The importance of interpersonal aspects of the practice of medicine has been universally recognized since ancient times.1 The doctor-patient relationship is at the heart of the practice of medicine, and it has been an object of rigorous scientific inquiry for the past 40 years.
Several models for doctor-patient relationships have been described over the years: biomedical, biopsychosocial, patient-centred, relationship-centred, negotiated, consumerist, and systemic.2–10 In recent years, however, the patient-centred model has dominated the literature on doctor-patient communication in the education and research domains. It is now endorsed by governing bodies of physicians in Canada as the accepted norm.11–12 There seems to have been a certain parallelism between the development of the concept of patient-centredness and of the discipline of contemporary family medicine. This paradigmatic shift was certainly instrumental in distinguishing family medicine from other medical and surgical specialties.13
If patient-centredness is now widely accepted, there remains the necessity to specify how the patient-centred model of care translates into responsive communication that is required for the diverse contexts in which family physicians practise. Kiesler and Auerbach14 indicate the necessity to further examine the influence of various contextual factors on communication, such as patient demographic characteristics, severity of the disease, the specific illness, and the type of medical decision being made. We propose that physicians should master numerous styles of relationships and learn to adjust their styles of communication for the context in which care is provided.
Coming to terms
A relationship is defined as a recurrent pattern of communication that exists between 2 people. Communication and relationships are each the source and the result of the other. The doctor-patient relationship constitutes a particular kind of interpersonal relationship; it is a “service” relationship, in which both parties have predetermined roles and the standards of behaviour for the physician are clearly defined by a code of ethics.1 The doctor-patient relationship requires mutual trust, acceptance of each other, and recognition of the ability to influence because of expertise. The physician’s behaviour must be guided by his or her concern for the patient at all times. Physicians must always adopt an attitude of respect for individuals, their autonomy, and their right to confidentiality.
Contemporary research has focused mainly on personal characteristics of patients, such as their preference for information provision or participation in decision making, their physical and mental ability to take the necessary steps to implement treatment, their understanding of their illnesses and the treatments, and their motivation to self-manage. But, like other interpersonal relationships, the doctor-patient relationship cannot be removed from the larger context in which the encounter occurs, and therefore it must be adjusted accordingly. Context is multidimensional.15
The doctor-patient relationship is determined by the characteristics of the problem at hand, such as the type of illness and its severity. The relationship is also defined by the physical place where the relationship develops (the hospital ward, office, emergency room, home, etc). Lastly, it is defined by the interlocutors.
We believe that context must be reintroduced to complete the map of possible relationships, which is why we are calling for a repertoire of doctor-patient relationships. The “one shoe fits all” approach does not allow optimal matching of physicians and patients.14 Favouring a single model such as the patient-centred model could prevent physicians from mastering relationship and communication skills that enable them to adjust to various situations.
We certainly recognize that there is a substantial body of research indicating that patient-centred relationships are associated with better outcomes16–21; however, most of these were associative (not causal) studies, and were conducted largely in the context of office consultations with patients with relatively stable medical conditions instead of normal health. Nothing can be stated with certainty about other clinical situations.
Looking at the problem
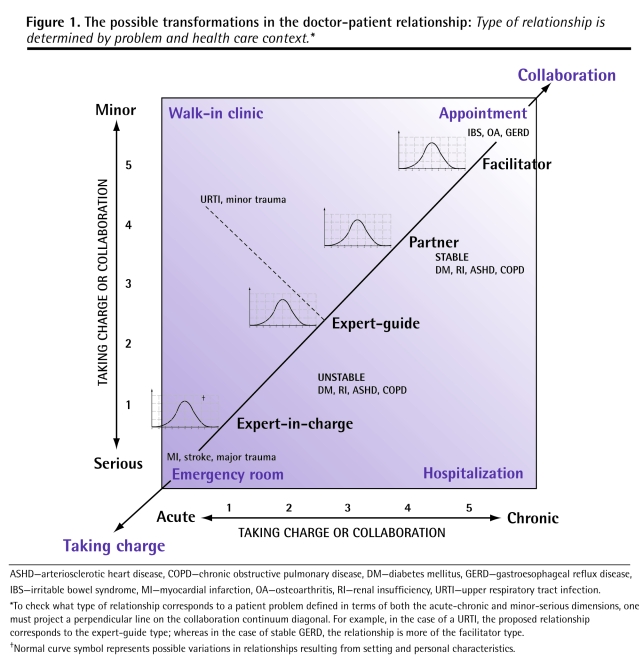
Figure 1 is a graphic representation of the possible transformations in the doctor-patient relationship along a decisional control continuum (taking charge or collaboration), suggesting different relationships defined by 2 characteristics of the patient problem: the nature of the problem (acute vs chronic) and its degree of severity (serious vs minor). This graph allows us to group together problems with similar characteristics and to indicate the care contexts in which the problems are most likely to be encountered. It should be noted, however, that the relationship that develops between the patient and the physician is not determined only by the characteristics of the problem; the setting and personal characteristics also contribute to defining the relationship. We have not included these aspects in Figure 1, but we have inserted a normal curve symbol at each dominant relationship as a reminder of this variation.
Figure 1. The possible transformations in the doctor-patient relationship.
Type of relationship is determined by problem and health care context.*
ASHD—arteriosclerotic heart disease, COPD—chronic obstructive pulmonary disease, DM—diabetes mellitus, GERD—gastroesophageal reflux disease, IBS—irritable bowel syndrome, MI—myocardial infarction, OA—osteoarthritis, RI—renal insufficiency, URTI—upper respiratory tract infection.
*To check what type of relationship corresponds to a patient problem defined in terms of both the acute-chronic and minor-serious dimensions, one must project a perpendicular line on the collaboration continuum diagonal. For example, in the case of a URTI, the proposed relationship corresponds to the expert-guide type; whereas in the case of stable GERD, the relationship is more of the facilitator type.
†Normal curve symbol represents possible variations in relationships resulting from setting and personal characteristics.
Based on the nature of the problem and the degree of severity, we suggest the following 4 types of relationships in which patients and physicians can engage and in which physicians’ roles vary: expert-in-charge, expert-guide, partner, and facilitator.
Expert-in-charge
In acute, serious circumstances, a physician is expected to make decisions unilaterally and carry out a certain number of actions on the patient’s behalf, the goal being to address the immediate threat to that person’s life. In such cases, the physician plays the role of an “expert-in-charge.” This relationship generally involves patients whose medical conditions are unstable and require immediate treatment (acute myocardial infarction, multiple trauma with shock, unstable angina, decompensated diabetes, decompensated chronic obstructive pulmonary disease, sepsis, etc). Physicians use their medical expertise to make decisions in these critical situations. Psychosocial aspects of care and patient beliefs often become secondary considerations, if they are considered at all. Caring is demonstrated by mobilizing medical resources to treat the individual.22–24 Verbally, it is expressed succinctly and is limited to brief statements, such as “We’re going to take care of you.”
Expert-guide
Moving along the axes in Figure 1 toward either more minor or chronic problems, which include common subacute situations that are not very serious (acute infections, lacerations, minor trauma, etc), the physician provides the patient with a professional opinion with regard to the diagnosis and offers advice and treatment suggestions. The physician adopts the role of “expert-guide.”
The physician’s goal is to inform the patient, prescribe treatment, and convince the patient of the treatment’s relevance. In this situation, it is possible to assess and take into account the psychosocial aspects of care and the patient’s beliefs. There is definitely more room for patient collaboration. Caring is demonstrated by obtaining information about the condition and meeting the patient’s need to feel heard.
Partner
With more chronic illnesses, regardless of being minor (irritable bowel syndrome, osteoarthritis, gastroesophageal reflux, etc) or more serious (diabetes, chronic obstructive pulmonary disease, renal insufficiency, heart disease, osteoporosis, etc), the physician might seek to build a relationship in which a partnership is established,22,23 adopting the role of “partner.” In these circumstances, the patient’s knowledge of the health problem develops progressively, and the patient becomes more competent to discuss various alternative treatments. The result is a true partnership. The physician’s objective is to motivate the patient and provide the necessary information, which enables the patient to carry out the agreed-upon treatment.
The psychosocial aspects of care and the patient’s beliefs are considered in the assessment of the condition, and the patient can participate in decisions regarding treatment. Caring is demonstrated through empathy and by welcoming the patient’s point of view. The verbal expression of caring can be quite developed and is characterized by more dialogue, which involves collaboration to determine acceptable solutions. This relationship most closely corresponds to what is considered a patient-centred approach.
Facilitator
Lastly, in the case of chronic illnesses that are well controlled, the physician often has to deal with patients who have developed good understanding of their diseases and the ability to monitor themselves independently, taking the necessary steps to adjust their treatments.25,26 In these situations, patients might have specific requests. Action has already been initiated by the patient at the time of the consultation, and the physician’s objective is to complete the patient’s information, if necessary, and help implement treatment. The patient and physician enter a relationship in which the physician acts as a health care facilitator and motivator. The psychosocial aspects and the patient’s beliefs are affirmed by the patient and play a role in requests to the physician. Caring is demonstrated by inviting and listening to the patient’s point of view. The encounter is characterized by dialogue, often initiated by the patient, by the physician’s careful assessment of the solutions proposed, and by suggestions to facilitate treatment implementation.
Conclusion
We have identified a set of clinical conditions that argue in favour of a variety of doctor-patient relationships rather than one type of relationship that is theoretically or ideologically suited to all situations. We must recognize that it is useful for physicians to master a repertoire of relationships. From our standpoint, all of the proposed relationships must be based on an attitude of respect for individuals, their autonomy, their right to confidentiality, and on behaviour guided by concern; these characteristics are the core of patient-centredness and, in this sense, patient-centredness remains fundamental in practice. However, we firmly believe that it has become necessary to further specify these fundamental characteristics of the doctor-patient relationship, as it would help physicians adapt to the demands of the various contexts in which they are now called upon to exercise their profession.
In order to continue a constructive discussion on doctor-patient relationships, we suggest moving toward a discussion about a repertoire of relationships rather than insisting physicians apply only one type of relationship to all clinical circumstances. There is risk associated with claiming that only one type of doctor-patient relationship is acceptable: when physicians find that that particular relationship is not applicable to their everyday clinical practice, they will reject it and revert to more paternalistic and expert-in-charge models, even in situations in which these models are clearly inappropriate.
We have provided a framework for various doctor-patient relationships for you to consider in differing circumstances. This framework is very similar to the situational leadership framework introduced by Hersey and Blanchard,27 who described the following styles of leadership: directing, coaching, supporting, and delegating; of these, none is considered optimal or desired. Flexibility and adaptation to a specific situation are required. We share this point of view.
We have tried to delineate the conditions under which doctor-patient relationships develop; thus, we have treated the relationship that develops not from an ideological or moral standpoint but from a practice-based perspective in which no unique model could possibly fit all circumstances. This is the first step in countering the oversimplification of the physician-patient relationship.
Footnotes
Competing interests
None declared
The opinions expressed in commentaries are those of the authors. Publication does not imply endorsement by the College of Family Physicians of Canada.
Cet article se trouve aussi en français à la page 1096.
References
- 1.Le Collège des médecins du Québec. Le serment d’Hippocrate. Montreal, QC: Le Collège des médecins du Québec; 2003. [Accessed 2008 May 13]. Available from: www.cmq.org/CmsPages/PageCmsSimpleSplit.aspx?PageID=05aa9276-c26a-4528-aab1-105fe58a800c. [Google Scholar]
- 2.Szasz TS. A contribution to the philosophy of medicine: the basic models of the doctor-patient relationship. AMA Arch Intern Med. 1956;97(5):585–92. doi: 10.1001/archinte.1956.00250230079008. [DOI] [PubMed] [Google Scholar]
- 3.Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129–36. doi: 10.1126/science.847460. [DOI] [PubMed] [Google Scholar]
- 4.McWhinney IR. Patient-centered and doctor-centered models of clinical decision making. In: Sheldon M, editor. Decision making in general practice. New York, NY: Stockton Press; 1985. pp. 31–45. [Google Scholar]
- 5.McWhinney IR. The need for a transformed clinical method. In: Stewart M, editor. Communicating with medical patients. Newbury Park, CA: Sage Publications; 1989. pp. 25–49. [Google Scholar]
- 6.Emanuel EJ. Four models of the physician-patient relationship. JAMA. 1992;267(16):2221–6. [PubMed] [Google Scholar]
- 7.Botelho RJ. A negotiation model for the doctor-patient relationship. Fam Pract. 1992;9(2):210–8. doi: 10.1093/fampra/9.2.210. [DOI] [PubMed] [Google Scholar]
- 8.Girard G. L’approche négociée: modèle de relation médecin-patient. Le Médecin du Québec. 1993;28(5):31–9. [Google Scholar]
- 9.Tresolini CP; Pew-Fetzer Task Force. Health professions education and relationship-centered care. San Francisco, CA: Pew Health Professions Commission; 1994. [Accessed 2008 May 13]. [Google Scholar]
- 10.Giroux L. Les modèles de relation médecin-patient. In: Richard C, editor. La communication professionnelle en santé. Montreal, QC: ERPI; 2005. pp. 113–43. [Google Scholar]
- 11.Le Collège des médecins de famille du Canada. Rapport du comité conjoint de la formation postdoctorale en médecine familiale sur le programme de résidence en médecine familiale. Mississauga, ON: Le Collège des médecins de famille du Canada; 1990. [Google Scholar]
- 12.Le Collège royal des médecins et chirurgiens du Canada. Le cadre des compétences des médecins CanMEDS. L’excellence des normes, des médecins et des soins. Ottawa, ON: Le Collège royal des médecins et chirurgiens du Canada; 2008. [Accessed 2008 Jul 9]. Available from: http://crmcc.medical.org/canmeds/index.php. [Google Scholar]
- 13.Kuhn TS. La structure des révolutions scientifiques. Paris, Fr: Flammarion; 1992. [Google Scholar]
- 14.Kiesler DJ, Auerbach SM. Optimal matches of patient preferences for information, decision-making and interpersonal behavior: evidence, models and interventions. Patient Educ Couns. 2006;61(3):319–41. doi: 10.1016/j.pec.2005.08.002. Epub 2005 Dec 20. [DOI] [PubMed] [Google Scholar]
- 15.Brown P. Speech as a marker of situation. In: Scherer KR, editor. Social markers in speec. Cambridge, UK: Cambridge University Press; 1979. [Google Scholar]
- 16.Hall JA. Meta-analysis of correlates of provider behaviour in medical encounters. Med Care. 1988;26(7):657–75. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Stewart MA. Effective physician-patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–33. [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart MA, et al. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49(9):796–804. [PubMed] [Google Scholar]
- 19.Maguire P. Key communication skills and how to acquire them. BMJ. 2002;325(7366):697–700. doi: 10.1136/bmj.325.7366.697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schillinger D, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- 21.Lewin SA. Interventions for providers to promote a patient-centred approach in clinical consultations. Cochrane Database Syst Rev. 2001;(4):CD003267. doi: 10.1002/14651858.CD003267. [DOI] [PubMed] [Google Scholar]
- 22.Mayeroff M. On caring. New York, NY: Harper and Row; 1971. [Google Scholar]
- 23.Roach MS. The human act of caring. Ottawa, ON: Canadian Hospital Association; 1992. [Google Scholar]
- 24.Cara C. A pragmatic view of Jean Watson’s caring theory. Int J Human Caring. 2003;7(3):51–7. [Google Scholar]
- 25.Thorne SE. Guarded alliance: health care relationships in chronic illness. Image J Nurs Sch. 1989;21(3):153–7. doi: 10.1111/j.1547-5069.1989.tb00122.x. [DOI] [PubMed] [Google Scholar]
- 26.Seaburn DB. Models of collaboration: a guide for mental health professionals working with health care practitioners. New York, NY: Basic Books; 1996. [Google Scholar]
- 27.Hersey P. Management of organizational behavior. Utilizing human resources. 4. New York, NY: Prentice Hall; 1987. [Google Scholar]