative treatment are treated most commonly with statically locked intramedullary nailing [2, 3]. Despite the fact that nail design has improved, the most demanding part of their implementation remains distal locking [28]. This leads to increased surgical time and increased radiation exposure to the patient and surgical personnel [14, 16, 22, 25]. One study suggests distal locking can increase radiation exposure for the surgeon and the patient as much as 2.6 times [22]. Positioning of the distal screws may present difficulties resulting from bending deformities and torsion after nail insertion [12, 20].
Numerous attempts have been described to resolve this matter [6, 7, 11, 18, 19, 21, 23, 28]. Among these, handheld targeting devices [9, 15], radiolucent drill guides [7, 21], computer-assisted systems [21, 24], proximally mounted devices [10, 12, 19], devices fixed to the image intensifier [5, 8, 27], and navigation-assisted distal locking devices [25] are the most popular. However, despite the plethora of targeting devices, the issues of radiation exposure and decrease of operation time remain controversial [11, 14, 16, 23, 29]. Additionally, the accompanying instrumentation, the technically demanding skills, and the longer learning curve seem to prevent their broader application [11, 28]. This may be why the freehand technique has the most familiarity among surgeons [11, 17, 28].
We asked whether an alternative surgical technique for distal locking of tibial nails would reduce radiation exposure and operation time.
Materials and Methods
We prospectively followed 60 patients with 63 tibial shaft fractures treated using the Stryker S2™ Tibial Intramedullary Nail (Stryker Trauma GmbH, Schönkirchen, Germany) from September 2004 to September 2006. During that time, we saw 95 patients with tibial fractures. Among the 60 patients, 57 patients had unilateral tibial shaft fractures and three had bilateral fractures. We treated all patients with tibial shaft fractures by intramedullary nailing when they met standard inclusion criteria for nailing. These criteria included unstable closed (45 patients) or open (Gustilo Types I, II, and III-A) (15 patients) shaft fractures. We included patients with contralateral injuries (n = 3), stable multitrauma (n = 11), concomitant upper extremity injuries (n = 6), floating knee injuries (n = 2), and segmental tibial fractures (n = 9). We excluded patients with unstable multitrauma (n = 8), Gustilo Types III-B and III-C open fractures (n = 9), preexisting deformity (n = 1), open physes (n = 1), fractures with a wound over the entry portal (n = 2), tibial shafts with a very small (< 8 mm) medullary canal (n = 2), and fractures with intraarticular participation proximally or distally (above the tibial tubercle and 3 cm below the ankle) (n = 3). Nine patients with stable transverse fractures were managed nonoperatively. We (GA, PGN, DC, AP, AA) treated all patients in the study group who had surgery using the same standard operative technique with the same surgical team. An unslotted reamed tibial nail with a proximally mounted targeting device was used. The minimum followup was 18 months (mean, 24 months; range, 18–31 months). Two patients (3%) were lost to followup because they did not return for examinations.
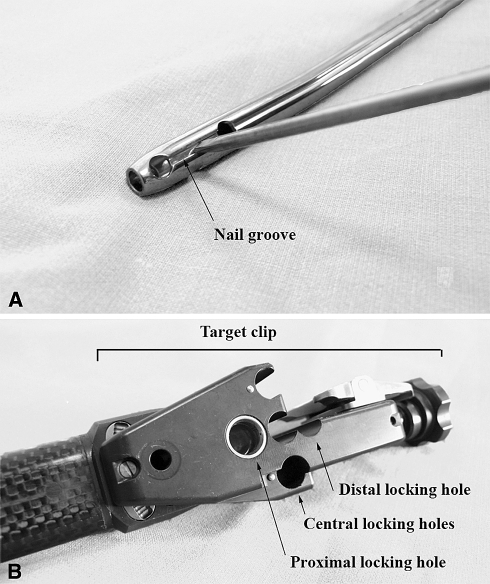
The concept of the specific device lies in the identification and positioning of a landmark on the medial side of the nail [1]. The targeting system consists of three major elements: (1) a nail groove between the two distal locking holes, providing a landmark that pinpoints the exact location of the distal holes (Fig. 1A); (2) a beveled-tip probe to facilitate accurate positioning of the nail groove (Fig. 1A); and (3) a targeting device that permits correct positioning of the distal screws according to the nail’s length. More specifically, the distal end of the device includes a target clip that features two locking holes corresponding to the nail’s holes and three central holes aligned on a perpendicular axis between them. The three central holes serve as a guide for insertion of the probe and localization of the nail’s groove (Fig. 1B).
Fig. 1A–B.
(A) The probe is positioned in the nail’s groove between the two locking holes. (B) The targeting device with the two locking holes and the three central holes is aligned perpendicular between them.
We positioned all patients on a fracture table in the supine position. Using skeletal traction from the talus, nail insertion was performed using the same standard operative technique in all cases [1]. The locking nail and the targeting device were accurately calibrated before insertion. The nail was inserted 10 mm deeper than the intended final position. Once the nail was introduced in the medullary canal, the targeting device was attached to the nail proximally. In cases of very distal tibial shaft fractures (e.g., as much as 30 mm from the metaphysis), the nail could be placed 10 mm deeper than its intended final position, and instead of withdrawing, the nail then was forwarded gently by 10 mm. Afterward, one lateral fluoroscopic image of the distal tibia was obtained to identify possible deformation of the nail and to select which of the three central holes would serve as a pilot hole. Through the central hole that overlapped the nail’s shadow, only the medial cortex was drilled (Fig. 2A). There was no need for the radiographic circles of the pilot holes to be perfect circles. These served as guides for positioning in the anteroposterior plane and helped to choose the most proximal to the nail shadow. Then, the targeting device was removed to clean the pilot hole from the remaining debris. The probe then was introduced through the pilot hole, the groove was palpated, and its position was verified by turning the probe around its axis (Fig. 1A). When the probe was in the groove, it could be turned only a few degrees. Subsequently, the nail was gently retracted proximally by 10 mm while constantly applying pressure on the probe against the groove until the probe fell into the distal locking hole. Verification of proper placement of the probe in the distal locking hole was determined by the inability to twist the nail by the aiming arm. A fixation sleeve then was introduced over the probe to secure the location of the distal locking hole. The targeting device was reattached and firmly fixed to the fixation sleeve. A drill sleeve was positioned through the proximal locking hole (Fig. 1B), the proximal locking hole was drilled, and an appropriately sized screw was inserted. Finally, the probe and the fixation sleeve were removed, the lateral cortex of the distal locking hole was drilled, and another screw was inserted (Fig. 2B). The technique was completed with proximal locking of the nail.
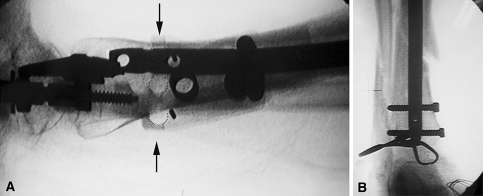
Fig. 2A–B.
(A) Intraoperative C-arm imaging of the distal tibia was performed to select one central hole as the pilot hole (arrows). Through the central hole (dotted circles) that overlapped the nail’s shadow, drilling of the medial cortex was performed only once. In this case, the upper central hole overlaps the shadow of the nail after its deformation. The pilot holes need not be perfect circles because they just served as guides in the anteroposterior plane to choose the closest one to the nail. (B) A final C-arm image shows distal locking of the tibia through the two locking holes.
We recorded the following parameters in each case: the total time required for the operation and for distal locking, exposure from radiation, success or failure of the targeting device, and encountered intraoperative complications. The exposure of radiation was measured in shots, seconds, and milligrays according to intraoperative C-arm readings after each case. Failure of the technique was considered the inability to position the distal hole with the probe and subsequent conversion to the freehand technique; complications included screw penetration of the medial cortex.
Results
The duration of the procedure was 47 ± 9.5 minutes (mean ± standard deviation; range, 35–68 minutes), whereas the duration for distal locking was 6.5 ± 2.1 minutes (range, 4–15 minutes).
In all successful cases, radiation exposure for distal locking was two shots (one shot before targeting and another for confirmation of proper screw insertion). Radiation exposure was an average of 0.85 seconds (range, 0.4–1.2 seconds) and 1.4 mGy (range, 0.8–1.9 mGy).
We had two failures (3.1%) with the procedure. In both cases, identification of the nail’s groove was not possible through the selected pilot hole. Three cases (4.7%) of screw penetration of the medial cortex were recorded. There was no misdrilling because of the circles in the lateral radiograph not being perfect, and there were no problems regarding the nail being placed too proximally after gentle retraction and resulting in being proud. We placed the nail during targeting 10 mm more distally than its final intended position.
Discussion
Deformation of the nail in the coronal and sagittal planes is the main reason proximally mounted targeting devices fail to identify the location of the distal holes [10]. Although rotational and bending forces are less in tibial than in femoral shaft fractures, considerable deformation may occur that can lead to misdrilling of distal holes [10–13]. All types of nails are subject to deformation. Nail deformation increases from solid unreamed nails to unslotted reamed nails to slotted reamed nails, which experience the greatest deformation [4]. The specific nail used in our patients also undergoes an amount of deformation. To address this issue, the specific device introduced an adequate range of distance between the central pilot holes. Additionally, the use of the aiming arm proximally to turn the nail clockwise or counterclockwise and the use of a probe to detect the groove between the distal locking holes made it feasible to detect any rotational deformities as well. These are the main factors that contributed to successful use of the specific operative method.
Although we prospectively followed the patients, we planned no control group for comparison with patients having another concurrent method of distal locking. This allows us to state the reduction in times, but not to directly compare them with times from other approaches. Furthermore, the results from application of the described method may be dependent on the surgeon and the level of familiarity with the instrumentation. A certain learning curve was required to achieve optimal results. Intraoperative radiation exposure varies and depends on the radiographer or the technician assisting in the procedure or the fluoroscopic equipment used. The study design rather was intended to determine problems or complications with the new targeting technique for a 2-year period and to ascertain radiation exposure.
We required two exposures of 0.85 seconds (range, 0.4–1.2 seconds) and 1.4 mGy (range, 0.8–1.9 mGy) in all successful cases. When compared with the results using other techniques [6], radiation exposure during distal locking was 36 seconds (19.08 minutes of surgical time for distal locking and 81 seconds of total fluoroscopy time) for the freehand technique versus 15 seconds (17.06 minutes of surgical time during distal locking and 69 seconds of total fluoroscopy time) for the Orthofix® targeting device (three distal screws). Levin et al. [14] documented 2.7 minutes of fluoroscopy time (range, 0.6–6.6 minutes; 12 mrem average of radiation exposure) for distal locking of tibial nails. Sanders et al. [22] required a mean fluoroscopy time of 3.44 minutes, and Tsalafoutas et al. [26] recently reported an average 137 ± 111 mGy and 5.7 ± 3.5 minutes of radiation exposure for tibial fracture nailing. Nevertheless, a comparison with similar techniques is beyond the scope of this study.
One of the disadvantages of this method is the instrumentation, as with all similar techniques, is associated with a learning curve for the surgeon to become familiar with the technique. Additionally, meticulous débridement of the initial pilot hole before probe insertion helps to securely localize the groove and is of paramount importance.
We encountered no major complications during the technique. Minor complications included screw penetration of the medial cortex (n = 2), which was attributed to poor bone quality. Although initial placement of the distal screws was more time-consuming for the surgeon (mean, 12 minutes), after repeating the procedure (mean n = 4 times), the surgeons gained greater familiarity with it and managed to reduce the mean duration of distal locking to 6 minutes. In all successful cases, exposure from fluoroscopy was only two shots. In 61 attempts, distal locking was uneventful, whereas in two cases, identification of the nail’s groove was unsuccessful. This was attributed to inadequate débridement of the pilot hole. The experienced high success rate can be explained by the fact that nail deformation was within the range of the three central holes, resulting in proper insertion of the probe in the groove.
We believe this method has certain advantages. Principally, its ability to correct for deformation of the nail and properly identify the distal holes can reduce operation time and radiation exposure to the surgeon during nailing of the tibia. Familiarity with the instrumentation and accurate implementation of the operative method are prerequisites for accurate distal locking.
Acknowledgments
We thank Bernd Robioneck, Ronald Prager, Dr. Gilbert Taglang, CTO-Strasbourg, France, and Dr. Henry Mathevon, Dunquerque, France, for contributions to the operative technique.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Anastopoulos G. Distal locking with mechanical jig (author’s own technique). In: Leung KS, Taglang G, Schnettler R, eds. Practice of Intramedullary Locked Nails: New Developments in Techniques and Applications. Vol 3. New York, NY: Springer; 2006:271–274.
- 2.Archdeacon M. Knee and leg: bone trauma—treatment of tibial shaft fractures. In: Vaccaro A, ed. AO Orthopaedic Knowledge Update 8: Home Study Syllabus. 8th ed. Vol 1. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2006:438–439.
- 3.Bong MR, Kummer FJ, Koval KJ, Egol KA. Intramedullary nailing of the lower extremity: biomechanics and biology. J Am Acad Orthop Surg. 2007;15:97–106. [DOI] [PubMed]
- 4.Gausepohl T, Pennig D, Koebke J, Harnoss S. Antegrade femoral nailing: an anatomical determination of the correct entry point. Injury. 2002;33:701–705. [DOI] [PubMed]
- 5.Goodall JD. An image intensifier laser guidance system for the distal locking of an intramedullary nail. Injury. 1991;22:339. [DOI] [PubMed]
- 6.Gugala Z, Nana A, Lindsey RW. Tibial intramedullary nail distal interlocking screw placement: comparison of the free-hand versus distally-based targeting device techniques. Injury. 2001;32(suppl 4):SD21–SD25. [DOI] [PubMed]
- 7.Hashemi Nejad A, Garlick N, Goddard NJ. A simple jig to ease the insertion of distal screws in intramedullary locking nails. Injury. 1994;25:407–408. [DOI] [PubMed]
- 8.Kelley SS, Bonar S, Hussamy OD, Morrison JA. A simple technique for insertion of distal screws into interlocking nails. J Orthop Trauma. 1995;9:227–230. [DOI] [PubMed]
- 9.Knudsen CJ, Grobler GP, Close RE. Inserting the distal screws in a locked femoral nail. J Bone Joint Surg Br. 1991;73:660–661. [DOI] [PubMed]
- 10.Krettek C, Könemann B, Miclau T, Schandelmaier P, Blauth M, Tscherne H. In vitro and in vivo radiomorphometric analyses of distal screw hole position of the solid tibial nail following insertion. Clin Biomech (Bristol, Avon). 1997;12:198–200. [DOI] [PubMed]
- 11.Krettek C, Könemann B, Miclau T, Schandelmaier P, Blauth M, Tscherne H. A new technique for the distal locking of solid AO unreamed tibial nails. J Orthop Trauma. 1997;11:446–451. [DOI] [PubMed]
- 12.Krettek C, Mannss J, Könemann B, Miclau T, Schandelmaier P, Tscherne H. The deformation of small diameter solid tibial nails with unreamed intramedullary insertion. J Biomech. 1997;30:391–394. [DOI] [PubMed]
- 13.Krettek C, Mannss J, Miclau T, Schandelmaier P, Linnemann I, Tscherne H. Deformation of femoral nails with intramedullary insertion. J Orthop Res. 1998;16:572–575. [DOI] [PubMed]
- 14.Levin PE, Schoen RW Jr, Browner BD. Radiation exposure to the surgeon during closed interlocking intramedullary nailing. J Bone Joint Surg Am. 1987;69:761–766. [PubMed]
- 15.MacMillan M, Gross RH. A simplified technique of distal femoral screw insertion for the Grosse-Kempf interlocking nail. Clin Orthop Relat Res. 1988;226:252–259. [PubMed]
- 16.Miller ME, Davis ML, MacClean CR, Davis JG, Smith BL, Humphries JR. Radiation exposure and associated risks to operating-room personnel during use of fluoroscopic guidance for selected orthopaedic surgical procedures. J Bone Joint Surg Am. 1983;65:1–4. [PubMed]
- 17.Pardiwala D, Prabhu V, Dudhniwala G, Katre R. The AO distal locking aiming device: an evaluation of efficacy and learning curve. Injury. 2001;32:713–718. [DOI] [PubMed]
- 18.Pennig D. An improved screw design for locked intramedullary nailing. Injury. 1997;28:162–164. [DOI] [PubMed]
- 19.Pennig D, Oppenheim W, Faccioli G, Rossi S. Intramedullary locked nailing of femur and tibia: insertion of distal locking screws without image intensifier. Injury. 1997;28:323–326. [DOI] [PubMed]
- 20.Prokuski L. Principles of intramedullary nailing. In: Bulstrode C, Buckwalter J, Carr A, Marsh L, Fairbank J, Wilson-McDonald J, Bowden G, eds. Oxford Textbook of Orthopedics, Trauma. Vol 3. 3rd ed. Oxford, UK: Oxford University Press; 2002:1711–1716.
- 21.Rahman MM, Taha WS, Shaheen MM. A simple technique for distal locking of tibial nails. Injury. 1998;29:789–790. [DOI] [PubMed]
- 22.Sanders R, Koval KJ, DiPasquale T, Schmelling G, Stenzler S, Ross E. Exposure of the orthopaedic surgeon to radiation. J Bone Joint Surg Am. 1993;75:326–330. [DOI] [PubMed]
- 23.Saw Y. Closed intramedullary distal locking made easier. Injury. 1993;24:214–215. [DOI] [PubMed]
- 24.Slomczykowski MA, Hofstetter R, Sati M, Krettek C, Nolte LP. Novel computer-assisted fluoroscopy system for intraoperative guidance: feasibility study for distal locking of femoral nails. J Orthop Trauma. 2001;15:122–131. [DOI] [PubMed]
- 25.Suhm N, Messmer P, Zuna I, Jacob LA, Regazzoni P. Fluoroscopic guidance versus surgical navigation for distal locking of intramedullary implants: a prospective, controlled clinical study. Injury. 2004;35:567–574. [DOI] [PubMed]
- 26.Tsalafoutas IA, Tsapaki V, Kaliakmanis A, Pneumaticos S, Tsoronis F, Koulentianos ED, Papachristou G. Estimation of radiation doses to patients and surgeons from various fluoroscopically guided orthopaedic surgeries. Radiat Prot Dosimetry. 2007 June 11. [Epub ahead of print]. [DOI] [PubMed]
- 27.Tyropoulos S, Garnavos C. A new distal targeting device for closed interlocking nailing. Injury. 2001;32:732–735. [DOI] [PubMed]
- 28.Whatling GM, Nokes LD. Literature review of current techniques for the insertion of distal screws into intramedullary locking nails. Injury. 2006;37:109–119. [DOI] [PubMed]
- 29.Wu CC, Shih CH. Biomechanical analysis of the mechanism of interlocking nail failure. Arch Orthop Trauma Surg. 1992;111:268–272. [DOI] [PubMed]