Abstract
We present a case of a 20-year-old college student who had myositis ossificans traumatica develop after a fraternity hazing. The patient was struck repeatedly on both of his thighs while standing at attention, and he presented with bilateral thigh pain and stiffness 6 weeks after the incident. Physical examination revealed 130° flexion of his right knee and 50° flexion of his left knee, which had a firm end point. Radiographs showed extensive new bone located adjacent to the anterior and lateral aspects of his left femur with less involvement of his right thigh. Magnetic resonance imaging revealed considerable edema involving much of the rectus femoris and vastus lateralis of both thighs. The patient was treated with physical therapy and indomethacin for pain and inflammation control. At his 1.5-year followup, the patient’s left knee flexion had improved to 130°. Nonoperative treatment with careful followup resulted in a favorable outcome in this patient despite considerable formation of bilateral thigh myositis ossificans traumatica.
Introduction
Muscle contusion injuries commonly occur in contact sports, potentially leading to considerable morbidity in athletes. Contusions are the second most common cause of disability in athletes, the most common causes being muscular tears and strain. Because of increased awareness of this injury pattern, several contact sports have implemented the use of additional protective padding to help diminish and dissipate the energy sustained by a direct blow. However, sports such as rugby and soccer use minimal protective padding, making these athletes more susceptible to muscle contusion injuries.
Myositis ossificans traumatica (MOT) occurs after blunt trauma to muscle tissue. Although the mechanism of bone formation in the muscle is unclear, the process occurs with an incidence ranging from 9% to 20% in athletes who sustain a direct blow by a body part of an opponent (most often the knee) or by the impact of an opponent’s helmet [15]. The most common site of occurrence is the anterior thigh, and the process develops subsequent to the formation of an intramuscular hematoma [4, 8, 15]. Patients experience tenderness and swelling at the site of injury, and their symptoms are generally unresponsive to 1 week of rest and activity modification. In the acute phase, treatment consists of immobilization of the muscle in tension, ice, and elevation. Pharmacologic interventions such as indomethacin and other nonsteroidal antiinflammatory drugs (NSAIDs) may be used as an adjunct to therapy [4]. Surgery usually is considered in patients who have had continued pain, limited motion, or deterioration of function and is done once ectopic bone has matured.
We present a case report of a college student who was involved in a fraternity hazing and subsequently had MOT develop. To our knowledge, this is the first report of symptomatic MOT secondary to fraternity hazing. The patient and his family members were informed that his case would be used for publication.
Case Report
A 20-year-old male college student presented to the student health department with bilateral thigh pain and swelling of 3 weeks’ duration. The patient, who initially claimed to have sustained the injury during a sporting event, was evaluated by a primary care physician. He subsequently was sent to physical therapy, three times per week for 3 weeks, where he underwent passive quadriceps stretching exercises. At the conclusion of his 3-week course of physical therapy, he began to experience a decrease in motion and function of his left knee and subsequently was referred to the orthopaedic service for further evaluation. At that time, he admitted to having been the victim of a hazing incident, where he was struck repeatedly on both of his thighs for a prolonged period of time while standing at attention. He had been so badly bruised he was unable to walk for the ensuing 2 days. The patient did not seek medical attention at that time, hoping his symptoms would resolve. His medical history was unremarkable and he was not taking any medications.
Examination of his lower extremities revealed full range of motion without pain in both hips. Range of motion of his right knee was from full extension to 130° flexion. There was a 14-cm fixed palpable mass in the proximal anterior right thigh but minimal tenderness to palpation. Examination of the left leg revealed a firm mass spanning much of the entire length of his anterior and lateral thigh. Knee range of motion was from full extension to 50° flexion, at which point there was a relatively firm end point.
Radiographs showed extensive new bone located adjacent to the anterior and lateral aspects of the left femur (Fig. 1) and less involvement of his right thigh (Fig. 2). An MRI was performed at his initial evaluation in the student health clinic to assess soft tissue damage. It revealed edema involving the rectus femoris, vastus lateralis, and an extensive portion of the vastus intermedius (Fig. 3). A diagnosis of MOT was established and the patient was started on an additional 6-week course of outpatient physical therapy consisting of passive quadriceps stretching exercises three times per week. The patient was prescribed 25 mg oral indomethacin three times per day for pain and inflammation control.
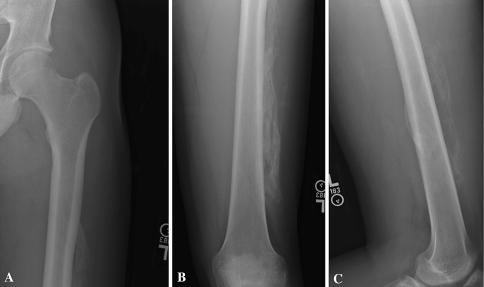
Fig. 1A–C.
(A) An AP radiograph of the left proximal femur taken 6 weeks after injury shows extensive bone formation along the lateral aspect of the thigh. (B) Anteroposterior and lateral (C) views of the left distal femur also reveal bone formation both anteriorly and laterally 6 weeks after injury.
Fig. 2A–C.
(A) An AP radiograph of the right proximal femur taken 6 weeks after injury shows less extensive bone formation along the lateral aspect of the thigh. (B) Anteroposterior view of the right distal femur shows mild bone formation and a lateral (C) view of the right distal femur shows no evidence of bone formation along the anterior or posterior aspects of the thigh.
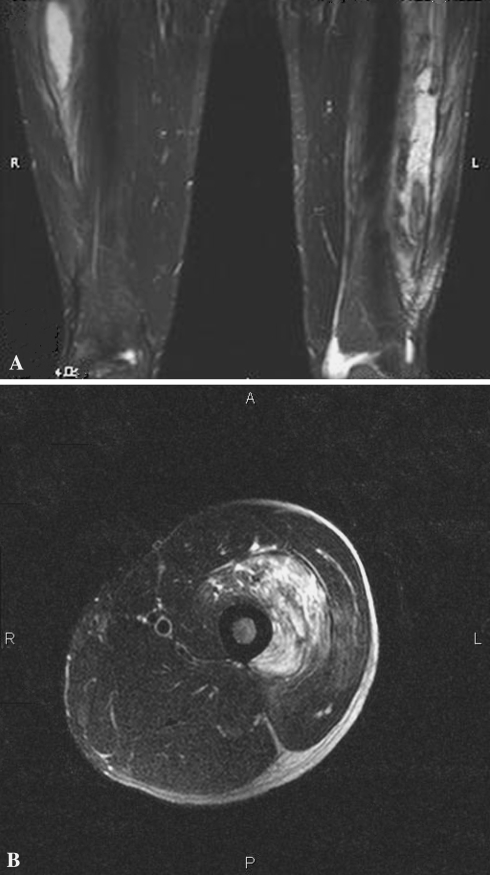
Fig. 3A–B.
(A) A T2-weighted MR scan shows the extent of myositis ossificans measuring approximately 13.3 × 2.3 × 3.5 cm in the left vastus lateralis muscle. There is a similar-appearing lesion in the upper right vastus lateralis measuring approximately 12.2 × 2.2 cm. (B) A T2-weighted axial MR scan shows a well-circumscribed multiloculated signal intensity focus in the vastus intermedius.
Four months after his injury, the patient’s physical examination revealed left knee range of motion from full extension to 115° flexion. Range of motion of his right knee was from full extension to 130° flexion. Radiographs of the left (Fig. 4) and right (Fig. 5) thighs revealed MOT bone formation, which was smaller when compared with previous films. Because of the improvement in his flexion range of motion of both knees, he was continued on a regimen of passive knee stretching at home, which would maximize knee motion and quadriceps strength while minimizing any secondary trauma. In addition, we started him on a home therapy program to evaluate whether his passive range of motion would be hindered by new MOT formation and to determine whether the presence of new bone formation would be sufficiently prominent to cause pain with external pressure. The patient was last seen in followup 1.5 years after injury with no complaints of lower extremity pain. Physical examination revealed bilateral knee flexion to 130°. Repeat radiographs were not performed because of the improvement observed in the clinical examination.
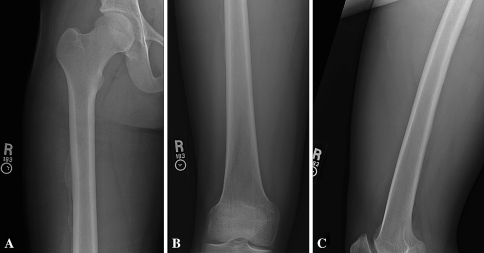
Fig. 4A–C.
(A) An AP radiograph of the left proximal femur taken 4 months after injury shows mature bone formation along the lateral aspect of the thigh. (B) Anteroposterior and lateral (C) views of the left distal femur also reveal mature bone formation both anteriorly and laterally 4 months after injury.
Fig. 5A–C.
(A) An AP radiograph of the right proximal femur taken 4 months after injury shows mature bone formation along the lateral aspect of the thigh. (B) Anteroposterior view of the right distal femur shows mature bone formation and a lateral (C) view of the right distal femur shows no evidence of bone formation along the anterior or posterior aspects of the thigh.
Discussion
Hazing has been practiced for ages, dating back to the days of the ancient Greeks [9]. This process, which was termed “penalism,” was accepted in universities in Greece and Western Europe during the 17th century [16]. University administrators and upperclassmen believed underclassmen were uncivilized and had to be properly groomed. Thus, penalism became a requirement for graduation and students had to produce an official statement that they completed this process before receiving their degree. As a result of serious injuries and reported deaths, state legislation abolished penalism from European universities in the 18th century [16]. Despite the occurrence of accidental deaths, surprisingly, it once again was resurrected in the 20th century as a way for newcomers to learn respect for school organization [9]. In 1933, an agreement was signed among educators of 14 colleges to eliminate serious hazing practices among fraternities and sororities [18]. Despite that agreement, hazing continues to occur at alarming rates and is responsible for frequent injuries. At least 56 fraternity and sorority deaths occurred from 1970 to 1999 [9, 16].
Myositis ossificans traumatica is defined as a nonneoplastic proliferation of cartilage and bone in an area of muscle that has been exposed to trauma. Three different types of MOT have been described in the literature: flat bone formation adjacent to the shaft of bone with damage to the periosteum (periosteal); bone formation that remains attached to the shaft of bone with damage to the periosteum (stalk); and intramuscular bone formation without disruption of the periosteal sleeve (intramuscular or disseminated) [4, 8]. The pathogenesis of MOT formation is largely unknown. Illes et al. [12] hypothesized rapidly proliferating mesenchymal cells ultimately differentiate into bone-forming cells and osteoblasts in the presence of localized tissue anoxia, producing ectopic bone and cartilage. In addition, muscle damage leads to prostaglandin synthesis, which attracts inflammatory cells to the site of injury, aiding the formation of heterotopic bone [19].
Blunt injuries sustained during athletic events or by other traumatic means predispose patients to the formation of MOT. West Point cadets who sustained thigh contusions during intramural athletic events, such as tackle football, lacrosse, and rugby, had a 20% incidence of MOT formation [15]. Ryan et al. [20] subsequently reported an incidence of 9% in 117 cadets who sustained a blunt thigh injury in the same athletic events and were followed for a minimum of 6 months. Both of these studies report the most common sites for MOT formation are the anterior thigh and the brachialis muscle [11, 15, 20].
Myositis ossificans traumatica should be anticipated in patients who sustain substantial blunt trauma to a large muscle or muscle group. Clinicians should have a heightened suspicion in patients who have had major direct trauma to muscle and who have not responded to nonoperative treatment after a period of 5 days or have worsened symptoms after 2 weeks from the inciting event. Patients often describe muscle tenderness, swelling, and stiffness located at the site of impact [5]. According to Ryan et al. [20], a decrease in range of motion adjacent to the site of trauma is the most reliable predictor of MOT formation. Laboratory tests also may help with the diagnosis. Serum alkaline phosphatase levels generally are elevated, as is the erythrocyte sedimentation rate. Some authors propose using a declining alkaline phosphatase level to determine when ectopic bone has reached maturity, allowing for excision [1, 13, 22], but this has never been substantiated as a reliable test.
Initial radiographic changes may be seen as early as 2 to 3 weeks after injury, with definite bone formation evident by 2 months. Computed tomography is a useful adjunct during this maturation phase because it provides a three-dimensional view of the heterotopic bone mass. In the acute phase, MRI is useful, helping to localize the soft tissue lesion [13]. Once bone formation occurs, MR images become increasingly difficult to interpret and no longer are considered a clinically useful moderator at this later stage [4, 8, 15]. Triple-phase bone scans are most helpful in the early detection of MOT and are typically positive a few weeks before bone mineralization is detected on radiographs; they are also helpful in determining the maturity of the lesion once a diagnosis has been made [7]. Ultrasound has been used by many investigators to determine the extent of hematoma formation, and the progression of bone maturation, in blunt muscle injuries [2].
Treatment of MOT in the acute phase consists of rest, ice, short-term splinting in muscle tension, and elevation followed by early range of motion. Twenty-four hours immobilization for mild injuries and 48-hours immobilization for severe injuries followed by well-leg and gravity-assisted motion as soon as pain relief permits are recommended. These studies have led to the currently accepted clinical practice of immobilization only in the period immediately after injury to limit hematoma formation followed by early mobilization.
Although indomethacin is widely used for prevention of heterotopic ossification after total joint arthroplasty, its efficacy in MOT has not been clearly established [3–6, 13–15, 21]. The benefits of NSAIDs such as prostaglandin inhibition and reduced pain in the short term must be weighed against decreased muscular tensile strength and force properties in the longer term. Fisher et al. [10] studied the effect of systemic inhibition of prostaglandin synthesis on muscle protein balance after contusion injury in the rat and reported prostaglandin inhibition reduced the catabolic loss of muscle protein seen locally and peripheral to the injury site. However, Mishra et al. [17] observed rabbit muscles subjected to contusion injury had a deficit in torque and force generation at 28 days if treated with NSAIDs when compared with the control group.
Surgery often is recommended when the patient is left with a limited range of motion, functional limitation, a prominent mass, or enduring pain. Surgery is performed when the bone has fully matured as judged by the presence of a cortex on radiographs typically 6 to 12 months after the inciting event [4, 15].
Patients diagnosed with MOT in the early stages of the disease process often do well with nonoperative therapy. Our patient’s lower extremity function improved considerably despite a delay in diagnosis and treatment. This delay occurred because of the patient’s embarrassment about the true mechanism of injury. Bilateral thigh swelling and pain of this magnitude rarely occur in contact sports. When the presenting history and physical examination do not correlate, as in this case, the evaluating physician should have a high index of suspicion for more profound injury.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Arrington ED, Miller MD. Skeletal muscle injuries. Orthop Clin North Am. 1995;26:411–422. [PubMed]
- 2.Aspelin P, Ekberg O, Thorsson O, Wilhelmsson M, Westlin N. Ultrasound examination of soft tissue injury of the lower limb in athletes. Am J Sports Med. 1992;20:601–603. [DOI] [PubMed]
- 3.Beiner JM, Jokl P. Muscle contusion injuries: current treatment options. J Am Acad Orthop Surg. 2001;9:227–237. [DOI] [PubMed]
- 4.Beiner JM, Jokl P. Muscle contusion injury and myositis ossificans traumatica. Clin Orthop Relat Res. 2002;403(suppl):S110–S119. [DOI] [PubMed]
- 5.Booth DW, Westers BM. The management of athletes with myositis ossificans traumatica. Can J Sport Sci. 1989;14:10–16. [PubMed]
- 6.Danchik JJ, Yochum TR, Aspegren DD. Myositis ossificans traumatica. J Manipulative Physiol Ther. 1993;16:605–614. [PubMed]
- 7.Drane WE. Myositis ossificans and the three-phase bone scan. AJR Am J Roentgenol. 1984;142:179–180. [DOI] [PubMed]
- 8.Ehara S, Shiraishi H, Abe M, Mizutani H. Reactive heterotopic ossification: its patterns on MRI. Clin Imaging. 1998;22:292–296. [DOI] [PubMed]
- 9.Finkel MA. Traumatic injuries caused by hazing practices. Am J Emerg Med. 2002;20:228–233. [DOI] [PubMed]
- 10.Fisher BD, Baracos VE, Reid DC. Effect of systemic inhibition of prostaglandin synthesis on muscle protein balance after trauma in the rat. Can J Physiol Pharmacol. 1991;69:831–836. [DOI] [PubMed]
- 11.Huss CD, Puhl JJ. Myositis ossificans of the upper arm. Am J Sports Med. 1980;8:419–424. [DOI] [PubMed]
- 12.Illés T, Dubousset J, Szendröi M, Fischer J. Characterization of bone forming cells in posttraumatic myositis ossificans by lectins. Pathol Res Pract. 1992;188:172–176. [DOI] [PubMed]
- 13.Iorio R, Healy WL. Heterotopic ossification after hip and knee arthroplasty: risk factors, prevention, and treatment. J Am Acad Orthop Surg. 2002;10:409–416. [DOI] [PubMed]
- 14.Kienapfel H, Koller M, Wüst A, Sprey C, Merte H, Engenhart-Cabillic R, Griss P. Prevention of heterotopic bone formation after total hip arthroplasty: a prospective randomised study comparing postoperative radiation therapy with indomethacin medication. Arch Orthop Trauma Surg. 1999;119:296–302. [DOI] [PubMed]
- 15.King JB. Post-traumatic ectopic calcification in the muscles of athletes: a review. Br J Sports Med. 1998;32:287–290. [DOI] [PMC free article] [PubMed]
- 16.Leslie J, Taff ML, Mulvihill M. Forensic aspects of fraternity hazing. Am J Forensic Med Pathol. 1985;6:53–67. [DOI] [PubMed]
- 17.Mishra DK, Fridén J, Schmitz MC, Lieber RL. Anti-inflammatory medication after muscle injury: a treatment resulting in short-term improvement but subsequent loss of muscle function. J Bone Joint Surg Am. 1995;77:1510–1519. [DOI] [PubMed]
- 18.Nuwer H. Wrongs of Passage: Fraternities, Sororities, Hazing, Binge Drinking. Bloomington IN: Indiana University Press; 1999:24–59.
- 19.Ritter MA, Sieber JM. Prophylactic indomethacin for the prevention of heterotopic bone formation following total hip arthroplasty. Clin Orthop Relat Res. 1985;196:217–225. [PubMed]
- 20.Ryan JB, Wheeler JH, Hopkinson WJ, Arciero RA, Kolakowski KR. Quadriceps contusions: West Point update. Am J Sports Med. 1991;19:299–304. [DOI] [PubMed]
- 21.Thorsson O, Lilja B, Nilsson P, Westlin N. Immediate external compression in the management of an acute muscle injury. Scand J Med Sci Sports. 1997;7:182–190. [DOI] [PubMed]
- 22.Young JL, Laskowski ER, Rock MG. Thigh injuries in athletes. Mayo Clin Proc. 1993;68:1099–1106. [DOI] [PubMed]