Abstract
Ebola virus causes hemorrhagic fever in humans and nonhuman primates, resulting in mortality rates of up to 90%. Studies of this virus have been hampered by its extraordinary pathogenicity, which requires biosafety level 4 containment. To circumvent this problem, we developed a novel complementation system for functional analysis of Ebola virus glycoproteins. It relies on a recombinant vesicular stomatitis virus (VSV) that contains the green fluorescent protein gene instead of the receptor-binding G protein gene (VSVΔG*). Herein we show that Ebola Reston virus glycoprotein (ResGP) is efficiently incorporated into VSV particles. This recombinant VSV with integrated ResGP (VSVΔG*-ResGP) infected primate cells more efficiently than any of the other mammalian or avian cells examined, in a manner consistent with the host range tropism of Ebola virus, whereas VSVΔG* complemented with VSV G protein (VSVΔG*-G) efficiently infected the majority of the cells tested. We also tested the utility of this system for investigating the cellular receptors for Ebola virus. Chemical modification of cells to alter their surface proteins markedly reduced their susceptibility to VSVΔG*-ResGP but not to VSVΔG*-G. These findings suggest that cell surface glycoproteins with N-linked oligosaccharide chains contribute to the entry of Ebola viruses, presumably acting as a specific receptor and/or cofactor for virus entry. Thus, our VSV system should be useful for investigating the functions of glycoproteins from highly pathogenic viruses or those incapable of being cultured in vitro.
The family Filoviridae contains Marburg and Ebola viruses, which are filamentous, enveloped, and nonsegmented negative-stranded RNA viruses (1, 2). Both viruses cause severe hemorrhagic disease in humans and nonhuman primates with high mortality rates (1, 2). The Ebola virus group consists of the Zaire and Sudan subtypes, first identified in 1976; Reston, initially isolated from cynomolgus monkeys imported from the Philippines into the United States in 1989; and a strain discovered in the Tai Forest of the Ivory Coast in 1994. The natural reservoir of filoviruses remains elusive.
The filoviruses contain at least seven structural proteins, all of which are translated from monocistronic polyadenylylated mRNA transcripts (2–7). The surface glycoprotein (GP) is expressed from the fourth of the seven structural protein genes (3, 6). Because filoviruses contain a single transmembrane GP that forms spikes on the virion surface, the GP is most likely to be responsible for receptor binding and membrane fusion, leading to virus penetration. Filovirus GP is a type I glycoprotein, containing both N-linked and O-linked carbohydrates (2, 8, 9), which contribute to considerably larger molecular weights than those predicted from deduced amino acid sequences. However, little is known about the biological functions of GP and the other filovirus proteins. Attempts to analyze the structure and biological behavior of the filoviruses have been impeded by the need for biosafety level 4 containment, leading to keen interest in strategies that might circumvent this obstacle.
Vesicular stomatitis virus (VSV), the prototype rhabdovirus, has been used as a model system for studying the replication and assembly of enveloped RNA viruses. It grows in many animal and some insect cells and can be propagated in large quantities. Lawson et al. (10) and Whelan et al. (11) generated recombinant VSV from plasmids, raising the possibility of its use as a vector to express foreign proteins (12). More recently, Schnell et al. (13) reported the incorporation of foreign glycoproteins (i.e., cellular CD4 or measles virus glycoproteins) into VSV particles. In the present study, we generated a recombinant VSV that contains the green fluorescent protein (GFP) gene, instead of the G protein gene, and thus is not infectious unless the envelope protein responsible for receptor binding and membrane fusion is provided in trans. We then investigated the potential utility of this novel recombinant VSV in functional analysis of the Ebola virus GP. Herein we report successful complementation of the recombinant VSV with the Ebola Reston GP.
MATERIALS AND METHODS
Plasmids.
Full-length cDNAs encoding the Ebola Reston virus glycoprotein (ResGP) (14), VSV G protein (15), and influenza A/turkey/Ireland/1378/83 (H5N8) virus hemagglutinin (16) were cloned into a mammalian expression vector, pCAGGS (17), and designated pCResGP, pCVSVG, and pCTH, respectively.
Cells.
Vero, BHK, MDCK, and MDBK cells were grown in Eagle’s MEM supplemented with 10% fetal calf serum (FCS), l-glutamine (GIBCO/BRL), vitamin and amino acid solutions (GIBCO/BRL), and penicillin-streptomycin solution (Sigma). For L cells, horse serum was used instead of FCS. 293T, COS-1, NIH 3T3, and Tb1Lu cells were cultured in high glucose DMEM containing 10% FCS, l-glutamine, and antibiotics. Chinese hamster ovary clone 22 cells, provided by E. Ruley (Vanderbilt University) were cultured in Ham’s F-12 medium containing 5% FCS, l-glutamine, and antibiotics. DBT cells, a murine astrocytoma cell line, provided by S. Makino (University of Texas), were grown in MEM supplemented with 10% newborn calf serum, tryptose phosphate broth (GIBCO/BRL), and antibiotics. Clone C6/36 cells from a mosquito larvae cell line were grown in MEM supplemented with Earle’s balanced salt solution and 10% FCS.
Generation of Recombinant VSV.
The coding region of the G protein gene in a full-length cDNA clone of the VSV genome (Indiana serotype) (10) was replaced with the coding region of a modified version of the GFP gene (18) in which Ser-65 was replaced with Thr. This plasmid was designated pVSV-ΔG*. BHK cells in 60-mm dishes were infected at a multiplicity of 10 with the recombinant vaccinia virus vTF7–3 (19), which encodes bacteriophage T7 RNA polymerase, for 1 hr at 37°C. The infected cells were then cotransfected with pVSV-ΔG*, the VSV nucleocapsid protein-, phosphoprotein-, polymerase protein-, and glycoprotein-expressing plasmids at weight ratios of 10, 3, 5, 1, and 3 μg, respectively, as indicated (20). The supernatant fluid was harvested 48 hr after transfection, and one-half of the supernatant fluid was used to infect a second plate of cells that had been infected with vTF7–3 and transfected with 5 μg of plasmid encoding the G protein only. Cells were examined for GFP expression 24 hr after infection by fluorescence microscopy. The presence of fluorescent cells indicated that VSV genome had been successfully recovered. Additional passages of supernatant containing VSVΔG* complemented with G protein (VSVΔG*-G) through cells expressing G protein from plasmid DNA in the presence of 25 μg of cytosine β-d-arabinofuranoside per ml were performed to obtain high-titer stocks of VSVΔG*-G. For the experiments described below, a supernatant containing approximately 109 infectious units of VSVΔG*-G was filtered through a membrane with a 0.2-μm pore size to remove vaccinia virus. Virus titer in the supernatant fluid was then determined again by infecting BHK cells and quantifying the number of cells expressing GFP by fluorescence microscopy.
Preparation of VSVΔG* Complemented with VSV G or ResGP or Without Complementation.
293T cells were transfected with pCVSVG, pCResGP, or pCAGGS by using Lipofectamine (GIBCO/BRL). Thirty-six hours after transfection, cells were infected with VSVΔG*-G at a multiplicity of infection of 1 for 1 hr at 37°C. They were then washed with PBS three times, and medium was added. After 24 hr of incubation at 37°C in a CO2 incubator, culture fluid was collected and centrifuged to remove cells. Each virus stock was stored at −80°C until used.
Titration of Recombinant VSVs Complemented with Receptor-Binding Proteins in Different Cell Lines.
The cell monolayers were grown on coverslips, washed with PBS, and then infected with serially diluted virus stocks. After 1 hr of adsorption at 37°C, inoculum was aspirated, and growth medium was added. The cells were incubated at 37°C for 12–14 hr in a CO2 incubator, washed with PBS, and fixed with 10% formalin in PBS. Infectious units of virus in different cell lines were determined by counting the number of GFP-expressing cells.
Chemical Modification of Cells.
Vero cells were preincubated in the presence of tunicamycin (Sigma) at 37°C for 8 hr in a CO2 incubator and then infected with viruses for 1 hr. After aspiration of the inoculum and addition of growth medium, the cells were incubated for 12 hr, and infected cells were counted. For treatment with proteases, neuraminidase, or sodium periodate (NaIO4), the cells were washed with PBS three times and incubated in the presence of Pronase (Calbiochem), trypsin (GIBCO/BRL), Vibrio cholerae neuraminidase (GIBCO/BRL), or NaIO4 (Fisher) in serum-free medium at 37°C in a CO2 incubator for 20 min (protease) or 1 hr (neuraminidase and NaIO4). To stop the reaction, we added an equal volume of complete medium to each well and the cells were washed with PBS. Subsequently, the cells were infected with viruses, and the infected cells were counted. Vero cells were also preincubated in the presence of ammonium chloride (Sigma) at 37°C for 2 hr in a CO2 incubator. They were then infected with viruses and incubated in the presence of ammonium chloride.
RESULTS
To investigate the functions of the Ebola Reston virus GP, we first expressed it by transfection with a plasmid vector, pCAGGS, that contains a chicken β-actin promoter. Two molecular mass species (130 and 160 kDa), both reactive with a mAb to ResGP (14), were detected by radioimmunoprecipitation (Fig. 1). The GP was efficiently transported to the cell surface, as indicated by flow cytometry analysis (data not shown). We next examined whether the expressed GP induces polykaryon formation at neutral pH or upon exposure to low pH, as described for the influenza virus hemagglutinin (16). ResGP did not induce polykaryon formation at neutral pH or upon exposure to low pH, even under conditions that lead to polykaryon formation of cells expressing influenza virus hemagglutinin or VSV G protein (data not shown). We therefore sought an alternative approach to the investigation of Ebola virus GP function.
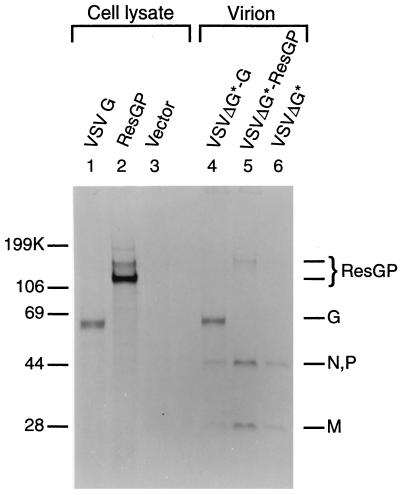
Figure 1.
Incorporation of ResGP into VSV particles. Viral proteins were analyzed by SDS/PAGE in 10% gels under reducing conditions. 293T cells transfected with an expression vector plasmid containing the VSV G gene (lane 1), the ResGP gene (lane 2), or the vector plasmid only (lane 3) were labeled for 5 hr with [35S]methionine 30 hr after transfection. Proteins in cell lysates were precipitated by a mAb to VSV G protein (lane 1) or ResGP (lanes 2 and 3). Recombinant VSVs, including VSVΔG* complemented with VSV G protein (lane 4, VSVΔG*-G) or with ResGP (lane 5, VSVΔG*-ResGP) or lacking complementation (lane 6, VSVΔG*), were labeled with [35S]methionine and purified by differential centrifugation and sedimentation through 25–45% sucrose gradients.
Incorporation of ResGP into VSV Particles.
By using reverse genetics, we generated VSV containing the GFP gene instead of the G protein gene (VSVΔG*). The infectivity of VSVΔG* can be rescued by providing G protein in trans (VSVΔG*-G). To determine whether ResGP would complement infectivity of this recombinant VSV, we first tested whether it was incorporated into the VSV particle. 293T cells transfected with pCVSVG, pCResGP, or pCAGGS were infected with VSVΔG*-G and labeled with [35S]methionine. Purified virions from the culture fluid of pCVSVG-transfected cells contained all of the VSV structural proteins (Fig. 1, lane 4), with the exception of L protein, which was detected only after longer exposures (data not shown). Although two proteins with approximate molecular masses of 130 and 160 kDa were immunoprecipitated with anti-ResGP mAb from the lysates of cells transfected with pCResGP (lane 2), virions from the culture fluid of these cells (VSVΔG*-ResGP) contained only the 160-kDa protein (lane 5). The smaller protein detected in the cell lysate was likely an immature form of GP. The virions from vector-transfected cells (VSVΔG*) contained only internal proteins (N, P, and M, lane 6).
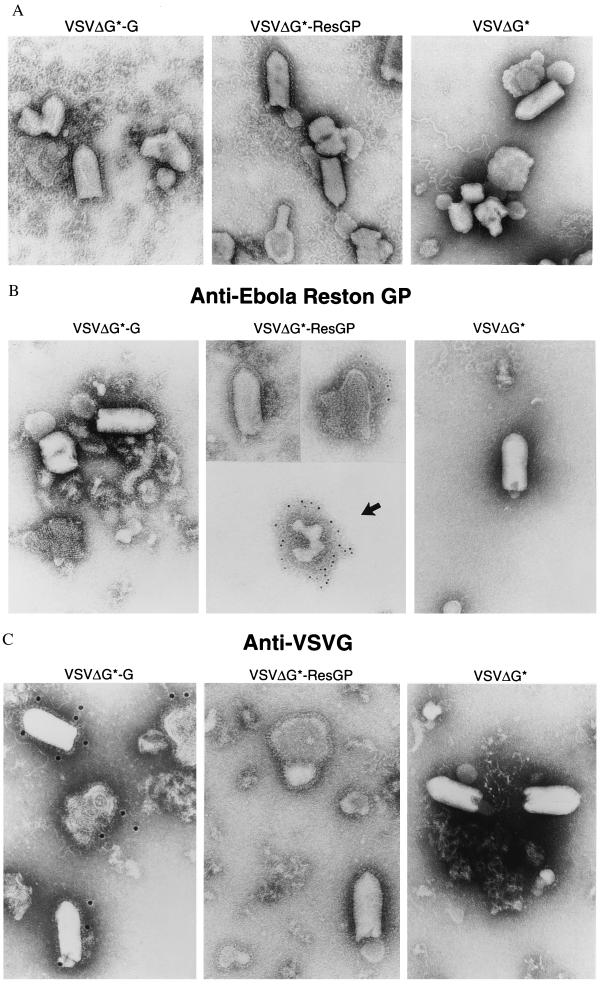
Electron microscopy of partially purified virions revealed densely arrayed spikes on the envelopes of both VSVΔG*-ResGP and VSVΔG*-G virions, but VSVΔG* virions were spikeless (Fig. 2A). Immunogold staining showed that a monoclonal antibody to ResGP bound to partially disrupted VSVΔG*-ResGP virions (Fig. 2B Middle, at the upper right) but not to intact particles (Fig. 2B Middle, at the upper left), suggesting that the antibody lacks access to the determinant on GP molecules that are tightly packaged into virions. Indeed, the same mAb does not neutralize Ebola Reston virus (A.S., unpublished data). Membrane vesicles copurified with virions (Fig. 2B Middle, at the lower middle with an arrow) contained spikes that were also decorated with the mAb. By contrast, a neutralizing mAb I1 (21) to VSV G protein recognized morphologically intact VSV particles containing the G protein, as well as disrupted ones, but not VSVΔG*-ResGP and VSVΔG*-G (Fig. 2C).
Figure 2.
Electron microscopy of recombinant VSV particles. VSVΔG* complemented with VSV G protein (VSVΔG*-G) or with ResGP (VSVΔG*-ResGP) or without complementation (VSVΔG*) was prepared and partially purified by centrifugation through 20% sucrose. Viruses were negatively stained (A) or labeled with a mouse mAb to ResGP (B) or VSV G protein (C) and anti-mouse IgG conjugated with colloidal gold, followed by negative staining.
Complementation of Recombinant VSV Infectivity by ResGP.
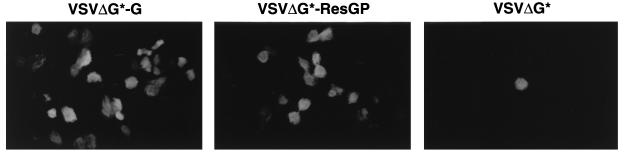
To test whether ResGP can rescue the infectivity of VSV lacking any receptor binding/fusion protein, we infected Vero cells with VSVΔG*-G, VSVΔG*-ResGP, or VSVΔG*. A large number of cells expressed GFP when infected with VSVΔG*-ResGP or VSVΔG*-G, but few cells expressed GFP when infected with VSVΔG* (Fig. 3). The background infectivity of VSVΔG* (as shown in Table 1) was attributed to the inoculum of VSVΔG*-G, because it was neutralized by an antiserum to VSV (data not shown). These findings indicate that Ebola virus GP itself is sufficient for attachment and penetration of the virus into Vero cells.
Figure 3.
Expression of GFP upon infection with recombinant VSVs. Vero cells were infected with VSVΔG*-G, VSVΔG*-ResGP, or VSVΔG*, and GFP expression was examined 12 hr after infection by fluorescence microscopy.
Table 1.
Infectivities of recombinant VSVs for different cell lines
| Cell line (species) | Infectious unit(s), log10/0.1 ml
|
||
|---|---|---|---|
| VSVΔG*-G | VSVΔG*-ResGP | VSVΔG* | |
| Vero (monkey) | 6.7 | 5.2 | 2.1 |
| COS-1 (monkey) | 6.3 | 5.1 | 2.1 |
| 293T (human) | 6.5 | 5.1 | 2.0 |
| BHK (hamster) | 6.7 | 3.4 | 2.4 |
| CHO (hamster) | 5.7 | 3.7 | 2.1 |
| L (mouse) | 6.1 | 3.6 | 1.8 |
| NIH3T3 (mouse) | 5.0 | 3.3 | 1.0 |
| DBT (mouse) | 6.6 | 3.7 | 2.5 |
| MDCK (dog) | 6.2 | 3.9 | 1.8 |
| MDBK (cow) | 5.2 | 2.6 | 0.8 |
| CEF (chicken) | 6.4 | 3.5 | 2.2 |
| Tb1Lu (bat) | 5.1 | 2.9 | 0.3 |
| C6/36 (mosquito) | 3.3 | 0.6 | 0.3 |
Cells from a given line were infected with viruses from the same batch. The data are representative results from experiments repeated with three batches of viruses. Twelve to 14 hr after infection, infectious units of virus in different cells were determined by counting the number of GFP-expressing cells.
Susceptibility of Cell Lines to Recombinant VSVs.
To test the utility of our VSV system for functional analysis of Ebola virus glycoproteins, we screened various cell lines for susceptibility to recombinant VSVs to estimate the prevalence of Ebola Reston virus receptors (Table 1). A VSVΔG*-G virus stock uniformly infected all of the mammalian and avian cells tested, regardless of their species of origin with infectivity titers (as measured by counting the number of GFP-expressing cells) ranging from 105.0 to 106.5. An insect cell line (C6/36) was less susceptible to VSVΔG*-G than were other lines. The infectivity of a VSVΔG*-ResGP virus stock, by contrast, depended greatly on the type of cell line examined. With cells originating from primates (Vero, 293T, and COS-1), infectivity titers of VSVΔG*-ResGP were 100-fold higher than those with cells from hamsters, dogs, cattle, mice, chickens, or bats. VSVΔG*-ResGP did not infect the C6/36 insect cell line. These results suggest that key determinants of Ebola virus entry into cells (e.g., specific characteristics of the receptor) differ among animal species.
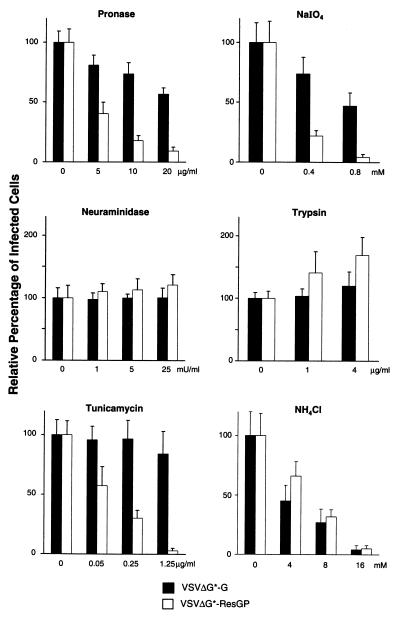
Effects of Chemical Modifications of Vero Cells on the Infectivity of Recombinant VSVs.
To obtain information on the biological characteristics of cellular receptors for Ebola Reston virus, we compared the infectivities of VSVΔG*-ResGP and VSVΔG*-G against chemically modified cells. Because the background infectivity (as described above) was considered to be negligible (0.08% of the total VSVΔG*-ResGP infectivity with Vero cells), viruses were not treated with VSV antibodies in the following experiments. We preincubated Vero cells with proteases, neuraminidase, or sodium periodate to determine the role of cell surface proteins, sialic acids, or carbohydrate, respectively, in virus infection. The treated cells were then infected with VSVΔG*-ResGP or VSVΔG*-G and diluted to yield 100–200 infected cells per microscopic field. Preincubation of cells with Pronase or sodium periodate markedly reduced the infectivity of VSVΔG*-ResGP but was less effective with VSVΔG*-G (Fig. 4). When cells were treated with Pronase at 20 μg/ml or 0.8 mM NaIO4, the infectivity of VSVΔG*-ResGP was reduced to 9.1% or 4.4%, respectively, of that with nontreated cells. Although VSVΔG*-G infectivity was also reduced to some extent under these conditions, the effect was likely indirect, reflecting excessive cell damage. Trypsin or neuraminidase treatment did not reduce the infectivity of either virus (Fig. 4). Trypsinization of cells with a higher concentration of the enzyme (16 μg/ml) caused excessive proteolysis with marked detachment and structural changes of cells. Neuraminidase treatment with 20 milliunits/ml was sufficient to abolish the susceptibility of cells to influenza virus, which recognizes sialic acids as a critical component of its receptor (data not shown). These findings suggest that VSVΔG*-ResGP interacts with glycoproteins on the cell surface but does not use sialic acid as a receptor. The role of cell surface GPs in VSVΔG*-ResGP infection was further assessed with tunicamycin, an inhibitor of N-glycosylation. As shown in Fig. 4, this agent markedly reduced the infectivity of VSVΔG*-ResGP but not that of VSVΔG*-G, indicating a major contribution by surface glycoproteins with N-linked oligosaccharide chains to VSVΔG*-ResGP infectivity.
Figure 4.
Infectivity of recombinant VSVs on chemically modified Vero cells. Vero cells were preincubated with indicated concentrations of reagents. Infectivities of VSVΔG*-G and VSVΔG*-ResGP were then examined. Each bar represents the percentage of infectious units calculated from 10 microscopic fields (mean ± SD).
Lysosomotropic agents raise the pH of the acidic compartments in cells. Ammonium chloride (NH4Cl) neutralizes the pH of endosomes, so that viruses with low pH-dependent fusion activity are incapable of fusing their envelope with endosomal membrane upon NH4Cl treatment, resulting in loss of infectivity (22). We therefore examined whether ResGP requires exposure to low pH for its ability to initiate infection. The infectivity of both VSVΔG*-ResGP and VSVΔG*-G were reduced in a dose-dependent manner, becoming completely inhibited at 16 mM NH4Cl (Fig. 4). These results suggest that both GPs require a low pH for fusion with the cellular membrane, as other VSV proteins do not require low pH exposure for the initiation of virus infection.
DISCUSSION
We have developed a VSV system that can be used to study the function of Ebola virus GPs at an early step of infection. ResGP was efficiently incorporated into VSV particles and complemented the infectivity of VSV lacking the receptor binding/fusion G protein. These findings indicate that ResGP is capable of binding to a cellular receptor and mediating membrane fusion. Because GP is the only surface glycoprotein of Ebola virus, it has been assumed, but not proven, to participate in virus binding and membrane fusion. The results presented herein substantiate this role and demonstrate how the GP can be manipulated to allow safe investigations of Ebola virus binding and fusion to the cell membrane.
One putative receptor of filoviruses is the asialoglycoprotein receptor. Found exclusively in hepatocytes (23), it recognizes GPs that have N-linked sugar chains with terminal galactose residues (24). However, because filoviruses are pantropic and cell lines lacking this receptor (e.g., human endothelial cells) are susceptible to the virus (25), other cellular receptors must exist. All of the cell lines examined in this study were susceptible to VSVΔG*-ResGP but to different degrees, raising the possibility that they harbor a common molecule that can serve as a receptor for ResGP. However, species-dependent structural differences appear to influence the interaction of ResGP with this molecule, resulting in the reduced susceptibility of nonprimate cells to VSVΔG*-ResGP.
Assays of virus infectivity to chemically modified cells suggest that certain surface GPs with N-linked oligosaccharide side chains play an important role in the cellular entry of VSVΔG*-ResGP and presumably serve as a specific cellular receptor for the virus, or perhaps a cofactor, as has been shown for HIV or herpes simplex virus, both of which require cell surface molecules besides specific receptors to mediate their entry (26, 27). Thus, we have provided direction for future research on cellular receptors and possible cofactors that affect Ebola virus entry into cells.
It is noteworthy that ResGP was efficiently packaged into VSV particles. It was reported previously that the cytoplasmic tail of the G protein of VSV was required for efficient incorporation into virions (28), but we have recently found, by using a reverse genetics approach, that the cytoplasmic tail is in fact not required for G protein incorporation (C.R. and M.A.W., unpublished data). In only one case was a non-VSV protein bearing the cytoplasmic tail of VSV G protein efficiently incorporated into VSV (29). In the present study, we showed by electron microscopy that ResGP is tightly packaged into VSV particles. Although the deduced amino acid sequence of the putative cytoplasmic domain is not significantly homologous between Ebola Reston GP and VSV G protein, the GP may contain structural features in this domain that would allow interaction of ResGP with other VSV proteins.
The complementation system we describe may permit the study of the functional domains of GP that are responsible for virus entry and thus could have considerable utility in research on membrane protein function. More importantly, it could obviate the need for in vitro cultivation and biosafety level 4 containment in studies to analyze the membrane proteins of highly pathogenic viruses and those incapable of being cultured in vitro.
Acknowledgments
We thank Beth Rodgers, Krisna Wells, and Peggy Brown for excellent technical assistance and John Gilbert for editing the manuscript. We also thank Dr. D. S. Lyles for the I1 hybridoma and Dr. M. Chalfie for the GFP cDNA. This study was supported by Public Health Service Research Grants AI33989 to Y.K. and GM53726 to M.A.W. from the National Institutes of Health, by a Cancer Center Support grant, and by the American Lebanese Syrian Associated Charities.
ABBREVIATIONS
- VSV
vesicular stomatitis virus
- GP
glycoprotein
- GFP
green fluorescent protein
- ResGP
Reston GP
- FCS
fetal calf serum
References
- 1.Peters C J, Sanchez A, Rollin P E, Ksiazek T G, Murphy F A. In: Fields Virology. Fields B N, Knipe D M, Howley P M, editors. Philadelphia: Lippincott-Raven; 1995. pp. 1161–1176. [Google Scholar]
- 2.Feldmann H, Klenk H D, Sanchez A. Arch Virol Suppl. 1993;7:81–100. doi: 10.1007/978-3-7091-9300-6_8. [DOI] [PubMed] [Google Scholar]
- 3.Feldmann H, Muhlberger E, Randolf A, Will C, Kiley M P, Sanchez A, Klenk H D. Virus Res. 1992;24:1–19. doi: 10.1016/0168-1702(92)90027-7. [DOI] [PubMed] [Google Scholar]
- 4.Kiley M P, Regnery R L, Johnson K M. J Gen Virol. 1980;49:333–341. doi: 10.1099/0022-1317-49-2-333. [DOI] [PubMed] [Google Scholar]
- 5.Elliott L H, Kiley M P, McCormick J B. Virology. 1985;147:169–176. doi: 10.1016/0042-6822(85)90236-3. [DOI] [PubMed] [Google Scholar]
- 6.Sanchez A, Kiley M P, Holloway B P, Auperin D D. Virus Res. 1993;29:215–240. doi: 10.1016/0168-1702(93)90063-s. [DOI] [PubMed] [Google Scholar]
- 7.Sanchez A, Kiley M P. Virology. 1987;157:414–420. doi: 10.1016/0042-6822(87)90283-2. [DOI] [PubMed] [Google Scholar]
- 8.Feldmann H, Will C, Schikore M, Slenczka W, Klenk H D. Virology. 1991;182:353–356. doi: 10.1016/0042-6822(91)90680-A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feldmann H, Nichol S T, Klenk H D, Peters C J, Sanchez A. Virology. 1994;199:469–473. doi: 10.1006/viro.1994.1147. [DOI] [PubMed] [Google Scholar]
- 10.Lawson N D, Stillman E A, Whitt M A, Rose J K. Proc Natl Acad Sci USA. 1995;92:4477–4481. doi: 10.1073/pnas.92.10.4477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whelan S P, Ball L A, Barr J N, Wertz G T. Proc Natl Acad Sci USA. 1995;92:8388–8392. doi: 10.1073/pnas.92.18.8388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schnell M J, Buonocore L, Whitt M A, Rose J K. J Virol. 1996;70:2318–2323. doi: 10.1128/jvi.70.4.2318-2323.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schnell M J, Buonocore L, Kretzschmar E, Johnson E, Rose J K. Proc Natl Acad Sci USA. 1996;93:11359–11365. doi: 10.1073/pnas.93.21.11359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sanchez A, Trappier S G, Mahy B W, Peters C J, Nichol S T. Proc Natl Acad Sci USA. 1996;93:3602–3607. doi: 10.1073/pnas.93.8.3602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rose J K, Bergmann J E. Cell. 1982;30:753–762. doi: 10.1016/0092-8674(82)90280-x. [DOI] [PubMed] [Google Scholar]
- 16.Kawaoka Y, Webster R G. Proc Natl Acad Sci USA. 1988;85:324–328. doi: 10.1073/pnas.85.2.324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Niwa H, Yamamura K, Miyazaki J. Gene. 1991;108:193–200. doi: 10.1016/0378-1119(91)90434-d. [DOI] [PubMed] [Google Scholar]
- 18.Chalfie M, Tu Y, Euskirchen G, Ward W W, Prasher D C. Science. 1994;263:802–805. doi: 10.1126/science.8303295. [DOI] [PubMed] [Google Scholar]
- 19.Fuerst T R, Niles E G, Studier F W, Moss B. Proc Natl Acad Sci USA. 1986;83:8122–8126. doi: 10.1073/pnas.83.21.8122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stillman E A, Rose J K, Whitt M A. J Virol. 1995;69:2946–2953. doi: 10.1128/jvi.69.5.2946-2953.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lefrancois L, Lyles D S. Virology. 1982;121:168–174. doi: 10.1016/0042-6822(82)90126-x. [DOI] [PubMed] [Google Scholar]
- 22.Marsh M, Helenius A. Adv Virus Res. 1989;36:107–151. doi: 10.1016/S0065-3527(08)60583-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Becker S, Spiess M, Klenk H -D. J Gen Virol. 1995;76:393–399. doi: 10.1099/0022-1317-76-2-393. [DOI] [PubMed] [Google Scholar]
- 24.Spiess M. Biochemistry. 1990;29:10009–10018. doi: 10.1021/bi00495a001. [DOI] [PubMed] [Google Scholar]
- 25.Schnittler H J, Mahner F, Drenckhahn D, Klenk H-D, Feldmann H. J Clin Invest. 1993;91:1301–1309. doi: 10.1172/JCI116329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bates P. Cell. 1996;86:1–3. doi: 10.1016/s0092-8674(00)80070-7. [DOI] [PubMed] [Google Scholar]
- 27.Montgomery R I, Warner M S, Lum B J, Spear P G. Cell. 1996;87:427–436. doi: 10.1016/s0092-8674(00)81363-x. [DOI] [PubMed] [Google Scholar]
- 28.Whitt M A, Chong L, Rose J K. J Virol. 1989;63:3569–3578. doi: 10.1128/jvi.63.9.3569-3578.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Owens R J, Rose J K. J Virol. 1993;67:360–365. doi: 10.1128/jvi.67.1.360-365.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]