Abstract
Alpha-mannosidosis is an inherited lysosomal storage disorder characterized by immune deficiency, facial and skeletal abnormalities, hearing impairment, and intellectual disability. It occurs in approximately 1 of 500,000 live births. The children are often born apparently normal, and their condition worsens progressively. Some children are born with ankle equinus or develop hydrocephalus in the first year of life. Main features are immune deficiency (manifested by recurrent infections, especially in the first decade of life), skeletal abnormalities (mild-to-moderate dysostosis multiplex, scoliosis and deformation of the sternum), hearing impairment (moderate-to-severe sensorineural hearing loss), gradual impairment of mental functions and speech, and often, periods of psychosis. Associated motor function disturbances include muscular weakness, joint abnormalities and ataxia. The facial trait include large head with prominent forehead, rounded eyebrows, flattened nasal bridge, macroglossia, widely spaced teeth, and prognathism. Slight strabismus is common. The clinical variability is significant, representing a continuum in severity. The disorder is caused by lysosomal alpha-mannosidase deficiency. Alpha-mannosidosis is inherited in an autosomal recessive fashion and is caused by mutations in the MAN2B1 gene located on chromosome 19 (19 p13.2-q12). Diagnosis is made by measuring acid alpha-mannosidase activity in leukocytes or other nucleated cells and can be confirmed by genetic testing. Elevated urinary secretion of mannose-rich oligosaccharides is suggestive, but not diagnostic. Differential diagnoses are mainly the other lysosomal storage diseases like the mucopolysaccharidoses. Genetic counseling should be given to explain the nature of the disease and to detect carriers. Antenatal diagnosis is possible, based on both biochemical and genetic methods. The management should be pro-active, preventing complications and treating manifestations. Infections must be treated frequently. Otolaryngological treatment of fluid in the middle ear is often required and use of hearing aids is invariably required. Early educational intervention for development of social skills is needed and physiotherapy is important to improve bodily function. Orthopedic surgery may be necessary. The long-term prognosis is poor. There is an insidiously slow progression of neuromuscular and skeletal deterioration over several decades, making most patients wheel-chair dependent. No patients manage to be completely socially independent. Many patients are over 50 years of age.
Disease name and synonyms
α-Mannosidosis, Lysosomal α-D-Mannosidase Deficiency, α-Mannosidase B Deficiency. OMIM 248500.
History
Hurler-like syndrome had been known for a number of years when the Swedish physician Öckerman in Lund described a 4 year old boy with a Hurler-like phenotype in 1967 [1]. He died at the age of 4 from pneumonia, and in his tissues appeared large amounts of oligosaccharide material with the dominance of mannose. Therefore, the term "Mannosidosis" was suggested as the name of the disorder [2]. In 1977 Loeb described an atypical form of mucopolysaccharidosis which later turned out to be α-mannosidosis [3].
In 1978, Gideon Bach described two Palestinian siblings with a mild clinical phenotype and residual mannosidase activity, which increased by 40% with the addition of zinc (Zn++) to cell extracts of both patients and control subjects [4]. It took 25 years before the molecular mechanism of this observation could be explained [5]. Meanwhile, this observation led to many therapeutic attempts with zinc substitution in cattle [6] and man [7], which all proved futile.
Since these early clinical descriptions, many research groups have contributed to the characterization of the enzyme and the corresponding gene in several species such as human, cow, cat, mouse and guinea pig. Furthermore, underlying genetic, biochemical and physiological mechanisms of the disease have been explored, and additional clinical aspects of the disease such as immunodeficiency and psychiatric complications of the disease have been described (see below). Subsequently, two EU Research Consortiums, EURAMAN 2002–2005 (A systematic and multidisciplinary approach towards understanding and therapy of the inborn lysosomal storage disease α-mannosidosis), and HUE-MAN 2006–2009 (Towards the Development of an Effective Enzyme Replacement Therapy for Human α-Mannosidosis) were established [8].
Definition and diagnosis criteria
Alpha-mannosidosis is a genetic disorder of metabolism characterized by immune deficiency, facial and skeletal abnormalities, hearing impairment, and mental retardation. The disorder is caused by lysosomal α-mannosidase deficiency and is inherited in an autosomal recessive fashion.
Elevated urinary secretion of mannose-rich oligosaccharides is suggestive, but not diagnostic for α-mannosidosis. Diagnosis is made by measuring acid α-mannosidase activity in leukocytes or other nucleated cells, e.g. fibroblasts. Genetic diagnostics by mutation analysis is available from a few laboratories.
Alpha-mannosidosis has been described as two distinct phenotypes: one severe form with hepatomegaly and early death following severe infections (Type I), and a mild form with hearing loss, mental retardation, and survival into adulthood (Type II) [4,9,10].
However, when studying published cases, the patients present a continuum of clinical presentations, many of which probably can be influenced by background genetics or external factors like infectious diseases, educational opportunities, proactive initiatives, and quality of health services [11-13].
At present, three clinical types have been suggested [14-16]: Type 1: Mild form clinically recognized after 10 years of age, without skeletal abnormalities and very slow progression; Type 2: Moderate form, clinically recognized before 10 years of age, with skeletal abnormalities, and slow progression with development of ataxia at age 20–30; Type 3: Severe form, immediately recognized, with skeletal abnormalities, and obvious progression, leading to an early death from primary central nervous system (CNS) involvement or myopathy (Table 1). Most patients belong to clinical type 2.
Table 1.
Clinical types of alpha-mannosidosis
| Type II: Less severe, late onset form involving hearing loss, coarse face, mental retardation, and hepatosplenomegaly. | Type I: Severe infantile form which is fatal at <3–8 years of age. | |
| Type 1: Mild form clinically, recognized after 10 years of age, without skeletal abnormalities and very slow progression. | Type 2: Moderate form, clinically recognized before 10 years of age, with skeletal abnormalities, and slow progression with development of ataxia at age 20–30. | Type 3: Severe form, immediately recognized, with skeletal abnormalities, and obvious progression, leading to an early death from primary CNS involvement or myopathy. |
Epidemiology
The prevalence of the disease is not precisely known. A study from Norway reported six (later eight) patients in a population of 4.5 millions [17]. This corresponds with a study from Australia, reporting a disease frequency of one in 500,000 live births [18]. Mannosidosis is expected to be found in any ethnic group anywhere in the world.
Clinical description
Alpha-mannosidosis should be suspected in individuals with mental retardation, skeletal changes, hearing loss, and recurrent infections. The children are often born apparently normal, and their condition worsens progressively. Therefore, early diagnosis is important if bone marrow transplantation (BMT) is to be considered a therapeutic modality. Since inborn errors of lysosomal metabolism occur in approximately 1:5,000 live births, many have argued for screening of newborns for early diagnosis and initiation of treatment [18].
Onset of symptoms
Early references have described that early psychomotor development appears normal, and that pathophysiology develops over time [4,19]. However, some children are born with ankle equinus or develop hydrocephalus in the first year of life [17,20].
In α-mannosidosis guinea pigs, long before the onset of obvious neurologic abnormalities at 2 months, cerebral pathophysiology like neuronal lysosomal vacuolation, and reduced myelination of white matter was observed. Thus, complex neuropathologic changes in α-mannosidosis guinea pigs are already present at birth, long before clinical changes are evident, and similar events are likely to occur in humans with this disorder [21].
Associated facial features
Facial traits may be subtle, but independent of race and background genetics, all patients have some degree of coarse Hurler-like features. This is classically a large head with prominent forehead, rounded eyebrows, flattened nasal bridge, macroglossia, widely spaced teeth, and prognathism. The neck is usually short (Fig 1).
Figure 1.
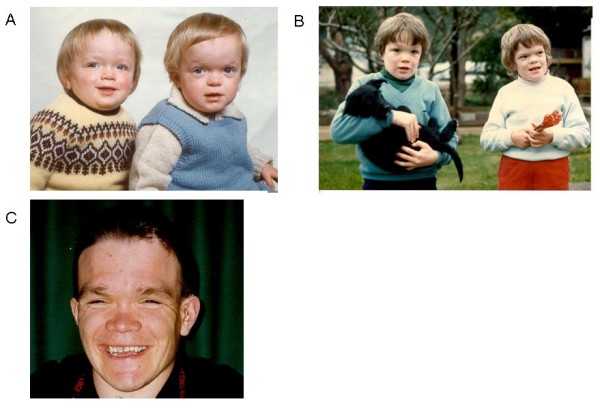
Facial features in alpha-mannosidosis. A. Twins aged 18 Months. Note enlarged head, short neck, rounded eyebrows, saddle nose, and prominent forehead. B. Same twins aged 8 years. Note slight muscular atrophy of the hands. C. Boy, aged 27. Note: Hearing aid.
Associated skeletal abnormalities
According to Chester (1982), clinical or radiographic signs of mild-to-moderate dysostosis multiplex are present in 90% of the patients [14]. The most frequent abnormalities are scoliosis and deformation of the sternum [22] (Fig 2). These changes are present at birth. Genu valgus (knucle knee) is common and, like the same complication in Gaucher disease, may be treated with epiphyseal arthrodesis at a young age before the epiphyseal lineation of the knee is closed [23]. Over time, from the second till the fourth decade of life the patients may develop destructive polyarthropathy, especially coxarthrosis (Fig 3), but also gonarthrosis [24,25]. These are often so serious that orthopedic corrections are needed [26]. Patellar bilateral dislocation and severe synovial hypertrophy have also been described along with Charcot elbow and bilateral hip and elbow avascular necrosis in one patient [27].
Figure 2.
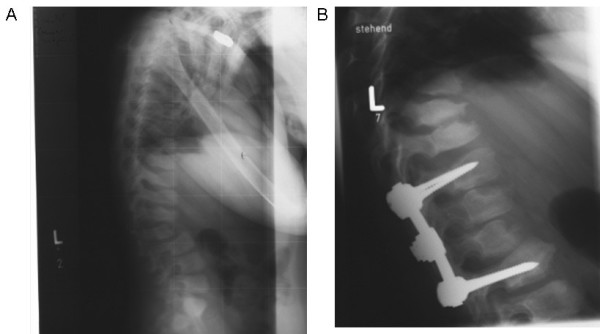
Radiography of kyphoscoliosis in alpha-mannosidosis before and after orthopedic correction. A. Kyphoscoliosis with skeletal abnormalities of all vertebrae. B. Orthopedic correction of kyphosis.
Figure 3.
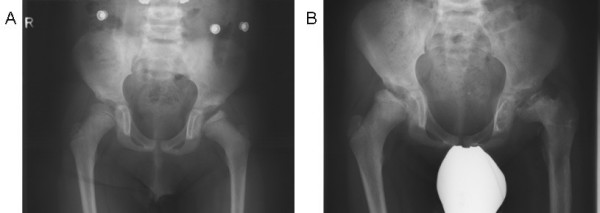
Coxarthrosis in alpha-mannosidosis. A. Coxarthrosis at 8 years of age. B. Progression of coxarthrosis at age 13.
Associated hearing impairment
Moderate or severe sensorineural hearing loss seems inevitable [12,22,28,29]. It is regularly worsened by otitis or accumulation of fluid in the middle ear, adding a mechanical component to the hearing deficit [17].
Associated ocular changes
Slight strabismus is common and also hyperopia more frequently than myopia [14,30]. Blurred discs [31], superficial corneal opacities, and lenticular changes seem to be rare but have been reported [4].
Associated mental retardation
As soon as the age of the patients makes intelligence quotient (IQ) measurements feasible, almost all patients show some degree of mental retardation. In a clinical study that included eight patients the age at onset of symptoms varied from 6 months to 3 years [10]. The first symptom was usually delayed development of speech or motor or mental functions. All the patients were mildly or moderately mentally retarded with an IQ of 60–80, with a declining tendency over later decades. With their poor ability to speak combined with sensorineural hearing loss, patients score generally better in nonverbal tests [10]. Although some have suggested the disease stabilises in puberty [32], most follow-up observations suggest gradual impairment of mental and motor functions and speech with age. Longitudinal assessments of three brothers have been done by testing of general intelligence, language, visual spatial skills, and overall adaptive abilities over two years. During the follow-up, the cognitive findings showed that the patients manifested mild cognitive deficits. Cognitive deficits were generally uniform with no signs of progressive deterioration, except receptive language abilities [33]. Other patients are described as having profound retardation even at young age [19,34]. Again, there can be remarkable differences in mental functioning among siblings [28,35,36].
Patients learn to speak late, sometimes in the second decade of life. This impaired development of language with limited vocabularies and poor pronunciation might be explained by their congenital and/or later-onset hearing loss. Many patients learn to read, but have difficulties in understanding abstracts (Malm D: personal observation).
Associated motor function disturbances
The development of motor functions in affected patients is generally slow, and the children appear clumsy. This is caused by a combination of factors like muscular weakness, joint abnormalities and ataxia due to cerebral atrophy and cerebral demyelination [37].
The impairment is by nature progressive, with gradual worsening in the second and third decade of life [10]. However, as for mental retardation, there is a considerable variation in the clinical progression and in a long term observation of two patients, no progression of neurological function has been noted [28], whereas some investigators have suggested that the disease progression is halted after puberty [32]. Additional studies on the natural course of the disease are needed.
Associated psychiatric disease
In intellectually disabled patients, psychiatric symptoms may be overlooked. However, a systematic survey found psychiatric symptoms in more than 25% of adult patients with mannosidosis [38]. It typically presented in adolescence or early adulthood. In mentally retarded patients, psychiatric symptoms form part of a more diffuse clinical picture with systemic, cognitive or motor neurological signs. It can present with acute and recurrent attacks of confusion, sometimes with anxiety, depressions or, hallucinations. These might be associated with loss of function, like decreased appetite with severe weights loss or incontinence for urine and feces. The periods of psychosis usually last 3 to 12 weeks, followed by a long period of hypersomnia and sometimes loss of abilities, like difficulty speaking or inability to read. Search for organic causes has been negative [38]. As specific treatments should be more effective at the initial stage before the occurrence of irreversible neurological lesions, clinicians should be aware of atypical psychiatric symptoms in patients with inborn errors of metabolism [39].
Associated immunodeficiency and autoimmunity
Mannosidosis patients suffer from recurrent infection, especially in the first decade of life. In one single patient, impaired leukocyte chemotaxis and reduced phagocytosis were found [9]. Malm and co-workers compared the humoral and cellular immunological functioning in six patients to that of six age- and sex-matched healthy controls [40]. They found that post-immunization levels of antibody were lower in patients, proving a decreased ability to produce specific antibodies after antigen presentation. More interestingly, there was a serum factor in patient plasma, inhibiting phagocytosis [40]. In mannosidosis, there are increased levels of oligosaccharides in plasma [41]. Oligomannosides with five and six mannose residues bind to interleukin-2 (IL-2) receptors disturbing the IL-2-dependent responses [42]. IL-2 activates T-, B-, and NK cells. It can therefore be speculated that blockage of this receptor is the mechanism causing the immune deficiency seen in mannosidosis.
The same mechanism could contribute to the increased prevalence of autoimmune disorders among mannosidosis patients ([13] and Malm D: personal observations). Interestingly, in a mice model, alpha-mannosidase II deficiency reduces complex-type N-glycan branching and induces an autoimmune disease similar to human systemic lupus erythematosus (SLE) with induction of antinuclear antibodies with reactivity towards histone, Sm antigen, and DNA [43].
Associated renal and cardiac complications
End-stage kidney failure has been reported only once, where an Italian patient successfully received a kidney transplant [44]. In a study in mannosidosis mice, deposits of storage material in myocardium were reduced after enzyme replacement [45]. In some case descriptions, a murmur of the heart is mentioned, but so far, reports on manifest heart disease have not been reported.
Molecular etiology
During normal turnover and catabolism glycoproteins are digested by proteinases and glycosidases within the lysosomes. These enzymes degrade glycoproteins into fragments small enough to be excreted or transported to the cytosol for reuse. Lack or deficiency of such hydrolases results in the multi-systemic accumulation of undigested material in the lysosomes. Consequently, the lysosomes swell resulting in severe impairment of cellular functions (Fig 4). However, the pathophysiology of lysosomal storage disorders is complex, and accumulation of storage material alone cannot fully explain the cause of disease.
Figure 4.
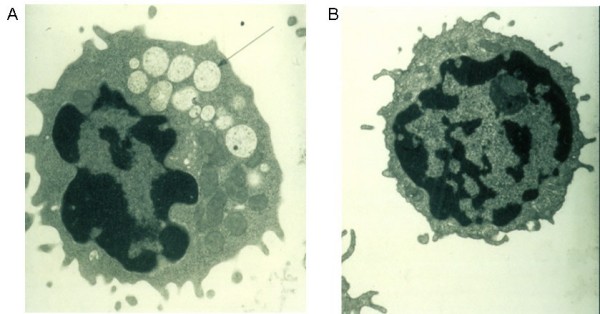
Electron micrograph of a vacuolated lymphocyte. Electron micrograph of a vacuolated lymphocyte from a mannosidosis patient (A) as compared to a lymphocyte from a normal control (B).
Lysosomal α-mannosidase is an exoglycosidase which cleaves the α-mannosidic linkages during the ordered degradation of N-linked oligosaccharides. The enzyme has the capacity to cleave α(1 → 2), α(1 → 3) and α(1 → 6) mannosidic linkages found in high mannose and hybrid type glycans [46,47]. Deduced from the analyses of mannose rich fractions from urine of affected individuals the major lysosomal storage products are the oligosaccharides:
Man(α1 → 3)Man(β1 → 4)GlcNac, Man(α1 → 2)Man(α1 → 3)Man(β1 → 4)GlcNac and Man(α1 → 2)Man(α1 → 2)Man(α1 → 3)Man(β1 → 4)GlcNac [48].
However, several additional, but apparently less abundant urinary oligosaccharides have been identified [49], all of them with GlcNac at the reducing end (reviewed by [50]).
Alpha-mannosidosis is caused by mutations in the MAN2B1 (LAMAN) gene encoding lysosomal α-mannosidase. The MAN2B1 is located on chromosome 19 (19p13.2-p13.11) and is composed of 24 exons spanning 21.5 kb [51,52]. The MAN2B1 mRNA has the capacity to encode a polypeptide of 988 [53] or 1011 [54] amino acids depending on the start site of translation (Genebank accession numbers U68382/U68567 and U60266.1). As judged by Northern blot analyses, the level of MAN2B1 expression appears to be highest in lung [54], kidney, pancreas [53,54], and peripheral blood leukocyte [53]. In CNS the highest level of expression appears to be in corpus callosum and spinal cord, whereas considerably lower levels are observed in the larger structures, which include cerebellum, cerebral cortex, frontal and temporal lobes [54]. The significance (if any) of this variation is not clear.
The enzyme is synthesized as a single chain precursor that is processed into three glycopeptides of 70, 42 and 15 kDa [54]. In humans, the 70 kDa peptide is further partially proteolysed into three more peptides that are joined by disulfide bridges – constituting all together 5 peptides (a-e) [54]. α-mannosidase contains 11 potential N-linked glycosylation sites all of which are occupied with either high mannose or complex type oligosaccharides [54]. Based on electron microscopy, X-ray diffraction data and the structure of D. melanogaster Golgi II α-mannosidase, the structure of the bovine lysosomal α-mannosidase was resolved at 2.7 Å resolution [5]. α-mannosidase is a di-mer and the 3-dimensional structure of bovine lysosomal α-mannosidase (which shares 80% identity to its human counterpart) nicely defines the fold of each peptide, identifies the active site and provide clues to understand lysosomal transport and low pH activation (Fig 5). Furthermore, the 3-dimensional structure provides the basis for understanding α-mannosidosis at the atomic level.
Figure 5.
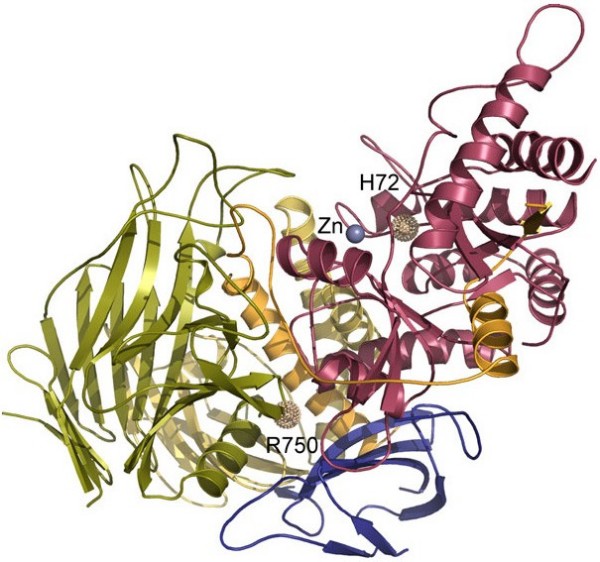
The 3-dimensional structure of lysosomal α-mannosidase. Peptides are coloured a-red, b-orange, c-yellow, d-green and e-blue. The active site is denoted by a Zn++ ion. Two mutant sites are displayed, demonstrating the effect of mutations c.215A>T: p.H72L affecting Zn++ coordination in the actives site (group 1 mutation, see text for explanation) and the prevalent mutation c.2248C>T: p.R750W which is likely affecting peptide e-d interaction (group 2 mutation, see text for explanation). The figure was kindly provided by Dr. P. Heikinheimo, University of Helsinki, Finland. It has been prepared with the program PyMol [72].
Disease-causing mutations
A total of 40 different disease-causing mutations have been reported over the last 10 years. Except for two unrelated patients from Japan and one patient of Arabian origin [13,54,55], the patients studied originate from Europe [11,15,54,56-60]. The genetic aberrations reported are scattered all over the MAN2B1 gene and include missense, nonsense, small and large deletions, small insertions and splice site mutations. Most mutations are private as they occur in single or in a few families only. However, missense mutation c.2248C>T resulting in the replacement of arginine with tryptophane at amino acid position 750 (p.R750W) appears to be frequent among mannosidosis patients, as it has been reported from most European populations studied, accounting for more than 30% of all disease alleles detected by Berg et al. (1999) [15]. Haplotyping based on 5 internal single nucleotide polymorphisms (SNP) markers showed that a common haplotype was shared by Finnish, Polish and Italian homozygotes, whereas a second haplotype, deviating at one marker, was observed in a Turkish patient [15]. These findings indicate that the frequency and wide geographical distribution of the "p.750W" allele may result both from founder effects and from recurrent mutational events. However, further analysis including patients of other origins must be carried out in order to explore this fully.
Altogether 12 missense mutations have been functionally characterized by expression analysis in mammalian cell lines followed by enzyme activity measurements and modeling into the MAN2B1 3-dimensional structure. Missense mutations affect residues located in the active site, in the dimer interphase as well as in the interior of the protein [5,58,59,61]. Based on pulse chase experiments and immune fluorescence microscopy, Hansen et al. (2004) monitored the intracellular transport of mutant enzymes. They concluded that mutant enzymes (missense) could be divided into two groups: Group 1 that was correctly sorted to the lysosomes and group 2 that was retained (transport arrested) in the endoplasmic reticulum (ER) [61].
Genotype phenotype relationships
There is no apparent correlation between MAN2B1 genotype and clinical phenotype in α-mannosidosis [15]. Clinical variation within sib ships has been observed [17,28,35,36], and patients characterized as less severely or moderately affected were shown to be homozygous for null mutations [15]. However, attempts to predict genotype/phenotype relationships often suffer from lack of data. Case reports on clinical findings are few and often include few patients and variability of methods used. Likewise, mutation reports often lack sufficient clinical data.
Enzyme activity measurements from patient leukocytes or fibroblast cells provide no clue either to a MAN2B1 genotype/phenotype correlation as these values range from 5% to 15% of normal levels. Using a refined method Berg et al. (1999) demonstrated that the level of cross-reacting α-mannosidase activity was less than 1.3% of that in controls, with no consistent variation among affected individuals. However, one cannot rule out the existence of MAN2B1 genotypes ("mild" mutations) that cause sub-clinical symptoms associated with residual enzyme activity. Such cases would likely escape detection as they will not be severe enough to arouse the suspicion of α-mannosidosis.
Environmental factors and other genetic factors may contribute to the clinical heterogeneity seen in α-mannosidosis. Environmental factors might be exposure to pathogens causing recurrent infections and thereby worsening of the disease symptoms. Other genetic factors might be those that encode other mannosidases like cytosolic α-mannosidase that potentially might contribute to the intra cellular clearance of undigested oligosaccharides [14,41,62-64]. However, no such salvage pathway has yet been proven to contribute to the clinical variability.
A thorough clinical and molecular investigation of many patients is warranted in order to explore the clinical variability of α-mannosidosis. Indeed, a study on the natural history of mannosidosis was recently initiated by HUE-MAN – a multinational research project supported by the sixth framework program of the European Union [8].
Diagnostic methods
Peripheral blood examination
Light microscopy or transmission electron microscopy (TEM) demonstrates vacuoles in bone marrow smears and lymphocytes from peripheral blood in most affected individuals (Fig 4) (reviewed in [14]). Although detection of vacuoles by microscopy is a useful screening test, supplementary investigations are necessary when α-mannosidosis is suspected.
Oligosaccharides in urine
Elevated urinary excretion of mannose-rich oligosaccharides can be demonstrated by thin-layer chromatography [41] or high performance liquid chromatography (HPLC) [65]. This finding is suggestive of α-mannosidosis, but not diagnostic.
Acid α-mannosidase activity
The most efficient and reliable method of establishing the diagnosis of α-mannosidosis is the assay of acidic α-mannosidase activity in leukocytes or other nucleated cells. This fluorometric assay is performed at low pH (usually at pH 4) with the substrate 4-methylumbelliferyl α-D-mannopyranoside. In affected individuals, acid α-mannosidase enzyme activity in peripheral blood leukocytes is 5%–15% of normal activity. Residual enzyme activity could possibly represent α-mannosidase activity from other organelles or compartments (e.g., Golgi apparatus; MAN2A1, cytosol; MAN2C1 or ER; MAN1B1), showing some activity also at low pH. Following immunoprecipitation with anti-acid α-mannosidase polyclonal antibodies, acid α-mannosidase enzyme activity ranges from 0.1% to 1.3% of normal [15]. Such testing is not performed routinely. In carriers, acid α-mannosidase enzyme activity is usually 40%–60% of normal, and is therefore unreliable for carrier detection because of the overlap between carriers and non-carriers.
Genetic testing
Identification of disease causing mutations is carried out on DNA from peripheral blood cells, by polymerase chain reaction (PCR) amplification of all 24 MAN2B1 exons followed by DNA sequencing.
Differential diagnosis
The main symptoms of mannosidosis, like dysmorphic traits, dysostosis, and mental retardation, are shared with the symptoms in many lysosomal storage diseases like mucopolysaccharidosis.
Genetic counseling
According to autosomal recessive inheritance, offspring of carrier parents have 25% risk of being affected whereas 50% will be non-symptomatic carriers.
Antenatal diagnosis
Prenatal testing is available for pregnancies of carrier parents. Prenatal testing may be performed by analysis of acid α-mannosidase enzyme activity in fetal cells obtained by chorionic villus sampling at 10–12 weeks gestation or by amniocentesis at 15–18 weeks. DNA from the same sources can be used for mutation analysis. Preferably, mutation analysis should be carried out in the parents in advance of pregnancy. Genotype does not allow prediction of severity of disease.
Management
Non-specific management
In general, the approach to the patients should be pro-active, searching for emerging complications. After a full physical examination, focusing on the known complications of mannosidosis like hydrocephalus, otitis media, hearing loss, dental state, joint status, kyphoscoliosis, and mental state, a plan should be made to limit the health consequences for the patient.
This would also include examination by an ophthalmologist, an otolaryngologist, audiometry and neuropsychological assessment, blood tests, and skeletal evaluation with radiographs, especially of the head, spine, knees or other skeletal sites displaying symptoms.
Hydrocephalus
Early diagnosis with measurement of head circumference, diagnosis with ultrasound, skull radiographs or computed tomography (CT) [20]. Ventriculocaval shunt should be preferred before ventriculoperitoneal shunt due to reduced ability of resorption in the peritoneal cavity in mannosidosis (Malm D: personal observation).
Otitis media
Diagnosis is simple and insertion of pressure-equalizing tubes will reduce the impact of the mechanical component of reduced hearing. There is a variety of tubes, and tubes with long-term stability should be preferred, since the condition is usually long lasting [29].
Hearing
Diagnosis is made with audiometry in cooperating patients, but can be difficult in young children and severely retarded patients. In some cases the brainstem auditory evoked response (BAER) test measuring brain wave activity that occurs in response to clicks or certain tones, can be useful. For speech therapy to be effective, hearing aids should be provided.
Dental state
Caries seem frequent because of reduced dental quality combined with tooth grinding or acid reflux from the stomach. Regular dental support and good dental hygiene is obviously important.
Joint status
Goniometry is used in the measurement of joint pathology. Kyphoscoliosis is measured according to Cobb, and can be corrected with orthopedic surgery (Fig 2). Genu valgum deformity can be treated with epiphyseal stapling in growing children, but must be performed early to be effective [23].
Mental state
Can be monitored with various tests, such as Wechsler. Nonverbal tests can compensate for the hearing deficit.
Specific treatment
In α-mannosidosis all cells are devoid of α-mannosidase activity. Early observations showed that cells producing α-mannosidase were able to transfer the enzyme to mannosidosis cells [63,66]. The rationale for bone marrow transplantation (BMT) in mannosidosis is that enzyme-producing donor cells repopulate the host tissues and transfer enzyme to nearby enzyme-deficient host cells.
In 1987 Will et al. performed BMT in a patient with α-mannosidosis. However, the patient died 18 weeks after successful grafting due to procedure related complications. The post mortem examination showed that transplantation reversed the somatic changes of α-mannosidosis, but did not affect lysosomal storage within brain tissue. It was therefore concluded that BMT may not be a suitable treatment for α-mannosidosis [67]. However, the findings of nil effect in the brain could be explained by the only 50% activity in donor cells which came from the mother (being a carrier of alpha-mannosidosis), the treatment of prednisone which could have influenced synthesis of protein, or the short observation period. Because of the blood-brain barrier, the main question remained whether BMT could improve the pathology of the central nervous system. In 1994, Steven Walkley reported that an early BMT could prevent neurological deterioration in a cat model [68]. A possible explanation of the neuronal benefits of BMT could be migration of donor-derived cells to the CNS of the recipient [69]. Later, Wall et al. (1998) presented a single case with BMT, claiming complete resolution of the recurrent infectious disease and organomegaly, improvement in the bone disease, and stabilization of neurocognitive function during a 2 year observation period [70].
Subsequently, a number of unpublished BMTs were performed, and in 2004, Grewal et al. could present results from four patients, aged 3 to 23 years, that had undergone BMT [69]. In short, they claimed that intellectual function stabilized, with improvement in adaptive skills and verbal memory function in 3 of 4 patients. Especially hearing improved to normal or near normal, but for speech frequencies only.
The possible benefits of BMT must be weighed against the overall risk of procedure related morbidity and mortality. The benefits are greater in younger patients before complications have developed, and also transplant related complications are more frequent and severe in older patients. Therefore, BMT is an option in the first decade of life which makes early identification of affected patients critical.
Prognosis
The long-term prognosis is poor. There is an insidiously slow progression of neuromuscular and skeletal deterioration over several decades, making most patients wheel-chair dependent. No patients manage to be completely socially independent. Many patients are over 50 years of age.
Unresolved questions
Enzyme replacement therapy (ERT) is a therapeutic modality in other lysosomal storage diseases, like Gaucher, Fabry or Pompe disease. In α-mannosidosis, experiments with ERT have been performed in an artificial knock-out mouse model [45], and in a naturally occurring guinea pig model [71]. The reduction in storage material was evident in almost all tissues in both models. However, whereas the first study found a reduction of mannose containing oligosaccharides in the brain to less than 30% of that in control mice with α-mannosidosis [45], a similar cerebral improvement was not found in guinea-pigs [71]. The development of ERT in human is the long term objective of the European HUE-MAN project [8].
Abbreviations
Central nervous system: CNS; bone marrow transplantation: BMT; intelligence quotient: IQ; interleukin-2: IL-2; systemic lupus erythematosus: SLE; single nucleotide polymorphisms: SNP; endoplasmic reticulum: ER; polymerase chain reaction: PCR; computed tomography: CT; brainstem auditory evoked response: BAER; Enzyme replacement therapy: ERT.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
The authors equally contributed to this review article. They read and approved the final version of the manuscript.
Consent
Written consent for publication of photographs was obtained from the patients or legal guardians where required.
Acknowledgments
Acknowledgements
The authors wish to thank Professor Pirko Heikinheimo, University of Helsinki, Finland, for contributing the α-Mannosidose 3-D model (Fig 5). Also, we wish to thank Dr. Hilde Monica Stensland, University Hospital of North Norway, and President of the ISMRD, John Forman, New Zealand, for valuable comments to the manuscript. We appreciate the European HUE-MAN project [8] enabling us to work in this field.
Contributor Information
Dag Malm, Email: dag.malm@unn.no.
Øivind Nilssen, Email: oivind.nilssen@fagmed.uit.no.
References
- Ockerman PA. A generalised storage disorder resembling Hurler's syndrome. Lancet. 1967;2:239. doi: 10.1016/S0140-6736(67)92303-3. [DOI] [Google Scholar]
- Ockerman PA. Mannosidosis: isolation of oligosaccharide storage material from brain. J Pediatr. 1969;75:360–365. doi: 10.1016/S0022-3476(69)80259-3. [DOI] [PubMed] [Google Scholar]
- Loeb H, Vamos-Hurwitz E. Mannosidosis. Arch Neurol. 1977;34:650–651. doi: 10.1001/archneur.1977.00500220084022. [DOI] [PubMed] [Google Scholar]
- Bach G, Kohn G, Lasch EE, El Massri M, Ornoy A, Sekeles E, Legum C, Cohen MM. A new variant of mannosidosis with increased residual enzymatic activity and mild clinical manifestation. Pediatr Res. 1978;12:1010–1015. doi: 10.1203/00006450-197810000-00012. [DOI] [PubMed] [Google Scholar]
- Heikinheimo P, Helland R, Leiros HK, Leiros I, Karlsen S, Evjen G, Ravelli R, Schoehn G, Ruigrok R, Tollersrud OK, McSweeney S, Hough E. The structure of bovine lysosomal alpha-mannosidase suggests a novel mechanism for low-pH activation. J Mol Biol. 2003;327:631–644. doi: 10.1016/S0022-2836(03)00172-4. [DOI] [PubMed] [Google Scholar]
- Jolly RD, Water NS Van de, Janmaat A, Slack PM, McKenzie RG. Zinc therapy in the bovine mannosidosis model. Birth Defects Orig Artic Ser. 1980;16:305–318. [PubMed] [Google Scholar]
- Wong LT, Vallance H, Savage A, Davidson AG, Applegarth D. Oral zinc therapy in the treatment of alpha-mannosidosis. Am J Med Genet. 1993;46:410–414. doi: 10.1002/ajmg.1320460413. [DOI] [PubMed] [Google Scholar]
- HUE-MAN Towards the Development of an Effective Enzyme Replacement Therapy for Human á-Mannosidosis. 2006. http://www.uni-kiel.de/Biochemie/hue-man/
- Desnick RJ, Sharp HL, Grabowski GA, Brunning RD, Quie PG, Sung JH, Gorlin RJ, Ikonne JU. Mannosidosis: clinical, morphologic, immunologic, and biochemical studies. Pediatr Res. 1976;10:985–996. doi: 10.1203/00006450-197612000-00008. [DOI] [PubMed] [Google Scholar]
- Autio S, Louhimo T, Helenius M. The clinical course of mannosidosis. Ann Clin Res. 1982;14:93–97. [PubMed] [Google Scholar]
- Olmez A, Nilssen O, Coskun T, Klenow H. Alpha-mannosidosis and mutational analysis in a Turkish patient. Turk J Pediatr. 2003;45:46–50. [PubMed] [Google Scholar]
- Gutschalk A, Harting I, Cantz M, Springer C, Rohrschneider K, Meinck HM. Adult alpha-mannosidosis: clinical progression in the absence of demyelination. Neurology. 2004;63:1744–1746. doi: 10.1212/01.wnl.0000143057.25471.4f. [DOI] [PubMed] [Google Scholar]
- Urushihara M, Kagami S, Yasutomo K, Ito M, Kondo S, Kitamura A, Malm D, Klenow H, Nilssen O, Kuroda Y. Sisters with alpha-mannosidosis and systemic lupus erythematosus. Eur J Pediatr. 2004;163:192–195. doi: 10.1007/s00431-004-1404-2. [DOI] [PubMed] [Google Scholar]
- Chester MA, Lundblad A, Öckerman PA, Autio S. Mannosidosis. In: Duran P, O'Brien JF, editor. Genetic Errors of Glyco-Protein Metabolism. Milan: Edi-Hermes; 1982. pp. 89–120. [Google Scholar]
- Berg T, Riise HM, Hansen GM, Malm D, Tranebjaerg L, Tollersrud OK, Nilssen O. Spectrum of mutations in alpha-mannosidosis. Am J Hum Genet. 1999;64:77–88. doi: 10.1086/302183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malm D, Nilssen O. Alpha-Mannosidosis. GeneReviews. Medical Genetics Information Resource [Database online] 2006. http://www.geneclinics.org/
- Malm D, Tollersrud OK, Tranebjaerg L, Mansson JE. [Alpha-mannosidosis] Tidsskr Nor Laegeforen. 1995;115:594–597. [PubMed] [Google Scholar]
- Meikle PJ, Ranieri E, Simonsen H, Rozaklis T, Ramsay SL, Whitfield PD, Fuller M, Christensen E, Skovby F, Hopwood JJ. Newborn screening for lysosomal storage disorders: clinical evaluation of a two-tier strategy. Pediatrics. 2004;114:909–916. doi: 10.1542/peds.2004-0583. [DOI] [PubMed] [Google Scholar]
- Aylsworth AS, Taylor HA, Stuart CM, Thomas GH. Mannosidosis: phenotype of a severely affected child and characterization of alpha-mannosidase activity in cultured fibroblasts from the patient and his parents. J Pediatr. 1976;88:814–818. doi: 10.1016/S0022-3476(76)81120-1. [DOI] [PubMed] [Google Scholar]
- Halperin JJ, Landis DM, Weinstein LA, Lott IT, Kolodny EH. Communicating hydrocephalus and lysosomal inclusions in mannosidosis. Arch Neurol. 1984;41:777–779. doi: 10.1001/archneur.1984.04050180099027. [DOI] [PubMed] [Google Scholar]
- Crawley AC, Walkley SU. Developmental analysis of CNS pathology in the lysosomal storage disease alpha-mannosidosis. J Neuropathol Exp Neurol. 2007;66:687–697. doi: 10.1097/nen.0b013e31812503b6. [DOI] [PubMed] [Google Scholar]
- de Jong G, Petersen EM. First reported case of alpha-mannosidosis in the RSA. S Afr Med J. 1992;82:126–128. [PubMed] [Google Scholar]
- Odunusi E, Peters C, Krivit W, Ogilvie J. Genu valgum deformity in Hurler syndrome after hematopoietic stem cell transplantation: correction by surgical intervention. J Pediatr Orthop. 1999;19:270–274. doi: 10.1097/00004694-199903000-00026. [DOI] [PubMed] [Google Scholar]
- Eckhoff DG, Garlock JS. Severe destructive polyarthropathy in association with a metabolic storage disease. A case report. J Bone Joint Surg Am. 1992;74:1257–1261. [PubMed] [Google Scholar]
- DeFriend DE, Brown AE, Hutton CW, Hughes PM. Mannosidosis: an unusual cause of a deforming arthropathy. Skeletal Radiol. 2000;29:358–361. doi: 10.1007/s002560000213. [DOI] [PubMed] [Google Scholar]
- Gerards AH, Winia WP, Westerga J, Dijkmans BA, van Soesbergen RM. Destructive joint disease in alpha-mannosidosis. A case report and review of the literature. Clin Rheumatol. 2004;23:40–42. doi: 10.1007/s10067-003-0770-x. [DOI] [PubMed] [Google Scholar]
- Hale SS, Bales JG, Rosenzweig S, Daroca P, Bennett JT. Bilateral patellar dislocation associated with alpha-mannosidase deficiency. J Pediatr Orthop B. 2006;15:215–219. doi: 10.1097/01.bpb.0000188248.79029.1d. [DOI] [PubMed] [Google Scholar]
- Ara JR, Mayayo E, Marzo ME, Guelbenzu S, Chabás A, Pina MA, Calderón C. Neurological impairment in alpha-mannosidosis: a longitudinal clinical and MRI study of a brother and sister. Childs Nerv Syst. 1999;15:369–371. doi: 10.1007/s003810050416. [DOI] [PubMed] [Google Scholar]
- Ahmmed AU, O'Halloran SM, Roland NJ, Starkey M, Wraith JE. Hearing loss due to mannosidosis and otitis media with effusion. A case report and review of audiological assessments in children with otitis media with effusion. J Laryngol Otol. 2003;117:307–309. doi: 10.1258/00222150360600931. [DOI] [PubMed] [Google Scholar]
- Arbisser AI, Murphree AL, Garcia CA, Howell RR. Ocular findings in mannosidosis. Am J Ophthalmol. 1976;82:465–471. doi: 10.1016/0002-9394(76)90496-7. [DOI] [PubMed] [Google Scholar]
- Kjellman B, Gamstorp I, Brun A, Ockerman PA, Palmgren B. Mannosidosis: a clinical and histopathologic study. J Pediatr. 1969;75:366–373. doi: 10.1016/S0022-3476(69)80260-X. [DOI] [PubMed] [Google Scholar]
- Yunis JJ, Lewandowski RC, Jr, Sanfilippo SJ, Tsai MY, Foni I, Bruhl HH. Clinical manifestations of mannosidosis – a longitudinal study. Am J Med. 1976;61:841–848. doi: 10.1016/0002-9343(76)90408-3. [DOI] [PubMed] [Google Scholar]
- Noll RB, Netzloff ML, Kulkarni R. Long-term follow-up of biochemical and cognitive functioning in patients with mannosidosis. Arch Neurol. 1989;46:507–509. doi: 10.1001/archneur.1989.00520410041020. [DOI] [PubMed] [Google Scholar]
- Gordon BA, Carson R, Haust MD. Unusual clinical and ultrastructural features in a boy with biochemically typical mannosidosis. Acta Paediatr Scand. 1980;69:787–792. doi: 10.1111/j.1651-2227.1980.tb07154.x. [DOI] [PubMed] [Google Scholar]
- Mitchell ML, Erickson RP, Schmid D, Hieber V, Poznanski AK, Hicks SP. Mannosidosis: two brothers with different degrees of disease severity. Clin Genet. 1981;20:191–202. doi: 10.1111/j.1399-0004.1981.tb01829.x. [DOI] [PubMed] [Google Scholar]
- Michelakakis H, Dimitriou E, Mylona-Karayanni C, Bartsocas CS. Phenotypic variability of mannosidosis type II: report of two Greek siblings. Genet Couns. 1992;3:195–199. [PubMed] [Google Scholar]
- Dietemann JL, Filippi de la Palavesa MM, Tranchant C, Kastler B. MR findings in mannosidosis. Neuroradiology. 1990;32:485–487. doi: 10.1007/BF02426460. [DOI] [PubMed] [Google Scholar]
- Malm D, Pantel J, Linaker OM. Psychiatric symptoms in alpha-mannosidosis. J Intellect Disabil Res. 2005;49:865–871. doi: 10.1111/j.1365-2788.2005.00765.x. [DOI] [PubMed] [Google Scholar]
- Sedel F, Baumann N, Turpin JC, Lyon-Caen O, Saudubray JM, Cohen D. Psychiatric manifestations revealing inborn errors of metabolism in adolescents and adults. J Inherit Metab Dis. 2007:631–641. doi: 10.1007/s10545-007-0661-4. [DOI] [PubMed] [Google Scholar]
- Malm D, Halvorsen DS, Tranebjaerg L, Sjursen H. Immunodeficiency in alpha-mannosidosis: a matched case-control study on immunoglobulins, complement factors, receptor density, phagocytosis and intracellular killing in leucocytes. Eur J Pediatr. 2000;159:699–703. doi: 10.1007/s004310000545. [DOI] [PubMed] [Google Scholar]
- Michalski JC, Klein A. Glycoprotein lysosomal storage disorders: alpha- and beta-mannosidosis, fucosidosis and alpha-N-acetylgalactosaminidase deficiency. Biochim Biophys Acta. 1999;1455:69–84. doi: 10.1016/s0925-4439(99)00077-0. [DOI] [PubMed] [Google Scholar]
- Zanetta JP, Bonaly R, Maschke S, Strecker G, Michalski JC. Differential binding of lectins IL-2 and CSL to candida albicans and cancer cells. Glycobiology. 1998;8:221–225. doi: 10.1093/glycob/8.3.221. [DOI] [PubMed] [Google Scholar]
- Green RS, Stone EL, Tenno M, Lehtonen E, Farquhar MG, Marth JD. Mammalian N-glycan branching protects against innate immune self-recognition and inflammation in autoimmune disease pathogenesis. Immunity. 2007;27:308–320. doi: 10.1016/j.immuni.2007.06.008. [DOI] [PubMed] [Google Scholar]
- Segoloni GP, Colla L, Messina M, Stratta P. Renal transplantation in a case of mannosidosis. Transplantation. 1996;61:1654–1655. doi: 10.1097/00007890-199606150-00019. [DOI] [PubMed] [Google Scholar]
- Roces DP, Lüllmann-Rauch R, Peng J, Balducci C, Andersson C, Tollersrud O, Fogh J, Orlacchio A, Beccari T, Saftig P, von Figura K. Efficacy of enzyme replacement therapy in alpha-mannosidosis mice: a preclinical animal study. Hum Mol Genet. 2004;13:1979–1988. doi: 10.1093/hmg/ddh220. [DOI] [PubMed] [Google Scholar]
- Michalski JC, Haeuw JF, Wieruszeski JM, Montreuil J, Strecker G. In vitro hydrolysis of oligomannosyl oligosaccharides by the lysosomal alpha-D-mannosidases. Eur J Biochem. 1990;189:369–379. doi: 10.1111/j.1432-1033.1990.tb15498.x. [DOI] [PubMed] [Google Scholar]
- Daniel PF, Winchester B, Warren CD. Mammalian alpha-mannosidases – multiple forms but a common purpose? Glycobiology. 1994;4:551–566. doi: 10.1093/glycob/4.5.551. [DOI] [PubMed] [Google Scholar]
- DeGasperi R, al Daher S, Daniel PF, Winchester BG, Jeanloz RW, Warren CD. The substrate specificity of bovine and feline lysosomal alpha-D-mannosidases in relation to alpha-mannosidosis. J Biol Chem. 1991;266:16556–16563. [PubMed] [Google Scholar]
- Yamashita K, Tachibana Y, Mihara K, Okada S, Yabuuchi H, Kobata A. Urinary oligosaccharides of mannosidosis. J Biol Chem. 1980;255:5126–5133. [PubMed] [Google Scholar]
- Thomas GH. Disorders of Glycoprotein Degradation: Alpha-Mannosidosis, beta-Mannosidosis, Fucosidosis, and Sialidosis. In: Schriver CR, Beudet AL, Sly WS, editor. The Metabolic & Molecular Basis of Inherited Diseases. 8. III. New York: McGraw-Hill; 2001. pp. 3507–3516. [Google Scholar]
- Riise HM, Berg T, Nilssen O, Romeo G, Tollersrud OK, Ceccherini I. Genomic structure of the human lysosomal alpha-mannosidase gene (MANB) Genomics. 1997;42:200–207. doi: 10.1006/geno.1997.4668. [DOI] [PubMed] [Google Scholar]
- Wakamatsu N, Gotoda Y, Saito S, Kawai H. Characterization of the human MANB gene encoding lysosomal alpha-D-mannosidase. Gene. 1997;198:351–357. doi: 10.1016/S0378-1119(97)00337-5. [DOI] [PubMed] [Google Scholar]
- Liao YF, Lal A, Moremen KW. Cloning, expression, purification, and characterization of the human broad specificity lysosomal acid alpha-mannosidase. J Biol Chem. 1996;271:28348–28358. doi: 10.1074/jbc.271.20.11838. [DOI] [PubMed] [Google Scholar]
- Nilssen O, Berg T, Riise HM, Ramachandran U, Evjen G, Hansen GM, Malm D, Tranebjaerg L, Tollersrud OK. alpha-Mannosidosis: functional cloning of the lysosomal alpha-mannosidase cDNA and identification of a mutation in two affected siblings. Hum Mol Genet. 1997;6:717–726. doi: 10.1093/hmg/6.5.717. [DOI] [PubMed] [Google Scholar]
- Gotoda Y, Wakamatsu N, Kawai H, Nishida Y, Matsumoto T. Missense and nonsense mutations in the lysosomal alpha-mannosidase gene (MANB) in severe and mild forms of alpha-mannosidosis. Am J Hum Genet. 1998;63:1015–1024. doi: 10.1086/302048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frostad Riise HM, Hansen GM, Tollersrud OK, Nilssen O. Characterization of a novel alpha-mannosidosis-causing mutation and its use in leukocyte genotyping after bone marrow transplantation. Hum Genet. 1999;104:106–107. doi: 10.1007/s004390050918. [DOI] [PubMed] [Google Scholar]
- Beccari T, Bibi L, Ricci R, Antuzzi D, Burgalossi A, Costanzi E, Orlacchio A. Two novel mutations in the gene for human alpha-mannosidase that cause alpha-mannosidosis. J Inherit Metab Dis. 2003;26:819–820. doi: 10.1023/B:BOLI.0000010006.87571.48. [DOI] [PubMed] [Google Scholar]
- Sbaragli M, Bibi L, Pittis MG, Balducci C, Heikinheimo P, Ricci R, Antuzzi D, Parini R, Spaccini L, Bembi B, Beccari T. Identification and characterization of five novel MAN2B1 mutations in Italian patients with alpha-mannosidosis. Hum Mutat. 2005;25:320. doi: 10.1002/humu.9310. [DOI] [PubMed] [Google Scholar]
- Pittis MG, Montalvo AL, Heikinheimo P, Sbaragli M, Balducci C, Persichetti E, Van Maldergem L, Filocamo M, Bembi B, Beccari T. Funtional characterization of four novel MAN2B1 mutations causing juvenile onset alpha-mannosidosis. Clin Chim Acta. 2007;375:136–139. doi: 10.1016/j.cca.2006.06.034. [DOI] [PubMed] [Google Scholar]
- Lyons MJ, Wood T, Espinoza L, Stensland HM, Holden KR. Early onset alpha-mannosidosis with slow progression in three Hispanic males. Dev Med Child Neurol. 2007;49:854–857. doi: 10.1111/j.1469-8749.2007.00854.x. [DOI] [PubMed] [Google Scholar]
- Hansen G, Berg T, Riise Stensland HM, Heikinheimo P, Klenow H, Evjen G, Nilssen Ø, Tollersrud OK. Intracellular transport of human lysosomal alpha-mannosidase and alpha-mannosidosis-related mutants. Biochem J. 2004;381:537–546. doi: 10.1042/BJ20031499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warner TG, Mock AK, Nyhan WL, O'Brien JS. Alpha-mannosidosis: analysis of urinary oligosaccharides with high performance liquid chromatography and diagnosis of a case with unusually mild presentation. Clin Genet. 1984;25:248–255. doi: 10.1111/j.1399-0004.1984.tb01985.x. [DOI] [PubMed] [Google Scholar]
- Abraham D, Muir H, Winchester B, Olsen I. Lymphocytes transfer only the lysosomal form of alpha-D-mannosidase during cell-to-cell contact. Exp Cell Res. 1988;175:158–168. doi: 10.1016/0014-4827(88)90263-7. [DOI] [PubMed] [Google Scholar]
- Grard T, Herman V, Saint-Pol A, Kmiecik D, Labiau O, Mir AM, Alonso C, Verbert A, Cacan R, Michalski JC. Oligomannosides or oligosaccharide-lipids as potential substrates for rat liver cytosolic alpha-D-mannosidase. Biochem J. 1996;316:787–792. doi: 10.1042/bj3160787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egge H, Michalski JC, Strecker G. Heterogeneity of urinary oligosaccharides from mannosidosis: mass spectrometric analysis of permethylated Man9, Man8, and Man7 derivatives. Arch Biochem Biophys. 1982;213:318–326. doi: 10.1016/0003-9861(82)90468-4. [DOI] [PubMed] [Google Scholar]
- Olsen I, Abraham D, Shelton I, Bou-Gharios G, Muir H, Winchester B. Cell contact induces the synthesis of a lysosomal enzyme precursor in lymphocytes and its direct transfer to fibroblasts. Biochim Biophys Acta. 1988;968:312–322. doi: 10.1016/0167-4889(88)90022-5. [DOI] [PubMed] [Google Scholar]
- Will A, Cooper A, Hatton C, Sardharwalla IB, Evans DI, Stevens RF. Bone marrow transplantation in the treatment of alpha-mannosidosis. Arch Dis Child. 1987;62:1044–1049. doi: 10.1136/adc.62.10.1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkley SU, Thrall MA, Dobrenis K, Huang M, March PA, Siegel DA, Wurzelmann S. Bone marrow transplantation corrects the enzyme defect in neurons of the central nervous system in a lysosomal storage disease. Proc Natl Acad Sci USA. 1994;91:2970–2974. doi: 10.1073/pnas.91.8.2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grewal SS, Shapiro EG, Krivit W, Charnas L, Lockman LA, Delaney KA, Davies SM, Wenger DA, Rimell FL, Abel S, Grovas AC, Orchard PJ, Wagner JE, Peters C. Effective treatment of alpha-mannosidosis by allogeneic hematopoietic stem cell transplantation. J Pediatr. 2004;144:569–573. doi: 10.1016/j.jpeds.2004.01.025. [DOI] [PubMed] [Google Scholar]
- Wall DA, Grange DK, Goulding P, Daines M, Luisiri A, Kotagal S. Bone marrow transplantation for the treatment of alpha-mannosidosis. J Pediatr. 1998;133:282–285. doi: 10.1016/S0022-3476(98)70237-9. [DOI] [PubMed] [Google Scholar]
- Crawley AC, King B, Berg T, Meikle PJ, Hopwood JJ. Enzyme replacement therapy in alpha-mannosidosis guinea-pigs. Mol Genet Metab. 2006;89:48–57. doi: 10.1016/j.ymgme.2006.05.005. [DOI] [PubMed] [Google Scholar]
- DeLano WL. The PyMOL Molecular Graphics System. DeLano Scientific, Palo Alto, CA, USA; 2002. http://www.pymol.org [Google Scholar]


