Abstract
The signal transduction pathway underlying the cAMP-dependent modulation of rat striatal N-methyl-d-aspartate (NMDA) responses was investigated by using the two-electrode voltage-clamp technique. In oocytes injected with rat striatal poly(A)+ mRNA, activation of cAMP-dependent protein kinase (PKA) by forskolin potentiated NMDA responses. Inhibition of protein phosphatase 1 (PP1) and/or protein phosphatase 2A (PP2A) by the specific inhibitor calyculin A occluded the PKA-mediated potentiation of striatal NMDA responses, suggesting that the PKA effect was mediated by inhibition of a protein phosphatase. Coinjection of oocytes with striatal mRNA and antisense oligodeoxynucleotides directed against the protein phosphatase inhibitor DARPP-32 dramatically reduced the PKA enhancement of NMDA responses. NMDA responses recorded from oocytes injected with rat hippocampal poly(A)+ mRNA were not affected by stimulation of PKA. When oocytes were coinjected with rat hippocampal poly(A)+ mRNA plus complementary RNA coding for DARPP-32, NMDA responses were potentiated after stimulation of PKA. The results provide evidence that DARPP-32, which is enriched in the striatum, may participate in the signaling between the two major afferent striatal pathways, the glutamatergic and the dopaminergic projections, by the cAMP-dependent regulation of striatal NMDA currents.
Keywords: protein kinase, protein phosphatase, calyculin A, rat striatum, rat hippocampus
The striatum receives dense dopaminergic afferents from midbrain areas (1, 2) and glutamatergic projections from all areas of the cerebral cortex (3, 4) and thalamus (5). Ionotropic glutamate receptors have been traditionally classified into three families on the basis of pharmacological and electrophysiological data: N-methyl-d-aspartate (NMDA), amino-3-hydroxy-5-methyl-4-isoxazole propionate (AMPA), and kainate (KA) receptors.
In the striatum excessive activation of NMDA receptors has been associated with neurological disorders such as Huntington’s (6, 7) and Parkinson’s diseases (8).
Phosphorylation of neurotransmitter receptors plays an important role in the modulation of their function. NMDA receptors contain multiple consensus sites for phosphorylation by several protein kinases (9). Protein kinase C (PKC) and tyrosine kinases have been shown to phosphorylate NMDA receptor subunits directly (10–12). Moreover, forskolin, dopamine, and a D1 agonist increased the phosphorylation of the NMDAR1 receptor apparently through activation of cAMP-dependent protein kinase (PKA) (13). In rat neostriatal brain slices NMDA-induced excitatory synaptic transmission was potentiated by the PKA activators forskolin and SP-cAMPS (14). Furthermore, activation of D1 receptors potentiated NMDA-induced responses (15), whereas stimulation of metabotropic glutamate receptors had inhibitory effects on NMDA receptor function (16). In both cases, it was suggested that a cAMP/PKA-dependent mechanism was involved. However, it could not be concluded from those experiments whether the NMDA receptor complex and/or an additional intracellular regulatory protein was the target of PKA phosphorylation.
In the present study, we used the Xenopus oocyte expression system to further unravel the molecular mechanisms underlying the modulation of striatal NMDA receptor function by PKA. In initial experiments, we recorded NMDA-induced currents from Xenopus oocytes expressing NR1b, NR1b/NR2A, NR1b/NR2B, or NR1b/NR2A/NR2B NMDA receptor subunits, the main subunits found in rat striatum (17, 18). These currents were not affected by PKA stimulation (T.B. and I.N., unpublished data) suggesting the involvement of an indirect mechanism underlying the PKA-dependent modulation of striatal NMDA receptor function.
MATERIALS AND METHODS
RNA Preparation and Expression in Xenopus Oocytes.
Total RNA was isolated from striatum and hippocampus of adult Wistar rats by extraction of fresh tissue with guanidine thiocyanate and precipitation with LiCl (19). Poly(A)+ mRNA was purified by oligo(dT)-cellulose chromatography (Pharmacia mRNA Purification Kit) and dissolved in RNase-free water at a concentration of 0.5 μg/μl.
Plasmid pET3A-DARPP-32 containing the cDNA coding for the rat Mr 32,000 dopamine and adenosine 3′,5′-monophosphate-regulated phosphoprotein (DARPP-32) was linearized by digestion with NheI and used as transcription template. In vitro transcription was carried out by T7 RNA polymerase in the presence of a cap analog. RNA transcripts were precipitated by ethanol and the precipitate was dissolved in water treated with diethyl pyrocarbonate.
Oocytes were collected from anesthetized specimens of Xenopus laevis as described (20). Follicular cell layers were removed manually after incubation for 2 h at room temperature in Ca2+-free modified Barth’s saline solution containing 2.2 mg/ml collagenase, type II. Stage V and stage VI oocytes were pressure-injected with 50 ng of poly(A)+ mRNA per oocyte. In some experiments, hippocampal poly(A)+ mRNA was coinjected with DARPP-32 cRNA (20 or 80 ng per oocyte). Oocytes were kept at 18°C in modified Barth’s solution.
RNA (Northern) Blot Analysis.
Samples were size-fractionated on 1.5% agarose-formaldehyde gels and were transferred to nylon membranes (Hybond) according to standard protocols (Amersham). The full-length cDNA encoding DARPP-32 was labeled with [α-32P]dATP by random priming using a Prime-It II-Kit (Stratagene). Blots were hybridized at 68°C for 18 h in Church buffer (21). Blots were washed in 2× SSC/1% SDS for 5 min, twice in 1× SSC/1% SDS at 65°C for 15 min, and finally twice in 0.1× SSC/1% SDS at 65°C for 15 min. They were exposed to x-ray film with an intensifying screen at −70°C.
Antisense Oligodeoxynucleotides (ODNs).
Antisense 14-mer ODNs complementary to part of the cRNA coding for the phosphoprotein DARPP-32, and random and reversed control ODNs, were synthesized by Biognostik (Goettingen, Germany). ODNs were shipped as lyophilized DNA Na salt. The lyophilized ODNs were dissolved in 1× TE buffer (10 mM Tris⋅HCl/1 mM EDTA, pH 7.2) to a final concentration of 250 μM and stored at −20°C. The ODN suspension (100 nl, 2.5 μM) was injected according to the poly(A)+ mRNA injection protocol. The ODNs were injected 5 days after the oocytes were injected with striatal mRNA and then tested for NMDA/glycine-induced responses on day 7. The nucleotide sequences of the synthetic oligomers corresponding to base numbers 995-1009 of the rat DARPP-32 cDNA were as follows: antisense-DARPP-32, 5′-CTGAGCTTATGTGC-3′; reversed control-DARPP-32, 5′-CGTGTATTCGAGTC-3′; random control-DARPP-32, 5′-AGTCGCTGTGATCT-3′.
Electrophysiological Recordings.
Seven to eight days after injection, oocytes were placed in a recording chamber (volume ≈40 μl) and continuously superfused (1.5 ml/min) with recording solution at room temperature (20–24°C). The oocytes were voltage-clamped by a conventional two-microelectrode voltage-clamp technique (22). The membrane potential of the oocytes was held at −80 mV (unless otherwise indicated), using a Turbo Clamp Tec 01C amplifier (N.P.I. Electronic, Tamm, Germany). The two microelectrodes were filled with 3 M KCl and had resistances between 1 and 3 MΩ. Drugs were applied with a micropipette (200 μl) after stopping solution flow. If not indicated otherwise, NMDA and glycine were coapplied at concentrations of 100 μM and 10 μM, respectively. In some experiments, oocytes were preincubated with a drug-containing solution. During incubation, oocytes were continuously superfused with solutions containing the drugs to be applied. Calyculin A was prepared in 100% ethanol as a 1 mM stock solution. Immediately after dilution in distilled water to the appropriate concentration, calyculin A was microinjected into the oocytes according to the RNA injection protocol. Oocytes were preinjected 1–1.5 h before voltage-clamping. Aliquots of concentrated stock solutions of phorbol 12-myristate 13-acetate (PMA), 4-α-phorbol 12-myristate 13-acetate (4-α-PMA), forskolin, and 1,9-dideoxyforskolin in dimethyl sulfoxide (DMSO) and NMDA and glycine in distilled water were added to the recording solution immediately before the experiments. 8-Bromoadenosine 3′,5′monophosphate (8-Br-cAMP, sodium salt) was directly dissolved to the final concentration in the external solution. The final DMSO as well as the final ethanol concentration never exceeded 0.1% (vol/vol), which, upon application, induced no change in membrane current on its own and which had no effect on NMDA-induced ion currents in control experiments. Effects of the various compounds tested were studied after at least two or three identical responses to NMDA could be elicited. Oocytes were not used for experiments when reproducible responses to NMDA could not be recorded within 60 min. Current signals were low-pass filtered at 30 Hz by using a four-pole Bessel filter and digitized by an ITC 16-MAC interface (Instrutech, Great Neck, NY). Data were sampled at 100 Hz and stored on a Macintosh (7100/66) computer using data acquisition software (Pulse 7.40, HEKA Electronic, Lambrecht/Pfalz, Germany). The relative current amplitude of 100 μM NMDA- and 10 μM glycine-induced inward currents is defined as the ratio (I/Ic) of the maximum current amplitude after (I) and before (Ic) treatment with drugs.
Statistics.
Statistical comparisons were made by using Student’s t test. Results were expressed as mean ± standard error of the mean (SEM). P values ≥ 0.05 were regarded as not significant.
Solutions.
Modified Barth’s solution contained (in mM): 88 NaCl, 1 KCl, 2.4 NaHCO3, 15 Hepes, 0.8 MgSO4, 0.3 Ca(NO3)2, and 0.6 CaCl2, and 50 units/ml penicillin and 50 μg/ml streptomycin (adjusted to pH 7.6 with NaOH). Ca2+-free modified Barth’s solution contained (in mM): 88 NaCl, 1 KCl, 2.4 NaHCO3, 15 Hepes, 0.8 MgSO4 (adjusted to pH 7.6 with NaOH). Electrophysiological recordings were carried out in saline solution containing (in mM): 115 NaCl, 2.5 KCl, 1.8 BaCl2, 10 Hepes (pH adjusted to 7.2 with NaOH).
Materials.
Mature female specimens of Xenopus laevis were obtained from Kähler (Hamburg, Germany). Collagenase, type II, was from Worthington, and mRNA Purification Kit was from Pharmacia LKB Biotechnology. PMA and 4-α-PMA were obtained from Research Biochemicals (Natick, MA). Calyculin A was from Boehringer Mannheim. 1,9-Dideoxyforskolin and 8-Br-cAMP (sodium salt) were from Calbiochem. Penicillin and streptomycin were from GIBCO. All other drugs and salts were purchased from Sigma. Molecular biology reagents and restriction enzymes were purchased from Pharmacia, Promega, and New England Biolabs.
RESULTS
PKC and PKA Modulate Striatal NMDA Responses.
The effects of protein kinases on NMDA responses were studied by using Xenopus oocytes injected with mRNA isolated from rat striatum or hippocampus. Coapplication of NMDA and glycine at a holding potential of −80 mV elicited responses with the conventional properties of NMDA receptors expressed in oocytes (e.g., see refs. 23 and 24). When NMDA was applied without glycine, the amplitude of the NMDA responses was markedly reduced. The NMDA-induced ion currents were nearly completely inhibited by 20 μM of the competitive antagonist 2-amino-5-phosphonovaleric acid (APV). NMDA responses were almost completely blocked by coapplication of 1 mM Mg2+ or 1 μM MK-801, a noncompetitive NMDA receptor antagonist (data not shown). Repeated applications of NMDA and glycine with 4-min washing intervals between subsequent applications resulted in a stable NMDA-induced inward current (indicated as control values; Fig. 1; Table 1).
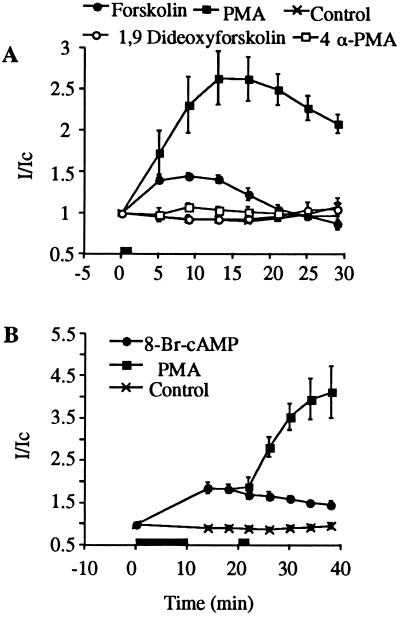
Figure 1.
Striatal NMDA-induced currents are potentiated by forskolin and PMA. The bar indicates drug superfusion. External solution was applied as control (×). (A) Forskolin (50 μM; •), PMA (10 nM; ▪), 1,9-dideoxyforskolin (50 μM; ○) and 4-α-PMA (10 nM; □) were applied for 1 min. (B) After a 10-min incubation with 8-Br-cAMP (10 mM; •), a 1-min incubation with PMA (10 nM; ▪) followed. Each point represents the mean ± SEM of three to seven oocytes.
Table 1.
Effect of protein kinase modulators on striatal NMDA-induced currents
| Compound | I/Ic* | n | P† |
|---|---|---|---|
| Control (9 min) | 0.92 ± 0.02 | 3 | — |
| Control (13 min) | 0.92 ± 0.04 | 3 | — |
| Control (14 min) | 0.91 ± 0.01 | 4 | — |
| PMA (10 nM)§ | 2.64 ± 0.33 | 6 | ≤0.01 |
| PMA (10 nM; −25 mV)§ | 2.40 ± 0.12 | 4 | ≤0.001 |
| 4-α-PMA (10 nM)§ | 1.07 ± 0.04 | 4 | NS |
| Forskolin (50 μM)‡ | 1.45 ± 0.03 | 4 | ≤0.001 |
| Forskolin (50 μM; −25 mV)‡ | 1.50 ± 0.10 | 4 | ≤0.01 |
| 1,9-Dideoxyforskolin (50 μM)‡ | 0.93 ± 0.04 | 3 | NS |
| 8-Br-cAMP (10 mM)¶ | 1.86 ± 0.13 | 7 | ≤0.001 |
Experiments were performed at a holding potential of −80 mV unless indicated otherwise.
The relative current amplitude is determined by the ratio (I/Ic) of steady-state responses to 100 μM NMDA and 10 μM glycine after (I) and before (Ic) drug treatment. With the exception of 8-Br-cAMP, which was applied for 10 min, all drugs were applied for 1 min. Results are mean ± SEM.
P values of Student’s t test obtained by comparing drug-treated oocytes with nontreated control oocytes. For comparisons controls recorded at 9 min (
), 13 min (
), and 14 min (
) were taken. NS, not significant.
After incubation with PMA, a potent PKC activator (25), a rapid potentiation of striatal NMDA-induced responses occurred, and a continuous rise was observed until a maximum was reached after 13 min (Fig. 1A; Table 1). Subsequently, the current amplitude decreased again (Fig. 1A). The inactive isomer 4-α-PMA had no significant effect (Fig. 1A; Table 1). Incubation with forskolin, which activates PKA by means of cAMP stimulation (reviewed in ref. 26), enhanced NMDA-induced currents in a time-dependent manner with a maximum at 9 min (Fig. 1A; Table 1). Because forskolin has been reported to act directly on ion channels in addition to its action on the cAMP cascade (e.g., ref. 27), the inactive forskolin analog 1,9-dideoxyforskolin was applied to test for this possible mode of action. This compound, which does not stimulate adenylyl cyclase, but mimics other actions of forskolin, did not exhibit a significant potentiating effect on NMDA-induced currents (Fig. 1A; Table 1).
Oocytes contain endogenous chloride channels that can be activated by an increase in the intracellular calcium concentration (28). Thus, influx of calcium through NMDA receptor channels (29) may lead to a secondary activation of endogenous chloride channels. To exclude the involvement of these chloride channels in the observed potentiation of NMDA-induced currents, all experiments were performed by replacing extracellular Ca2+ with Ba2+ ions, which are known to be less effective than Ca2+ ions in activating the calcium-dependent chloride currents in oocytes (28, 30). The influence of endogenous chloride channels has further been excluded by repeating the experiments at a holding potential of −25 mV, which is the reported reversal potential for chloride in oocytes (28, 31). At this holding potential, the potentiation induced by PMA and forskolin was not significantly different from the one observed at −80 mV (P > 0.05; Table 1). It was concluded that the observed potentiation was not due to the modulation of endogenous chloride channels.
Incubation with 8-Br-cAMP, a membrane-permeant analog of cAMP, increased striatal NMDA receptor-induced responses to 186% ± 13% (n = 7) of control. Interestingly, incubation with PMA produced further potentiation. The additional increase did not deviate significantly from the potentiation found with PMA alone (Fig. 1B).
PMA incubation of oocytes injected with hippocampal mRNA resulted in a transient potentiation of the NMDA-induced current responses. This potentiation reached a maximum value within approximately 13 min (Table 2). Similar incubation with the biologically inactive analog 4-α-PMA did not induce any change in responses to the agonists (93% ± 7%, n = 3; Table 2). At a holding potential of −25 mV the maximal increase of NMDA-induced ion currents after incubation with PMA was 227% ± 19% (n = 6). This degree of potentiation was not statistically different from the potentiation (241% ± 32%, n = 9) found at a holding potential of −80 mV (P > 0.05; Table 2). In contrast to the observed enhancement of the striatal NMDA response to PKA activation, incubation with forskolin did not significantly alter the hippocampal NMDA response (Fig. 4A; Table 2).
Table 2.
Effect of protein kinase modulators on hippocampal NMDA-induced currents
| Compound | I/Ic | n | P |
|---|---|---|---|
| Control (9 min) | 1.01 ± 0.03 | 5 | — |
| Control (13 min) | 1.02 ± 0.03 | 5 | — |
| PMA (10 nM)§ | 2.41 ± 0.32 | 9 | ≤0.01 |
| PMA (10 nM; −25 mV)§ | 2.27 ± 0.19 | 6 | ≤0.001 |
| 4-α-PMA (10 nM)§ | 0.93 ± 0.07 | 3 | NS |
| Forskolin (50 μM)‡ | 1.01 ± 0.03 | 5 | NS |
Data are presented as for Table 1.
Figure 4.
Forskolin-mediated potentiation of hippocampal NMDA responses is observed in the presence of DARPP-32. Forskolin (50 μM, •), 1,9-dideoxyforskolin (50 μM; ○), and external solution (control, ×) were applied for 1 min as indicated by the bar. NMDA-induced current responses were recorded from oocytes injected with hippocampal mRNA (A) or oocytes injected with hippocampal mRNA and DARPP-32 cRNA (80 ng per oocyte) (B). Each point represents the mean ± SEM of three to nine oocytes.
Striatal and Hippocampal NMDA Responses Are Regulated by Endogenous Protein Phosphatases.
The possibility that NMDA responses could be regulated not only by protein kinases but also by endogenous protein phosphatases was investigated by 5-min application of calyculin A (100 nM), a potent inhibitor of PP1 and PP2A (32, 33). Following this treatment, NMDA responses increased and reached maximal potentiation after 70–90 min. Striatal NMDA-induced currents were potentiated to 157% ± 12% (n = 5) and hippocampal NMDA-induced currents were enhanced to 137% ± 8% (n = 4) of the corresponding control values. The enhancement of striatal NMDA responses observed after application of calyculin A did not differ significantly from the value obtained after PKA stimulation.
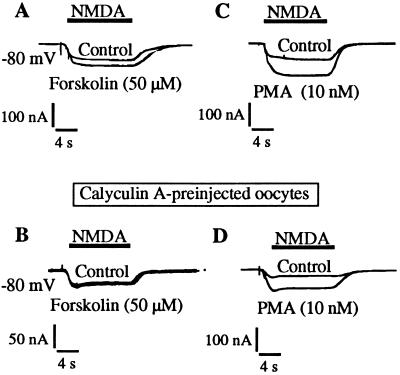
Calyculin A Antagonizes PKA- but Not PKC-Mediated Potentiation of Striatal NMDA Responses.
In oocytes injected with striatal mRNA, the potentiation of NMDA-induced currents observed after forskolin application (Fig. 2A; Table 1) could be prevented by preinjection of calyculin A 60–90 min before voltage-clamping (Fig. 2B). The inhibitory effect of calyculin A on the PKA-mediated potentiation of striatal NMDA responses was dose dependent. A 50% reduction (IC50) of the potentiation was observed at 0.56 nM calyculin A (final intracellular concentration). The PMA-induced potentiation of striatal NMDA responses (Fig. 2C; Table 1) was not significantly altered when oocytes were preinjected with calyculin A (Fig. 2D).
Figure 2.
Calyculin A inhibits forskolin- but not PMA-mediated potentiation of striatal NMDA responses. The NMDA-induced currents of striatal mRNA-injected oocytes were measured before and 8 min after 1-min application of 50 μM forskolin (A) or before and 12 min after 1-min application of 10 nM PMA (C). (B and D) The same protocol was followed after injecting oocytes with calyculin A to a final intracellular concentration of 500 nM 60–90 min before voltage-clamping. The intracellular concentration of calyculin A was calculated by assuming standard oocytes with a volume of 0.5 μl.
Expression of DARPP-32 Renders Hippocampal NMDA Receptors Sensitive to PKA.
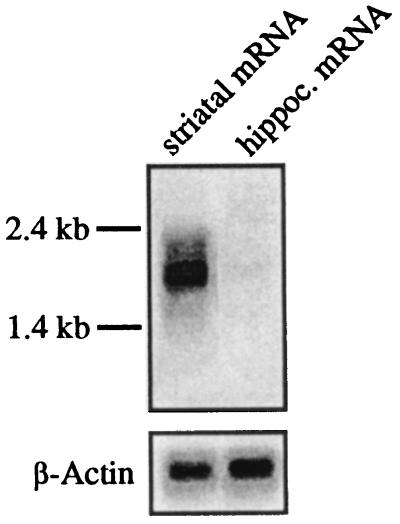
The observation that calyculin A was able to prevent the PKA-mediated potentiation of striatal NMDA responses suggested the involvement of a third messenger, which would inhibit protein phosphatases after stimulation of PKA. One possible molecule to be considered was DARPP-32, which is highly enriched in rat striatum (34, 35). A variety of studies demonstrated that DARPP-32 is converted into a potent inhibitor of PP1 by PKA-mediated phosphorylation (36, 37). The amount of DARPP-32 mRNA in mRNA aliquots used for injecting the oocytes was assessed by Northern blot analysis. Hybridization with radioactively labeled DARPP-32 cDNA revealed an RNA doublet of approximately 1.8 and 2 kb in striatum. By contrast, only extremely small amounts of DARPP-32 mRNA were detectable in hippocampal mRNA (Fig. 3). Hybridization with β-actin demonstrated that equal amounts of mRNA were used for each sample.
Figure 3.
Northern blot analysis of poly(A)+ mRNA isolated from rat striatum and hippocampus. In each lane 3 μg of RNA was loaded. The full-length cDNA encoding DARPP-32 was radioactively labeled and used as a probe. The lower bands show the hybridization of the RNA probes with mouse β-actin.
To investigate whether activation of DARPP-32 could cause an enhancement of NMDA-induced currents after stimulation of PKA, hippocampal mRNA was coinjected with DARPP-32 cRNA. Under these conditions, incubation with forskolin potentiated NMDA-induced currents within 9 min to 123% ± 6% (n = 3; 20 ng of DARPP-32 cRNA per oocyte) or 128% ± 4% of control values (n = 8; 80 ng of DARPP-32 cRNA per oocyte; Fig. 4B). This enhancement of hippocampal NMDA responses was not significantly different from the one observed after calyculin A treatment. The inactive forskolin analog 1,9-dideoxyforskolin had no effect (Fig. 4B). When oocytes were preinjected with calyculin A 60–90 min before voltage-clamping, forskolin could not alter NMDA-induced currents. These data resembled the results observed with oocytes injected with striatal mRNA.
Inhibition of DARPP-32 Expression Reduces the PKA-Mediated Potentiation of Striatal NMDA Responses.
Oocytes injected with striatal mRNA and antisense ODNs directed against DARPP-32 were tested for PKA-mediated potentiation of NMDA-induced currents. After injection of the antisense ODNs in striatal mRNA-injected oocytes, PKA stimulation caused a markedly reduced potentiation of NMDA-induced currents (112% ± 4%, n = 7; Fig. 5) compared with control NMDA-induced currents recorded from oocytes injected with striatal mRNA and TE buffer (160% ± 12%, n = 4; Fig. 5). The specificity of the antisense ODNs was assessed by injecting striatal mRNA-injected oocytes with either random or reversed control ODNs. Neither random nor reversed control ODNs abolished the PKA-mediated potentiation of NMDA responses (163% ± 16%, n = 4; 158% ± 6%, n = 4; Fig. 5, respectively).
Figure 5.
Forskolin-mediated potentiation of striatal NMDA responses requires DARPP-32. (A) Representative NMDA responses of oocytes injected with striatal mRNA and ODNs or TE buffer before (controls) and 8 min after 1-min application of forskolin (50 μM). (B) Averaged relative current amplitudes (I/Ic) of the experiments presented in A. Each bar represents the mean ± SEM of four or seven oocytes as indicated.
DISCUSSION
PMA enhanced the NMDA receptor function in Xenopus oocytes injected with rat mRNA isolated from either striatum or hippocampus. In contrast, forskolin enhanced the NMDA-induced currents recorded from oocytes injected with striatal mRNA but not hippocampal mRNA. These findings were in general agreement with previous experiments performed in rat hippocampal and striatal neurons (14, 38–42). PKC and PKA acted additively, indicating that the two enzymes exerted their modulatory action on the NMDA receptor complex by phosphorylation at separate sites.
The finding that PKA-induced potentiation of striatal NMDA responses was prevented by preinjection of oocytes with the protein phosphatase inhibitor calyculin A suggested the involvement of PP1 and/or PP2A. The basal activity of endogenous protein phosphatases was indicated by the fact that application of calyculin A enhanced striatal and hippocampal NMDA currents. These results were in agreement with the observation by Colwell and Levine (14) that the phosphatase inhibitor okadaic acid enhanced excitatory synaptic transmission in the neostriatum.
After application of calyculin A, striatal NMDA currents were enhanced to the same extent as observed after the activation of PKA. In contrast, calyculin A did not prevent the PKC-mediated potentiation of striatal NMDA responses.
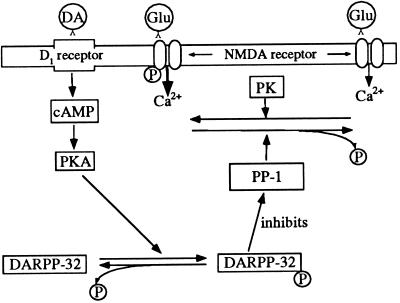
DARPP-32 is phosphorylated by PKA, and it acts in its phosphorylated form as a potent and specific inhibitor of PP1 (34, 36, 43). On the basis of our experimental data, DARPP-32 seemed to play a pivotal role in the PKA-mediated enhancement of NMDA-induced currents. This hypothesis was strongly supported by the observation that the PKA-mediated enhancement of striatal NMDA responses was significantly reduced by the injection of antisense ODNs directed against mRNA coding for DARPP-32. It is also in agreement with this hypothesis that hippocampal NMDA responses could be enhanced by forskolin when cRNA coding for DARPP-32 was coinjected. Interestingly, the PKA-mediated enhancement of NMDA responses recorded from oocytes injected with hippocampal mRNA plus DARPP-32 cRNA was similar to the enhancement of hippocampal NMDA responses following the inhibition of protein phosphatases by calyculin A. The PKA-mediated potentiation of NMDA responses recorded from striatal mRNA-injected oocytes or hippocampal mRNA-injected oocytes coexpressing DARPP-32 was prevented by preinjecting calyculin A. Thus the effects of forskolin and of calyculin A were not additive in either system. These results suggested that PKA, acting by means of phosphorylation of DARPP-32, as well as calyculin A, modulated NMDA responses by inhibiting endogenous PP1.
Cepeda et al. (15) reported the enhancement of NMDA-evoked excitations in cat and rat neostriatal slices after application of D1 receptor agonists. Stimulation of D2 receptors attenuated responses evoked by NMDA. On the basis of our findings, one can speculate that dopamine modulates striatal NMDA responses by indirect regulation of PP1 activity via DARPP-32. In agreement with this speculation, previous studies have shown that D1 receptor agonists increased the amount of both cAMP (44) and phosphorylated DARPP-32 (43, 45). The increasing phosphorylation of DARPP-32 was mediated through the activation of PKA (46, 47). Conversely, stimulation of D2 receptors in rat striatum reduced the amount of both cAMP (48, 49) and phosphorylated DARPP-32 (50). This effect of D2 receptor activation on DARPP-32 appeared to be due both to decreased phosphorylation of DARPP-32 through the cAMP/PKA pathway and to increased dephosphorylation of DARPP-32 through the Ca2+/calcineurin pathway (50).
The regional distribution of DARPP-32 within the rat brain is very similar to the pattern of dopamine-innervated brain regions. Immunocytochemical studies have localized DARPP-32 at particularly high levels in the substantia nigra, olfactory tubercle, bed nucleus of the stria terminalis, globus pallidus, caudatoputamen, nucleus accumbens, portions of the amygdaloid complex, and corticothalamic neurons (51). Therefore, the signal transduction cascades described above may contribute to synaptic plasticity in these brain regions. Neurotransmitters (e.g., dopamine) coupled either positively or negatively to the adenylyl cyclase system could differentially modulate the intracellular cAMP level and thereby the amount of phosphorylated DARPP-32. The concentration of phosphorylated DARPP-32 in turn would be responsible for the degree of PP1 inhibition, thus modulating NMDA receptor function by decreasing or increasing the dephosphorylation of the NMDA receptor itself or, alternatively, a regulatory protein (Fig. 6). On the other hand, stimulation of NMDA receptors in rat striatal slices has been shown to induce dephosphorylation of phosphorylated DARPP-32, presumably by the calcium-dependent phosphatase calcineurin (52). This mechanism might reflect a negative feedback-loop protecting striatal cells from NMDA receptor-mediated toxicity in the presence of high amounts of phosphorylated DARPP-32 (53).
Figure 6.
Schematic diagram illustrating the possible role of DARPP-32 and PP1 in mediating dopamine-induced increase in conductance through NMDA receptors in rat striatum. Glu, glutamate; DA, dopamine; P, phosphate group; PK, protein kinase.
The present study provides electrophysiological evidence that PKA may regulate NMDA receptor function by means of DARPP-32 and an endogenously active protein phosphatase. In the DARPP-32-enriched striatum this third-messenger pathway may participate in the control of the phosphorylation state of NMDA receptors and thereby control the excitability of striatal neurons and the efficacy of synaptic transmission. The complex control system of NMDA receptor phosphorylation may facilitate the integration of multiple neuronal signals converging on DARPP-32-containing neurons.
Acknowledgments
We thank Dr. Frank Dautzenberg and Dr. Sabine Sydow for discussions and Gudrun Fricke-Bode for technical assistance. Support for this work was received from U.S. Public Health Service Grants MH-40899 and DA-10044 to P.G.
ABBREVIATIONS
- DARPP-32
dopamine and cyclic AMP-regulated phosphoprotein of Mr 32,000
- NMDA
N-methyl-d-aspartate
- PKA
cAMP-dependent protein kinase
- PKC
protein kinase C
- PP1 and PP2A
protein phosphatases 1 and 2A
- ODNs
oligodeoxynucleotides
- PMA
phorbol 12-myristate 13-acetate
References
- 1.Voorn P, Jorritsma-Byham B, Van Dijk B, Buijs R M. J Comp Neurol. 1986;251:84–99. doi: 10.1002/cne.902510106. [DOI] [PubMed] [Google Scholar]
- 2.Doucet G, Descarries L, Garcia S. Neuroscience. 1986;19:427–445. doi: 10.1016/0306-4522(86)90272-1. [DOI] [PubMed] [Google Scholar]
- 3.McGeer P L, McGeer E G, Scherer U, Singh K. Brain Res. 1977;128:369–373. doi: 10.1016/0006-8993(77)91003-4. [DOI] [PubMed] [Google Scholar]
- 4.Fonnum F, Storm-Mathisen J, Divac I. Neuroscience. 1981;6:863–873. doi: 10.1016/0306-4522(81)90168-8. [DOI] [PubMed] [Google Scholar]
- 5.Dube L, Smith A D, Bolam J P. J Comp Neurol. 1988;267:455–471. doi: 10.1002/cne.902670402. [DOI] [PubMed] [Google Scholar]
- 6.Choi D W. Neuron. 1988;1:623–634. doi: 10.1016/0896-6273(88)90162-6. [DOI] [PubMed] [Google Scholar]
- 7.DiFiglia M. Trends Neurosci. 1990;13:286–289. doi: 10.1016/0166-2236(90)90111-m. [DOI] [PubMed] [Google Scholar]
- 8.Greenamyre J T, O’Brien C F. Arch Neurol. 1991;48:977–981. doi: 10.1001/archneur.1991.00530210109030. [DOI] [PubMed] [Google Scholar]
- 9.Hollmann M, Heinemann S. Annu Rev Neurosci. 1994;17:31–108. doi: 10.1146/annurev.ne.17.030194.000335. [DOI] [PubMed] [Google Scholar]
- 10.Tingley W G, Roche K W, Thompson A K, Huganir R L. Nature (London) 1993;364:70–73. doi: 10.1038/364070a0. [DOI] [PubMed] [Google Scholar]
- 11.Moon I S, Apperson M L, Kennedy M B. Proc Natl Acad Sci USA. 1994;91:3954–3958. doi: 10.1073/pnas.91.9.3954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lau L F, Huganir R L. J Biol Chem. 1995;270:20036–20041. doi: 10.1074/jbc.270.34.20036. [DOI] [PubMed] [Google Scholar]
- 13.Snyder G, Fienberg A, Dulubova I, Nairn A C, Greengard P. Soc Neurosci Abstr. 1996;22:153.11. [Google Scholar]
- 14.Colwell C S, Levine M S. J Neurosci. 1995;15:1704–1713. doi: 10.1523/JNEUROSCI.15-03-01704.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cepeda C, Buchwald N A, Levine M S. Proc Natl Acad Sci USA. 1993;90:9576–9580. doi: 10.1073/pnas.90.20.9576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Colwell C S, Levine M S. Neuroscience. 1994;61:497–507. doi: 10.1016/0306-4522(94)90429-4. [DOI] [PubMed] [Google Scholar]
- 17.Portera-Cailliau C, Price D L, Martin L J. J Neurochem. 1996;66:692–700. doi: 10.1046/j.1471-4159.1996.66020692.x. [DOI] [PubMed] [Google Scholar]
- 18.Petralia R S, Wang Y X, Wenthold R J. J Neurosci. 1994;14:6102–6120. doi: 10.1523/JNEUROSCI.14-10-06102.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cathala G, Savouret J F, Mendez B, West B L, Karin M, Martial J A, Baxter J D. DNA. 1983;2:329–335. doi: 10.1089/dna.1983.2.329. [DOI] [PubMed] [Google Scholar]
- 20.Kushner L, Lerma J, Zukin R S, Bennett M V L. Proc Natl Acad Sci USA. 1988;85:3250–3254. doi: 10.1073/pnas.85.9.3250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Church G M, Gilbert W. Proc Natl Acad Sci USA. 1984;81:1991–1995. doi: 10.1073/pnas.81.7.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stühmer W. Methods Enzymol. 1992;207:319–339. doi: 10.1016/0076-6879(92)07021-f. [DOI] [PubMed] [Google Scholar]
- 23.Leonard J P, Kelso S R. Neuron. 1990;2:53–60. doi: 10.1016/0896-6273(90)90443-j. [DOI] [PubMed] [Google Scholar]
- 24.Kelso S R, Nelson T E, Leonard J P. J Physiol (London) 1992;449:705–718. doi: 10.1113/jphysiol.1992.sp019110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stea A, Soong T W, Snutch T P. Neuron. 1995;15:929–940. doi: 10.1016/0896-6273(95)90183-3. [DOI] [PubMed] [Google Scholar]
- 26.Seamon K B, Daly J W. Adv Cyclic Nucleotide Protein Phosphorylation Res. 1986;20:1–150. [PubMed] [Google Scholar]
- 27.Laurenza A, Sutkowski E M, Seamon K B. Trends Pharmacol Sci. 1989;10:442–447. doi: 10.1016/S0165-6147(89)80008-2. [DOI] [PubMed] [Google Scholar]
- 28.Barish M E. J Physiol (London) 1983;342:309–325. doi: 10.1113/jphysiol.1983.sp014852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.MacDermott A B, Mayer M L, Westbrook G L, Smith S J, Barker J L. Nature (London) 1986;321:261–263. doi: 10.1038/321519a0. [DOI] [PubMed] [Google Scholar]
- 30.Miledi R, Parker I. J Physiol (London) 1984;357:173–183. doi: 10.1113/jphysiol.1984.sp015495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miledi R. Proc R Soc London Ser B. 1982;215:491–497. doi: 10.1098/rspb.1982.0056. [DOI] [PubMed] [Google Scholar]
- 32.Ishihara H, Martin B L. Biochem Biophys Res Commun. 1989;159:871–877. doi: 10.1016/0006-291x(89)92189-x. [DOI] [PubMed] [Google Scholar]
- 33.Suganuma M, Fujiki H, Furuya-Suguri H, Yoshizawa S, Yasumoto S, Kato Y, Fusetani N, Sugimura T. Cancer Res. 1990;50:3521–3525. [PubMed] [Google Scholar]
- 34.Walaas S I, Greengard P. J Neurosci. 1984;4:84–98. doi: 10.1523/JNEUROSCI.04-01-00084.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hemmings H C, Jr, Greengard P. J Neurosci. 1986;6:1469–1481. doi: 10.1523/JNEUROSCI.06-05-01469.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hemmings H C, Jr, Greengard P, Tung H Y L, Cohen P. Nature (London) 1984;310:503–505. doi: 10.1038/310503a0. [DOI] [PubMed] [Google Scholar]
- 37.Hemmings H C, Jr, Girault J A, Nairn A C, Bertuzzi G, Greengard P. J Neurochem. 1992;59:1053–1061. doi: 10.1111/j.1471-4159.1992.tb08347.x. [DOI] [PubMed] [Google Scholar]
- 38.Aniksztejn L, Otani S, Ben-Ari Y. Eur J Neurosci. 1992;4:500–505. doi: 10.1111/j.1460-9568.1992.tb00900.x. [DOI] [PubMed] [Google Scholar]
- 39.O’Connor J J, Rowan M J, Anwyl R. J Neurosci. 1995;15:2013–2020. doi: 10.1523/JNEUROSCI.15-03-02013.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Harvey J, Collingridge G H. Br J Pharmacol. 1993;109:1085–1090. doi: 10.1111/j.1476-5381.1993.tb13733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Greengard P, Jen J, Nairn A C, Stevens C F. Science. 1991;253:1135–1138. doi: 10.1126/science.1716001. [DOI] [PubMed] [Google Scholar]
- 42.Wang L Y, Salter M W, MacDonald J F. Science. 1991;253:1132–1135. doi: 10.1126/science.1653455. [DOI] [PubMed] [Google Scholar]
- 43.Walaas S I, Aswad D W, Greengard P. Nature (London) 1983;301:69–71. doi: 10.1038/301069a0. [DOI] [PubMed] [Google Scholar]
- 44.Azzaro A J, Liccione J, Lecci J. Naunyn-Schmiedebergs Arch Pharmacol. 1987;336:133–138. doi: 10.1007/BF00165796. [DOI] [PubMed] [Google Scholar]
- 45.Szmigielski A, Zalewska-Kaszubska L. Neuropharmacol. 1991;30:259–266. doi: 10.1016/0028-3908(91)90153-3. [DOI] [PubMed] [Google Scholar]
- 46.Hemmings H C, Jr, Nairn A C, Greengard P. J Biol Chem. 1984;259:14491–14497. [PubMed] [Google Scholar]
- 47.Hemmings H C, Jr, Nairn A C, Elliott J I, Greengard P. J Biol Chem. 1990;265:20369–20376. [PubMed] [Google Scholar]
- 48.Weiss S, Sebben M, Garcia-Sainz J A, Bockaert J. Molec Pharmacol. 1985;27:595–599. [PubMed] [Google Scholar]
- 49.Cooper D M F, Bier-Laning C M, Halford M K, Ahlijanian M K, Zahniser N R. Mol Pharmacol. 1986;29:113–119. [PubMed] [Google Scholar]
- 50.Nishi A, Snyder G L, Greengard P. J Neurosci. 1997;17:8147–8155. doi: 10.1523/JNEUROSCI.17-21-08147.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ouimet C C, Miller P E, Hemmings H C, Jr, Walaas S I, Greengard P. J Neurosci. 1984;4:111–124. doi: 10.1523/JNEUROSCI.04-01-00111.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Halpain S, Girault J A, Greengard P. Nature (London) 1990;343:369–372. doi: 10.1038/343369a0. [DOI] [PubMed] [Google Scholar]
- 53.Colwell C S, Altemus K L, Cepeda C, Levine M S. Proc Natl Acad Sci USA. 1996;93:1200–1204. doi: 10.1073/pnas.93.3.1200. [DOI] [PMC free article] [PubMed] [Google Scholar]