Abstract
Purpose
The major purpose of this study was to provide information about expected spoken language skills of preschool-aged children who are deaf and who use a cochlear implant. A goal was to provide “benchmarks” against which those skills may be compared, for a given age at implantation. We also examined whether parent-completed checklists of children's language were correlated with results of standardized language tests and whether scores increased linearly with decreasing age-of-implantation and increasing duration of cochlear implant use.
Method
Participants were a nation-wide sample of 76 children who were deaf and orally-educated and who received an implant by 38 months of age. Formal language tests were administered at age 4.5 years. The MacArthur-Bates Communicative Development Inventory (MBCDI) was completed by parents when children were ages 3.5 and 4.5 years.
Results
Based on regression analyses, expected test scores for each age at implant are provided for two commonly administered language tests at 4.5 years of age and MBCDI subscale scores at 3.5 and 4.5 years. Concurrent test scores were significantly correlated on all measures. A linear relation was found which predicted increasing test scores with younger ages at implantation for all scales administered.
Conclusions
While the expected scores reported here should not be considered as normative data, they are benchmarks which may be useful for evaluating spoken language progress of children with cochlear implants in enrolled in spoken language-based programs.
Published literature shows that children who are profoundly deaf and who receive a cochlear implant often achieve spoken language skills much closer to the skills of their hearing peers than previously possible. Levels of spoken language skill previously achieved only occasionally in children who were profoundly deaf and used hearing aids have now become the norm, with higher levels seen in the areas of speech perception (Eisenberg et al., 2006), speech production (Chin, Tsai & Gao, 2003; Flipsen & Colvard, 2006; Horga & Liker, 2006; Tobey, Geers, Brenner, Altuna, & Gabbert, 2003), language (Moog, 2002; Nicholas & Geers, 2006a; 2006b), and reading (Geers, 2003; Spencer, Tomblin & Gantz, 1998). Many educators and clinicians working with children who have severe-profound hearing loss are revising educational strategies and expectations based upon the general success facilitated by cochlear implant (CI) devices.
Sources of Variability
Prior to surgery, parents often ask clinicians to describe the spoken language proficiency that may be expected following cochlear implantation. During post-implant habilitation, they may ask whether their child is making expected progress in relation to other children with CIs. Despite the impressive skills achieved by many children with CIs, variability in progress remains a significant concern. The range of observed outcomes adds uncertainty to projecting future progress for individual children and to assessing relative progress as the child gains experience with the implant. When attempting to estimate the spoken language level expected for an individual child, the clinician must consider a range of possible factors that might contribute to or detract from post-implant outcomes.
Early cochlear implantation, in itself, does not insure that a child will develop facility with spoken language. Even in the best case, several years of intensive intervention in a school, therapy, or home setting is usually required for children to be able to achieve age-appropriate spoken language skills. The need for this period of orientation, training, and practice cannot be over-estimated. However, even with this programming in place, there are some children who do not progress in spoken communication skills as quickly as others. It is unclear, in many cases, why some children seem to benefit more from the hearing provided by the implant than others.
There are a number of factors that are being investigated as possible causes of this variability. Potential sources include rehabilitative factors such as the age of the child at diagnosis, amplification, habilitation, CI fitting (Yoshinaga-Itano, 2003; Kirk, Miyamoto, Lento et al., 2002; Nicholas & Geers, 2006a) and whether post-implant educational intervention is speech-based or sign-speech based (Connor, Hieber, Arts & Zwolan, 2000; Moog & Geers, 2003), and whether the child is in a special education or mainstream classroom (Geers, Nicholas & Sedey, 2003). Another set of factors being examined are medical/audiological in nature, including cause of deafness (Mitchell, Psarros, Pegg, Rennie & Gibson, 2000; Bauer, Geers, Brenner, Moog & Smith, 2003; Nikolopoulos, Archbold, & O'Donoghue, 2006), age at onset of deafness (Geers, 2004a), whether better or poorer hearing ear receives the implant (Friedland, Venick & Niparko, 2003; Francis, Yeagle, Bowditch & Niparko, 2005), whether a contralateral hearing aid is used (Holt, Kirk, Eisenberg, Martinez & Campbell, 2005; Ching, Psarros, Hill, Dillon & Incerti, 2001), the CI technology (Geers, Brenner, & Davidson, 2003) and the degree of pre-implant hearing available to the child (Nicholas & Geers, 2006b). The impact of all of these factors must be considered in light of child and family characteristics that may affect language development, including level of nonverbal intelligence (Holt & Kirk, 2005), motor skills (Horn, Pisoni & Miyamoto, 2006), memory/processing abilities (Pisoni & Cleary, 2003; Dawson, Busby, McKay & Clark, 2002), and demographic characteristics such as the child's gender, family size and parents' education (Stacey, Fortnum, Barton & Summerfield, 2006; Geers, Nicholas & Sedey, 2003). In addition, expected language skills change over time as the child matures and accumulates more experience with the CI device. It is important to take into account the effects of these factors on an individual child's expected spoken language achievement at any given point in time.
Pre-Implant Residual Hearing
There is evidence that children with some pre-implant speech recognition ability achieve better open-set speech perception at one year post-implant than children with no pre-implant speech recognition (Zwolan et al., 1997). Furthermore, children with pre-implant speech perception scores as high as 30% with hearing aids have shown improved speech perception following cochlear implantation. This finding has resulted in expanded FDA candidacy criteria (ASHA, 2003) for children implanted at age 24 months or later. However, children implanted at the youngest ages (12-23 months) tend to have more profound hearing losses than those implanted somewhat later (Nicholas & Geers, 2006b). Further, children with greater residual hearing pre-implant have been found to exhibit better spoken language skills following cochlear implantation (Nicholas & Geers, 2006b; Szagun, 2001). This may be due to their early pre-implant access to language or to better auditory nerve survival. Kuo and Gibson (2000) found better post-implant gains for those with better aided hearing ability above 2000 Hz, though only for children implanted above the age of 10 years. Regardless of the reason for a possible advantage, it is important to control for the effects of pre-implant hearing before examining the effects of implant age on spoken language outcome. We have previously reported (Nicholas & Geers, 2006b) that when the effects of pre-implant hearing were controlled, children who received a CI by their 2nd birthday exhibited an advantage over children who received one between 25-38 months of age.
Validity of Early Language Measures
Obtaining valid estimates of language levels at young ages may present difficulties. Preschool-aged children's day-to-day or hour-to-hour behavior can be highly variable. This variability is one of the major advantages of parent report measures over direct testing, and of using multiple over single measures (Lidz, 1983). While direct sampling of conversational language rates high marks for face validity, it is not a procedure that is easily translated into classroom or therapy assessment situations and it may be affected by a child's attitude or willingness to communicate. On the other hand, use of parent-completed checklists take into consideration a child's maximum performance across a wide variety of situations and are not dependent upon child cooperation at a given moment in time (Fenson et al., 1994; Fenson et al., 1993). However, because parents may not be truly objective, it is important to establish validity of these reports by comparing them to measures based on direct observation, such as from a language sample or formal testing. Studies have been published showing good agreement between such measures when used with normally hearing, typically-developing children (Dale, 1991; Feldman, Dale, Campbell, et al., 2005).
Several recent studies have confirmed the validity of using a parent report checklist in estimating the language of young children with CIs. Thal, DesJardin, & Eisenberg (2007) asked parents to complete the MacArthur-Bates Communicative Development Inventory (MBCDI; Fenson et al., 1993) with reference to 24 children with CIs who were between 32-86 months of age at time of testing. These children were considerably older than the MBCDI's chronologic age norming range. They reported moderate-large correlations between scores on the MBCDI with both formal language test scores and with language variables derived from spontaneous language samples. Similarly, Stallings, Gao & Svirsky (2002) utilized the MBCDI to document the language skills of children with CIs who were older than children in the normative sample and found significant correlations between those scores and concurrent scores on the Reynell Developmental Language Scales (Reynell & Gruber, 1990). Other validity studies have been published utilizing the MBCDI with children who experienced language delay and who also were older the normative sample (Thal, O'Hanlon, Clemmons & Fralin, 1999).
In our previous work, comparison of scores on variables derived from videotaped language samples with those based on parent- or teacher- checklist reports revealed a high degree of association, with correlation coefficients ranging from .64 to .89 (all p ≤ .001). In fact, the scores on these measures could be combined into a single score that accounted for 77% of the variance in the original set of variables. Those results suggested that parent and teacher reporting instruments may provide valid estimates of language level in a more convenient manner than language sampling, especially at very young ages (Nicholas & Geers, 2006b).
By the time a child is four to five years old, teachers and clinicians typically must limit their assessment efforts to the use of standardized tests that provide age-appropriate normative data for reasons of efficiency and accountability. At the present time no tests are available that provide normative spoken language data gathered on preschool aged children with CIs. Clinicians are left to “make do” with tests designed for administration to children with normal hearing or those normed on children with hearing loss before the advent of CIs. Neither comparison provides information entirely appropriate for use with this population of children. Comparisons based on children who have heard normally since birth set an unrealistically high standard for those who have not had access to sound during the early language-learning years. On the other hand, comparisons with children who are profoundly deaf and have had very limited auditory speech perception with hearing aids may be unrealistically low when assessing those who have had the benefit of early cochlear implantation.
Language Test Scores following Early Cochlear Implantation
Rate of spoken language progress is often reflected in standardized language tests by a language quotient score. This score is sometimes expressed as a ratio between a norm-based language age-equivalency score and chronological age. More recently, the language quotient is expressed as a standard score relative to the mean and standard deviation of an age-appropriate normative group. Hearing children who comprise normative samples for language tests tend to maintain a fairly constant quotient score over time. Children who are profoundly deaf and use hearing aids display slower spoken language development than hearing age-mates, averaging about half the rate of hearing peers (Boothroyd, Geers, & Moog, 1991). On the other hand, other studies have shown that following cochlear implantation these children start developing language at a near-normal rate (Svirsky, Teoh & Neuberger, 2004). Children who receive a CI by age 3 years have been observed to narrow the gap between their language abilities and those expected for hearing children at their chronologic age. As a result language quotient scores actually improve with longer duration of CI experience (Kirk, Miyamoto, Lento et al., 2002; Kirk, Miyamoto, Ying, Perdew & Zuganelis, 2002) and speech production skills develop at an accelerated rate (Connor, Craig, Raudenbush, Heavner & Zwolan, 2006). Consequently, many children who receive a CI under the age of two years and who receive speech and language services during the preschool years can achieve nearly age-appropriate spoken language by 4.5-6.0 years of age (Nicholas & Geers, 2007; Moog, 2002; Manrique, Cervera-Paz, Huarte, & Molina, 2004). Age-appropriate language scores on standardized tests may be considered an important prerequisite to successful placement in classes with hearing age-mates. Knowing in advance when an individual child might be expected to score at age-appropriate levels on standardized language tests could greatly aid educational planning. Knowing that a child is on-track for achieving normal levels as he/she progresses through a special education program can be reassuring for parents and teachers alike and may help to determine when a move to mainstream placement can be beneficial for the child's development.
Purposes of the Present Study
There were three purposes of the present study. The first was to determine whether parent reports of children's language were consistent with results of standardized language tests and whether they predicted later language scores. Second, it was important to further explore the relationship between language outcomes and age at implantation that was observed in previous studies and to determine whether those results hold for multiple language evaluation instruments. Third, we wanted to provide “benchmarks” against which some children's spoken language skills may be evaluated in comparison to children with similar characteristics and experiences.
Method
Participants
A nation-wide sample of 76 children was selected for participation in this study, 38 girls and 38 boys. This sample of children has been previously described in related publications (Nicholas & Geers, 2006b; Nicholas & Geers, 2007). Audiological characteristics of the sample are summarized in Table 1. Sample selection was used to control for a number of relevant variables as follows. (1) Age at Onset: All hearing losses were presumed to be congenital as candidate children were not included in the study if there was any evidence of previously normal hearing or a progressive hearing loss. (2) Learning Ability: All children scored within or above the average range on either a nonverbal intelligence test administered by their school (specific test varied by school preference) or the Daily Living Skills and Motor domains of the Vineland Adaptive Behavior Scales (Sparrow, Balla & Cicchetti, 1984). No other developmental or medical conditions that would likely interfere with communication had been identified. (3) Communication Mode: All children had been enrolled in some form of oral educational programming since receiving a CI and spoken English was the primary language of the home. (4) Technology: The children had received a CI between 1998 and 2003 and therefore used a similar generation of implant technology. Forty-seven of the children had received a Nucleus-24 implant from the Cochlear Corporation, 28 had a Clarion 1.2 or “CII” implant from the Advanced Bionics Corporation, and one child had a Med-El device. Seventy percent of the children in this sample were using processing strategies that were considered “up-to-date” at the time of this publication. Table 2 provides a complete listing of the processing strategies used with each of these implant types. All children entering the study had a full insertion of the electrode array and no prior problems with the implant leading to loss of use for more than 30 days. After the children entered the study at age 3.5 years, actual interruption of CI use was minimal. Three of the 76 children had processors replaced after 2-3 weeks of intermittent functioning. One child received a second (bilateral) implant and had the original implant turned off for a 10-week adjustment period. 5) Age at Implant: CI surgery took place between the ages of 12-38 months of age with the following distribution: N = 26 at 12-18 months, N = 20 at 19-24 months, N = 10 at 24-30 months, and N = 20 at 31-38 months. Seven children currently wore hearing aids in the ear contra-lateral to the CI.
Table 1.
Participant Audiological Characteristics
| Mean | Standard Deviation | Range | N | ||
|---|---|---|---|---|---|
| Unaided PTA (dB HL) | 107.19 | 10.81 | 77-120 | 76 | |
| at 500 Hz | 100.46 | 11.76 | 75-120 | 70 | |
| at 1,000 Hz | 107.14 | 12.38 | 70-120 | 70 | |
| at 2,000 Hz | 109.57 | 12.54 | 75-120 | 69 | |
| Pre-CI Aided PTA (dB HL) | 64.62 | 14.57 | 32-80 | 76 | |
| at 500 Hz | 60.99 | 14.60 | 30-80 | 71 | |
| at 1,000 Hz | 62.69 | 15.12 | 35-80 | 66 | |
| at 2,000 Hz | 66.23 | 15.00 | 30-80 | 64 | |
| Age first aided (months) | 12.13 | 8.04 | 1-30 | 76 | |
| Duration of HA use (months)* | 11.0 | 6.27 | 0-30 | 76 | |
| Age at Implant (months) | 23.16 | 7.73 | 12-38 | 76 | |
| CI PTA (dB HL) | 30.21 | 5.19 | 20-43 | 76 | |
| Age at 3.5 Test (months) | 42.75 | 1.16 | 40-45 | 76 | |
| Duration of CI use (in months) at age 3.5 years Test Session | 19.76 | 7.64 | 7-32 | 76 | |
| Age at 4.5 Test (months) | 55.09 | 1.15 | 52-57 | 76 | |
| Duration of CI use (in months) at age 4.5 years Test Session | 31.95 | 7.85 | 18-45 | 76 |
Notes: HL = Hearing Level, HA = hearing aid, CI = cochlear implant, Hz = Hertz, PTA = Pure tone average threshold in the sound field at 500, 1000 and 2000 Hz. Maximum possible response level was 120 dB, HL for unaided and 80 dB, HL for aided threshold. When calculating averages, if “No Response” was indicated for a specific frequency on an audiogram, the value of “120” was entered if Unaided and “80” if Aided. Aided PTAs for 4 children were reported as a single figure by the audiologist, with no aided audiogram provided.
7 children wore a hearing aid on the contra-lateral ear at the age of 4.5 years
Table 2.
Configurations of implants, associated processors, and software.
| Device | Processor | Programming Strategy | Number of Children |
|---|---|---|---|
| Cochlear | Sprint | ACE | 38 |
| Cochlear | 3G | ACE | 5 |
| Cochlear | ESPrit | ACE | 3 |
| Cochlear | ESPrit | SPEAK | 1 |
| Advanced Bionics | PSP | SAS | 10 |
| Advanced Bionics | PSP | MPS | 5 |
| Advanced Bionics | PSP | HiRes-P | 5 |
| Advanced Bionics | PSP | CIS | 1 |
| Advanced Bionics | S-Series | CIS | 1 |
| Advanced Bionics | S-Series | SAS | 1 |
| Advanced Bionics | Auria | HiRes-P | 1 |
| Advanced Bionics | Platinum BTE | CIS | 1 |
| Advanced Bionics | Platinum BTE | MPS | 1 |
| Advanced Bionics | **S-Series & BTE | CIS | 2 |
| Med-El | Tempo+ | CIS | 1 |
At the time of testing, two participants were using both a body-worn (S-Series) and a BTE
Programming Strategies:
ACE = Advanced Combination Encoder
SPEAK = Spectral Peak
SAS = Simultaneous Analog Stimulation
MPS = Multi-Paired Stimulation
HiRes-P = High Resolution Paired
CIS = Continuous Interleaved Sampling
Processor Types:
BTE = Behind the Ear
PSP = Platinum Speech Processor
Pre-implant hearing and hearing aid use
Audiograms were provided directly from each child's audiological services provider or school audiological records. Additionally, several questions regarding pre- and post- implant hearing aid and CI use were included in both audiologist- and parent- questionnaires. All pre-implant unaided pure-tone averages were calculated using better ear responses at 500, 1000, and 2000 Hertz under earphones. Aided PTA thresholds at 500, 1000 and 2000 Hz were obtained in the sound field. Average threshold values are presented in Table 1, along with responses at each of the component frequencies. Aided thresholds were obtained at an average of 3 months (SD = 3, Range = 0 to 16 months) prior to CI surgery. Parents' report on hearing aid use prior to CI surgery indicated that 67% of the children in the study wore their hearing aids “Almost All Waking Hours”. The average aided PTA threshold was 62 dB HL (SD = 15.7, range = 32-80) for this group. Children who were reported to have worn their HAs less often had an average aided PTA of 70 (SD = 9.93, range = 48 - 80). Specific information about the type of hearing aid used was provided for 56/76 children. Only 6 of these children used digital aids with Wide Dynamic Range Compression. Aided thresholds may not accurately reflect audibility for children using compression hearing aids. However, because most of the children used linear amplification, audibility was accurately reflected in the mean aided PTA threshold. Measurements using real-ear systems were not reported for most of the children.
Demographics
Participants were recruited from 23 different U.S. states (18% Northeast, 16% Southeast, 20% Midwest, 5% Southwest, 11% West) as well as one Canadian province (6%). Host sites (and associated percentage of the sample) were: 14 private oral schools for the deaf (62%), four hospital-based implant programs (8%), three county child development centers (4%), four public schools (8%), and seven auditory-verbal therapy practices (18%). Administrators at each of these locations were asked to review their rosters for all children who met the criteria listed above. The parents of all children who met the criteria were given a letter describing the study and a release of information form to sign if they were interested in participating. A research team member then traveled to the child's school or therapy location and completed the data collection in that setting. Family socio-economic characteristics as well as the educational setting of the children are summarized in Table 3. The demographics of this sample are consistent with previously reported income and education levels for the families of CI recipients nationwide (Stern, Yueh, Lewis, Norton, & Sie, 2005; Eisenberg et al., 2006).
Table 3.
Percent of sample with various family demographic characteristics and child educational setting
| MOTHER'S LEVEL OF EDUCATION | TOTAL FAMILY INCOME | ||
|---|---|---|---|
| < High school graduation | 4 % | < $15,000 | 1 % |
| HS graduation | 14 % | $ 15,000 – 45,000 | 11 % |
| Some college or 2-Year Degree | 9 % | $ 45,000 – 75,000 | 24 % |
| 4-year college graduate | 62 % | $ > 75,000 | 33 % |
| Graduate school | 9 % | Did not provide information | 31 % |
| Did not provide information | 1 % | ||
| RACE / ETHNICITY | EDUCATIONAL SETTING FROM 3.5 TO 4.5 YEARS OF AGE | ||
| Asian | 3 % | Special Education Preschool | 82 % |
| Black / African American | 4 % | Regular (Mainstream) Preschool | 12 % |
| Hispanic | 1 % | At home with speech/language therapy | 6 % |
| White, not Hispanic | 75 % | ||
| Other or Multi-Ethnicity | 17 % | ||
Procedure
The following analysis was based on results of a parent-report instrument completed when the children were 3.5 years and again when they were 4.5 years of age (± 2 months) and two standardized language tests administered when they were 4.5 years old. All examiners had prior experience with testing young children
The MacArthur-Bates Communicative Development Inventories (MBCDI) – Words and Sentences (Fenson et al., 1993)
The Words and Sentences form was developed to facilitate estimation of the spoken vocabulary and early syntactic skills of 16-30 month-old toddlers with normal hearing but has been shown to be appropriate for older children with hearing loss, a CI, and delayed spoken language, as discussed above. Parent MBCDI reports were obtained when the children were 3.5 and again at 4.5 years of age (± 2 months of age), thereby allowing us to document change in expected outcomes with longer duration of CI use. The inventory is organized into four subscales: Vocabulary (productive), Irregular Words, Sentence Complexity, and 3 Longest Sentences. Standard instructions were provided to parents for completion of the MBCDI. Parents were asked to indicate their child's productive vocabulary from a list of 680 words organized into 22 semantic categories. The parent indicated the words they had heard their child produce spontaneously (i.e., not in imitation) to provide the score on the Vocabulary subscale. Use of syntax was indicated on a list of 37 examples of bound morphemes, function words and early-emerging complex sentence forms that were similarly based on the observed production, yielding scores for the Irregular Words as well as Sentence Complexity sub-scales. The 3 Longest Sentences score was estimated by having the parent provide examples of the three longest utterances that the child had recently produced.
Preschool Language Scale: Third Edition (PLS; Zimmerman, Steiner, & Pond, 1992)
This formal language test was administered by a trained research assistant at the child's school or speech-language therapy office at age 4.5 years (± 2 months). It consists of two subscales: Auditory Comprehension (AC) and Expressive Communication (EC). The test was standardized with a large (N = 1,200) normative sample of hearing children from birth through 6 years of age. The diversity of items provides a sampling of performance in several developmental areas in a relatively short time (20-30 minutes). The test was administered using spoken language with no deviations from standard administration procedures. In the current study, results were expressed as standard scores (mean = 100; SD = 15) for Auditory Comprehension and Expressive Communication in relation to hearing children between 4;0 - 4;5 (years; months) or 4:6 – 4;11 years of age, depending upon exact age at test, which ranged from 4;4 to 4;8. Because only standard scores were used and reported and do not differ substantially as new versions of the test are developed (Zimmerman, Steiner & Pond, 1992) interpretation of standard scores from the PLS – 4 are also applicable. A second research assistant re-scored 20% of the videotapes of the Expressive Communication portion as a check on inter-scorer reliability. This procedure resulted in point-by-point scoring agreement average of 94% for each individual test item.
Peabody Picture Vocabulary Test-III (PPVT; Dunn & Dunn, 1997)
This measure of receptive vocabulary was administered by a trained research assistant when the children were 4.5 years old (± 2 months). The test involves presentation of a picture to elicit a pointing response; no verbal response is required. Standard scores were developed with a large (N = 2,725) carefully-selected normative sample of typically-developing children. Each child was tested only on the vocabulary appropriate for his or her age and language development. Test administration used spoken language only. Scores are expressed as standard scores (mean = 100; SD = 15) in relation to hearing children between 4;4 and 4;9 years of age.
Results
Validation of Language Measures
To first aim was to establish the degree of predictive and concurrent validity among the language measures. Correlations were calculated between scores derived from MBCDI checklists and scores on the PLS and the PPVT at 4.5 years of age. Correlations summarized in Table 4 indicated a moderate to high degree of consistency among the three language assessment techniques. On the MBCDI, vocabulary size, use of irregular words, sentence complexity, and longest sentence length were all highly associated with one another. Further, MBCDI scores at age 3.5 years were compared with results obtained on the PLS and the PPVT at 4.5 years of age. These MBCDI scores, derived from parent checklists, were highly predictive of formal language test results at 4.5 years of age. Note that the alpha level was set, a priori, at p < .01 to account for multiple comparisons. Results indicated that similar estimates of language level could be obtained from either parent-completed checklists or from formal language tests. In a number of cases, predictive validity coefficients actually exceeded concurrent validity because of a tendency for scores on some MBCDI sub-scales to reach ceiling at age 4.5 years. The next issue concerned the performance level to be anticipated for an individual child in relation to the duration of accumulated experience with a CI.
Table 4.
Inter-correlations related to concurrent and predictive reliability of the MacArthur-Bates Communicative Development Inventory (MBCDI: Words and Sentences form.
| Score | M/V 4.5 | M/I 4.5 | M/SC 4.5 | M/3L 4.5 | PLS/AC | PLS/EC | PPVT-III |
|---|---|---|---|---|---|---|---|
| CONCURRENT VALIDITY | |||||||
| M/V 4.5 | - | .820
(74) |
.865
(74) |
.496
(74) |
.728
(74) |
.718
(74) |
.813
(73) |
| M/I 4.5 | - | .853
(74) |
.508
(74) |
.672
(74) |
.728
(74) |
.708
(73) |
|
| M/SC 4.5 | - | .534
(74) |
.670
(74) |
.706
(74) |
.753
(73) |
||
| M/3L 4.5 | - | .433
(74) |
.471
(74) |
.506
(73) |
|||
| PREDICTIVE VALIDITY | |||||||
| M/V 3.5
N= 75 |
.731
(75) |
.800
(75) |
.757
(74) |
||||
| M/I 3.5
N = 75 |
.590
(75) |
.685
(75) |
.580
(74) |
||||
| M/SC 3.5
N= 75 |
.629
(75) |
.801
(75) |
.632
(74) |
||||
| M/3L 3.5
N= 75 |
.617
(75) |
.689
(75) |
.589
(74) |
||||
Notes: All correlations are significant at p < .01
Parentheses indicate number of children for whom both data points were available for correlation
M/V = MBCDI Vocabulary subscale
M/I = MBCDI Irregular Words subscale
M/SC = MBCDI Sentence Complexity subscale
M/3L = MBCDI - Three Longest Sentences subscale
PLS/AC = Preschool Language Scale-III – Auditory Comprehension scale
PLS/EC = Preschool Language Scale-III – Expressive Communication scale
PPVT-III = Peabody Picture Vocabulary Test – 3rd edition
3.5 = Test age 3;4 to 3;8 (Years;months)
4.5 = Test age 4;4 to 4;8
Age at Implantation Effects
The second aim was to determine whether the current data were consistent with our earlier finding (Nicholas & Geers, 2006b; Nicholas & Geers, 2007) that language scores increase with decreasing pre-implant aided thresholds and longer duration of CI use (i.e., younger age at implant). Tables 5, 6, and 7 summarize results of a set of regression analyses that examined the linear relation between language test scores and age at cochlear implantation along with the effects of pre-implant aided residual hearing for test ages 3.5 and 4.5 years. In addition, the increment in those relations explained by looking at the quadratic component (i.e. change in the linear relation with increasing age at implant) was also documented. For all language measures there was a significant linear decrease in language scores with increasing age at cochlear implantation and increasing pre-implant aided threshold. The quadratic component was only significant for the following measures: MBCDI Irregular Words at 3.5, MBCDI Sentence Complexity at 3.5 years (Table 3), and PLS Expressive Language at 4.5 years (in Table 5). In all of these instances, the linear relation leveled off for children who received a CI at relatively older ages. Tables 5-7 report both linear and quadratic analyses, adopting an approach that uses the same model for examining all outcome variables. Consequently, for some analyses, quadratic effects are included that are not significant for that outcome. We believe that it is easier to make comparisons across outcomes when all have been analyzed using the same statistical model. Note that the analyses are reported in two steps. The first step is the linear model, which is more appropriate in those cases where the quadratic effect is not significant.
Table 5.
Results of linear and quadratic regression analyses for parent MBCDI subscales from chronologic Test Age 3.5
| Step 1 – Linear Regression | Step 2 – Quadratic Regression | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Test/Subscale | Parameter | Regression Coefficient (β) | Standard Error | Semi-Partial r2 | Step Increment in R2 | Regression Coefficient (β) | Standard Error | Semi-Partial r2 | Step Increment in R2 |
| MBCDI Vocabulary RS | .460 | .016 | |||||||
| Intercept | 1065.209 | 106.998 | 1284.605 | 184.911 | |||||
| Pre-CI Aided | -4.749*** | 1.164 | .125 | -4.633*** | 1.158 | .118 | |||
| Age at CI | -17.201*** | 2.225 | .448 | -38.320** | 14.738 | .050 | |||
| (Age at CI)2 | - | - | .441 | .304 | .016 | ||||
| MBCDI Irregular Words RS | .328 | .075 | |||||||
| Intercept | 26.008 | 4.516 | 44.281 | 7.462 | |||||
| Pre-CI Aided | -.102* | .049 | .040 | -.092 | .047 | .032 | |||
| Age at CI | -.557*** | .094 | .328 | -2.316*** | .595 | .127 | |||
| (Age at CI)2 | - | - | .037** | .012 | .075 | ||||
| MBCDI Sentence Complexity RS | .389 | .036 | |||||||
| Intercept | 48.341 | 7.453 | 70.348 | 12.673 | |||||
| Pre-CI Aided | -.172* | .081 | .038 | -.160* | .079 | .033 | |||
| Age at CI | -1.047*** | .155 | .387 | -3.166** | 1.010 | .080 | |||
| (Age at CI)2 | - | - | .044* | .021 | .036 | ||||
| MBCDI 3 Longest Sentences RS | .313 | .035 | |||||||
| Intercept | 16.189 | 2.290 | 22.466 | 3.912 | |||||
| Pre-CI Aided | -.078** | .025 | .093 | -.075** | .024 | .085 | |||
| Age at CI | -.268*** | .048 | .302 | -.872** | .312 | .072 | |||
| (Age at CI)2 | - | - | .013 | .006 | .035 | ||||
p ≤ .001
p ≤ .01
p ≤ .05
Note: Squared semi-partial correlations can sum to greater than the squared multiple correlation under conditions of suppression. This occurs when the effect of a predictor is suppressed by another predictor and is only revealed when the other predictor is partialled. CI = Cochlear Implant, RS = Raw Score
Table 6.
Results of linear and quadratic regression analyses for MBCDI subscales from chronologic Test Age 4.5
| Step 1 – Linear Regression | Step 2 – Quadratic Regression | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Test/Subscale | Parameter | Regression Coefficient (β) | Standard Error | Semi-Partial r2 | Step Increment in R2 | Regression Coefficient (β) | Standard Error | Semi-Partial r2 | Step Increment in R2 |
| MBCDI Vocabulary RS | .441 | .001 | |||||||
| Intercept | 1183.699 | 94.994 | 1138.906 | 168.593 | |||||
| Pre-CI Aided | -5.378*** | 1.029 | .215 | -.401*** | 1.038 | .215 | |||
| Age at CI | -13.614*** | 1.960 | .379 | -9.351 | 13.363 | .004 | |||
| (Age at CI)2 | - | - | - | - | -.088 | .273 | .001 | ||
| MBCDI Irregular Words RS | .372 | .004 | |||||||
| Intercept | 44.290 | 5.160 | 49.383 | 9.135 | |||||
| Pre-CI Aided | -.252*** | .056 | .180 | .249*** | .056 | .175 | |||
| Age at CI | -.642*** | .106 | .321 | -1.126 | .724 | .022 | |||
| (Age at CI)2 | - | - | - | .010 | .015 | .004 | |||
| MBCDI Sentence Complexity RS | .479 | .001 | |||||||
| Intercept | 78.834 | 7.417 | 82.598 | 13.162 | |||||
| Pre-CI Aided | -.429*** | .080 | .209 | -.426*** | .081 | .205 | |||
| Age at CI | -1.170*** | .153 | .429 | -1.529 | 1.043 | .016 | |||
| (Age at CI)2 | - | - | - | - | .007 | .021 | .001 | ||
| MBCDI 3 Longest Sentences RS | .178 | <.001 | |||||||
| Intercept | 19.051 | 3.423 | 19.215 | 6.08 | |||||
| Pre-CI Aided | -.084* | .037 | .060 | -.084* | .037 | .059 | |||
| Age at CI | -.269*** | .071 | .169 | -.285 | .482 | .004 | |||
| (Age at CI)2 | - | - | - | - | .000 | .010 | <.001 | ||
p ≤ .001
p ≤ .01
p ≤ .05
Note: Squared semi-partial correlations can sum to greater than the squared multiple correlation under conditions of suppression. This occurs when the effect of a predictor is suppressed by another predictor and is only revealed when the other predictor is partialled. CI = Cochlear Implant, RS = Raw Score
Table 7.
Results of linear and quadratic regression analyses for PLS and PPVT at chronologic Test Age 4.5 years
| Step 1 – Linear Regression | Step 2 – Quadratic Regression | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Test/Subscale | Parameter | Regression Coefficient (β) | Standard Error | Semi-Partial r2 | Step Increment in R2 | Regression Coefficient (β) | Standard Error | Semi-Partial r2 | Step Increment in R2 |
| PLS Auditory Comprehension | .337 | .016 | |||||||
| Intercept | 152.868 | 12.495 | 176.297 | 21.703 | |||||
| Pre-CI Aided | -.574*** | .136 | .161 | -.563*** | .136 | .154 | |||
| Age at CI | -1.456*** | .257 | .292 | -3.700* | 1.723 | .042 | |||
| (Age at CI)2 | - | - | .047 | .035 | .016 | ||||
| PLS Expressive Communication | .361 | .050 | |||||||
| Intercept | 151.082 | 13.812 | 198.187 | 23.314 | |||||
| Pre-CI Aided | -.521*** | .151 | .104 | -.498*** | .146 | .095 | |||
| Age at CI | -1.794*** | .284 | .349 | -6.305*** | 1.851 | .095 | |||
| (Age at CI)2 | - | - | .094* | .038 | .050 | ||||
| PPVT | .363 | .002 | |||||||
| Intercept | 158.664 | 12.406 | 167.900 | 21.740 | |||||
| Pre-CI Aided | -.607*** | .135 | .178 | -.602*** | .136 | .174 | |||
| Age at CI | -1.511*** | .254 | .312 | -2.402 | 1.735 | .017 | |||
| (Age at CI)2 | - | - | .019 | .036 | .002 | ||||
p ≤ .001
p ≤ .01
p ≤ .05
Note: Squared semi-partial correlations can sum to greater than the squared multiple correlation under conditions of suppression. This occurs when the effect of a predictor is suppressed by another predictor and is only revealed when the other predictor is partialled. CI = Cochlear Implant, RS = Raw Score
In each regression model listed in Tables 5-7, the squared semi-partial correlations for Age at CI and Pre-CI Aided Threshold represent the proportion of variance in the outcome variable that is accounted for by a given predictor after partialling or removing the variance accounted for by the other predictor from the outcome variable. Close inspection reveals that these sum to a value greater than the squared multiple correlation. In each case, the standardized regression coefficients are also larger than the simple correlations between predictors and outcome. These analysis features indicate the presence of suppression (see Cohen & Cohen, 1983), which occurs when the simple relations between predictors and outcome are hidden or suppressed because of the relations between predictors. For example, the underlying analyses performed to allow for the creation of Table 6 revealed that both Age at CI (r = -.48) and Pre-CI Aided Threshold (r = -.25) are negatively related to the outcome, MBCDI Vocabulary raw score (RS), but are also negatively related to each other (r = -.38). That latter negative relation in part hides the relationship that each can have with the outcome variable. When each predictor is partialled from the other, the full and unsuppressed relation emerges, evident in this case by standardized regression coefficients that are larger in magnitude than the simple relations: Age at CI and MBCDI Vocabulary RS (β= -.67); Pre-CI Aided Threshold and MBCDI Vocabulary RS (β = -.50).
Expected Scores at Given Cochlear Implantation Ages
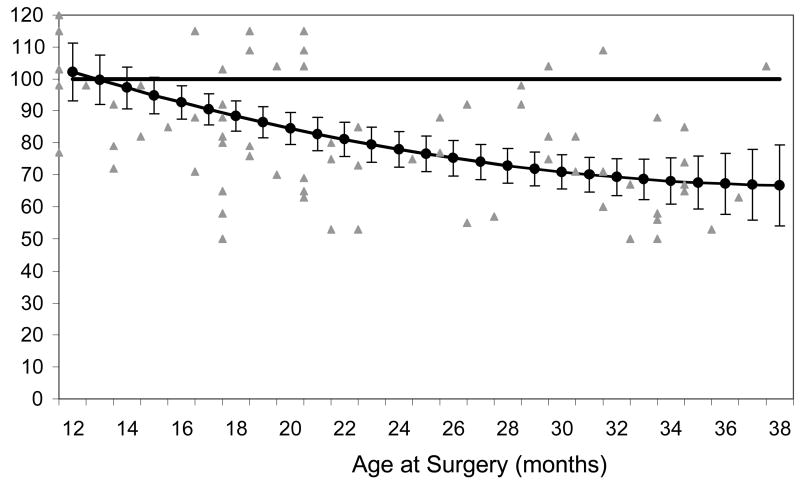
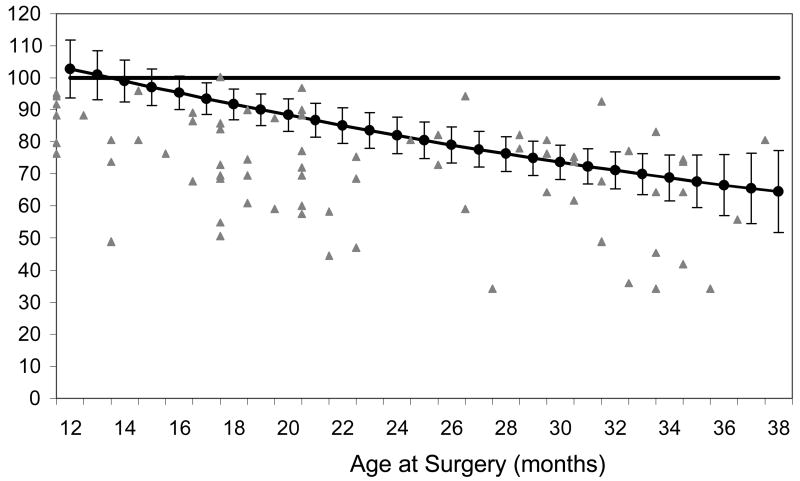
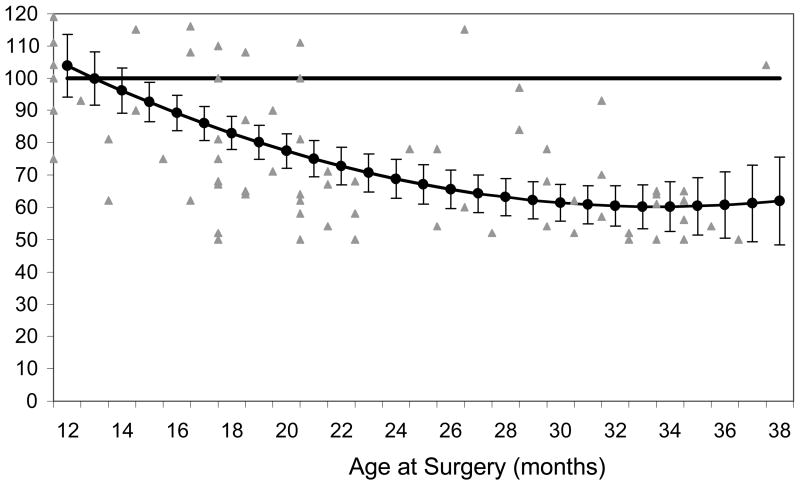
Further, we sought to obtain expected values on each language measure as a function of predictor variables. The quadratic analysis was used to establish an expected language score at each age of implantation when pre-implant aided PTA threshold at 500, 1000, and 2000 Hertz was set at the sample mean (which was 65 dB). To the extent that the relation between implant age and language score deviates from a strictly linear one, the quadratic analysis resulted in the most accurate estimate. The reader should refer back to the regression results in Tables (5-7) for significance of linear and quadratic effects for each outcome. Figures 1-3 are plots of the expected mean scores on the PLS and PPVT tests for any given age at implantation (or duration of use, given a test age of 4.5 years). Each expected score has an associated prediction interval. The size of the prediction interval is related to the amount of variance in the linear model accounted for by age at implantation and pre-implant aided threshold. The prediction interval describes the range over which an individual's score (with a specified age at implant and average aided threshold) would be located with approximately 68% confidence. Note that these prediction intervals are wider than commonly reported “confidence intervals” because they represent confidence around an individual score as opposed to a mean score. These prediction intervals should not be confused with standard deviation units.
Figure 1.
Regression lines for PLS Auditory Comprehension subtest standard score by age at cochlear implantation (chronologic age at testing = 4.5 years). Note that expected scores are corrected for pre-implant aided hearing thresholds. Horizontal black line at 100 represents the average score of typically-developing, hearing children at the same chronologic age at test.
Figure 3.
Regression line for Peabody Picture Vocabulary Test standard scores by age at cochlear implantation (chronologic age at testing = 4.5 years). Note that expected scores are corrected for pre-implant aided hearing thresholds. Horizontal black line at 100 represents the average score of typically-developing, hearing children at the same chronologic age at test.
Interpretation of Expected Scores
The same mean scores and associated prediction intervals are presented in tabular form in Appendices A1-4. They represent predicted values from regression models in which pre-CI aided thresholds were set equal to the sample mean and age at implantation was specified for values between 12 and 38 months. All predictions were based on models that included linear and quadratic effects for age at implantation. The quadratic effect was not statistically significant in every model but its inclusion in the generation of the expected scores provides consistency in the prediction models. Moreover, models including the quadratic terms provided more accurate predictions to the extent that the quadratic component accounts for variability in the outcome measure, even when that component does not reach a traditional level of statistical significance.
Preschool Language Scale
Figure 1 shows an expected mean Auditory Comprehension (AC) standard score for 4.5 year old children ranging from 67 for an implant age of 36-38 months to 102 for age at implant of 12 months. The expected score reached the average range for hearing age-mates (85 or higher) at 34 months of implant use (age at implant = 20 months). Similar results are depicted in Figure 2 for the Expressive Communication (EC) subscale. Expected mean EC scores ranged from a low of 60 for children implanted at 32-35 months of age to 104 for those implanted at 12 months of age. Expected scores within the prediction interval reached the average range (85 or higher) when children were implanted by 13 months of age. Similarly, an individual tested on the PLS at 4.5 years of age would be expected to achieve age-appropriate AC and EC scores if they received a CI by about 13 months of age. Expected scores for each implant age are provided in tabular form in Appendix A1, along with the associated prediction intervals.
Figure 2.
Regression line for PLS Expressive Communication subscale standard score by age at cochlear implantation (chronologic age at testing = 4.5 years). Note that expected scores are corrected for pre-implant aided hearing thresholds. Horizontal black line at 100 represents the average score of typically-developing, hearing children at the same chronologic age at test.
Peabody Picture Vocabulary Test
Figure 3 summarizes expected vocabulary standard scores by age at CI surgery Expected mean scores ranged from 64 for children implanted at 38 months of age to 103 for children implanted at 12 months. These results are summarized in Tabular form in Appendix A2. Children implanted by 12-13 months of age with a pre-CI aided threshold of about 65 dB can be expected to achieve age-appropriate vocabulary quotient scores on the PPVT by the time they are 4.5 years old.
MacArthur Communicative Development Inventory
Expected scores on the MBCDI are presented in Appendix A3 for test age 3.5 years and Appendix A4 for test age 4.5 years. Separate results are presented for each subscale: Vocabulary, Irregular Words, Sentence Complexity, and Three Longest Sentences.
Discussion
Consistency of Language Outcome Measures
These results indicate convergence of language level estimates obtained using a variety of instruments and techniques. At 4.5 years of age, children with CIs exhibited similar language levels on a parent report checklist (MBCDI), a comprehensive language measure (the PLS), and a specific receptive vocabulary test (PPVT). This result is consistent with the findings of Thal, DesJardin, & Eisenberger (2007) and Stallings, Gao, & Svirsky (2002) who also found good validity for the MBCDI. Furthermore, scores obtained via the parent checklist completed at child's age 3.5 years predicted performance on a language assessment one year later. It is tempting to conclude from these results that completion of a parent inventory is sufficient for tracking language development. However the complementary information obtained by including both observational ratings and formal language testing is extremely valuable. A child's response to specific language tasks that comprise a formal assessment is useful for planning intervention. Furthermore, standard scores derived from testing permit monitoring a child's progress in relation to a large normative sample of hearing children. It should also be noted that the parents providing MBCDI reports in this study were relatively well-educated and had participated in education programs following their child's diagnosis of deafness. As a result, these parents might have completed the forms in a manner that was more reliable and thus better correlated with clinician-administered language tests than would be expected from the general population.
Accounting for Variance in Language Outcome Scores
It should be noted here that we did consider the potential effect of gender, mother's education level, type of therapy setting, whether or not the CI technology is considered up-to-date in 2007, and whether the education/therapy services were provided in a private vs. public setting in the models presented in Tables 5-7. We explored these potentially important explanatory variables in the present study by also analyzing the data in two additional ways: (a) with these variables entered as separate co-variates and (b) using “propensity scores” (see Connor et al., 2006). The result was that neither procedure added additional explained variance and with neither method did the influence of the predictor variables that we had originally identified (pre-CI aided thresholds and duration of use) change or diminish. Approximately one-third of our sample declined to provide income information, therefore that variable was not available for analysis. That these factors were not found to be significant predictors in the present study may be due to the homogeneous nature of this sample (80% in private oral schools or Auditory-Verbal Therapy, all 4 years old, all implanted by 3 years of age, all used relatively recent CI technology).
In contrast, significant amounts of variance were explained by degree of aided residual hearing before receiving a CI and age at implantation (i.e., duration of CI experience). Together the latter two factors accounted for 18 - 48% of the variance in language outcome, depending upon the particular outcome measure. The significant contribution of these factors to language outcomes reflects the importance of two recent trends in pediatric cochlear implantation: a reduction in CI candidacy age to 12 months and an expansion of the hearing loss criterion into the severe range. These results confirm our previous findings (Nicholas & Geers, 2006b) suggesting that enriched auditory experience in infancy, whether provided with hearing aids or CIs, is an essential ingredient for promoting age-appropriate spoken language acquisition during the preschool years.
The use of aided PTA thresholds provides only partial information about pre-implant residual hearing. The clinics that submitted pre-CI hearing aid data did not report real-ear measures and resulting speech intelligibility indices. Given the period in which most of these hearing aids were fitted (1997-2002) and the severity of the hearing losses represented, most children used linear rather than compression hearing aids. Although aided thresholds may overestimate the audibility of typical conversational speech inputs (especially for compression aids) they provide an estimate of audibility across the frequency range that is important for speech. Therefore, the lower the aided threshold obtained, the better the opportunity to hear the acoustic cues of soft speech (e.g., soft-level consonants that are important for speech understanding).
Using “Benchmark” Tables for Assessing Spoken Language Progress
Tables in the Appendix provide an expected mean score for each implantation age along with a range of values within which the expected score is likely to fall. Clinicians may use these tables to estimate the degree to which an individual child is making expected progress with a CI in relation to the sample described in this article. Children scoring within the expected range for implantation age may be considered “on track” in relation to a group of children who have experienced early oral intervention with an emphasis on auditory and speech development.
The values in Appendices A1-4 should not be considered normative for all children with CIs for several reasons. First, stratified randomization was not used in sample selection so that geographic location, family, child, and educational program characteristics may not be representative of the larger population of children with CIs. Second, children enrolled in programs based on Total Communication or American Sign Language were not included in this study. Finally, the number of children at each individual month of implantation age is relatively small. Nevertheless, these tables may allow clinicians in oral education settings to estimate whether a 3- or 4-year-old child is making expected progress in spoken language for his/her age at implant and duration of use. Because results are depicted for an average pre-CI aided threshold, the expectation would be somewhat higher for children with better pre-CI hearing and somewhat lower for children with poorer pre-CI hearing. This point is illustrated by examining the raw data plotted in Figures 1-3. For example, some children with relatively older ages at implantation (30+ months) scored unexpectedly well, probably due to better than average pre-implant aided hearing ability.
Additionally, these estimates are only accurate to the extent that the individual child meets the criteria of the sample used in this analysis. The following is a list of those factors along with the hypothesized impact (positive or negative) on projected language outcome scores based on the current literature. These tables are most accurate for children who:
are within 2 months of the specified test age (either 3.5 or 4.5 years): Increasing age at test should have a positive impact on scores to the extent that chronologic age is associated with increased CI experience.
have been deaf since birth: A period of normal hearing or relatively better hearing before the onset of profound hearing loss has been shown to positively affect language scores, especially if the period of profound deafness was less than one year prior to cochlear implantation (Geers, 2004a; Sarant, Blamey, Dowell, Clark & Gibson, 2001).
have been enrolled in an oral education setting since the time of implantation. The literature on this point shows mixed findings. Educational settings that include a sign language emphasis may negatively affect spoken language scores (Svirsky, Robbins, Kirk, Pisoni & Miyamoto, 2000; Geers, Nicholas & Sedey, 2003; Geers, 2004b). On the other hand, including sign along with speech has been associated with higher vocabulary scores in some samples (Connor et al., 2000) and with no difference in post-CI vocabulary scores in other samples (Connor & Zwolan, 2004). Although this study does not include children with sign language backgrounds and therefore does not demonstrate validity of the MBCDI for use with those children, a clinician may nonetheless choose to utilize the MBCDI to monitor a child's progress in spoken language development, noting strengths and weaknesses in the child's acquisition of spoken vocabulary, grammar and sentence length with or without reference to the Appendices.
have pre-CI aided thresholds of 65 dB HL. With better pre-CI aided thresholds, language scores have been shown to increase (Eisenberg, Kirk, Martinez, Ying & Miyamoto, 2004; Nicholas & Geers, 2006b). Therefore, language score expectations might be somewhat higher for children with pre-CI aided thresholds that are better (i.e., lower) than 65 dB, HL and somewhat lower for those with poor (i.e., greater) thresholds.
use a generation of CI technology similar to that of the children in this sample (see Table 2). The CI technology utilized by most of the children in the present study is considered “current” or “up-to-date” at the time of this publication. Our analyses revealed that whether or not the technology was the most current (in 2007) did not have a significant influence on the outcome scores. There are features on newer processors which may directly affect speech perception abilities but further research would be needed to determine whether these and future changes in hardware or software would result in different expected scores.
were without an interruption of implant use lasting more than 30 days. Technical problems with CI hardware or speech processor mapping may be expected to negatively affect spoken language scores (Nicholas, Geers & Sedey, 2003) but so few children in this study experienced CI problems that this was impossible to assess.
have nonverbal intelligence (or motor development) at least in the average range and no other medical or developmental conditions that might be expected to interfere with communication. Measured nonverbal intelligence scores are positively associated with language outcome (Holt & Kirk, 2005; Geers, Nicholas & Sedey, 2003).
live in middle to upper-middle class households (see Table 3). The majority of children in our sample (71%) were part of families in which the mother had a college degree. While this may not be representative of the maternal education of children who are deaf in general, it may indeed be representative of the educational levels found in families of children who have received a CI. Fortnum, Stacey & Summerfield (2006) reported that children with CIs tend to come from families who were more affluent, more likely to use spoken language at home, and were more likely to provide an educational environment for their child which utilized spoken language only, in comparison with deaf peers who did not use a CI. Post-CI language levels in children are reported to be positively affected by parent education and income (Geers, Nicholas & Sedey, 2003). The fact that mother's education level was not related to language outcome in this sample may have resulted from the restricted range of education levels represented. Children from lower SES families might not be expected to acquire language at the levels reported here.
live in a household in which English is the only language spoken to the child. The effects of using a second language on the acquisition of spoken English following cochlear implantation have not been thoroughly documented. Results from a small sample of children in bilingual families who received their CI by age 3 years indicated that the primary language continued to develop at normal rates (Robbins, Green & Waltzman, 2004). However, to the extent that the child's exposure to spoken English input is reduced, one might expect slower progress.
A final caveat is that decisions about whether or not a child is progressing appropriately should always be made with as many sources of objective information as possible. In addition to modifications based on the degree to which the child shares characteristics of this sample, decisions utilizing the information provided here should also include a host of other observation/testing information. The goal is to gain a comprehensive view of language (form, content, use) and to gain information to guide education/intervention. Use of only the MBCDI or a single language test would give an overly narrow view of language, particularly at ages 4 and 5 years, when narrative skills and verbal reasoning may be important predictors of mainstream success. Clinicians/educators should use these benchmarks as augmenting material, and not be tempted to substitute this procedure for a complete assessment. Similarly, use of these benchmarks would not be appropriate for inclusion in a formal report on a child's language progress. As Thal et al. (2007) have noted, however, the MBCDI may also be useful in highlighting the strengths and weaknesses in the developing spoken language abilities of this population of children.
Directions for Future Research
It remains an empirical question if standard scores within normal limits on these measures at age 4.5 years are predictive of maintenance of language within normal limits and/or success in the mainstream. This is an important avenue for future research. The challenges of spoken language development at age 4.5 years may be qualitatively different than the challenges in the upcoming elementary school years. These include the acquisition of subject-matter vocabulary, verbal reasoning, literacy and narrative skills, as well as complex syntactic, grammatical, and non-literal language competencies.
Further research is needed to determine whether different scores would be expected from children who use a contra-lateral hearing aid or who have bilateral implantation, features that were not sufficiently represented in this sample for analysis. The significant positive effect of degree of aided residual hearing on language outcome in this study is consistent with positive speech perception findings from severely hearing impaired children who continued using hearing aids in their non-implanted ears (Holt, Kirk, Eisenberg, Martinez & Campbell, 2005).
Conclusions
Scores listed in the Appendices of this paper can allow the clinician to determine how closely children with early cochlear implantation approximate estimated benchmarks of spoken language development. They have the potential to be useful in tracking within-child progress and making mainstreaming decisions in conjunction with other information. While variability in spoken language outcomes remains high, for families seeking mainstream placement, these data can be considered as benchmarks associated with early oral education and cochlear implantation by a child's third birthday.
Acknowledgments
This study was supported by a grant from the National Institute on Deafness and Other Communication Disorders. Special thanks to Sarah Fessenden, Melissa Truesdell, Sallie Shiel van der Hoof, and Chris Brenner for assistance with testing and data management and to Michael Strube for statistical expertise. We also thank the families, schools, audiologists, and therapy centers across the country that participated in, or facilitated participation in, this study.
Appendix A1: Expected Standard Scores on Preschool Language Scales (PLS) by Age at Implantation
Chronologic Age at Test = 4 years, 6 months (± 2 months).
| Expressive Communication
(EC) Scale – Standard Score |
Auditory Comprehension
(AC) Scale – Standard Score |
||||
|---|---|---|---|---|---|
| Age at implant (in months) | Duration of Use | Expected Standard Score | 68% Prediction Interval | Expected Standard Score | 68% Prediction Interval |
| 12 | 42 | 104 | 86-122 | 102 | 86-119 |
| 13 | 41 | 100 | 82-118 | 100 | 83-116 |
| 14 | 40 | 96 | 79-114 | 97 | 81-114 |
| 15 | 39 | 93 | 75-110 | 95 | 79-111 |
| 16 | 38 | 89 | 72-107 | 93 | 77-109 |
| 17 | 37 | 86 | 69-103 | 91 | 74-107 |
| 18 | 36 | 83 | 66-100 | 88 | 72-105 |
| 19 | 35 | 80 | 63-97 | 86 | 70-103 |
| 20 | 34 | 77 | 60-95 | 85 | 68-101 |
| 21 | 33 | 75 | 58-92 | 83 | 67-99 |
| 22 | 32 | 73 | 55-90 | 81 | 65-97 |
| 23 | 31 | 71 | 53-88 | 80 | 63-96 |
| 24 | 30 | 69 | 51-86 | 78 | 62-94 |
| 25 | 29 | 67 | 50-84 | 77 | 60-93 |
| 26 | 28 | 66 | 48-83 | 75 | 59-91 |
| 27 | 27 | 64 | 47-82 | 74 | 58-90 |
| 28 | 26 | 63 | 46-80 | 73 | 57-89 |
| 29 | 25 | 62 | 45-79 | 72 | 56-88 |
| 30 | 24 | 61 | 44-79 | 71 | 55-87 |
| 31 | 23 | 61 | 43-78 | 70 | 54-86 |
| 32 | 22 | 60 | 43-78 | 69 | 53-86 |
| 33 | 21 | 60 | 48-78 | 69 | 52-85 |
| 34 | 20 | 60 | 43-78 | 68 | 52-84 |
| 35 | 19 | 60 | 43-78 | 68 | 51-84 |
| 36 | 18 | 61 | 43-79 | 67 | 51-84 |
| 37 | 17 | 61 | 43-79 | 67 | 50-84 |
| 38 | 16 | 62 | 43-80 | 67 | 50-84 |
Appendix A2: Expected Standard Scores on Peabody Picture Vocabulary Test (PPVT-III) by Age at Implantation
Chronologic Age at Test = 4 years, 6 months (± 2 months).
| Age at Implant (in months) | Duration of Use | Expected Standard Score at Age 4.5 | 68% Prediction Interval |
|---|---|---|---|
| 12 | 42 | 103 | 86-119 |
| 13 | 41 | 101 | 84-117 |
| 14 | 40 | 99 | 83-115 |
| 15 | 39 | 97 | 81-113 |
| 16 | 38 | 95 | 79-111 |
| 17 | 37 | 94 | 77-110 |
| 18 | 36 | 92 | 76-108 |
| 19 | 35 | 90 | 74-106 |
| 20 | 34 | 88 | 72-105 |
| 21 | 33 | 87 | 71-103 |
| 22 | 32 | 85 | 69-101 |
| 23 | 31 | 84 | 67-100 |
| 24 | 30 | 82 | 66-98 |
| 25 | 29 | 81 | 64-97 |
| 26 | 28 | 79 | 63-95 |
| 27 | 27 | 78 | 61-94 |
| 28 | 26 | 76 | 60-92 |
| 29 | 25 | 75 | 59-91 |
| 30 | 24 | 74 | 57-90 |
| 31 | 23 | 72 | 56-89 |
| 32 | 22 | 71 | 55-87 |
| 33 | 21 | 70 | 54-86 |
| 34 | 20 | 69 | 52-85 |
| 34 | 19 | 68 | 51-84 |
| 36 | 18 | 67 | 50-83 |
| 37 | 17 | 65 | 49-82 |
| 38 | 16 | 64 | 47-82 |
Appendix A3: Expected Raw Scores on MacArthur-Bates Communicative Development Inventory (MBCDI) by Age at Implantation
Chronologic Age at Test = 3 years, 6 months (± 2 months).
|
Vocabulary Scale
Raw Score |
Irregular Words Scale
Raw Score |
||||
|---|---|---|---|---|---|
| Age at Implant (in months) | Duration of Use | Expected Raw Score * | 68% Prediction Interval | Expected Raw Score | 68% Prediction Interval |
| 12 | 30 | 589 | 448 + | 16 | 10-22 |
| 13 | 29 | 562 | 422 + | 14 | 9-20 |
| 14 | 28 | 535 | 396 + | 13 | 8-19 |
| 15 | 27 | 510 | 372 + | 12 | 6-17 |
| 16 | 26 | 485 | 347-623 | 11 | 5-16 |
| 17 | 25 | 461 | 324-599 | 10 | 4-15 |
| 18 | 24 | 438 | 301-576 | 9 | 3-14 |
| 19 | 23 | 416 | 279-554 | 8 | 2-13 |
| 20 | 22 | 395 | 258-533 | 7 | 1-12 |
| 21 | 21 | 375 | 237-513 | 6 | 0-11 |
| 22 | 20 | 356 | 218-493 | 5 | 0-11 |
| 23 | 19 | 337 | 199-475 | 5 | 0-10 |
| 24 | 18 | 320 | 182-457 | 4 | 0-9 |
| 25 | 17 | 303 | 165-441 | 3 | 0-9 |
| 26 | 16 | 287 | 149-425 | 3 | 0-9 |
| 27 | 15 | 272 | 134-410 | 3 | 0-8 |
| 28 | 14 | 258 | 120-396 | 2 | 0-8 |
| 29 | 13 | 245 | 107-383 | 2 | 0-8 |
| 30 | 12 | 232 | 95-370 | 2 | 0-7 |
| 31 | 11 | 221 | 83-359 | 2 | 0-7 |
| 32 | 10 | 210 | 72-349 | 2 | 0-7 |
| 33 | 9 | 201 | 62-340 | 2 | 0-8 |
| 34 | 8 | 192 | 53-332 | 2 | 0-8 |
| 35 | 7 | 184 | 44-325 | 2 | 0-8 |
| 36 | 6 | 177 | 35-319 | 3 | 0-8 |
| 37 | 5 | 171 | 27-315 | 3 | 0-9 |
| 38 | 4 | 166 | 19-313 | 3 | 0-9 |
|
Sentence Complexity Scale
Raw Score |
3 Longest Sentences Scale
Raw Score |
||||
| Age at Implant (in months) | Duration of Use | Expected Raw Score * | 68% Prediction Interval | Expected Raw Score | 68% Prediction Interval |
| 12 | 30 | 28 | 19 + | 9 | 6-12 |
| 13 | 29 | 26 | 17 + | 8 | 5-11 |
| 14 | 28 | 24 | 15-34 | 8 | 5-11 |
| 15 | 27 | 22 | 13-32 | 7 | 4-10 |
| 16 | 26 | 21 | 11-30 | 7 | 4-10 |
| 17 | 25 | 19 | 10-28 | 6 | 4-9 |
| 18 | 24 | 17 | 8-27 | 6 | 3-9 |
| 19 | 23 | 16 | 6-25 | 6 | 3-9 |
| 20 | 22 | 14 | 5-24 | 5 | 2-8 |
| 21 | 21 | 13 | 4-22 | 5 | 2-8 |
| 22 | 20 | 12 | 2-21 | 5 | 2-7 |
| 23 | 19 | 11 | 1-20 | 4 | 1-7 |
| 24 | 18 | 10 | 0-19 | 4 | 1-7 |
| 25 | 17 | 9 | 0-18 | 4 | 1-7 |
| 26 | 16 | 8 | 0-17 | 3 | 1-6 |
| 27 | 15 | 7 | 0-16 | 3 | 0-6 |
| 28 | 14 | 6 | 0-15 | 3 | 0-6 |
| 29 | 13 | 5 | 0-15 | 3 | 0-6 |
| 30 | 12 | 5 | 0-14 | 3 | 0-6 |
| 31 | 11 | 4 | 0-14 | 3 | 0-6 |
| 32 | 10 | 4 | 0-13 | 3 | 0-6 |
| 33 | 9 | 4 | 0-13 | 3 | 0-6 |
| 34 | 8 | 4 | 0-13 | 3 | 0-6 |
| 35 | 7 | 3 | 0-13 | 3 | 0-6 |
| 36 | 6 | 3 | 0-13 | 3 | 0-6 |
| 37 | 5 | 3 | 0-13 | 3 | 0-6 |
| 38 | 4 | 4 | 0-14 | 3 | 0-6 |
The upper limit of the prediction interval for this age of implantation is within 5% of the subtest score ceiling. Therefore, expected raw scores denoted in italics should be interpreted with caution.
Appendix A4: Expected Scores on MacArthur-Bates Communicative Development Inventory (MBCDI) by Age at Implantation
Chronologic Age at Test = 4 years, 6 months (± 2 months).
|
Vocabulary Scale
Raw Score |
Irregular Words Scale
Raw Score |
||||
|---|---|---|---|---|---|
| Age at Surgery (in months) | Duration of Use | Expected Raw Score * | 68% Prediction Interval | Expected Raw Score* | 68% Prediction Interval |
| 12 | 42 | 665 | 539 + | 21 | 14 + |
| 13 | 41 | 653 | 529 + | 20 | 14 + |
| 14 | 40 | 642 | 518 + | 19 | 13 + |
| 15 | 39 | 630 | 507 + | 19 | 12 + |
| 16 | 38 | 618 | 495 + | 18 | 11 + |
| 17 | 37 | 605 | 483 + | 17 | 10 + |
| 18 | 36 | 593 | 471 + | 16 | 10-23 |
| 19 | 35 | 580 | 458 + | 16 | 9-22 |
| 20 | 34 | 568 | 446 + | 15 | 8-21 |
| 21 | 33 | 555 | 432 + | 14 | 7-21 |
| 22 | 32 | 541 | 419 + | 13 | 7-20 |
| 23 | 31 | 528 | 406 + | 13 | 6-19 |
| 24 | 30 | 515 | 392-637 | 12 | 5-19 |
| 25 | 29 | 501 | 379-623 | 11 | 5-18 |
| 26 | 28 | 487 | 365-610 | 11 | 4-17 |
| 27 | 27 | 473 | 351-595 | 10 | 4-17 |
| 28 | 26 | 459 | 337-581 | 10 | 3-16 |
| 29 | 25 | 445 | 322-567 | 9 | 2-16 |
| 30 | 24 | 430 | 308-552 | 9 | 2-15 |
| 31 | 23 | 415 | 293-538 | 8 | 1-15 |
| 32 | 22 | 400 | 278-523 | 8 | 0-14 |
| 33 | 21 | 385 | 262-508 | 7 | 0-14 |
| 34 | 20 | 370 | 246-494 | 7 | 0-13 |
| 35 | 19 | 355 | 230-479 | 6 | 0-13 |
| 36 | 18 | 339 | 213-465 | 6 | 0-13 |
| 37 | 17 | 323 | 195-451 | 5 | 0-12 |
| 38 | 16 | 307 | 177-437 | 5 | 0-12 |
|
Sentence Complexity Scale
Raw Score |
3 Longest Sentences Scale
Raw Score |
||||
| Age at Implant (in months) | Duration of Use | Expected Raw Score * | 68% Prediction Interval | Expected Raw Score | 68% Prediction Interval |
| 12 | 42 | 38 | 28 + | 10 | 6-15 |
| 13 | 41 | 36 | 27 + | 10 | 6-15 |
| 14 | 40 | 35 | 25 + | 10 | 5-14 |
| 15 | 39 | 34 | 24 + | 10 | 5-14 |
| 16 | 38 | 32 | 23 + | 9 | 5-14 |
| 17 | 37 | 31 | 22 + | 9 | 5-13 |
| 18 | 36 | 30 | 20 + | 9 | 4-13 |
| 19 | 35 | 29 | 19 + | 8 | 4-13 |
| 20 | 34 | 27 | 18 + | 8 | 4-13 |
| 21 | 33 | 26 | 17-36 | 8 | 4-12 |
| 22 | 32 | 25 | 15-35 | 8 | 3-12 |
| 23 | 31 | 24 | 14-33 | 7 | 3-12 |
| 24 | 30 | 23 | 13-32 | 7 | 3-12 |
| 25 | 29 | 21 | 12-31 | 7 | 2-11 |
| 26 | 28 | 20 | 11-30 | 7 | 2-11 |
| 27 | 27 | 19 | 10-29 | 6 | 2-11 |
| 28 | 26 | 18 | 9-28 | 6 | 2-10 |
| 29 | 25 | 17 | 7-26 | 6 | 1-10 |
| 30 | 24 | 16 | 6-25 | 6 | 1-10 |
| 31 | 23 | 15 | 5-24 | 5 | 1-10 |
| 32 | 22 | 14 | 4-23 | 5 | 1-9 |
| 33 | 21 | 13 | 3-22 | 5 | 0-9 |
| 34 | 20 | 12 | 2-21 | 4 | 0-9 |
| 35 | 19 | 11 | 1-20 | 4 | 0-9 |
| 36 | 18 | 10 | 0-19 | 4 | 0-8 |
| 37 | 17 | 9 | 0-19 | 4 | 0-8 |
| 38 | 16 | 8 | 0-18 | 3 | 0-8 |
The upper limit of the prediction interval for this age of implantation is within 5% of the subtest score ceiling. Therefore, expected raw scores denoted in italics should be interpreted with caution.
Contributor Information
Johanna G. Nicholas, CID at Washington University, Dept of Otolaryngology – Head and Neck Surgery, Washington University School of Medicine, St. Louis, Missouri 63110
Ann E. Geers, Dallas Cochlear Implant Program, Dept of Otolaryngology – Head and Neck Surgery, University of Texas Southwestern Medical Center and University of Texas at Dallas, Dallas, Texas 75235
References
- ASHA. Technical Report: Cochlear Implants. American Speech-Language Hearing Association. 2003 24:1–35. [Google Scholar]
- Bauer PW, Geers AE, Brenner CA, Moog JS, Smith RH. The effect of GJB2 allele variants on performance after cochlear implantation. Laryngoscope. 2003;113:2135–2140. doi: 10.1097/00005537-200312000-00015. [DOI] [PubMed] [Google Scholar]
- Boothroyd A, Geers AE, Moog JS. Practical implications of cochlear implants in children. Ear and Hearing. 1991;12:81–89. doi: 10.1097/00003446-199108001-00010. [DOI] [PubMed] [Google Scholar]
- Chin SB, Tsai PL, Gao S. Connected speech intelligibility of children with cochlear implants and children with normal hearing. American Journal of Speech-Language Pathology. 2003;12:440–451. doi: 10.1044/1058-0360(2003/090). [DOI] [PubMed] [Google Scholar]
- Ching TY, Psarros C, Hill M, Dillon H, Incerti P. Should children who use cochlear implants wear hearing aids in the opposite ear? Ear & Hearing. 2001;22:365–380. doi: 10.1097/00003446-200110000-00002. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1983. [Google Scholar]
- Connor CM, Craig HK, Raudenbush SW, Haevner K, Zwolan T. The age at which young deaf children receive cochlear implants and their vocabulary and speech-production growth: Is there an added value for early implantation? Ear & Hearing. 2006;27:628–644. doi: 10.1097/01.aud.0000240640.59205.42. [DOI] [PubMed] [Google Scholar]
- Connor CM, Hieber S, Arts HA, Zwolan TA. Speech, vocabulary, and the education of children using cochlear implants: Oral or Total Communication? Journal of Speech, Language, and Hearing Research. 2000;43:1185–1204. doi: 10.1044/jslhr.4305.1185. [DOI] [PubMed] [Google Scholar]
- Connor CM, Zwolan TA. Examining multiple sources of influence on the reading comprehension skills of children who use cochlear implants. Journal of Speech, Language and Hearing Research. 2004;47:496–508. doi: 10.1044/1092-4388(2004/040). [DOI] [PubMed] [Google Scholar]
- Dale P. The validity of a parent report measure of vocabulary and syntax at 24 months. Journal of Speech and Hearing Research. 1991;34:565–571. doi: 10.1044/jshr.3403.565. [DOI] [PubMed] [Google Scholar]
- Dawson PW, Busby PA, McKay CM, Clark GM. Short-term auditory memory in children using cochlear implants and its relevance to receptive language. Journal of Speech, Language, and Hearing Research. 2002;45:789–801. doi: 10.1044/1092-4388(2002/064). [DOI] [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. The Peabody Picture Vocabulary Test. 3rd. Circle Pines, MN: American Guidance Service; 1997. [Google Scholar]
- Eisenberg LS, Johnson KC, Martinez AS, Cokely CG, Tobey EA, Quittner AL, et al. Speech recognition at 1-year follow-up in the Childhood Development after Cochlear Implantation Study: Methods and preliminary findings. Audiology and Neurotology. 2006;11:259–268. doi: 10.1159/000093302. [DOI] [PubMed] [Google Scholar]
- Eisenberg LS, Kirk K, Martinez A, Ying E, Miyamoto R. Communication abilities of children with aided residual hearing. Archives of Otolaryngology - Head and Neck Surgery. 2004;130:563–569. doi: 10.1001/archotol.130.5.563. [DOI] [PubMed] [Google Scholar]
- Feldman HM, Dale PS, Campbell TF, Colborn DK, Kurs-Lasky M, Rockette HE, Paradise JL. Concurrent and predictive validity of parent reports of child language at ages 2 and 3 years. Child Development. 2005;76:856–868. doi: 10.1111/j.1467-8624.2005.00882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenson L, Dale PS, Reznick JS, Bates E, Thal DJ, Pethick SJ. Variability in early communicative development. Monographs of the Society for Research in Child Development. 1994;59(5) Serial No. 242. [PubMed] [Google Scholar]
- Fenson L, Dale PS, Reznick JS, Thal D, Bates E, Hartung JP, et al. MacArthur Communicative Development Inventories. San Diego, CA: Singular Publishing Group; 1993. [Google Scholar]
- Flipsen P, Jr, Colvard LG. Intelligibility of conversational speech produced by children with cochlear implants. Journal of Communication Disorders. 2006;39:93–108. doi: 10.1016/j.jcomdis.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Fortnum HM, Stacey PC, Summerfield AQ. An exploration of demographic bias in a questionnaire survey of hearing-impaired children: Implications for comparisons of children with and without cochlear implants. International Journal of Pediatric Otorhinolaryngology. 2006;70:2043–2054. doi: 10.1016/j.ijporl.2006.07.014. [DOI] [PubMed] [Google Scholar]
- Francis HW, Yeagle JD, Bowditch S, Niparko JK. Cochlear implant outcome is not influenced by the choice of ear. Ear and Hearing. 2005;26:7S–16S. doi: 10.1097/00003446-200508001-00003. [DOI] [PubMed] [Google Scholar]
- Friedland DR, Venick HS, Niparko JK. Choice of ear for cochlear implantation: The effect of history and residual hearing on predicted postoperative performance. Otology & Neurotology. 2003;24:582–589. doi: 10.1097/00129492-200307000-00009. [DOI] [PubMed] [Google Scholar]
- Geers AE. Predictors of reading skill development in children with early cochlear implantation. Ear & Hearing. 2003;241:59S–68S. doi: 10.1097/01.AUD.0000051690.43989.5D. [DOI] [PubMed] [Google Scholar]
- Geers A. Speech, language and reading skills after early cochlear implantation. Archives of Otolaryngology - Head and Neck Surgery. 2004a;130:634–638. doi: 10.1001/archotol.130.5.634. [DOI] [PubMed] [Google Scholar]
- Geers A. Educational intervention and outcomes of early cochlear implantation. International Congress Series. 2004b;1273:405–408. [Google Scholar]
- Geers A, Brenner C, Davidson L. Factors associated with development of speech perception skills in children implanted by age 5. Ear & Hearing. 2003;24:24–35. doi: 10.1097/01.AUD.0000051687.99218.0F. [DOI] [PubMed] [Google Scholar]
- Geers AE, Nicholas JG, Sedey AL. Language skills of children with early cochlear implantation. Ear & Hearing. 2003;24:46S–58S. doi: 10.1097/01.AUD.0000051689.57380.1B. [DOI] [PubMed] [Google Scholar]
- Holt RF, Kirk KI. Speech and language development in cognitively delayed children with cochlear implants. Ear & Hearing. 2005;26:132–148. doi: 10.1097/00003446-200504000-00003. [DOI] [PubMed] [Google Scholar]
- Holt RF, Kirk KI, Eisenberg L, Martinez AS, Campbell W. Spoken word recognition development in children with residual hearing using cochlear implants and hearing aids in opposite ears. Ear & Hearing. 2005;26:82S–91S. doi: 10.1097/00003446-200508001-00010. [DOI] [PubMed] [Google Scholar]
- Horga D, Liker M. Voice and pronunciation of cochlear implant speakers. Clinical Linguistics & Phonetics. 2006;20:211–217. doi: 10.1080/02699200400027015. [DOI] [PubMed] [Google Scholar]
- Horn DL, Pisoni DB, Miyamoto RT. Divergence of fine and gross motor skills in prelingually deaf children: Implications for cochlear implantation. The Laryngoscope. 2006;116:1500–1506. doi: 10.1097/01.mlg.0000230404.84242.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk KI, Miyamoto RT, Lento CL, Ying E, O'Neill T, Fears B. Effects of age at implantation in young children. Annals of Otology, Rhinology and Laryngology. 2002;111:69–73. doi: 10.1177/00034894021110s515. [DOI] [PubMed] [Google Scholar]
- Kirk KI, Miyamoto RT, Ying EA, Perdew AE, Zuganelis H. Cochlear implantation in young children: Effects of age at implantation and communication mode. The Volta Review. 2002;102:127–144. [Google Scholar]
- Kuo SCL, Gibson WPR. The influence of residual high-frequency hearing on the outcome in congenitally deaf cochlear implant recipients. The American Journal of Otology. 2000;21:657–662. [PubMed] [Google Scholar]
- Lidz CS. Issues in assessing preschool children. In: Paget K, Bracken B, editors. The psychoeducational assessment of preschool children. New York, NY: Grune & Stratton; 1983. [Google Scholar]
- Manrique M, Cervera-Paz FJ, Huarte A, Molina M. Advantages of cochlear implantation in prelingual deaf children before 2 years of age when compared with later implantation. Laryngoscope. 2004;114:1462–1469. doi: 10.1097/00005537-200408000-00027. [DOI] [PubMed] [Google Scholar]
- Mitchell TE, Psarros C, Pegg P, Rennie M, Gibson WPR. Performance after cochlear implantation: A comparison of children deafened by meningitis and congenitally deaf children. Journal of Laryngology and Otology. 2000;114:33–37. doi: 10.1258/0022215001903852. [DOI] [PubMed] [Google Scholar]
- Moog JS. Changing expectations for children with cochlear implants. Annals of Otology, Rhinology, & Laryngology. 2002;111:138–142. doi: 10.1177/00034894021110s527. [DOI] [PubMed] [Google Scholar]
- Moog JS, Geers AE. Epilogue: Major findings, conclusions and implications for deaf education. Ear and Hearing. 2003;24:121–125. doi: 10.1097/01.AUD.0000052759.62354.9F. [DOI] [PubMed] [Google Scholar]
- Nicholas JG, Geers AE. The process and early outcomes of cochlear implantation by three years of age. In: Marschark M, Spencer P, editors. Advances in spoken language development. New York: Oxford University Press; 2006a. [Google Scholar]
- Nicholas JG, Geers AE. Effects of early auditory experience on the spoken language of deaf children at 3 years of age. Ear and Hearing. 2006b;27:286–298. doi: 10.1097/01.aud.0000215973.76912.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholas JG, Geers AE. Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe-profound hearing loss. Journal of Speech, Language, and Hearing Research. 2007;50:xxx–xxx. doi: 10.1044/1092-4388(2007/073). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolopoulos TP, Archbold SM, O'Donoghue GM. Does cause of deafness influence outcome after cochlear implantation in children? Pediatrics. 2006;118:1350–1356. doi: 10.1542/peds.2006-0502. [DOI] [PubMed] [Google Scholar]
- Pisoni D, Cleary M. Measures of working memory span and verbal rehearsal speed in deaf children after cochlear implantation. Ear & Hearing. 2003;24:106S–121S. doi: 10.1097/01.AUD.0000051692.05140.8E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynell J, Gruber C. Reynell Developmental Language Scales. U.S. Los Angeles, Calif: Western Psychological Services; 1990. [Google Scholar]
- Robbins A, Green J, Waltzman S. Bilingual oral language proficiency in children with cochlear implants. Archives of Otolaryngology, Head and Neck Surgery. 2004;130:644–647. doi: 10.1001/archotol.130.5.644. [DOI] [PubMed] [Google Scholar]
- Sarant JZ, Blamey PJ, Dowell RC, Clark GM, Gibson WP. Variation in speech perception scores across children with cochlear implants. Ear & Hearing. 2001;22:18–28. doi: 10.1097/00003446-200102000-00003. [DOI] [PubMed] [Google Scholar]
- Sparrow S, Balla D, Cicchetti D. Vineland Adaptive Behavior Scales. Circle Pines, MN: American Guidance Service; 1984. [Google Scholar]
- Spencer L, Tomblin JB, Gantz B. Reading skills in children with multichannel cochlear implant experience. The Volta Review. 1998;99:193–202. [PMC free article] [PubMed] [Google Scholar]
- Stacey PC, Fortnum HM, Barton GR, Summerfield AQ. Hearing-impaired children in the United Kingdom, I. Auditory performance, communication skills, educational achievements, quality of life, and cochlear implantation. Ear & Hearing. 2006;27:161–186. doi: 10.1097/01.aud.0000202353.37567.b4. [DOI] [PubMed] [Google Scholar]
- Stallings LM, Gao S, Svirsky MA. Assessing the language abilities of pediatric cochlear implant users across a broad range of ages and performance abilities. The Volta Review. 2002;102:215–235. [Google Scholar]
- Stern RE, Yueh B, Lewis C, Norton S, Sie KCY. Recent epidemiology of pediatric cochlear implantation in the United States: Disparity among children of different ethnicity and socioeconomic status. Laryngoscope. 2005;115:125–131. doi: 10.1097/01.mlg.0000150698.61624.3c. [DOI] [PubMed] [Google Scholar]
- Svirsky MA, Robbins AM, Kirk KI, Pisoni DB, Miyamoto RT. Language development in profoundly deaf children with cochlear implants. Psychological Science. 2000;11:153–158. doi: 10.1111/1467-9280.00231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Svirsky MA, Teoh SW, Neuberger H. Development of language and speech perception in congenitally, profoundly deaf children as a function of age at cochlear implantation. Audiology and Neuro-Otology. 2004;9:224–233. doi: 10.1159/000078392. [DOI] [PubMed] [Google Scholar]
- Szagun G. Language acquisition in young German-speaking children with cochlear implants: Individual differences and implications for conceptions of a “sensitive phase”. Audiology and Neuro-otology. 2001;6:288–297. doi: 10.1159/000046134. [DOI] [PubMed] [Google Scholar]
- Thal DJ, DesJardin JL, Eisenberg LS. Validity of the MacArthur-Bates Communicative Development Inventories for measuring language abilities in children with cochlear implants. American Journal of Speech-Language Pathology. 2007;16:54–64. doi: 10.1044/1058-0360(2007/007). [DOI] [PubMed] [Google Scholar]
- Thal DJ, O'Hanlon L, Clemmons M, Fralin L. Validity of a parent report measure of vocabulary and syntax for preschool children with language impairment. Journal of Speech, Language, and Hearing Research. 1999;42:482–496. doi: 10.1044/jslhr.4202.482. [DOI] [PubMed] [Google Scholar]
- Tobey EA, Geers AE, Brenner C, Altuna D, Gabbert G. Factors associated with development of speech production skills in children implanted by age 5. Ear & Hearing. 2003;24:36–45. doi: 10.1097/01.AUD.0000051688.48224.A6. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C. Early intervention after universal neonatal hearing screening: Impact on outcomes. Mental Retardation and Developmental Disabilities Research Reviews. 2003;9:252–266. doi: 10.1002/mrdd.10088. [DOI] [PubMed] [Google Scholar]
- Zimmerman IL, Steiner VG, Pond RE. Preschool Language Scale -3. San Antonio, TX: The Psychological Corp; 1992. [Google Scholar]
- Zwolan TA, Zimmerman-Phillips S, Ashbaugh CJ, Hieber SJ, Kileny PR, Telian SA. Cochlear implantation of children with minimal open-set speech recognition skills. Ear and Hearing. 1997;18:240–251. doi: 10.1097/00003446-199706000-00007. [DOI] [PubMed] [Google Scholar]