Abstract
Guided by a stress process perspective, we investigated (a) whether marital conflict might directly lead to changes in depression and functional impairment, (b) whether marital conflict might indirectly lead to changes in functional impairment via depression, and (c) whether marital conflict might indirectly lead to changes in depression via functional impairment. We estimated a latent variable causal model using 3 waves of data from the National Survey of Families and Households (N = 1,832). Results indicated that marital conflict directly led to increases in depression and functional impairment and indirectly led to a rise in depression via functional impairment. Overall, findings suggest marital conflict is a significant risk factor for psychological and physical health among midlife and older adults.
Keywords: depressive symptoms, functional limitations, marital conflict, marital quality, physical health, psychological well-being
The marital relationship can be a critical physical health resource for adults. Numerous studies have indicated that married men and women, compared to their single counterparts, enjoy better health and longer life (e.g., Gove, 1973; Lillard & Waite, 1995; also see Waite & Gallagher, 2000, for a review). Being married typically is expected to lead to greater availability of emotional, social support, meaning and purpose in life, and social control, which are considered key processes that promote physical wellness (Umberson, 1987). Yet relatively limited population research thus far has explored how differences in marital quality might be associated with differences in health among married adults.
Laboratory-based biopsychosocial research has provided suggestive evidence that poor marital quality might lead to overall deterioration in physical health. For instance, negative verbal and nonverbal exchanges observed in a marital problem-solving task directly led to problematic autonomies, endocrine, and immune alterations at least for short periods of time after the task (Burman & Margolin, 1992; Kiecolt-Glaser & Newton, 2001; Kiecolt-Glaser et al, 2005). Also, a few recent community-based surveys have demonstrated that poor marital quality is associated with negative physical health outcomes such as greater functional impairment or lower self-rated health (Bookwala, 2005; Hawkins & Booth, 2005; Umberson, Williams, Powers, Liu, & Needham, 2006).
This study examined the effects of marital conflict on changes in depressive symptoms and functional impairment among married men and women with a longitudinal national sample. Ample evidence exists that lower marital quality is associated with deleterious mental health out-comes such as lower levels of life satisfaction or higher levels of depressive symptoms (see Ross, Mirowsky, & Goldsteen, 1990, for a review). Existing research, however, has been limited to evaluating only the direct effects of marital quality, without considering the linkage between mental and physical health. For instance, past research did not take into account depressive symptoms in investigating the effect of marital quality on functional limitations.
To extend previous literature on marital quality and health, we investigated the following three research questions: (a) Does marital conflict directly lead to increases in depressive symptoms and functional impairment? (b) Does marital conflict indirectly lead to an increase in functional impairment via an increase in depressive symptoms? (c) Does marital conflict indirectly lead to an increase in depressive symptoms via an increase in functional impairment? We estimated a latent variable causal model with three waves of data from a nationally representative sample of midlife and older adults, which allowed us to take into account all possible bidirectional associations among the variables of interest.
Theoretical Background
A stress process theoretical framework (e.g., Cassel, 1976; Pearlin, Menaghan, Lieberman, & Mullan, 1981) guided this study. Stress process perspectives posit that chronic strains in key social roles such as marriage, parenthood, or work can cause stress, which typically manifests in the form of psychological or physical distress. Health researchers have proposed physiological, psychological, and behavioral mechanisms that might explain how marital role strain takes a toll on health. First, scholars have asserted that negative verbal and nonverbal exchanges with a spouse that persist over time might incur permanent autonomic, endocrine, and immunological changes (Robles & Kiecolt-Glaser, 2003). The effect of altered physiology from repeated exposure to stress might accumulate over time as a heightened allostatic load or cumulative physiological dysregulation, eventually leading to disease and illness (McEwen, 1998). Also, persons in a high-conflict marriage might be more likely to engage in unhealthy behaviors (e.g., smoking, drinking) and less likely to receive the benefits of benevolent social control (e.g., be encouraged by their partner to exercise and engage in preventive medical care) because their spouses might refrain from exercising social control to avoid more conflict. Once health problems develop or are aggravated, they might be experienced as a stressful life event or chronic stress, subsequently leading to negative mental health outcomes such as depression (Bruce, 2000).
Marital conflict might also directly temper processes leading to good mental health. A distressed marriage might limit spouses’ desire to seek emotional support from their partners or other relationships because of the binding nature of the marital relationship. Being in a low-quality marriage might deplete a sense of meaning and purpose in life. Marital discord might also place greater strains in other areas of life such as work (Rogers & May, 2003) or parenting (Erel & Burman, 1995). Numerous studies have found that a low-quality marriage puts individuals at greater risk for depression (see Whisman, 2001, for a review). Subsequently, depression might lead to the onset or aggravation of physical health conditions in various ways. Depressive symptoms have been associated with poor health behaviors (e.g., poor diet, lack of exercise), less motivation to use preventive care and seek medical treatments if health problems exist, and increased tendency to exaggerate physical symptoms (Bruce, 2000; Ormel, Rijsdijk, Sullivan, van Sonderen, & Kempen, 2002).
Literature Review
The aim of this study was to better understand the potentially complex processes through which marital disagreement may affect changes in depressive symptoms and functional limitations, both directly and indirectly. Because of the lack of studies investigating prospective associations among all three variables, we reviewed empirical studies examining associations between any two of them. In doing so, we placed emphasis on evaluating the strength of evidence regarding reciprocal associations. Thus far, the relation between depressive symptoms and functional limitations has consistently been found to be bidirectional. Research findings regarding reciprocity between marital conflict and depressive symptoms appear to be mixed, perhaps because of extensive dependence on convenience samples. Marital conflict and functional health appear to have bidirectional effects, but only a handful of population studies has examined prospective associations between marital conflict and functional limitations.
The Association Between Marital Quality and Depressive Symptoms
Cross-sectional studies have provided consistent evidence that marital dissatisfaction is associated with higher levels of depressive symptoms (see Whisman, 2001, for a review). Congruent with cross-sectional findings, longitudinal studies also have demonstrated that individuals in unhappy marriages experience increases in depressive symptoms (e.g., Beach, Katz, Kim, & Brody, 2003; Whisman & Bruce, 1999; Williams, 2003). Often, however, research has assumed the direction of causality, thereby examining only the unidirectional relation from marital quality to depressive symptomatology.
To disentangle reciprocal patterns of influences, Fincham, Beach, Harold, and Osborne (1997) employed a cross-lagged panel model with 150 newlywed couples. Results indicated that, for men, depression led to deceases in marital quality, whereas low marital quality increased depressive symptoms for women. Kurdek (1998), however, did not replicate the findings of Fincham and colleagues, even though Kurdek also evaluated the bidirectional associations with newly married couples. Whisman (2001) concluded that findings from longitudinal studies of the marital quality and depressive symptoms linkage are inconsistent in terms of the strength of bidirectional influences and gender differences.
The Association Between Marital Quality and Physical Health
Only a small number of studies have investigated the association between marital quality and physical well-being using population data either cross-sectionally or longitudinally. In a cross-sectional study, Bookwala (2005) found that negative spouse behaviors were positively associated with physical symptoms, chronic health problems, and functional limitations. Congruent with the cross-sectional findings, longitudinal studies also have demonstrated that marital strain is associated with declines in self-rated health over time (Hawkins & Booth, 2005; Umberson et al., 2006).
Umberson and colleagues (2006) took their longitudinal research a step further by evaluating whether marital strain and self-rated health mutually influence each other. Without ruling out the possibility of reciprocity, their work suggested that the effect of marital strain on self-rated health might be stronger than the effect of self-rated health on marital strain. They found no significant gender variation in the marital strain and self-assessed health link.
Hawkins and Booth (2005) compared the health of individuals who consistently reported low marital quality over 12 years with that of divorced individuals, given that a significant minority of adults remains in chronically distressed marriages. They found that unhappily married individuals perceived their health to be significantly worse than did divorced persons who stayed unmarried. This result is significant, given findings from existing studies that divorced individuals fare worse compared to married individuals (see Waite & Gallagher, 2000, for a review).
Taking a different perspective, the marriage selection hypothesis (e.g., Goldman, 1993) suggests that reverse causality might also be operative between marital quality and physical health. That is, physically unhealthy persons might be more likely to be selected out of marriage or to end marriage. In support of this hypothesis, a decline in self-rated physical health was found to lead to lower marital quality for a national sample of married men and women (Booth & Johnson, 1994). Thus, for married persons, one possibility is that poor health might be a contributing factor to a decline in marital quality, and eventually divorce.
The Association Between Depressive Symptoms and Physical Health
Among all possible bivariate associations between marital quality, depressive symptoms, and physical health, associations between depressive symptoms and physical health outcomes have been examined and supported most systematically with older population samples. Studies have demonstrated mat depression is a risk factor for the onset of functional impairment for older adults, and effective treatment of depression improves functional health outcomes (Ormel et al., 2002). Changes in functional health also have consequences for depression, especially when functional impairment limits older persons’ ability to remain socially active (see Bruce, 2000, for a review). A vast majority of studies, however, have evaluated only unidirectional relations between depressive symptoms and physical health outcomes.
In contrast, Aneshensel, Frerichs, and Huba (1984) used a representative area sample of 744 men and women aged 18 or older to investigate both contemporaneous and lagged reciprocal associations between depressive symptoms and physical health. Depressive symptoms and physical health status were measured four times and the interval between each assessment was 4 months. Results from their study indicated that the effect of physical health on depressive symptoms tends to be contemporaneous, whereas the effect of depressive symptomatology on physical health emerges over time. Notably, no major differences in the prospective associations between depressive symptoms and physical health were found between men and women or between different age groups. Employing the same cross-lagged panel design for older adults with physical limitations, Ormel and colleagues (2002) replicated these findings.
Correlates of Marital Quality, Depressive Symptoms, and Physical Health
Previous research has suggested that age, gender, race/ethnicity, education, and income are socio-demographic correlates of marital quality, depressive symptoms, and general physical health outcomes. Studies have found that marital quality (Umberson et al, 2006; VanLaningham, Johnson, & Amato, 2001) and physical health (House, Kessler, & Herzog, 1990) deteriorate over time. In contrast, depressive symptoms tend to be highest in younger adulthood (Mirowsky & Ross, 1992). In terms of the effect of gender on marital quality and health, recent population studies suggest that women are no less happy than men in their marriages (Williams, 2003). Many studies, however, have found that women, compared to men, report more depressive symptoms (Kessler & McLeod, 1984) and physical health problems (Merrill, Seeman, & Kasl, 1997). Race and ethnicity also are significant correlates of our variables of interest. Whites, compared to non-Whites, have been found to be happier with their marriages (Broman, 1993), less depressed (George & Lynch, 2003), and physically healthier (Williams & Collins, 1995). Finally, persons with higher levels of education and income are happier with their marital relationships (Karney & Bradbury, 1995), less depressed (Stansfeld & Marmot, 1992), and healthier (Ross & Wu, 1995). Given all these documented associations, we controlled for age, gender, race/ethnicity, education, and income in our final model.
Limitations of Previous Research
The literature reviewed above regarding linkages between marital conflict, depressive symptoms, and health has three major limitations. First, despite physical, theoretical, and empirical indications, few studies to date have systematically examined bidirectional effects between marital conflict and depressive symptoms or functional impairment with population samples. Second, although previous research has demonstrated the bidirectional association between depressive symptoms and functional limitations, this reciprocity has rarely been taken into consideration in the context of marital conflict. Given the bidirectional influence between depressive symptoms and functional limitations, as well as the associations of these two health outcomes with marital conflict, we expected that marital conflict might evidence a different pattern of influence on depressive symptoms and functional limitations when the bidirectionality between the two health outcomes is taken into account. Third, marital discord, depressive symptomatology, and functional impairment measures, although typically skewed toward more positive levels in the population, have often been treated as normally distributed variables, thereby introducing bias in parameter estimates to some unknown degree and potentially leading to errors in conclusions (for an exception, see Aneshensel et al., 1984).
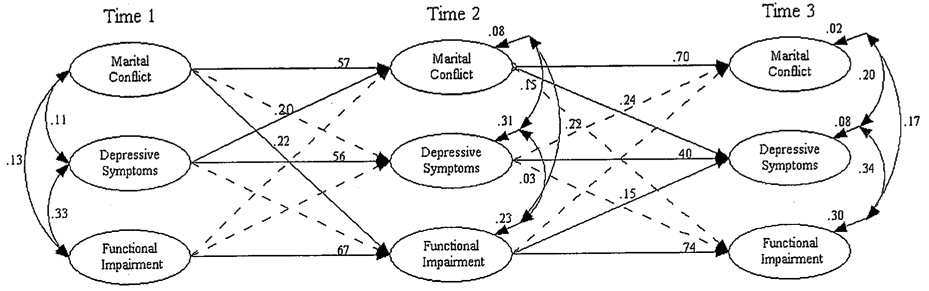
To address these limitations, we employed a cross-lagged panel model with three waves of data from a nationally representative sample of both midlife and older adults. Three data points allowed us to evaluate both direct and indirect effects of marital conflict on both depressive symptoms and functional limitations by estimating all possible bidirectional associations. We also employed a correction for the nonnormality of study variables. See Figure 1 for the conceptual model guiding this study.
FIGURE 1. Structural Equation Model of Marital Conflict, Depressive Symptoms, and Functional Impairment (Standardized Solution, N = 1,832).
Note: Straight lines denote statistically significant paths (t values ≥3). Dashed lines indicate estimated but nonsignificant paths. Curved arrows at Time 1 denote correlations among latent factors. Curved arrows within Time 2 and Time 3 refer to correlations among structural equation errors. Control variables (i.e., age, gender, race/ethnicity, education, and income at each wave), indicators of latent constructs, and their measurement errors are not shown.
METHOD
Data and Sample
The data for this study came from three waves of the National Survey of Families and Households (NSFH). At Time 1 (T1, 1987 – 1988), 13,007 noninstitutionalized U.S. adults aged 19 and older were recruited and interviewed in person. The T1 data consisted of a main sample of 9,637 respondents and an additional oversample of African Americans, Mexican Americans, Puerto Ricans, single parents, stepparents, cohabitors, and recently married persons (response rate = 75%). At Time 2 (T2, 1992 – 1994), 10,005 of the original respondents from the first wave completed a second face-to-face interview (response rate = 82%). At Time 3 (T3, 2001 – 2002), only a subset of T1 respondents was reinterviewed: specifically, individuals who did not have a focal child but who were 45 or older at T3 (about 30 or older at T1) or individuals who had an eligible focal child at T3. A total of 4,596 respondents (response rate = 59%) completed the telephone survey at T3. (See details on the NSFH and the Time 3 field report at http://www.ssc.wisc.edu/nsfh/codedata3.htm.) The analytic sample for this study was limited to persons aged 45 or older at T3 who were also continuously married to the same spouse across all three waves of data collection, a total of 1,832 adults (about 40% of the total of 4,596 who participated at T3). About one quarter of the 1,832 eligible cases had at least one missing value in analytic variables. Therefore, we employed multiple imputation for all analyses.
Measures
Marital disagreement was assessed with a four-item marital disagreement measure adapted from previous marital quality instruments for the NSFH. At each wave, respondents were asked to rate the frequency of their marital disagreement on a 6-point scale with the following questions: “How often, if at all, in the past year have you had open disagreements about each of the following: (a) household tasks, (b) money, (c) spending time together, (d) sex?” (1 = never, 2 = less than once a month, 3 = several times a month, 4 = about once a week, 5 = several times a week, 6 = almost everyday). (Descriptive statistics for all analytic variables are reported in Table 1.)
Table 1.
Descriptive Statistics for Analytic Variables (N = 1,832)
| Variables | M | SD |
|---|---|---|
| Sociodemographic controls | ||
| Age at T1 (in years) | 44.52 | 10.35 |
| Female (coded 1) | 0.54 | 0.50 |
| Non-White (coded 1) | 0.12 | 0.32 |
| Education at T1 (in years) | 13.70 | 2.89 |
| Logged couple income at T1 | 10.74 | 0.58 |
| Logged couple income at T2 | 10.77 | 0.73 |
| Logged couple income at T3 | 10.95 | 0.91 |
| Marital disagreement | ||
| T1 household tasks | 1.85 | 0.89 |
| T1 money | 1.89 | 0.96 |
| T1 time together | 1.84 | 1.14 |
| T1 sex | 1.64 | 0.97 |
| T2 household tasks | 1.93 | 0.98 |
| T2 money | 1.96 | 1.02 |
| T2 time together | 1.84 | 1.09 |
| T2 sex | 1.72 | 1.00 |
| T3 household tasks | 1.81 | 0.98 |
| T3 money | 1.76 | 0.94 |
| T3 time together | 1.60 | 0.89 |
| T3 sex | 1.45 | 0.77 |
| Negative affect | ||
| T1 blue | 0.60 | 1.33 |
| T1 depressed | 0.91 | 1.51 |
| T1 fearful | 0.51 | 1.30 |
| T1 lonely | 0.59 | 1.34 |
| T1 sad | 0.85 | 1.49 |
| T2 blue | 0.68 | 1.37 |
| T2 depressed | 0.97 | 1.52 |
| T2 fearful | 0.56 | 1.27 |
| T2 lonely | 0.60 | 1.32 |
| T2 sad | 0.93 | 1.50 |
| T3 blue | 0.54 | 1.32 |
| T3 depressed | 0.75 | 1.53 |
| T3 fearful | 0.50 | 1.37 |
| T3 lonely | 0.54 | 1.32 |
| T3 sad | 0.89 | 1.62 |
| Functional limitations | ||
| T1 functional limitations sum | 0.11 | 0.50 |
| T2 functional limitations sum | 0.43 | 0.95 |
| T3 functional limitations sum | 0.57 | 1.11 |
Note: Data source is the National Survey of Families and Households, 1987 – 2002. Respondents aged 45 or older at T3 who were continuously married to the same spouse across three waves. T1 = Time 1, T2 = Time 2, T3 = Time 3. Means for dichotomous variables are proportions. Descriptive statistics are averages from 10 imputed data sets.
Negative affect was measured with five items from the Center for Epidemiological Studies Depression (CES-D) index (Radloff, 1977). The NSFH included 12 items assessing two depressive symptoms subdimensions — negative affect and somatic symptoms — from the original 20-item version of the CES-D. We employed only the negative affect items in analyses to reduce potential confounding between depressive symptoms and functional limitations, especially among older adults (Grayson, Mackinnon, Jorm, Creasey, & Broe, 2000). The five negative affect items were, “On how many days during the past week did you: (a) feel blue, (b) feel depressed, (c) feel fearful, (d) feel lonely, (e) feel sad.” The responses varied from 0 = never to 7 = every day during the week.
Functional limitations were assessed with four items. At T1 of the NSFH, respondents indicated, with yes (1) or no (0), if they had a physical or mental condition that limited their ability to (a) care for personal needs, such as bathing, dressing, eating, or going to the bathroom; (b) do day-to-day household tasks; (c) climb a flight of stairs; (d) walk six blocks. At both T2 and T3, this yes or no response range was expanded to assess the degree to which respondents were functionally constrained in each of the four areas (i.e., 1 = does not limit at all, 2 = limits a little, 3 = limits a lot). To retain the consistency of measurement across waves, the 3-point Likert scale used at T2 and T3 was rescaled to 0 (does not limit at all) and 1 (limits a little or a lot).
Sociodemographic correlates: Our causal models were estimated with controls for age at T1 (in years), gender (1 = female, 0 = male), race/ethnicity (1 = non-White, 0 = non-Hispanic White), education at T1 (in years), and logged couple income measured at each wave [ln (5,000 + couple income)]. Income was measured by combining all possible sources of income: serf-employment, wages/salaries, social security, pensions/annuities, public assistance, any other government programs, child support/alimony, interest/dividends, and any other source of income.
Analytic Sequence
We used structural equation modeling (SEM) with latent variables (Bollen, 1989) to evaluate cross-lagged associations among marital conflict, depressive symptoms, and functional impairment. As noted above, a significant level of missing data motivated us to employ multiple imputation to help deal with the bias resulting from missing data (Allison, 2002). For example, income at T1 contributed to the greatest loss of cases, about 15% of the analytic sample reported missing on this variable. To avoid some of the bias to estimates that listwise deletion might cause, we created 10 imputed data sets with the Markov chain Monte Carlo (MCMC) algorithm. Results from each imputation were pooled through the standard process of generating parameter estimates and standard errors. Multiple imputation was performed using all variables included in measurement models (Allison).
Prior to estimating structural or causal relations among latent constructs, we specified associations between measured variables and latent factors. In other words, we first evaluated measurement properties of marital conflict, depressive symptoms, and functional impairment. To differentiate measured variables and latent constructs, we refer to latent constructs of marital disagreement, negative affect, and functional limitations as marital conflict, depressive symptoms, and functional impairment, respectively, in the Results section. We assumed that socio-demographic variables (i.e., age, gender, race/ethnicity, education, and logged couple income) were perfectly measured. As a result, they were included in analyses as latent factors with their measurement errors set to zero.
Because of the low prevalence of individuals high on marital disagreement; negative affect, or functional limitations, the distributions of these variables displayed high degrees of skewness and kurtosis. Therefore, we used polychoric correlations and their asymptotic covariance matrices that were estimated with PRELIS (Jöreskog & Sorbom, 1996). Polychoric correlations are correlations among the underlying continuous variables of the observed ordinal variables in the bivariate normal distribution (Jöreskog, 2002). Importantly, we assumed equal thresholds for the underlying continuous variable of the same observed ordinal variable across time so that the underlying continuous variable would be on the same scale over time (Jöreskog). To obtain parameter estimates and model fit indices, we used Weighted Least Squares (WLS). In addition to examining chi-square statistics as an indicator of overall model fit, we also evaluated the Bayesian Information Criterion (BIC) to assess model fit (Raftery, 1995). In evaluating individual paths, we considered t values equal to or greater than 3 as the evidence of statistical significance, given that our sample size is over 1,000 (Raftery).
RESULTS
Measurement Models
For all observed indicators of marital conflict, depressive symptoms, and functional impairment, we estimated a series of three-factor models. For instance, a marital conflict factor was hypothesized to have four marital disagreement indicators at each of three measurement occasions. Similarly, a depressive symptoms factor and a functional impairment factor were posited at each of the three time points, with five negative affect indicators and four functional limitations indicators, respectively. The three factors of the same latent construct (e.g., marital conflict factors at T1, T2, and T3) were allowed to correlate. In the first baseline model, none of the measurement errors was allowed to correlate (Model 1). Table 2 reports goodness of fit statistics for all measurement models evaluated for marital conflict, depressive symptoms, and functional impairment factors.
Table 2.
Goodness of Fit Statistics for Measurement Models of Marital Conflict, Depressive Symptoms, and Functional Impairment (N = 1,832)
| Marital Conflict | Depressive Symptoms | Functional Impairment | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| χ2 | df | p | BIC | χ2 | df | p | BIC | χ2 | df | p | BIC | |
| Model 1. Baseline Model | 662.92 | 51 | .00 | 279.75 | 369.79 | 87 | .00 | −283.86 | 119.44 | 51 | .01 | −263.73 |
| Model 2. Correlated errors among the same indicators across time | 150.62 | 39 | .00 | −142.40 | 244.96 | 72 | .00 | −295.99 | 63.58 | 39 | .01 | −229.43 |
| Model 3. Correlated errors between adjacent indicators | 492.39 | 42 | .00 | 176.84 | 279.35 | 75 | .00 | −284.14 | 82.23 | 42 | .00 | −233.32 |
| Model 4. Model 2 + Model 3 | 47.17 | 30 | .03 | −178.22 | 114.56 | 60 | .00 | −336.23 | 34.02 | 30 | .28 | −191.38 |
| Model 5. Model 4 + equality constraints on factor loadings on the same indicators across time | 54.40 | 36 | .00 | −216.07 | 124.84 | 68 | .00 | −386.06 | 41.41 | 36 | .25 | −229.06 |
| Model 6. Model 5 + equality constraints on all indicators across time | 100.03 | 38 | .00 | −185.47 | 301.66 | 71 | .00 | −231.78 | 42.25 | 38 | .29 | −243.26 |
Note: BIC = Bayesian Information Criterion.
Next, we examined two possible sources of measurement errors. First, we allowed measurement errors of the same indicators measured at different time points to correlate (Model 2). Second, we allowed measurement errors between adjacent items of a factor to correlate (Model 3). Model 4 introduced these two modifications for measurement errors at the same time. Most importantly, Model 5 placed equality constraints, in addition to introducing the two modifications for measurement errors that were included in Model 4, to investigate whether factor loadings of repeated measures would be equal across time. The invariance of factor loadings across time is a necessary condition for longitudinal analyses, allowing us to compare the same latent constructs over time on the same scale (Jöreskog, 2002). Lastly, Model 6 placed further equality constraints to test whether all the indicators were explained by the latent factor to the same degree across time (e.g., all factor loadings of functional limitations indicators were equated with each other at all three time points). Based on chi-square difference tests, Model 5 was the best-fitting model for marital conflict and depressive symptoms and Model 6 was the best-fitting model for functional impairment. We also evaluated BIC statistics for the best-fitting models for marital conflict and depressive symptoms, because their chi-square statistics were significant (see Table 2). Given that functional impairment was equally well measured with each indicator across time, we used sum scores of observed functional limitations variables in the structural model, with their measurement errors set to zero. Table 3 reports parameter estimates and standard errors for the best-fitting measurement models for marital conflict, depressive symptoms, and functional impairment.
Table 3.
Parameter Estimates and Standard Errors (SE)for Marital Conflict, Depressive Symptoms, and Functional Impairment Measurement Models (N = 1,832)
| Parameter | Unstandardized Estimate | SE | Standardized Estimate |
|---|---|---|---|
| Marital conflict (MC) | |||
| T1 MC → T1 household tasks | 1.00 | — | 0.72 |
| T1 MC → T1 money | 1.09 | 0.03 | 0.82 |
| T1 MC → T1 time together | 0.98 | 0.03 | 0.73 |
| T1 MC → T1 sex | 0.87 | 0.03 | 0.69 |
| T2 MC → T2 household tasks | 1.00 | — | 0.72 |
| T2 MC → T2 money | 1.09 | 0.03 | 0.82 |
| T2 MC → T2 time together | 0.98 | 0.03 | 0.73 |
| T2 MC → T2 sex | 0.87 | 0.03 | 0.70 |
| T3 MC → T3 household tasks | 1.00 | — | 0.73 |
| T3 MC → T3 money | 1.09 | 0.03 | 0.84 |
| T3 MC → T3 time together | 0.98 | 0.03 | 0.75 |
| T3 MC → T3 sex | 0.87 | 0.03 | 0.71 |
| Depressive symptoms (Dep) | |||
| T1 Dep → T1 blue | 1.00 | — | 0.90 |
| T1 Dep → T1 depressed | 1.08 | 0.02 | 0.94 |
| T1 Dep → T1 fearful | 0.87 | 0.02 | 0.77 |
| T1 Dep → T1 lonely | 0.90 | 0.02 | 0.85 |
| T1 Dep → T1 sad | 1.00 | 0.02 | 0.90 |
| T2 Dep → T2 blue | 1.00 | — | 0.90 |
| T2 Dep → T2 depressed | 1.08 | 0.02 | 0.95 |
| T2 Dep → T2 fearful | 0.87 | 0.02 | 0.78 |
| T2 Dep → T2 lonely | 0.90 | 0.02 | 0.86 |
| T2 Dep → T2 Sad | 1.00 | 0.02 | 0.91 |
| T3 Dep → T3 blue | 1.00 | — | 0.90 |
| T3 Dep → T3 depressed | 1.08 | 0.02 | 0.94 |
| T3 Dep → T3 fearful | 0.87 | 0.02 | 0.78 |
| T3 Dep → T3 lonely | 0.90 | 0.02 | 0.86 |
| T3 Dep → T3 sad | 1.00 | 0.02 | 0.91 |
| Functional impairment (FI) | |||
| T1 FI → T1 personal needs | 1.00 | — | 0.90 |
| T1 FI → T1 household tasks | 1.06 | 0.03 | 0.96 |
| T1 FI → T1 flight of stairs | 1.06 | 0.03 | 0.96 |
| T1 FI → T1 walk six blocks | 1.06 | 0.03 | 0.96 |
| T2 FI → T2 personal needs | 1.00 | — | 0.86 |
| T2 FI → T2 household tasks | 1.06 | 0.03 | 0.92 |
| T2 FI → T2 flight of stairs | 1.06 | 0.03 | 0.92 |
| T2 FI → T2 walk six blocks | 1.06 | 0.03 | 0.92 |
| T3 FI → T3 personal needs | 1.00 | — | 0.88 |
| T3 FI → T3 household tasks | 1.06 | 0.03 | 0.93 |
| T3 FI → T3 flight of stairs | 1.06 | 0.03 | 0.93 |
| T3 FI → T3 walk six blocks | 1.06 | 0.03 | 0.93 |
Note: t values (unstandardized estimate/standard error) for all parameters were significant (i.e., t values ≥ 3).
Structural Model
After specifying measurement models for marital conflict, depressive symptoms, and functional impairment, we evaluated a structural model examining causal relations among the three latent constructs. The model included a saturated set of immediate lagged effects (from T1 to T2 and from T2 and T3) among marital conflict, depressive symptoms, functional impairment, and income, which was also measured at each time point. Eight T1 exogenous latent factors (i.e., age, gender, race/ethnicity, education, income, marital conflict, depressive symptoms, functional impairment) were posited to correlate with one another. Measured only at T1, the four exogenous factors of age, gender, race/ethnicity, and education were allowed to have lagged effects on marital conflict, depressive symptoms, functional impairment, and income measured at T2 and T3. We included income as a time-varying covariate because income fluctuated significantly over time. Structural equation errors within T2 and T3 were posited to correlate with one another.
Note that we did not specify contemporaneous (instantaneous) reciprocal causal effects within T2 and T3 among marital conflict, depressive symptoms, and functional impairment. Positing contemporaneous reciprocal causal effects requires certain assumptions about causal relations. For instance, cross-lagged panel models typically impose equality constraints for stability effects (Kessler & Greenberg, 1981). Because most panel models are evaluated using data with equal time spacing between waves, equality constraints on stability coefficients are justified. The NSFH has a considerable difference in time intervals between waves (i.e., 5 years between T1 and T2 and 10 years between T2 and T3), which prevented us from estimating both contemporaneous and lagged associations by placing equality constraints on stability coefficients. Our model provided a good fit to the data (χ2 = 1,569.79, df = 501, BIC = −2194.3). Table 4 presents unstandardized and standardized parameter estimates. Figure 1 highlights significant paths of interest and provides standardized parameter estimates for those paths.
Table 4.
Parameter Estimates and Standard Errors for the Structural Model of Marital Conflict, Depressive Symptoms, and Functional Impairment (N = 1,832)
| Independent Variables | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent Variables | Female | Age | Non-White | Education | T1 MC | T1 Dep | T1 FI | T1 Inc | T2 MC | T2 Dep | T2 FI | T2 Inc |
| A. Unstandardized coefficients | ||||||||||||
| T2 marital conflict (T2 MC) | −0.06* (0.02) | −0.15* (0.04) | 0.02 (0.03) | 0.09 (0.04) | 0.57* (0.05) | 0.16* (0.03) | 0.00 (0.03) | −0.07* (0.02) | ||||
| T2 depressive symptoms (T2 Dep) | 0.07* (0.02) | −0.06 (0.03) | 0.03 (0.03) | 0.03 (0.03) | 0.01 (0.05) | 0.56* (0.04) | 0.03 (0.04) | −0.04 (0.02) | ||||
| T2 functional impairment (T2 FI) | 0.11 (0.04) | 0.25 (0.09) | −0.11 (0.05) | −0.31* (0.08) | 0.30* (0.09) | −0.05 (0.06) | 0.64* (0.05) | 0.02 (0.04) | ||||
| T2 income (T2 Inc) | −0.09* (0.02) | 0.54* (0.18) | −0.02 (0.03) | −0.28 (0.13) | 0.45* (0.12) | −0.06 (0.04) | −0.24* (0.05) | 0.55* (0.05) | ||||
| T3 marital conflict (T3 MC) | 0.01 (0.02) | −0.12* (0.03) | 0.07* (0.02) | 0.12* (0.03) | 0.71* (0.04) | −0.01 (0.02) | 0.07 (0.03) | 0.06* (0.02) | ||||
| T3 depressive symptoms (T3Dep) | 0.11* (0.02) | 0.01 (0.02) | 0.08 (0.03) | 0.02 (0.02) | 0.30* (0.04) | 0.40* (0.03) | 0.14* (0.03) | 0.03* (0.01) | ||||
| T3 functional impairment (T3 FI) | 0.07 (0.03) | 0.12* (0.04) | 0.06 (0.03) | −0.07 (0.04) | 0.00 (0.05) | −0.02 (0.03) | 0.77* (0.04) | −0.01 (0.02) | ||||
| T3 income (T3 Inc) | −0.09* (0.02) | −0.65* (0.09) | −0.07* (0.02) | 0.44* (0.09) | −0.31* (0.07) | −0.01 (0.02) | 0.19* (0.05) | 0.48* (0.09) | ||||
| B. Standardized coefficients | ||||||||||||
| T2 MC | −0.09 | −0.21 | 0.03 | 0.13 | 0.57 | 0.20 | −0.01 | −0.09 | ||||
| T2 Dep | 0.08 | −0.07 | 0.03 | 0.04 | 0.01 | 0.56 | 0.03 | −0.05 | ||||
| T2 FI | 0.11 | 0.26 | −0.11 | −0.32 | 0.22 | −0.04 | 0.67 | 0.02 | ||||
| T2 Inc | −0.09 | 0.54 | −0.02 | −0.28 | 0.32 | −0.05 | −0.24 | 0.55 | ||||
| T3 MC | 0.01 | −0.17 | 0.10 | 0.17 | 0.70 | −0.01 | 0.10 | 0.08 | ||||
| T3 Dep | 0.12 | 0.01 | 0.09 | 0.03 | 0.24 | 0.40 | 0.15 | 0.03 | ||||
| T3 FI | 0.07 | 0.12 | 0.06 | −0.07 | 0.00 | −0.02 | 0.74 | −0.01 | ||||
| T3 Inc | −0.09 | −0.65 | −0.07 | 0.44 | −0.22 | −0.01 | 0.18 | 0.48 | ||||
Note: Numbers in parentheses are standard errors
Significant path (i.e., t values ≥ 3).
Does Marital Conflict Predict Changes in Depressive Symptoms and Functional Impairment?
Congruent with previous research findings (Beach et al., 2003; Whisman & Bruce, 1999; Williams, 2003), marital conflict predicted increases in depressive symptoms (Figure 1). This relationship emerged only between T2 and T3, however, a 10-year lag. Reverse causality appeared between the first two waves, a 5-year lag, where depressive symptoms predicted increases in marital conflict. Note that the link between depressive symptoms and marital conflict was characterized by a positive feedback loop. That is, depressive symptoms led to more marital conflict, which, in turn, led to more depressive symptoms over time.
The pattern of causal association between marital conflict and functional impairment also was time specific. Consistent with previous cross-sectional research (Bookwala, 2005), marital conflict was associated with an increase in functional impairment, but only over the first 5 years (T1 to T2). Marital conflict was not associated with changes in functional impairment over the next 10 years (T2 to T3). Unlike findings from previous research (Booth & Johnson, 1994), functional impairment did not predict changes in marital conflict across either time interval.
Does Marital Conflict Indirectly Lead to an Increase in Functional Impairment via Depressive Symptoms?
Our results did not provide evidence that marital conflict indirectly affects functional impairment through depressive symptoms. As illustrated in Figure 1, depressive symptoms were not predictive of changes in functional impairment across either time interval. This result is incongruent with previous research (e.g., Aneshensel et al, 1984) that has indicated bidirectional influences between depressive symptoms and functional impairment.
Does Marital Conflict Indirectly Lead to an Increase in Depressive Symptoms via Functional Impairment?
Marital conflict at T1 was found to exacerbate functional impairment between T1 and T2, and the increase in functional impairment at T2 in turn aggravated depressive symptoms between T2 and T3. According to the standardized path coefficients (Table 4), three quarters of the total effect [(.57 × .24) + (.01 × .40) + (.22 × .15) + (.32 × .03)] of marital conflict on depressive symptoms was explained by its direct effect (.57 × .24). Additionally, about one fifth of its total effect was accounted for by the indirect effect of marital conflict on depressive symptoms through functional impairment (.22 × .15). The size of the indirect effect should be interpreted with caution, however, because it varies as a function of the temporal positioning of T2 between T1 and T3 (Gollob & Reichardt, 1991).
DISCUSSION
Guided by a general stress process perspective, we evaluated whether the major social role strain of higher marital conflict might lead to greater declines in physical and mental health over time. Most research has emphasized only the positive health consequences of being married, both psychological and physical (see Waite & Gallagher, 2000, for a review); yet evaluating how a distressed marriage may lead to negative health outcomes is critical to providing a more complete understanding of the marriage-health link. Our longitudinal design with three waves of data from a representative sample of U.S. adults allowed us to extend work in this area by evaluating reciprocal patterns of influences among marital conflict, depressive symptoms, and functional limitations.
Congruent with existing studies (see Bruce, 2000; Whisman, 2001, for reviews), our findings suggest that greater marital conflict directly increases depressive symptoms and functional health limitations, although the results were not replicated consistently across both time lags. We found that marital conflict predicted increases in depressive symptoms only over the second 10-year lag. In contrast, persons who reported higher levels of marital conflict indicated greater increases in functional impairment only during the first 5-year interval. Although it is challenging to interpret these inconsistent results, Umberson and colleagues (2006) speculated that the association between marital quality and health might partly depend on age. We suspect that marital quality might have more significant implications on physical health at younger ages through its effect on health behaviors and social control, whereas mental health might be more vulnerable to lower marital quality at older ages. Although our design globally controls for age, our longitudinal analyses of relatively long-term marriages may still be capturing evidence of relative age differences among respondents across the two time intervals of the NSFH.
With regard to the indirect effect of marital disagreement on functional limitations, we found no evidence that marital conflict leads to increases in functional impairment via increases in depressive symptoms. This result is puzzling, given the bidirectional association between depressive symptoms and functional impairment consistently demonstrated in previous studies (e.g., Aneshensel et al., 1984). We suspect that depressive symptoms might have been confounded with marital conflict among the married in previous studies. With the effects of both marital conflict and depressive symptoms on functional impairment estimated simultaneously, our study allowed evidence to emerge that marital conflict explains a greater portion of the variance in functional impairment than depressive symptoms.
Importantly, greater marital conflict indirectly led to increases in depressive symptoms via increases in functional impairment. Our finding suggests that persons in low-quality marriage might suffer physical health deterioration before experiencing a significant rise in negative affect. Therefore, developing strategies addressed at alleviating the negative effect of marital disagreements on functional health might be an effective way to moderate the deleterious effect of marital conflict on depressive symptomatology.
Study Limitations
We caution readers that the estimated causal relationships in our study might be biased to some extent. First, we were not able to control for medical illnesses that might cause both depressive symptomatology and functional limitations. Furthermore, our measures may not be optimal in differentiating mental and physical health. We included only negative affect items of the CES-D in our measure of depressive symptoms to attempt to avoid confounding depressive symptoms and functional impairment. Overcontrolling is also a possibility in this case. For example, some depressed individuals might experience only somatic symptomatology that is not linked to their functional health status. For these individuals, our assessment of depressive symptoms would have underestimated their mental health challenges.
Data limitations also hampered our ability to credibly investigate a positive aspect of marital quality. A growing literature has suggested that marital relationships consist of both positive and negative dimensions that might be independent predictors of health (Kiecolt-Glaser & Newton, 2001). Evidence from both laboratory-based and survey research, however, suggests that negative marital quality might be particularly detrimental to health (Bookwala, 2005; Kiecolt-Glaser & Newton; Umberson et al., 2006).
Importantly, our sample selection criteria might have introduced selection bias to some unknown degree (Berk, 1983). We examined NSFH respondents who were aged 30 and older and continuously married to the same spouse at least for 15 years across three waves of data collection. First, controlling for age, gender, race/ethnicity, education, and income, we found that respondents who indicated higher marital conflict and depressive symptoms at either T1 or T2 were more likely to be eliminated from the analytic sample by T2 or T3 because of separation or divorce. In addition, persons who indicated higher levels of marital conflict and depressive symptoms at T1 were more likely to become widowed, thus being excluded from the sample at T2. Depressive symptoms at T2 also predicted exclusion because of widowhood at T3. Higher levels of functional impairment at T1 or T2, however, did not predict separation, divorce, or widowhood at subsequent waves.
Second, to evaluate potential additional attrition bias, we also examined whether individuals with higher levels of marital conflict, depressive symptoms, and functional impairment were more likely to leave the sample through total non-response at subsequent waves. Controlling for age, gender, race/ethnicity, education, and income, neither marital conflict nor depressive symptoms predicted NSFH nonrespondents at T2 or T3 in contrast to individuals who remained respondents to the survey. Yet respondents who reported more difficulty in doing day-to-day activities (i.e., had more functional impairment) in a prior survey wave (i.e., T1 or T2) were more likely to have become nonrespondents at a subsequent survey wave (i.e., at T2 or T3). Therefore, our selection criteria did nonrandomly eliminate persons with more marital conflict, depressive symptoms, and functional limitations at T1 and T2, which might have biased our estimates.
Despite these limitations, our results suggest that conflict in marriage should be further studied as a public health concern. When marital conflict undermines physical health, it has multiple ramifications over time in terms of additional further declines in mental and physical health. Health prevention and intervention programs would do well to incorporate components to address the potential negative effects of marital conflict on physical health for married persons, given that some degree of conflict is inevitable in marital relationships.
Acknowledgments
NOTE
This research was supported by the National Institute on Aging (AG206983 and AG20166). We are also grateful to Dr. Robert M. Hauser for his astute statistical guidance during the development of this study.
Contributor Information
Heejeong Choi, Consumer Studies, Ewha Womans University, 11-1 Daehyun Dong, Seodaemun Gu, Seoul, 120–750, Korea (p.elphaba@gmail.com).
Nadine F. Marks, Human Development & Family Studies, University of Wisconsin – Madison, 1430 Linden Drive, Madison WI 53705.
REFERENCES
- Allison PD. Missing data. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- Aneshensel CS, Frerichs RR, Huba GJ. Depression and physical illness: A multi-wave, nonrecursive model. Journal of Health and Social Behavior. 1984;25:350–371. [PubMed] [Google Scholar]
- Beach SRH, Katz I, Kim S, Brody GH. Prospective effects of marital satisfaction on depressive symptoms in established marriages: A dyadic model. Journal of Social and Personal Relationships. 2003;20:355–371. [Google Scholar]
- Berk RA. An introduction to sample selection bias in sociological data. American Sociological Review. 1983;48:386–398. [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley: 1989. [Google Scholar]
- Bookwala J. The role of marital quality in physical health during the mature years. Journal of Aging and Health. 2005;17:85–104. doi: 10.1177/0898264304272794. [DOI] [PubMed] [Google Scholar]
- Booth A, Johnson DR. Declining health and marital quality. Journal of Marriage and the Family. 1994;56:218–223. [Google Scholar]
- Broman CL. Race differences in marital well-being. Journal of Marriage and the Family. 1993;55:724–732. [Google Scholar]
- Bruce ML. In: Physical illness and depression in older adults: A handbook of theory, research, and practice. Williams GM, Shaffer DR, Parmelee PA, editors. New York: Kluwer Academic; 2000. pp. 11–29. [Google Scholar]
- Burman B, Margolin G. Analysis of the association between marital relationships and health problems: An interactional perspective. Psychological Bulletin. 1992;112:39–63. doi: 10.1037/0033-2909.112.1.39. [DOI] [PubMed] [Google Scholar]
- Cassel J. The contribution of the social environment to host resistance. American Journal of Epidemiology. 1976;104:107–123. doi: 10.1093/oxfordjournals.aje.a112281. [DOI] [PubMed] [Google Scholar]
- Erel O, Burman B. Interrelatedness of marital relations and parent-child relations: A meta-analytic review. Psychological Bulletin. 1995;118:108–132. doi: 10.1037/0033-2909.118.1.108. [DOI] [PubMed] [Google Scholar]
- Fincham FD, Beach SRH, Harold GT, Osborne LN. Marital satisfaction and depression: Different causal relationships for men and women? Psychological Science. 1997;8:351–357. [Google Scholar]
- George LK, Lynch SM. Race differences in depressive symptoms: A dynamic perspective on stress exposure and vulnerability. Journal of Health and Social Behavior. 2003;44:353–369. [PubMed] [Google Scholar]
- Goldman N. Marriage selection and mortality patterns: Inferences and fallacies. Demography. 1993;30:189–208. [PubMed] [Google Scholar]
- Gollob HF, Reichartdt CS. Interpreting and estimating indirect effects assuming time lags really matter. In: Collins LM, Horn JL, editors. Best methods for the analysis of change: Recent advances, unanswered questions, future directions. Washington, DC: American Psychological Association; 1991. pp. 243–259. [Google Scholar]
- Gove WR. Sex, marital status, and mortality. American Journal of Sociology. 1973;79:45–67. doi: 10.1086/225505. [DOI] [PubMed] [Google Scholar]
- Grayson DA, Mackinnon A, Jorm AF, Creasey H, Broe GA. Item bias in the Center for Epidemiologic Studies Depression scale: Effects of physical disorders and disability in an elderly community sample. Journal of Gerontology: Psychological Sciences. 2000;55B:P273–P282. doi: 10.1093/geronb/55.5.p273. [DOI] [PubMed] [Google Scholar]
- Hawkins DN, Booth A. Unhappily ever after: Effects of long-term, low-quality marriages on well-being. Social Forces. 2005;84:445–465. [Google Scholar]
- House JS, Kessler RC, Herzog AR. Age, socioeconomic status, and health. Milbank Quarterly. 1990;68:383–411. [PubMed] [Google Scholar]
- Jöreskog K. [Retrieved May 23, 2005];Structural equation modeling with ordinal variables using LISREL. 2002 from http://www.ssicentral.com/lisrel/techdocs/ordinal.pdf.
- Jöreskog K, Sörbom D. LISREL 8: User’s reference guide. Chicago: Scientific Software International; 1996. [Google Scholar]
- Karney BR, Bradbury TN. The longitudinal course of marital quality and stability: A review of theory, method, and research. Psychological Bulletin. 1995;118:3–34. doi: 10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Greenberg DF. Linear panel analysis: Models of quantitative change. New York: Academic Press; 1981. [Google Scholar]
- Kessler RC, McLeod JD. Sex differences in vulnerability to undesirable life events. American Sociological Review. 1984;49:620–631. [Google Scholar]
- Kiecolt-Glaser JK, Loving TJ, Stowell JR, Malarkey WB, Lemeshow S, Dickinson SL, et al. Hostile marital interactions, proinflammatory cytokine production, and wound healing. Archives of General Psychiatry. 2005;62:1377–1384. doi: 10.1001/archpsyc.62.12.1377. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;727:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kurdek LA. The nature and predictors of the trajectory of change in marital quality over the first 4 years of marriage for first-married husbands and wives. Journal of Family Psychology. 1998;12:494–510. doi: 10.1037//0012-1649.35.5.1283. [DOI] [PubMed] [Google Scholar]
- Lillard LA, Waite LJ. Til death do us part: Marital disruption and mortality. American Journal of Sociology. 1995;100:1131–1156. [Google Scholar]
- McEwen BS. Protective and damaging effects of stress mediators. New England Journal of Medicine. 1998;338:171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- Merrill SS, Seeman TE, Kasl SV. Gender differences in the comparison of self-reported disability and performance measures. Journals of Gerontology: Biological Medical Sciences. 1997;52A:M19–M26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- Mirowsky J, Ross CE. Age and depression. Journal of Health and Social Behavior. 1992;33:187–205. [PubMed] [Google Scholar]
- Ormel J, Rijsdijk FV, Sullivan M, van Sonderen E, Kempen GIJM. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. Journal of Gerontology: Psychological Sciences. 2002;57B:338–347. doi: 10.1093/geronb/57.4.p338. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Raftery AE. Bayesian model selection in social research. Sociological Methodology. 1995;25:111–163. [Google Scholar]
- Robles TF, Kiecolt-Glaser JK. The physiology of marriage: Pathways to health. Physiology & Behavior. 2003;79:409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Rogers SJ, May DC. Spillover between marital quality and job satisfaction: long-term patterns and gender differences. Journal of Marriage and Family. 2003;65:482–495. [Google Scholar]
- Ross CE, Mirowsky J, Goldsteen K. The impact of the family on health: The decade in review. Journal of Marriage and the Family. 1990;52:1059–1078. [Google Scholar]
- Ross CE, Wu C. The links between education and health. American Sociological Review. 1995;60:719–745. [Google Scholar]
- Stansfeld S, Marmot MG. Social class and minor psychiatric disorder in British civil servants: A validated screening survey using the general health questionnaire. Psychological Medicine. 1992;22:739–749. doi: 10.1017/s0033291700038186. [DOI] [PubMed] [Google Scholar]
- Umberson D. Family status and health behaviors: Social control as a dimension of social integration. Journal of Health and Social Behavior. 1987;28:306–319. [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: Marital quality and health over the life course. Journal of Health and Social Behavior. 2006;47:1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanLaningham J, Johnson DR, Amato P. Marital happiness, marital duration, and the U-shaped curve: Evidence from a five-wave panel study. Social Forces. 2001;79:1313–1341. [Google Scholar]
- Waite L, Gallagher M. The case for marriage: Why married people are happier, healthier, and better off financially. New York: Broadway Books; 2000. [Google Scholar]
- Whisman MA. The association between depression and marital dissatisfaction. In: Beach SRH, editor. Marital and family processes in depression: A scientific foundation for clinical practice. Washington, DC: American Psychological Association; 2001. pp. 3–24. [Google Scholar]
- Whisman MA, Bruce ML. Marital dissatisfaction and incidence of major depressive episode in a community sample. Journal of Abnormal Psychology. 1999;108:674–678. doi: 10.1037//0021-843x.108.4.674. [DOI] [PubMed] [Google Scholar]
- Williams DR, Collins C. U.S. socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Williams K. Has the future of marriage arrived? A contemporary examination of gender, marriage, and psychological well-being. Journal of Health and Social Behavior. 2003;44:470–487. [PMC free article] [PubMed] [Google Scholar]