Abstract
Objective
Patient–ventilator synchrony during non-invasive pressure support ventilation with the helmet device is often compromised when conventional pneumatic triggering and cycling-off were used. A possible solution to this shortcoming is to replace the pneumatic triggering with neural triggering and cycling-off—using the diaphragm electrical activity (EAdi). This signal is insensitive to leaks and to the compliance of the ventilator circuit.
Design
Randomized, single-blinded, experimental study.
Setting
University Hospital.
Participants and subjects
Seven healthy human volunteers.
Interventions
Pneumatic triggering and cycling-off were compared to neural triggering and cycling-off during NIV delivered with the helmet.
Measurements and results
Triggering and cycling-off delays, wasted efforts, and breathing comfort were determined during restricted breathing efforts (<20% of voluntary maximum EAdi) with various combinations of pressure support (PSV) (5, 10, 20 cm H2O) and respiratory rates (10, 20, 30 breath/min). During pneumatic triggering and cycling-off, the subject–ventilator synchrony was progressively more impaired with increasing respiratory rate and levels of PSV (p < 0.001). During neural triggering and cycling-off, effect of increasing respiratory rate and levels of PSV on subject–ventilator synchrony was minimal. Breathing comfort was higher during neural triggering than during pneumatic triggering (p < 0.001).
Conclusions
The present study demonstrates in healthy subjects that subject–ventilator synchrony, trigger effort, and breathing comfort with a helmet interface are considerably less impaired during increasing levels of PSV and respiratory rates with neural triggering and cycling-off, compared to conventional pneumatic triggering and cycling-off.
Electronic supplementary material
The online version of this article (doi:10.1007/s00134-008-1163-z) contains supplementary material, which is available to authorized users.
Keywords: Non-invasive ventilation (NIV), Helmet, Neurally triggered ventilatory assist, Neural control, Pressure support ventilation, Trigger
Introduction
Non-invasive ventilation (NIV) is an important complement to invasive mechanical ventilation [1–4] in patients with acute exacerbations of chronic obstructive pulmonary disease (COPD) [5], and with severe cardiogenic pulmonary edema [6].
Problems with the commonly used interfaces for NIV application include air leakage [7, 8], patient discomfort [9] and pressure-related ulcerations of the nose [10], which can limit the duration of use and account for a large proportion of NIV failures [11]. Navalesi and co-workers [8] demonstrated that the type of interface used for NIV is important with respect to patient tolerance and the time of NIV application. A new NIV interface, the helmet, has been introduced recently and was tested in different clinical situations [12–15]. The results are promising in terms of user acceptance [13]. However, due to the large collapsible and compliant chamber encompassing the patient’s head it significantly impairs patient–ventilator synchrony with conventional pneumatic systems [16, 17] and is less effective in reducing the work of breathing than the face mask [16, 18].
New methods for neural triggering and cycling-off, using the diaphragm electrical activity (EAdi), can be used to initiate and terminate ventilatory assist in synchrony with inspiratory efforts and, hence, may overcome some of the shortcomings of conventional pneumatic triggering and cycling-off with the helmet [19]. The aim of this study was to compare synchrony between inspiratory effort and ventilator assist, as well as breathing comfort during neurally or pneumatically triggered and cycled-off non-invasive pressure support ventilation delivered with the helmet interface in healthy volunteers.
Some of the data have been presented at the Congress of the European Society of Intensive Care Medicine in 2006 [20].
Materials and methods
Subjects
Seven healthy subjects (four female) were studied. Their mean (±SD) age, height and weight were 37 ± 5 years, 173 ± 10 cm and 67 ± 14 kg, respectively. Six subjects had prior knowledge about mechanical ventilation. The study was approved by the Research Ethics Committee of St. Michael’s Hospital in Toronto. Subjects gave their informed consent in writing.
Instrumentation
An 8-Fr catheter equipped with sensors for measurement of EAdi [21], and balloons for measurement of esophageal (P es) and gastric (P ga) pressure [22] were inserted transnasally into the stomach [21, 23]. EAdi sensors were positioned at the level of the diaphragm by online supervision of recorded electrical and pressure signals [23]. Airway pressure was measured inside the helmet close to the subject’s mouth. All signals were digitized at 2 kHz and stored on a personal computer for off-line evaluation. Expiratory muscle activity was monitored by the differential EMG signal from two surface electrodes placed 30-cm apart on either side of the mid-line of the upper abdominal wall.
All subjects received NIV with the helmet (Starmed Castar “R”, Mirandola, Italy) via a modified conventional ICU ventilator (Servo 300, Maquet Critical Care, Solna, Sweden).
NIV was delivered either with pneumatic trigger (Ptr) and cycling-off (Poff) or with neural trigger (Ntr) and cycling-off (Noff). Ptr and Ntr were adjusted to avoid auto-cycling, verified by performing a 10-s period of apnea (group mean value for Ptr was −1.3 ±SD 0.6 cm H2O). Conventional flow cycling-off (Poff) was 5% of peak inspiratory flow (default on Servo300). Ntr was set to trigger when the EAdi exceeded the random noise-variability. Noff occurred when EAdi fell to 60% of peak EAdi. During all runs, a PEEP of 5 cm H2O was applied.
Protocol
All subjects were studied while seated. The maximum EAdi
 was obtained by a maximal inspiratory maneuver [23]. Subsequently, during a practice period, subjects were instructed to follow a specific respiratory rate with a predetermined rate displayed as a time-line on a computer screen until they were able to maintain the predetermined respiratory rate (RR). Afterward the subjects repeated periods of breathing on the ventilator with RR of 10, 20, or 30 breaths per min (bpm), at pressure support (PSV) levels of 5, 10, or 20 cm H2O above PEEP (5 cm H2O). NIV was either neurally (Ntr and Noff) or pneumatically (Ptr and Poff) triggered and cycled-off. A total of 18 combinations of 2-min duration, were randomly performed using ballots. Before the 2-min period of data recording, each subject breathed until the new target respiratory rate and assist level was reached. Each measurement period was followed by 2 min of rest with CPAP of 5 cm H2O. Subjects were not informed about the applied PSV level, or the trigger type.
was obtained by a maximal inspiratory maneuver [23]. Subsequently, during a practice period, subjects were instructed to follow a specific respiratory rate with a predetermined rate displayed as a time-line on a computer screen until they were able to maintain the predetermined respiratory rate (RR). Afterward the subjects repeated periods of breathing on the ventilator with RR of 10, 20, or 30 breaths per min (bpm), at pressure support (PSV) levels of 5, 10, or 20 cm H2O above PEEP (5 cm H2O). NIV was either neurally (Ntr and Noff) or pneumatically (Ptr and Poff) triggered and cycled-off. A total of 18 combinations of 2-min duration, were randomly performed using ballots. Before the 2-min period of data recording, each subject breathed until the new target respiratory rate and assist level was reached. Each measurement period was followed by 2 min of rest with CPAP of 5 cm H2O. Subjects were not informed about the applied PSV level, or the trigger type.
To limit the subjects’ breathing efforts, the inspiratory effort was monitored by the investigators throughout the protocol period, and subjects were instructed to lower their inspiratory effort if EAdi exceeded 20% of the voluntary maximum EAdi. Subjects were also instructed to not use expiratory muscles (supervised by monitoring the abdominal EMG).
Subjects comfort of breathing was assessed by a visual analogue scale (VAS) (0 mm = maximal comfort to 100 mm = unbearable) and marked by the subjects themselves at the end of each study period.
Off-line data analysis
Ntr and Ptr delays were determined by measuring the time between the onset of EAdi and the onset of ventilatory assist using the internal signal of the ventilator. Trigger delays during Ntr NIPSV could vary (see ESM for details). Noff and Poff were determined by measuring the time between the point where EAdi was reduced to 60% of its peak value and the onset of expiratory flow. Mean EAdi, 
 and the corresponding pressure time products were calculated for the unassisted period of inspiration
and the corresponding pressure time products were calculated for the unassisted period of inspiration  and for the entire neural inspiration
and for the entire neural inspiration  The peak EAdi was calculated for each breath and was expressed as percentage of the maximum EAdi obtained during the maximum inspiratory maneuvers. Mean tidal excursion of P
es (ΔP
es) and the pressure time product for the P
es (PTPes) were calculated for the unassisted pre-trigger inspiratory phase
The peak EAdi was calculated for each breath and was expressed as percentage of the maximum EAdi obtained during the maximum inspiratory maneuvers. Mean tidal excursion of P
es (ΔP
es) and the pressure time product for the P
es (PTPes) were calculated for the unassisted pre-trigger inspiratory phase  and for the entire neural inspiratory period
and for the entire neural inspiratory period 
The number of wasted inspiratory efforts, i.e., failure to initiate PSV in the presence of a neural inspiratory effort is expressed as percentage of all neural efforts within the same time period.
For successfully triggered breaths, asynchrony was calculated over the whole breathing cycle on a breath by breath basis [24, 25] and was presented as a percentage of the duration of the neural breath (neural T tot). Wasted efforts were counted as 100% asynchrony.
Statistical analysis
Data are presented as median and 25th and 75th percentiles if not stated otherwise. Analysis was performed using non-parametric repeated measures analysis [26], corrected for multiple testing by Bonferroni correction and pair-wise comparisons (Wilcoxon test). A p value <0.05 was considered to be significant. Correlation between comfort of breathing and the percentage of asynchrony was calculated using the Spearman’s R statistic (see ESM for details).
Results
All subjects successfully followed the breathing instructions and reached the targeted breathing frequency, i.e., there was neither significant difference between the neural breathing frequency during Ptr and Ntr at the same PSV level nor was there a difference in the neural inspiratory times (Table 1).  (Ntr: 26.0, 24.1–28.3; Ptr: 26.6, 24.8–28.8, p = 0.08) and
(Ntr: 26.0, 24.1–28.3; Ptr: 26.6, 24.8–28.8, p = 0.08) and  (Ntr: 64.0, 35.5–92.4; Ptr: 69.7, 47.1–96.5, p = 0.43) were comparable during Ptr and Ntr. The EAdi levels during inspiration were maintained at 9.5% (5.2–12.6) and 10.1% (6.1–16.0) of the
(Ntr: 64.0, 35.5–92.4; Ptr: 69.7, 47.1–96.5, p = 0.43) were comparable during Ptr and Ntr. The EAdi levels during inspiration were maintained at 9.5% (5.2–12.6) and 10.1% (6.1–16.0) of the  during Ntr and Ptr, respectively. There was no difference in
during Ntr and Ptr, respectively. There was no difference in  between Ntr and Ptr at PSV levels of 5 cm H2O (p = 0.74) and 10 cm H2O (p = 0.33), whereas at PSV levels of 20 cm H2O the height of
between Ntr and Ptr at PSV levels of 5 cm H2O (p = 0.74) and 10 cm H2O (p = 0.33), whereas at PSV levels of 20 cm H2O the height of  differed significantly (p = 0.0098) Thus, overall
differed significantly (p = 0.0098) Thus, overall  was slightly higher during Ptr (Ntr: 38.6, 22.5–52.9; Ptr: 43.1, 28.5–59.9, p = 0.045) (Table 1).
was slightly higher during Ptr (Ntr: 38.6, 22.5–52.9; Ptr: 43.1, 28.5–59.9, p = 0.045) (Table 1).
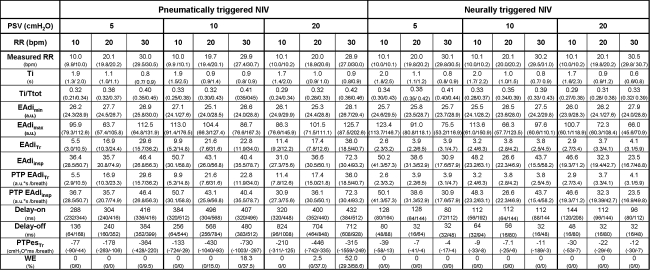
Table 1.
Pneumatic-triggered versus neural-triggered NIV at different levels of PSV and respiratory rates
There was no difference between mean measured respiratory rate (RR), neural inspiratory time, total inspiratory diaphragmatic activity  Inspiratory delay time (delay-on) (p < 0.001), expiratory cycling-off (delay-off) (p < 0.001)
Inspiratory delay time (delay-on) (p < 0.001), expiratory cycling-off (delay-off) (p < 0.001)  (p < 0.001),
(p < 0.001),  (p = 0.045) and the unassisted inspiratory effort
(p = 0.045) and the unassisted inspiratory effort  (p < 0.001) differed significantly. Wasted inspiratory efforts (WE) (expressed in percent of neural efforts) occurred at higher respiratory rates and levels of pressure support during Ptr while there were none during Ntr. Data are presented as median values (25th and 75th percentiles)
(p < 0.001) differed significantly. Wasted inspiratory efforts (WE) (expressed in percent of neural efforts) occurred at higher respiratory rates and levels of pressure support during Ptr while there were none during Ntr. Data are presented as median values (25th and 75th percentiles)
NIV non-invasive ventilation, PSV pressure support ventilation, RR respiratory rate, bpm breaths per minute, T
i neural inspiratory time, Tot total neural inspiratory and expiratory time, EA
di electrical diaphragmatic activity,  minimal and maximal EAdi during inspiration,
minimal and maximal EAdi during inspiration,  mean EAdi during inspiration,
mean EAdi during inspiration,  mean EAdi during unassisted phase of inspiration,
mean EAdi during unassisted phase of inspiration,  pressure time product of unassisted inspiratory phase and inspiration, delay-on time between onset of EAdi and the onset of ventilatory assist, delay-off time between end of neural T
i defined as reduction to 60% of peak activity and end of ventilator assist,
pressure time product of unassisted inspiratory phase and inspiration, delay-on time between onset of EAdi and the onset of ventilatory assist, delay-off time between end of neural T
i defined as reduction to 60% of peak activity and end of ventilator assist,  pressure time product of esophageal pressure during unassisted phase of inspiration, WE wasted inspiratory efforts
pressure time product of esophageal pressure during unassisted phase of inspiration, WE wasted inspiratory efforts
Subject–ventilator asynchrony
Figure 1 depicts tracings of EAdi and ventilator assist during neural and pneumatic triggering and cycling-off of NIV with the helmet in one healthy subject. Figure 2 shows differences between the delays during pneumatic and neural triggering. Ptr was delayed relative to Ntr (p < 0.001, Table 1), and the difference between the neural and pneumatic trigger delays increased (p < 0.001) as the level of PSV and RR increased (Fig. 2). During pneumatic triggering, the number of wasted inspiratory efforts increased at higher respiratory rates and with higher pressure support levels (Table 1). At a respiratory rate of 10 bpm, no wasted inspiratory efforts occurred regardless of the level of PSV, whereas at a PSV of 20 cm H2O, at a respiratory rate of 30 bpm, there was a significant increase of wasted efforts to 52.0% (29.3–58.6; p = 0.001) of all neural inspiratory efforts. No wasted inspiratory efforts occurred during neural control of NIV.
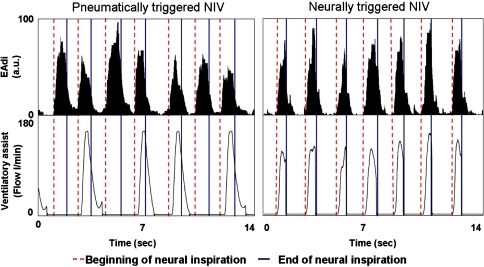
Fig. 1.
Example of diaphragm electrical activity (EAdi), and ventilatory assist during pneumatically (left panel) and neurally (right panel) triggered and cycled-off NIV in one healthy subject breathing with the helmet interface. In this example, respiratory rate was 30 bpm, PSV level was 20 cm H2O. The dashed line shows the start of neural inspiration and the continuous line shows the end of neural inspiration. Note excessive asynchrony during pneumatically triggered and cycled-off NIV
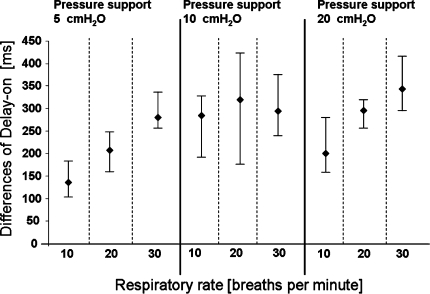
Fig. 2.
Differences in inspiratory delays (delay time Ptr − delay time Ntr) during NIV with a pressure support of 5, 10 and 20 cm H2O and respiratory rates of 10, 20 and 30 bpm were shown. During all combinations of respiratory rates and pressure support levels, there was a significant difference in inspiratory delays being highly increased during pneumatically triggered NIV. Symbols represent group median values and the bars indicate 25th and 75th percentiles. Delay-on inspiratory delay between the onset of the volunteers’ inspiratory effort and the start of the ventilatory support, P tr pneumatic trigger, N tr neural trigger, NIV non-invasive ventilation
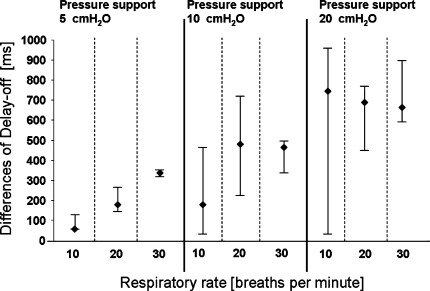
The expiratory delay for all combinations of PSV levels and RR during Poff was longer than during Noff (p < 0.001) (Table 1), and the expiratory delays during Poff became longer with increasing PSV levels and target RR compared to Noff (p < 0.001) as depicted in Fig. 3.
Fig. 3.
Differences in expiratory delays (delay time Poff − delay time Noff) during NIV with PSV of 5, 10 and 20 cm H2O and respiratory rates of 10, 20 and 30 bpm were shown. During all combinations of respiratory rates and pressure support levels, there was a significant difference in expiratory delays that were highly increased during pneumatically triggered NIV. Symbols represent group median values and the bars indicate 25th and 75th percentiles. Delay-off delay between the onset neural end of inspiration and the end of the ventilatory support, P off pneumatic cycling-off, N off neural cycling-off, NIV non-invasive ventilation
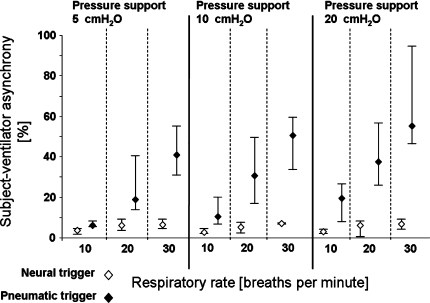
Overall, the subject–ventilator synchrony was progressively impaired with increasing respiratory rate and levels of PSV during pneumatic triggering and cycling-off as depicted in Fig. 4, (p < 0.001). In contrast, increasing respiratory rate and levels of assists only had negligible influence on the asynchrony during neural triggering and cycling-off (Fig. 4).
Fig. 4.
Percentage of asynchrony over the whole breath duration as calculated during Ntr and Ptr NIV: (delay-on + delay-off/neural T tot × 100). Wasted inspiratory efforts were counted as 100% asynchrony. Percentage of asynchrony during Ptr was markedly higher compared to Ntr. Symbols represent group median values and the bars indicate 25th and 75th percentiles. N tr neurally triggered, P tr pneumatically triggered, NIV non-invasive ventilation, PSV pressure support ventilation
Unassisted “pre-trigger” inspiratory effort during PSV
Depending on the combination between PSV and target RR, the efforts to trigger the ventilator were 5–60 times higher during Ptr than during Ntr. Median  during Ntr was 3.4 (2.7–4.2) compared to 16.9 (10.2–26.6) during Ptr (p < 0.001). For all combinations, the
during Ntr was 3.4 (2.7–4.2) compared to 16.9 (10.2–26.6) during Ptr (p < 0.001). For all combinations, the  during Ptr was −264 (−470 to −130) cm H20 ms per breath compared to −11.7 (−30.6 to −6.2; p < 0.001) during Ntr (Table 1). The median
during Ptr was −264 (−470 to −130) cm H20 ms per breath compared to −11.7 (−30.6 to −6.2; p < 0.001) during Ntr (Table 1). The median  expressed as percent of
expressed as percent of  was 21.5% (11.1–23.5) during Ptr and significantly lower during Ntr, 1.4% (0.9–1.6) (p < 0.001).
was 21.5% (11.1–23.5) during Ptr and significantly lower during Ntr, 1.4% (0.9–1.6) (p < 0.001).
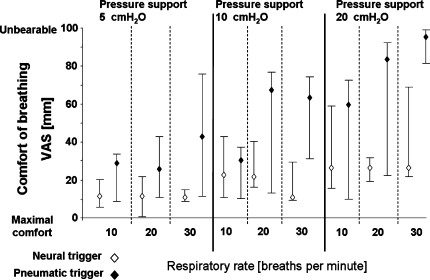
Comfort of breathing
Breathing comfort was lower during P tr than during N tr in 84.4% of all runs (p < 0.001) (Fig. 5). Overall, comfort of breathing was more than two times worse during pneumatic triggering compared to neural triggering [P tr median 43.0 mm (20.2–75.6) vs. N tr 19.2 mm (10.1–28.5)]. Increasing the respiratory rate resulted in minor changes of breathing comfort during neural triggering (p = 0.003), while there was a reduction in breathing comfort during pneumatic triggering (p = 0.953). Increasing PSV at a given respiratory rate tended to decrease breathing comfort during both neural triggering and pneumatic triggering, although the reduction in comfort tended to be larger with pneumatic triggering (Fig. 5). During pneumatic triggering, comfort of breathing was significantly correlated with the amount of asynchrony (r = 0.59, p < 0.001), whereas no such correlation was observed during neural triggering (r = −0.146, p = 0.253).
Fig. 5.
Breathing comfort in mm as assessed by a visual analogue scale during neurally and pneumatically triggered and cycled-off NIV at different levels of assist and respiratory rates (0 very comfortable, 100 unbearable). During all combinations of respiratory rates and PSV levels, comfort of breathing was better during neurally triggered and cycled-off NIV. Symbols represent group median values and the bars indicate 25th and 75th percentiles. NIV non-invasive ventilation, PSV pressure support ventilation, VAS visual analogue scale
Discussion
The present study demonstrates that the airway pressure generated by healthy subjects using ~10% of their maximal EAdi was less efficient to pneumatically control PSV with the helmet interface at increasing breathing frequencies and pressure support levels compared to a neural trigger and cycling-off algorithm using EAdi. Due to the trigger asynchrony during Ptr, also the neural and mechanical efforts during Ptr became several times higher than during Ntr. This suggests that during NIV with pneumatic triggering, it is necessary to force the ventilator into synchrony by increasing inspiratory effort, which would defeat the purpose of providing ventilatory assist.
Previous studies comparing the helmet to the face mask interface during pneumatically triggered and cycled-off PSV show that the helmet is less effective in unloading the respiratory muscles, which was partially explained by inspiratory trigger delays and the impaired pressurization rate [16–18].
The difference in trigger delays between Ntr and Ptr could not be due to mechanical response of the ventilator since NIV was delivered with the same ventilator throughout the study. Hence, apart from changes in trigger delays, no changes in raised time or pressure delivery could occur.
A critique on the present study was that a pressure trigger of −1.3 ± 0.6 cm H2O was required to avoid auto-triggering. This likely increased trigger delays and the fraction of the pressure time product necessary to pneumatically trigger the ventilator [27]. In the absence of leaks, studies suggest that flow triggering is more efficient than pressure triggering [28, 29]. However, there are also results in favor of pressure triggering [30]. The reported improvements of delays between flow and pressure triggering (40–43) are not of a magnitude that can match the improvement of implementing neural trigger relative to pressure trigger using a helmet interface in the present study. In fact, the trigger delays during Ptr were similar to those observed with helmet interface in previous studies, whereas the trigger delays during Ntr in the present study are within the range of those reported with face mask in previous studies [16–18]. Since the helmet interface is presumed to be frequently associated with leaks, which makes triggering and cycling very complex [31], it is questionable whether flow triggering is recommendable. It should be noted that in the present study, increasing breathing frequency and assist levels only increased trigger delays and  during Ptr and not during Ntr.
during Ptr and not during Ntr.
With regard to wasted inspiratory efforts, which are the worst type of trigger asynchrony, a previous study did not report wasted efforts during NIV (5 cm H2O) with helmet and face mask in a study with healthy volunteers who kept their breathing frequency around 15 bpm [12]. In a lung model study using the helmet interface, wasted inspiratory efforts occurred at a respiratory rate above 20 bpm (PSV level of 18 cm H2O) and were negatively influenced by increasing PEEP and PSV levels [17]. In the present study, where both inspiratory and expiratory efforts were monitored and restricted, wasted inspiratory efforts prevailed at highest PSV (20 cm H2O) or RR (30 bpm) levels.
Looking at the baseline characteristics of patients requiring non-invasive ventilatory support due to ARF respiratory rates above 30 would be expected [32–34]. Thus, compared to our results where RR did not exceed 30 bpm, the amount of wasted efforts might be even higher. With regard to Ntr, increasing frequencies above 30 bpm should not increase the risk of wasted inspiratory efforts.
In terms of cycling-off the PSV, the ventilator used in the present study included a fixed cycling-off algorithm that terminates assist when flow has dropped to 5% of peak inspiratory flow. Given that the addition of the compliant helmet into the respiratory circuit increases the time constant of the total respiratory system (helmet, respiratory circuit and respiratory system) the late pneumatic cycling-off at 5% of peak inspiratory flow is likely not ideal. To match flow cycling-off with neural inspiratory termination, Du et al. [35] demonstrated that prolonging the time constant of the total respiratory system requires that flow cycles-off at a higher percentage of peak inspiratory flow. The need for varying flow cycling-off criteria suggested to match neural breath termination has been demonstrated in obstructive patients where the flow cycling-off had to take place at about 50% of peak inspiratory flow [36], whereas 5% appears sufficient in patients with restrictive lung disease [37]. However, since the time constant of the respiratory system (and the helmet) changes as the pressure assist level and/or breathing frequency change—and that there is currently no standard to what percentages of peak flow should be used to cycle-off at various levels of assist—the authors chose to let the cycling-off criteria be dictated by the ventilator used.
Since the present study compared different levels of PSV and breathing frequency and that the results are presented as the difference in cycling-off delays between pneumatic and neural cycling-off at the same level of PSV and RR, our findings should be adequate in terms of comparing changes in time delays for cycling-off during Poff compared to Noff with increasing respiratory rates and PSV levels. It should be noted that the findings of increasing cycling-off delays during increasing levels of pneumatically controlled PSV observed in the present study agree with previous studies on PSV in intubated patients [27, 38]. The findings of the present study substantiate that neural off-cycling with EAdi can reduce the problem of excessive prolongation of assist into neural exhalation and its associated influence on breathing pattern [24, 38].
As indicated by the asynchrony percentage as high as 30% during pneumatically triggered and cycled NIV, which was reduced to 5% during neurally triggered and cycled-off NIV, the advantage of the latter appears undisputable with regard to helmet ventilation. Our data confirm those of Racca et al. [39] that wasted efforts and impaired trigger synchrony are likely due to the properties of the helmet itself, being a collapsible device that will dampen the transmission of pressures delivered to the patient as well as reduce the ability to sense the pressure generated by the patient. Thus, the present study suggests that neural triggering can achieve an important reduction in the trigger effort with a helmet device.
In the present study, breathing comfort was rated closer to maximal comfort when PSV and RR were low, which was in contrast to observations in patients with ARF. Vitacca et al. [40] reported that the highest level of comfort in patients on NIV with acute exacerbation of COPD occurred at a PSV level of 17 + 6 cm H2O and a breathing frequency of 18 + 6 bpm.
During neurally triggered and cycled-off PSV, our findings showed that comfort decreased with increasing PSV levels at similar breathing frequency despite no changes in subject–ventilator asynchrony was observed. Thus, it is reasonable to assume that in healthy subjects “no assist” equals maximal comfort and increased PSV is associated with a decrease in comfort. Hence, one should be careful in interpreting the findings of the present study in relation to a patient population with respiratory failure.
However, as evidenced by the strong correlations found between asynchrony and comfort during pneumatically triggered and cycled-off NIV, which was abolished during neurally controlled NIV, subject–ventilator asynchrony plays an important role in the perception of breathing comfort. It should be noted that adding a nasogastric tube is uncomfortable. However, given the complications of endotracheal intubation, it appears reasonable to examine the possible advantage of trading tracheal for esophageal invasiveness, using non-invasive interfaces.
Conclusion
The present study demonstrates in healthy subjects that subject–ventilator synchrony, trigger effort, and breathing comfort with a helmet interface is considerably less impaired during increasing levels of PSV and respiratory rates with neural triggering and cycling-off, compared to conventional pneumatic triggering and cycling-off.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
We are indebted to the volunteers for their participation, to Norman Comtois for his invaluable assistance, and to Orla Smith, RN and her team for the coordination given during the study. Statistical analysis of the data was performed after advisory service of the Department of Medical Statistics, University of Göttingen, Germany, with special gratitude to Dr. E. Kahler. This study was financed by departmental funds from the Department of Critical Care Medicine, St. Michael’s Hospital, University of Toronto, Canada and the Department of Anesthesiology, Emergency and Critical Care Medicine, University of Göttingen, Germany. Onnen Moerer holds a research grant from a research program, Faculty of Medicine, Georg-August-University Göttingen. Lukas Brander hold postdoctoral fellowships from the Swiss Foundation for Fellowships in Medicine and Biology (SSMBS) provided by Novartis AG and from the Division of Respirology at the University of Toronto provided by Merck-Frosst. Dr. Sinderby was financially supported by “R. Samuel McLaughlin Foundation”.
Conflict of interest
Dr. Beck and Dr. Sinderby have made inventions related to neural control of mechanical ventilation that are patented. The license for these patents belongs to Maquet Critical Care. Future commercial uses of this technology may provide financial benefit to Dr. Beck and Dr. Sinderby through royalties. Dr. Beck and Dr. Sinderby each own 50% of Neurovent Research Inc (NVR). NVR is a research and development company that builds the equipment and catheters for research studies. NVR has a consulting agreement with Maquet Critical Care. Dr. Slutsky consults for companies that make ventilators, specifically, Maquet Critical Care and Hamilton Medical, and is compensated for these consultations St. Michael's Hospital will get a small royalty if Maquet includes SMH-patented discoveries in the ventilator.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
This article is discussed in the editorial available at: doi:10.1007/s00134-008-1164-y.
References
- 1.Ferrer M, Valencia M, Nicolas JM, Bernadich O, Badia JR, Torres A. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med. 2006;173:164–170. doi: 10.1164/rccm.200505-718OC. [DOI] [PubMed] [Google Scholar]
- 2.Ferrer M, Esquinas A, Arancibia F, Bauer TT, Gonzalez G, Carrillo A, Rodriguez-Roisin R, Torres A. Noninvasive ventilation during persistent weaning failure: a randomized controlled trial. Am J Respir Crit Care Med. 2003;168:70–76. doi: 10.1164/rccm.200209-1074OC. [DOI] [PubMed] [Google Scholar]
- 3.Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L. Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med. 2001;163:874–880. doi: 10.1164/ajrccm.163.4.2006027. [DOI] [PubMed] [Google Scholar]
- 4.Brochard L, Mancebo J, Wysocki M, Lofaso F, Conti G, Rauss A, Simonneau G, Benito S, Gasparetto A, Lemaire F. Noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease. N Engl J Med. 1995;333:817–822. doi: 10.1056/NEJM199509283331301. [DOI] [PubMed] [Google Scholar]
- 5.Ram FS, Picot J, Lightowler J, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2004;3:CD004104. doi: 10.1002/14651858.CD004104.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Winck JC, Azevedo LF, Costa-Pereira A, Antonelli M, Wyatt JC. Efficacy and safety of non-invasive ventilation in the treatment of acute cardiogenic pulmonary edema—a systematic review and meta-analysis. Crit Care. 2006;10:R69. doi: 10.1186/cc4905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Conti G, Antonelli M, Navalesi P, Rocco M, Bufi M, Spadetta G, Meduri GU. Noninvasive vs. conventional mechanical ventilation in patients with chronic obstructive pulmonary disease after failure of medical treatment in the ward: a randomized trial. Intensive Care Med. 2002;28:1701–1707. doi: 10.1007/s00134-002-1478-0. [DOI] [PubMed] [Google Scholar]
- 8.Navalesi P, Fanfulla F, Frigerio P, Gregoretti C, Nava S. Physiologic evaluation of noninvasive mechanical ventilation delivered with three types of masks in patients with chronic hypercapnic respiratory failure. Crit Care Med. 2000;28:1785–1790. doi: 10.1097/00003246-200006000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Kramer N, Meyer TJ, Meharg J, Cece RD, Hill NS. Randomized, prospective trial of noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med. 1995;151:1799–1806. doi: 10.1164/ajrccm.151.6.7767523. [DOI] [PubMed] [Google Scholar]
- 10.Gregoretti C, Confalonieri M, Navalesi P, Squadrone V, Frigerio P, Beltrame F, Carbone G, Conti G, Gamna F, Nava S, Calderini E, Skrobik Y, Antonelli M. Evaluation of patient skin breakdown and comfort with a new face mask for non-invasive ventilation: a multi-center study. Intensive Care Med. 2002;28:278–284. doi: 10.1007/s00134-002-1208-7. [DOI] [PubMed] [Google Scholar]
- 11.Antonelli M, Pennisi MA, Conti G. New advances in the use of noninvasive ventilation for acute hypoxaemic respiratory failure. Eur Respir J Suppl. 2003;42:65s–71s. doi: 10.1183/09031936.03.00421003. [DOI] [PubMed] [Google Scholar]
- 12.Chiumello D, Pelosi P, Carlesso E, Severgnini P, Aspesi M, Gamberoni C, Antonelli M, Conti G, Chiaranda M, Gattinoni L. Noninvasive positive pressure ventilation delivered by helmet vs. standard face mask. Intensive Care Med. 2003;29:1671–1679. doi: 10.1007/s00134-003-1825-9. [DOI] [PubMed] [Google Scholar]
- 13.Antonelli M, Conti G, Pelosi P, Gregoretti C, Pennisi MA, Costa R, Severgnini P, Chiaranda M, Proietti R. New treatment of acute hypoxemic respiratory failure: noninvasive pressure support ventilation delivered by helmet—a pilot controlled trial. Crit Care Med. 2002;30:602–608. doi: 10.1097/00003246-200203000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Pelosi P, Severgnini P, Aspesi M, Gamberoni C, Chiumello D, Fachinetti C, Introzzi L, Antonelli M, Chiaranda M. Non-invasive ventilation delivered by conventional interfaces and helmet in the emergency department. Eur J Emerg Med. 2003;10:79–86. doi: 10.1097/00063110-200306000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Patroniti N, Foti G, Manfio A, Coppo A, Bellani G, Pesenti A. Head helmet versus face mask for non-invasive continuous positive airway pressure: a physiological study. Intensive Care Med. 2003;29:1680–1687. doi: 10.1007/s00134-003-1931-8. [DOI] [PubMed] [Google Scholar]
- 16.Navalesi P, Costa R, Ceriana P, Carlucci A, Prinianakis G, Antonelli M, Conti G, Nava S. Non-invasive ventilation in chronic obstructive pulmonary disease patients: helmet versus facial mask. Intensive Care Med. 2006;33:74–81. doi: 10.1007/s00134-006-0391-3. [DOI] [PubMed] [Google Scholar]
- 17.Moerer O, Fischer S, Hartelt M, Kuvaki B, Quintel M, Neumann P. Influence of two different interfaces for noninvasive ventilation compared to invasive ventilation on the mechanical properties and performance of a respiratory system: a lung model study. Chest. 2006;129:1424–1431. doi: 10.1378/chest.129.6.1424. [DOI] [PubMed] [Google Scholar]
- 18.Racca F, Appendini L, Gregoretti C, Stra E, Patessio A, Donner CF, Ranieri VM. Effectiveness of mask and helmet interfaces to deliver noninvasive ventilation in a human model of resistive breathing. J Appl Physiol. 2005;99:1262–1271. doi: 10.1152/japplphysiol.01363.2004. [DOI] [PubMed] [Google Scholar]
- 19.Sinderby C, Navalesi P, Beck J, Skrobik Y, Comtois N, Friberg S, Gottfried SB, Lindstrom L. Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999;5:1433–1436. doi: 10.1038/71012. [DOI] [PubMed] [Google Scholar]
- 20.Moerer O, Beck J, Brander L, Quintel M, Brunet F, Sinderby C. Subject–ventilator synchrony during neural vs. pressure triggered non-invasive helmet ventilation. Intensive Care Med. 2006;32:148. doi: 10.1007/s00134-008-1163-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sinderby CA, Beck JC, Lindstrom LH, Grassino AE. Enhancement of signal quality in esophageal recordings of diaphragm EMG. J Appl Physiol. 1997;82:1370–1377. doi: 10.1152/jappl.1997.82.4.1370. [DOI] [PubMed] [Google Scholar]
- 22.Benditt JO. Esophageal and gastric pressure measurements. Respir Care. 2005;50:68–75. [PubMed] [Google Scholar]
- 23.Sinderby C, Beck J, Spahija J, Weinberg J, Grassino A. Voluntary activation of the human diaphragm in health and disease. J Appl Physiol. 1998;85:2146–2158. doi: 10.1152/jappl.1998.85.6.2146. [DOI] [PubMed] [Google Scholar]
- 24.Beck J, Tucci M, Emeriaud G, Lacroix J, Sinderby C. Prolonged neural expiratory time induced by mechanical ventilation in infants. Pediatr Res. 2004;55:747–754. doi: 10.1203/01.PDR.0000119368.21770.33. [DOI] [PubMed] [Google Scholar]
- 25.Beck J, Campoccia F, Allo JC, Brander L, Brunet F, Slutsky AS, Sinderby C. Improved synchrony and respiratory unloading by neurally adjusted ventilatory assist (NAVA) in lung-injured rabbits. Pediatr Res. 2007;61:289–294. doi: 10.1203/01.pdr.0000257324.22406.93. [DOI] [PubMed] [Google Scholar]
- 26.Brunner E, Domhof S, Langer F. Nonparametric analysis of longitudinal data in factorial experiments. New York: Wiley; 2002. [Google Scholar]
- 27.Aslanian P, el Atrous S, Isabey D, Valente E, Corsi D, Harf A, Lemaire F, Brochard L. Effects of flow triggering on breathing effort during partial ventilatory support. Am J Respir Crit Care Med. 1998;157:135–143. doi: 10.1164/ajrccm.157.1.96-12052. [DOI] [PubMed] [Google Scholar]
- 28.Giuliani R, Mascia L, Recchia F, Caracciolo A, Fiore T, Ranieri VM. Patient–ventilator interaction during synchronized intermittent mandatory ventilation. Effects of flow triggering. Am J Respir Crit Care Med. 1995;151:1–9. doi: 10.1164/ajrccm.151.1.7812537. [DOI] [PubMed] [Google Scholar]
- 29.Nava S, Ambrosino N, Bruschi C, Confalonieri M, Rampulla C. Physiological effects of flow and pressure triggering during non-invasive mechanical ventilation in patients with chronic obstructive pulmonary disease. Thorax. 1997;52:249–254. doi: 10.1136/thx.52.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goulet R, Hess D, Kacmarek RM. Pressure vs flow triggering during pressure support ventilation. Chest. 1997;111:1649–1653. doi: 10.1378/chest.111.6.1649. [DOI] [PubMed] [Google Scholar]
- 31.Calderini E, Confalonieri M, Puccio PG, Francavilla N, Stella L, Gregoretti C. Patient–ventilator asynchrony during noninvasive ventilation: the role of expiratory trigger. Intensive Care Med. 1999;25:662–667. doi: 10.1007/s001340050927. [DOI] [PubMed] [Google Scholar]
- 32.Ray P, Birolleau S, Lefort Y, Becquemin MH, Beigelman C, Isnard R, Teixeira A, Arthaud M, Riou B, Boddaert J. Acute respiratory failure in the elderly: etiology, emergency diagnosis and prognosis. Crit Care. 2006;10:R82. doi: 10.1186/cc4926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Honrubia T, Garcia Lopez FJ, Franco N, Mas M, Guevara M, Daguerre M, Alia I, Algora A, Galdos P. Noninvasive vs conventional mechanical ventilation in acute respiratory failure: a multicenter, randomized controlled trial. Chest. 2005;128:3916–3924. doi: 10.1378/chest.128.6.3916. [DOI] [PubMed] [Google Scholar]
- 34.Phua J, Kong K, Lee KH, Shen L, Lim TK. Noninvasive ventilation in hypercapnic acute respiratory failure due to chronic obstructive pulmonary disease vs. other conditions: effectiveness and predictors of failure. Intensive Care Med. 2005;31:533–539. doi: 10.1007/s00134-005-2582-8. [DOI] [PubMed] [Google Scholar]
- 35.Du HL, Amato MB, Yamada Y. Automation of expiratory trigger sensitivity in pressure support ventilation. Respir Care Clin N Am. 2001;7:503–517. doi: 10.1016/S1078-5337(05)70046-0. [DOI] [PubMed] [Google Scholar]
- 36.Tassaux D, Gainnier M, Battisti A, Jolliet P. Impact of expiratory trigger setting on delayed cycling and inspiratory muscle workload. Am J Respir Crit Care Med. 2005;172:1283–1289. doi: 10.1164/rccm.200407-880OC. [DOI] [PubMed] [Google Scholar]
- 37.Tokioka H, Tanaka T, Ishizu T, Fukushima T, Iwaki T, Nakamura Y, Kosogabe Y. The effect of breath termination criterion on breathing patterns and the work of breathing during pressure support ventilation. Anesth Analg. 2001;92:161–165. doi: 10.1097/00000539-200101000-00031. [DOI] [PubMed] [Google Scholar]
- 38.Younes M, Kun J, Webster K, Roberts D. Response of ventilator-dependent patients to delayed opening of exhalation valve. Am J Respir Crit Care Med. 2002;166:21–30. doi: 10.1164/rccm.2107143. [DOI] [PubMed] [Google Scholar]
- 39.Racca F, Appendini L, Gregoretti C, Stra E, Patessio A, Donner CF, Ranieri VM. Effectiveness of mask and helmet interfaces to deliver noninvasive ventilation in a human model of resistive breathing. J Appl Physiol. 2005;99(4):1262–1271. doi: 10.1152/japplphysiol.01363.2004. [DOI] [PubMed] [Google Scholar]
- 40.Vitacca M, Bianchi L, Zanotti E, Vianello A, Barbano L, Porta R, Clini E. Assessment of physiologic variables and subjective comfort under different levels of pressure support ventilation. Chest. 2004;126:851–859. doi: 10.1378/chest.126.3.851. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.