Abstract
Background
Although several studies have reported positive effects of mindfulness-based stress reduction (MBSR) intervention on psychological well-being, it is not known whether these effects are attributable to a change in mindfulness.
Purpose
The aim of this study is to compare the effects of MBSR to a waiting-list control condition in a randomized controlled trial while examining potentially mediating effects of mindfulness.
Methods
Forty women and 20 men from the community with symptoms of distress (mean age 43.6 years, SD = 10.1) were randomized into a group receiving MBSR or a waiting-list control group. Before and after the intervention period, questionnaires were completed on psychological well-being, quality of life, and mindfulness.
Results
Repeated measures multiple analysis of variance (MANCOVAs) showed that, compared with the control group, the intervention resulted in significantly stronger reductions of perceived stress (p = 0.016) and vital exhaustion (p = 0.001) and stronger elevations of positive affect (p = 0.006), quality of life (p = .009), as well as mindfulness (p = 0.001). When mindfulness was included as a covariate in the MANCOVA, the group effects on perceived stress and quality of life were reduced to nonsignificance.
Conclusion
Increased mindfulness may, at least partially, mediate the positive effects of mindfulness-based stress reduction intervention.
Keywords: Mindfulness, Stress management, Well-being, Quality of life, Randomized controlled trial
Introduction
Mindfulness-based interventions aimed at reduction of psychological symptoms of distress and enhancement of quality of life [1, 2] are increasingly applied and popular in various kinds of settings in both mental health care and somatic health care [3–5]. These interventions are aiming at the cultivation of an open-minded and non-judgmental awareness of whatever is happening at each successive moment of perception. The objects of perception, which is direct and pre-reflexive, include the whole range of possible phenomena, from internal psychological states and processes (thoughts, feelings, images, etc.), proprioceptive information from the body, to external stimuli entering the senses. Phenomena are approached in an open, nonjudgmental and accepting way. It is “the clear and single-minded awareness of what actually happens to us and in us at the successive moments of perception” [6]. The approach is rooted in the core Buddhist notion that all psychological suffering is the result of the judgmental mind, dividing experiences into good and bad, which should be either strived for or avoided, inevitably leading to some level of frustration, distress, anxiety, and depression.
Several studies have been performed, especially in recent years, that have examined the effects of mindfulness-based stress reduction interventions, mainly in the form of the original MBSR protocol [1, 2] or derivatives thereof [3, 4]. Although some studies have been methodologically limited, such as not having included a control group [2, 7, 8], beneficial effects have been reported in diverse samples of patients and general population regarding a variety of psychological states, including symptoms of general distress [9–12], worry, rumination, and anxiety [13, 14], depressive symptoms [9, 10, 15], sleep quality [16, 17], pain [2, 18, 19], and quality of life [11, 20, 21]. Although results regarding symptoms of depression and anxiety have sometimes been equivocal [22], in general, MBSR has shown positive effects in different groups, such as chronic pain patients [2, 19], medical and premedical students [15], health care professionals [12], patients with fibromyalgia [19, 23], patients with heart disease [24], and cancer outpatients [10, 11, 25]. A meta-analysis on the available randomized controlled trials has shown a mean medium-sized (d = 0.54) effect on a composite score of psychological well-being [4].
Although the effects of MBSR on psychological well-being is beginning to get well established, the central assumption stating that the effects are attributable to increases in mindfulness skills induced by the training has hardly been studied [20]. Since the recent introduction of instruments assessing various aspects of mindfulness [20, 26], the first published studies on this topic have not been able to illuminate this issue. While some studies found correlations between pre- to post-intervention change in mindfulness and change in perceived stress and mood [7, 20, 27], a mediation effect could not be examined due to a lack of a control group in these studies.
An additional issue regarding the efficacy of MBSR is the question to what extent regular daily practice is necessary for obtaining the beneficial effects of the intervention as claimed [1]. Results of studies examining this issue have been inconsistent [9, 10, 13, 17, 27]. Methodological differences between the studies, including the outcome variables used, and varying power to detect effects may have been responsible for the inconsistencies.
In the present study, our main aim was to examine the extent to which effects of the mindfulness-based stress reduction intervention protocol may be attributable to increases in mindfulness skills induced by the training. Various measures of psychological well-being and quality of life were included, from general positive and negative affect and perceived stress to aspects of quality of life. We expected that, in general, change in mindfulness would statistically mediate the beneficial effects of the intervention on study outcomes. In addition, the association of the amount of home practice and attendance to the intervention sessions with outcome was examined, which was expected to be positive and significant [1].
Method
Participants
Participants were recruited in September 2005 by an advertisement in local papers around the city of Tilburg, The Netherlands, including the following solicitation: “In fall, a mindfulness-based training aiming at reducing feelings of distress will start at Tilburg University. […] Because this training is linked to an investigation into its precise effectiveness, the training is offered for free.” When participants applied (by phone), we verified if they had symptoms of distress by asking the question “how often would you say do you feel distressed?” Participants were eligible if they replied that they felt this way at least “regularly” or “often.” They were also asked if they had a psychological disorder that was present for at least 2 months. Serious psychopathology (e.g., suicidal ideation) and insufficient understanding of the Dutch language were the exclusion criteria. All people that were interested in participating complied with these criteria.
The power analysis was based upon a previous meta-analysis on the effects of MBSR on psychological well-being variables, showing a mean medium-sized effect size (d = 0.5). With an alpha level of 0.05 and a power of 0.80, a total of 50 participants were needed. Sixty participants with symptoms of distress volunteered and met the criteria for inclusion in the trial. They were randomized into an intervention group that would receive the MBSR training and a waiting-list control group that would receive MBSR after the intervention group finished their training. Random selection of the MBSR participants without stratification was performed using the SPSS software procedure ‘random selection of cases’ applied to numbers representing the participants. The performer of this procedure (second author) did not know which number represented which participant. After randomization, there was no blinding to group assignment, except for assessment of the outcomes, which was done by sending questionnaires to the participants by post.
The study was approved by the Medical Ethics Committee of the St. Elisabeth Hospital at Tilburg, The Netherlands.
Measures
Demographic Data
The questionnaire set included sociodemographic and medical questions regarding the participants’ age, sex, education, job status, current treatment, and medication.
Psychological Well-being
Psychological well-being was assessed by using the following four constructs: perceived stress, vital exhaustion, positive affect, and negative affect. The Perceived Stress Scale (PSS) [28] assesses the degree to which situations in one’s life are appraised as stressful. The PSS consists of 14 items, which are scored by using five-point Likert scales ranging from 0 (never) to 4 (very often). The PSS has an internal consistency (Cronbach’s α) coefficient of 0.85 and well-established validity [28, 29]. This was our primary outcome measure. Secondary outcomes were vital exhaustion, positive and negative affect, quality of life, and mindfulness skills.
Vital exhaustion, a mental state characterized by unusual fatigue, a feeling of being dejected or defeated, and increased irritability was assessed by means of the Maastricht Questionnaire (MQ) [30], ‘form B.’ This questionnaire consists of 21 items that can be answered with yes, do not know, or no, and has a Cronbach’s α of 0.89 [31]. It has been shown to have adequate concurrent validity as reflected by a substantial correlation with a validated interview-derived assessment of vital exhaustion [32] as well as predictive validity [30].
The Global Mood Scale (GMS) [33] was used to measure negative affect (characterized by fatigue and malaise) and positive affect (characterized by energy and sociability). This questionnaire comprises 20 items, of which ten are positive and ten reflect negative mood. By using a five-point Likert scale ranging from 0 (not at all) to 4 (extremely), respondents are asked to indicate to what extent they experienced each emotion lately. The GMS has been found to be an internally consistent scale (Cronbach’s α > 0.90), and correlations with existing measures of emotional functioning and self-deception indicated its convergent and discriminant validity [33].
Quality of Life
The World Health Organization Quality of Life (WHOQOL) group has designed the WHOQoL-Bref [34], which is a shortened version of the WHOQoL-100 quality of life questionnaire. In this study, the WHOQoL-Bref was used to obtain contentment in five domains of quality of life: physical health, psychological health, social relationships, environment, and general quality of life. The WHOQoL-Bref consists of 26 items and has been reported to show satisfactory internal consistency (Cronbach’s α ranging from 0.66 for the social domain to 0.82 for physical health). It also has adequate test–retest reliability and discriminant validity [34].
Mindfulness
Mindfulness was assessed by means of a combination of the Mindful Attention Awareness Scale (MAAS) [20] and two subscales from the Kentucky Inventory of Mindfulness Skills (KIMS) [35]: Observe and Accept Without Judgment.
The MAAS assesses to what extent an individual is attentive to and aware of what is taking place in the present. It consists of 15 items. Respondents have to indicate how frequently they currently experienced each condition, using a six-point Likert scale from 1 (almost always) to 6 (almost never). The MAAS is a reliable instrument with a Cronbach’s α of 0.87. Adequate test–retest reliability, convergent, and discriminant validity have also been reported [20].
The KIMS measures four components of being mindful in daily life: Observe (12 items), Describe (eight items), Act With Awareness (ten items), and Accept Without Judgment (nine items). Each of the 39 items is scored on five-point Likert scales ranging from 1 (never or very rarely true) to 5 (almost always or always true). The subscale Act With Awareness was not included in the present study because its content is largely overlapping with the content of the MAAS and the subscale Describe was omitted because describing one’s emotions and feelings is not a primary focus of MBSR, while observing whatever happens in the present moment (reflected by the subscale Observe) and especially a nonjudgmental and nonevaluative attitude (reflected by the subscale Accept Without Judgment) are important aspects of the intervention [4]. The Cronbach’s α coefficients for the subscales Observe and Accept Without Judgment have been found to be 0.91 and 0.87, respectively, which reflects a high internal consistency. Adequate test–retest reliability and content validity have also been found [35].
All items of the MAAS and the two subscales of the KIMS were translated into Dutch and back to English by three independent translators reaching the final version by consensus. The Cronbach’s α coefficients of these scales at baseline and at follow-up in the present study were 0.82 and 0.86 for the MAAS, 0.86 and 0.89 for Accept Without Judgment, and 0.87 and 0.89 for Observe, respectively. In addition, the pattern of intercorrelations between these scales were similar to correlations found for the original scales [35]: MAAS with Accept Without Judgment r = 0.48 at baseline and r = 0.62 at follow-up (both p < 0.001), MAAS with Observe r = 0.13 (p > 0.10) and r = 0.32 (p = 0.014), and Accept Without Judgment with Observe r = 0.07 and r = 0.09 (both p > 0.10), respectively.
Daily Practice
At each intervention session, participants were asked how many times they practiced at home according to the instructions during the past week.
Intervention and Procedure
At baseline, before the intervention, all participants completed all questionnaires at their homes. After randomization into the intervention and the waiting-list control group, the intervention group started the MBSR training at a meditation center in Tilburg. The current intervention completely followed the standard MBSR protocol as developed by Kabat-Zinn [1]. The training consisted of eight weekly group (15 persons) sessions with a duration of 150 min. In the sixth week, an additional session of practice in silence with a duration of 6 h was included. The intervention consisted of three primary components: (1) theoretical material related to relaxation, meditation, and body–mind connections; (2) experiential practice of meditation and yoga both during group meetings and at home on a daily basis, and (3) a group process focused on problem solving related to impediments to effective practice, day-to-day applications of mindfulness, and supportive interaction. In addition, a booklet was provided containing information relevant to each week’s instruction. Participants were instructed to practice daily for at least 40 min.
After 8 weeks at the end of the training, both participants in the MBSR group and those in the waiting-list control group were asked again to complete the questionnaire set assessing mindfulness, psychological well-being, and quality of life (follow-up). Hereafter, the control group also received the MBSR training.
Statistical Analysis
Missing values of participants were imputed using the last-observation-carried-forward method [36]. All analyses were according to the conservative intention-to-treat approach.
First, we examined if there were significant differences between the intervention and the control group regarding background characteristics: sex, age, education, job status, and the use of psychotropics. Education was dichotomized into high (degree from high professional education or college) and low education. A chi-square test for independence was performed on the variables sex, education, and the use of psychotropics, while for age, an independent sample t test was conducted.
Multivariate repeated measures analyses of covariance (MANCOVAs) including the questionnaire scores at baseline and follow-up as dependent variables were performed to test the effects of the intervention. Three analyses were performed for the three sets of variables: psychological well-being (perceived stress, vital exhaustion, positive, and negative affect), quality of life (including the five domains), and mindfulness (the three mindfulness scales). The factors in these analyses were group (intervention or control), time (baseline and follow-up), and potential categorical variables to correct for, while potentially confounding continuous variables were entered as covariates.
Bivariate correlations based on all participants were computed between change in mindfulness scores and change in well-being and quality of life. Mediation analyses were based on the approach of Baron and Kenny [37]. The following conditions have to be met for a test of potential mediation effects by mindfulness: (a) The independent variable (group) has a significant effect on the outcome variables, (b) the independent variable (group) has a significant effect on the mediator (mindfulness skills), and (c) the mediator is associated with the outcome variables. If all of these conditions are met, a final analysis involves a mutivariable model including both the independent variable and the mediator predicting change in the outcome variable. In this analysis, a drop of predictive power of the independent variable (group) suggests the existence of a mediation effect. Because we had a repeated measures design, we applied the repeated measures MANCOVA also to the test of the mediation effect. This approach is fundamentally equivalent to a series of regression analyses, as MANCOVA includes regression models.
Results
Participants Flow
After randomization of the 60 individuals, one man that was randomized into the control group declined participation (loss of interest), leaving a total of 59 participants. Two other persons (one women from the intervention group and one man from the control group) did not provide complete baseline questionnaires and could therefore not be included in the analyses.
Seven out of 29 participants (24%) in the intervention group dropped out before the end of the intervention. They attended between zero and five sessions (median = 3). No differences were found between these participants and those who completed the intervention on any of the measured variables (all p > 0.10). Five of the dropouts did complete follow-up questionnaires, leaving missing values of only two individuals. Their values were imputed using the last-observation-carried-forward method [36]. All analyses were according to the intention-to-treat approach. There were no adverse events.
Baseline Characteristics and Randomization Check
The final total group consisted of 38 women and 19 men, with a mean age of 46.0 years (SD = 9.89). Twenty-nine participants (50.9%) had a degree from high professional education or college (high education), 27 people (47.4%) had a job for at least 20 h per week, and 17 individuals (29.8%) were on psychotropics (mainly antidepressants). There were no significant differences between the intervention and control group regarding sex (χ 2(1) = 0.43, p > 0.10), age (t(56) = 0.17, p > 0.10), education (χ 2(1) = 2.13, p > 0.10), job status (χ 2(3) = 3.21, p > 0.10), or the use of psychotropics (χ 2(1) = 0.14, p > 0.10).
Baseline scores of perceived stress (Table 1) were very similar to those obtained in another study on MBSR in distressed adult individuals [7] and even somewhat higher than those obtained in a MBSR intervention study conducted in HIV-positive people [38]. Quality of life scores from all domains (Table 2) were lower compared to those obtained from healthy adult norm groups [39]. General mindfulness as measured by the MAAS was somewhat lower compared to groups of Canadian cancer patients who received MBSR [20, 40], while Observe and Accept Without Judgment scores (Table 3) were similar to the values obtained in American student samples [35]. None of these variables differed between the two groups at baseline (t(56) < 1.68, p > 0.10).
Table 1.
Means (and standard deviations) of distress and well-being scores at baseline and follow-up for the MBSR and control groups
| MBSR | Control | F(1,54) (p value) | Effect size d diff | |||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||
| Perceived stress | 32.44 (6.46) | 25.39 (7.54) | 31.37 (6.46) | 28.10 (7.51) | 6.17 (0.016) | 0.64 |
| Vital exhaustion | 27.74 (8.02) | 18.51 (9.75) | 27.27 (7.99) | 25.34 (9.79) | 13.72 (0.001) | 0.91 |
| Positive affect | 14.18 (7.05) | 18.96 (6.84) | 16.38 (7.04) | 16.90 (6.83) | 8.23 (0.006) | 0.73 |
| Negative affect | 20.49 (8.67) | 14.68 (9.21) | 20.39 (8.69) | 17.13 (9.21) | 1.77 (0.189) | 0.36 |
MBSR mindfulness-based stress reduction intervention, d diff effect size d of the difference between the groups regarding pre to post difference scores
Table 2.
Means (and standard deviations) of quality of life (QoL) scores at baseline and follow-up for the MBSR and control groups
| MBSR | Control | F (1,53) (p value) | Effect size d diff | |||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||
| General QoL | 2.98 (0.69) | 3.37 (0.63) | 2.97 (0.69) | 3.07 (0.63) | 2.77 (0.102) | 0.31 |
| Environmental QoL | 13.83 (1.96) | 14.47 (1.85) | 13.70 (1.96) | 13.85 (1.85) | 1.85 (0.180) | 0.18 |
| Physical QoL | 12.20 (2.28) | 13.64 (2.06) | 12.06 (2.33) | 12.91 (2.12) | 1.84 (0.181) | 0.19 |
| Psychological QoL | 11.72 (2.01) | 12.85 (2.17) | 11.57 (2.06) | 12.07 (2.22) | 2.66 (0.109) | 0.21 |
| Social QoL | 11.62 (3.17) | 12.94 (3.39) | 11.49 (3.23) | 12.22 (3.44) | 1.67 (0.203) | 0.13 |
MBSR mindfulness-based stress reduction intervention, d diff effect size d of the difference between the groups regarding pre to post difference scores
Table 3.
Means (and standard deviations) of mindfulness scores at baseline and follow-up for the MBSR and control groups
| MBSR | Control | F (1,53) (p value) | Effect size d diff | |||
|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | |||
| General Mindfulness | 3.38 (0.69) | 3.66 (0.63) | 3.41 (0.68) | 3.37 (0.62) | 4.99 (0.030) | 0.55 |
| Accept Without Judgment | 26.44 (7.57) | 30.79 (7.14) | 26.93 (7.27) | 28.35 (6.86) | 3.64 (0.062) | 0.44 |
| Observe | 41.25 (10.27) | 43.43 (9.37) | 43.21 (9.82) | 41.77 (8.99) | 7.17 (0.010) | 0.69 |
MBSR mindfulness-based stress reduction intervention, d diff effect size d of the difference between the groups regarding pre to post difference scores
Psychological Distress and Well-being
The first repeated measures MANCOVA involving baseline and follow-up scores was an omnibus test of the four measures of psychological distress: perceived stress, vital exhaustion, negative affect, and the reversed score on positive affect. A significant main effect of time [F(1,54) = 50.31, p < 0.001, partial η 2 = 0.48] showed that psychological distress decreased from baseline to follow-up for both groups. In addition, a significant interaction of time × group emerged [F (1,54) = 12.12, p = 0.001, partial η 2 = 0.18], showing that the intervention group experienced a larger reduction of distress than the control group. Of the potentially confounding variables, only education showed a significant main effect [F(1,54) = 11.75, p = 0.001, partial η 2 = 0.18]. Across both time measurements, the more highly educated people showed lower distress scores than their less-educated counterparts. No other effects were significant, such as main effects of group, age, sex, and the use of psychotropics, or interactions between the various factors.
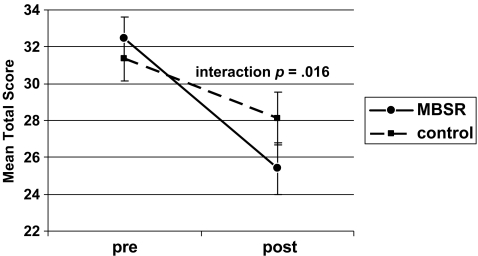
Univariate tests showed different effect sizes for the adjusted differences between the two groups (Table 1): d diff = 0.64 for perceived stress [F(1,54) = 6.17, p = 0.016; Fig. 1], d diff = 0.91 for vital exhaustion [F(1,54) = 13.72, p = 0.001], d diff = 0.36 for negative affect [F(1,54) = 1.77, p > 0.10], and d diff = 0.73 for positive affect [F (1,54) = 8.23, p = 0.006].
Fig. 1.
Change in perceived stress from pre- to post-treatment for the mindfulness-based stress reduction (MBSR) intervention (N = 29) and waiting-list control (N = 28) groups
Quality of Life
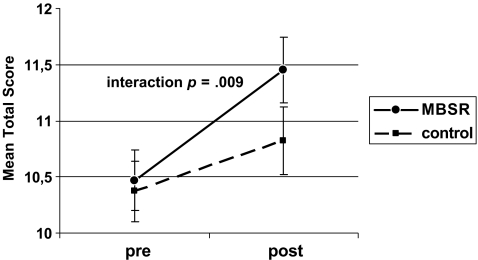
The second repeated measures MANCOVA showed significant effects for time [F(1,53) = 18.08, p < 0.001, partial η 2 = 0.25] and for the time × group interaction [F(1,53) = 7.27, p = 0.009, partial η 2 = 0.12]. Quality of life increased from baseline to follow-up, with the intervention group showing a larger increase than the control group (Fig. 2). Other significant effects emerged for education [F(1,53) = 22.29, p < 0.001, partial η 2 = 0.30], again showing more favorable scores across both time points for the more highly educated and for the time × age interaction [F(1,53) = 8.22, p = 0.006, partial η 2 = 0.13]. This effect reflected a sharper rise in quality of life with younger age across both groups. No other effects were significant.
Fig. 2.
Change in quality of life from pre- to post-treatment for the mindfulness-based stress reduction (MBSR) intervention (N = 29) and waiting-list control (N = 28) groups
Although the omnibus test showed a significant effect on quality of life, the univariate differences between the groups on the various subscales were rather small, ranging from d diff = 0.13 for the social domain of quality of life [F(1,53) = 1.67, p = 0.20] to d diff = 0.31 for general quality of life [F(1,53) = 2.77, p = 0.10; Table 2]. These small differences between the groups are due to the fact that both groups increased on quality of life over the course of time, with an average effect size of d = 0.49.
Mindfulness
In the repeated measures MANCOVA involving all three subscales measuring mindfulness, the effects of time [F(1,53) = 13.72, p = 0.001, partial η 2 = 0.21] and the interaction of time × group [F(1,53) = 13.54, p = 0.001, partial η 2 = 0.21] both emerged. The mindfulness scores increased between the baseline and the post-treatment, and this increase was larger in the intervention group. In addition, a time × age × subscale interaction emerged [F(2,52) = 5.89, p = 0.01, partial η 2 = 0.17), which could be interpreted as a sharper increase in mindfulness across both groups among younger participants shown by two of the three subscales: Accept Without Judgment and Observe.
The univariate differences between the intervention group and the control group were similar for the three mindfulness skills scales: d diff = 0.55 for general mindfulness as measured by the MAAS [F(1,53) = 4.99, p = 0.030], d diff = 0.44 for Accept Without Judgment [F(1,53) = 3.64, p = 0.062], and d diff = 0.69 for Observe [F(1,53) = 7.17, p = 0.010; Table 3].
Associations with Change
Because the omnibus test of the repeated measures MANCOVA on quality of life revealed an intervention effect on overall quality of life based on all subscales together but not on the separate subscales, we also included overall quality of life derived from the omnibus multivariate analysis in the subsequent analyses. This score is equivalent to the mean of the standardized scores on the five subscales.
Across both groups, sex, education, and the use of psychotropics were not associated with changes in outcome variables. Age did not correlate with change in the psychological distress and well-being variables, but older age was associated with smaller increases in physical, environmental, and overall quality of life (−0.34 ≤ r ≤ −0.26, p < 0.05). Higher baseline scores of positive affect and general, physical, and environmental quality of life were associated with smaller increases over time, ranging from r = −0.31, p = 0.017 for environmental quality of life to r = −0.48, p < 0.001, for general quality of life. In addition, higher initial negative affect was associated with larger decreases in negative affect (r = 0.33, p = 0.011), while no such associations were found for perceived stress or vital exhaustion.
Increase in general mindfulness, as measured by MAAS, correlated significantly with decreases in perceived stress (r = 0.28, p = 0.033), vital exhaustion (r = 0.57, p < 0.001), and negative affect (r = 0.30, p = 0.022), as well as with increases in physical, psychological, and overall quality of life (0.39 ≤ r ≤ 0.45, p < 0.004; Table 4). Accept Without Judgment correlated significantly only with increases in environmental, physical, psychological, and overall quality of life (0.31 ≤ r ≤ 0.41, p < 0.02). Changes in the Observe subscale did not show any significant correlations with changes in the outcome variables; only a trend for an association with a larger decrease in perceived stress appeared (r = 0.23, p = 0.08). When age and the baseline values of the outcome variables were included in partial correlations, the associations between changes in mindfulness and changes in outcome variables still were significant, except the association between Accept Without Judgment and physical quality of life (r = 0.19, p = 0.16).
Table 4.
Correlations between change in mindfulness scores and favorable change in outcome variables from baseline to follow-up across groups
| Δ General mindfulness | Δ Accept without judgment | Δ Observe | |
|---|---|---|---|
| Δ Perceived stress | 0.28* | 0.23# | |
| Δ Vital exhaustion | 0.57*** | 0.22 | |
| Δ Negative affect | 0.30* | ||
| Δ Positive affect | 0.22 | 0.20 | |
| Δ General QoL | |||
| Δ Environmental QoL | 0.41** | ||
| Δ Physical QoL | 0.39** | 0.31* | |
| Δ Psychological QoL | 0.45*** | 0.34** | |
| Δ Social QoL | |||
| Δ Overall QoL | 0.41** | 0.41** |
Only correlations of r > 0.20 are shown.
Δ favorable change from pre- to post-experimental period, QoL quality of life, overall QoL=total quality of life based on the mean of the standardized scores of all five subscales
*p < 0.05, **p < 0.01, ***p < 0.001, #0.05 < p < 0.10
Regarding weekly formal home practice, participants in the intervention group practiced on average 4.32 (SD = 1.27) times per week the whole practice (a shorter practice period was counted proportionally to the whole period). However, no associations were found between the amount of weekly practice and change in any of the outcome variables. Participants in the intervention group who attended the first session (two did not show up) further attended between one (one person) and all eight sessions (ten participants) with an average of 6.48 sessions (SD = 1.87). Also, the number of sessions attended did not correlate with the change in outcome variables, except for a trend for a larger increase in positive affect (r = 0.32, p = 0.09).
Mediation by Mindfulness
The previous analyses revealed that all conditions were met for a test of potential mediation effects by mindfulness: (a) The independent variable (group) had a significant effect on several outcome variables (see Tables 1 and 2), (b) the independent variable (group) had a significant effect on the potential mediators (change in mindfulness skills; see Table 3), and (c) in several cases, the potential mediator was associated with change in outcome (Table 4) [37]. All these conditions were met in the case of perceived stress and vital exhaustion with general mindfulness as a potential mediator and, in the case of the omnibus test-derived overall quality of life with general mindfulness and accept without judgment as potential mediators.
The final analysis testing the mediation effect of general mindfulness on perceived stress included both the independent variable (group) and the potential mediator (change in general mindfulness) as predictors in the ANCOVA. Except for the inclusion of the potential mediator as covariate, this analysis was identical to the original ANCOVA described above. In contrast to the results of the original analysis, in this final analysis the time × group interaction failed to reach significance [F(1,53) = 3.58, p = 0.064, partial η 2 = 0.06], suggesting that the effect of the intervention may have been mediated by a change in general mindfulness [37]. A similar analysis on vital exhaustion revealed a still significant effect of time × group [F(1,53) = 6.91, p = 0.011, partial η 2 = 0.12), albeit considerably smaller than in the original unmediated analysis (partial η 2 = 0.20).
Regarding the omnibus test-derived index of overall quality of life, the MANCOVA including general mindfulness as potential mediator reduced the previously significant time × group interaction effect to nonsignificance [F(1,52) = 2.73, p = 0.10, partial η 2 = 0.05). However, when accept without judgment was included as a predictor instead of general mindfulness, the time × group interaction remained significant [F(1,52) = 4.20, p = 0.045, partial η 2 = 0.08].
Discussion
Our main aim was to examine whether the expected beneficial effects of a mindfulness-based stress-reduction intervention (MBSR) (1) are attributable to actual changes in mindfulness skills.
First, it had to be shown that MBSR had the hypothesized effects in our sample of distressed individuals from the general population. We did replicate previous findings regarding the effectiveness of MBSR on decrease of feelings of distress [9, 10, 12] and increase of quality of life [11, 20, 21], and extended previous results to other measures of distress (vital exhaustion), mood, and quality of life than those applied earlier. The general convergence of findings underscores the fact that previous results are not limited to the specific measures used. Some nuances should be acknowledged, however. In our study, quality of life seems less sensitive to change than measures of psychological distress and positive affect. This is in line with research on temporal changes in quality of life in patient populations, indicating fairly stable levels [41]. In addition, decrease in negative affect showed no difference between the groups, probably because the control group decreased significantly as well. This may have been due either to natural improvement in mood over the course of time, to the expectancy of the participants of coming improvement as the intervention would start soon, or even just to the statistical effect of regression to the mean.
Regarding the main aim of our investigation, support was obtained for at least a partial mediation effect by mindfulness. This is the first study to show such an effect in a controlled study. Only few previous investigations have examined a mediation effect by mindfulness skills. While several studies reported correlations between change in mindfulness skills and decrease in feelings of distress [20, 27], a mediation effect of mindfulness could not be obtained due to the lack of a control group. The only study on the mediation issue that did apply a randomized controlled design did not find a correlation between change in mindfulness skills and change in outcome variables [42]. However, this was probably due to the fact that their sample consisted of students without any psychological symptoms. Perhaps because of our use of a truly distressed sample in a randomized study, we have been able to demonstrate an at least partial mediation effect of mindfulness in the case of some outcome variables.
We found evidence for a mediation effect of general mindfulness in the case of perceived stress, quality of life, and partially on vital exhaustion. For the facet accepting without judgment and observing mainly sensory phenomena, no mediation effects were found, although change in accepting without judgment did correlate with improvement in quality of life over time. A potential explanation of these findings may be that the focus of the intervention is on enhancing mindfulness in general, which is more strongly tapped by the MAAS, than on the specific aspects of accepting ones feelings and thoughts, and observing bodily and physical sensations, although these aspect are also addressed during the intervention.
Regarding relationships between outcome and home practice or attendance of sessions, we found no effects. The results concerning attendance are in line with three out of five studies that have examined this effect and found none [11, 23, 43]. Two other studies did report a positive effect of attendance on outcome [10, 44]. Ceiling or floor effects cannot explain this inconsistency as the number of attended sessions ranged from relatively low [43] to high [11]. Also the power to detect effects did not differ systematically between the studies. One may speculate that practice is more important for achieving positive effects than session attendance, which however, we did not observe either.
Previous studies on mindfulness-related interventions have reported mixed results regarding the relation between the amount of home practice and outcome. Clear consistent associations have been obtained in some studies [10, 27, 45], while in most studies, no or inconsistent associations were found [9, 11, 13, 17, 23, 43, 46, 47]. Some but not all null findings may have been due to either relatively low initial levels of distress [11] or ceiling effects of the amount of practice [11, 47]. However, studies reporting significant associations were based on larger samples (61 ≤ N ≤ 121 in the treatment group) than studies finding no or inconsistent associations (14 ≤ N ≤ 59), suggesting a power problem in many studies, including ours, to detect an effect of probably modest magnitude. Although it cannot be ruled out, a more fine-grained assessment of the amount of minutes spent in practice may not have produced stronger associations in our study, as most studies finding no or inconsistent associations did assess the number of minutes practicing.
One limitation of the present investigation is the relatively small sample size, which prevents the detection of small effects. Importantly, our results are restricted to immediate effects post-intervention. The investigation of potentially mediating effects of mindfulness skills on long-term outcome is very much needed. Furthermore, although we attempted for neutral wording in our advertisements, emphasizing the stress reduction aspect, our recruitment procedure by means of advertisements may have partially attracted a subset of people interested in this form of intervention, limiting the generalizability to the general population.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. New York: Delacourt; 1990. [Google Scholar]
- 2.Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen Hosp Psych. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- 3.Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosom Med. 2002;64:71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- 5.Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, Segal ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. J Consult Clin Psychol. 2002;70:275–287. doi: 10.1037/0022-006X.70.2.275. [DOI] [PubMed] [Google Scholar]
- 6.Thera N. The Power of Mindfulness. San Francisco, CA: Unity; 1972. [Google Scholar]
- 7.Chang VY, Palesh O, Caldwell R, et al. The effects of a mindfulness-based stress reduction program on stress, mindfulness self-efficacy, and positive states of mind. Stress Health. 2004;20:141–147. doi: 10.1002/smi.1011. [DOI] [Google Scholar]
- 8.Reibel DK, Greeson JM, Brainard GC, Rosenzweig S. Mindfulness-based stress reduction and health-related quality of life in a heterogeneous patient population. Gen Hosp Psych. 2001;23:183–192. doi: 10.1016/S0163-8343(01)00149-9. [DOI] [PubMed] [Google Scholar]
- 9.Astin JA. Stress reduction through mindfulness meditation. Effects on psychological symptomatology, sense of control, and spiritual experiences. Psychother Psychosom. 1997;66:97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- 10.Speca M, Carlson LE, Goodey E, Angen M. A randomized, wait-list controlled clinical trial: the effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosom Med. 2000;62:613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress, and immune parameters in breast and prostate cancer outpatients. Psychosom Med. 2003;65:571–581. doi: 10.1097/01.PSY.0000074003.35911.41. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro SL, Astin JA, Bishop SR, Cordova M. Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int J Stress Manag. 2005;12:164–176. doi: 10.1037/1072-5245.12.2.164. [DOI] [Google Scholar]
- 13.Jain S, Shapiro SL, Swanick S, et al. A randomized controlled trial of mindfulness meditation versus relaxation training: effects on distress, positive states of mind, rumination, and distraction. Annals Behav Med. 2007;33:11–21. doi: 10.1207/s15324796abm3301_2. [DOI] [PubMed] [Google Scholar]
- 14.Kabat-Zinn J, Massion AO, Kristeller J, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. Am J Psychiatr. 1992;149:936–943. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- 15.Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med. 1998;21:581–599. doi: 10.1023/A:1018700829825. [DOI] [PubMed] [Google Scholar]
- 16.Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med. 2005;12:278–285. doi: 10.1207/s15327558ijbm1204_9. [DOI] [PubMed] [Google Scholar]
- 17.Shapiro SL, Bootzin RR, Figueredo AJ, Lopez AM, Schwartz GE. The efficacy of mindfulness-based stress reduction in the treatment of sleep disturbance in women with breast cancer: an exploratory study. J Psychosom Res. 2003;54:85–91. doi: 10.1016/S0022-3999(02)00546-9. [DOI] [PubMed] [Google Scholar]
- 18.Kabat-Zinn J, Lipworth L, Burney R. The clinical use of mindfulness meditation for the self-regulation of chronic pain. J Behav Med. 1985;8:163–190. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- 19.Astin JA, Berman BM, Bausell B, Lee WL, Hochberg M, Forys KL. The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. J Rheumatol. 2003;30:2257–2262. [PubMed] [Google Scholar]
- 20.Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol. 2003;84:822–848. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- 21.Roth B, Robbins D. Mindfulness-based stress reduction and health-related quality of life: findings from a bilingual inner-city patient population. Psychosom Med. 2004;66:113–123. doi: 10.1097/01.PSY.0000097337.00754.09. [DOI] [PubMed] [Google Scholar]
- 22.Toneatto T, Nguyen L. Does mindfulness meditation improve anxiety and mood symptoms? A review of the controlled research. Can J Psychiatry. 2007;52:260–266. doi: 10.1177/070674370705200409. [DOI] [PubMed] [Google Scholar]
- 23.Sephton SE, Salmon P, Weissbecker I, et al. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis Rheum. 2007;57:77–85. doi: 10.1002/art.22478. [DOI] [PubMed] [Google Scholar]
- 24.Tacon AM, McComb J, Caldera Y, Randolph P. Mindfulness meditation, anxiety reduction, and heart disease: a pilot study. Fam Commun Health. 2003;26:25–33. doi: 10.1097/00003727-200301000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Ott MJ, Norris RL, Bauer-Wu SM. Mindfulness meditation for oncology patients: a discussion and critical review. Integrativ Cancer Therapies. 2006;5:98–108. doi: 10.1177/1534735406288083. [DOI] [PubMed] [Google Scholar]
- 26.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 27.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J Behav Med. (in press). [DOI] [PubMed]
- 28.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Tyrrell DA, Smith AP. Negative life events, perceived stress, negative affect, and susceptibility to the common cold. J Pers Soc Psychol. 1993;64:131–140. doi: 10.1037/0022-3514.64.1.131. [DOI] [PubMed] [Google Scholar]
- 30.Appels A, Mulder P. Fatigue and heart disease. The association between ‘vital exhaustion’ and past, present and future coronary heart disease. J Psychosom Res. 1989;33:727–738. doi: 10.1016/0022-3999(89)90088-3. [DOI] [PubMed] [Google Scholar]
- 31.van Diest R. Subjective sleep characteristics as coronary risk factors, their association with type A behaviour and vital exhaustion. J Psychosom Res. 1990;34:415–426. doi: 10.1016/0022-3999(90)90065-C. [DOI] [PubMed] [Google Scholar]
- 32.Meesters C, Appels A. An interview to measure vital exhaustion. I. Development and comparison with the Maastricht Questionnaire. Psychol Health. 1996;11:557–571. doi: 10.1080/08870449608401989. [DOI] [Google Scholar]
- 33.Denollet J. Emotional distress and fatigue in coronary heart disease: the Global Mood Scale (GMS) Psychol Med. 1993;23:111–121. doi: 10.1017/s0033291700038903. [DOI] [PubMed] [Google Scholar]
- 34.WHOQOL Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychol Med. 1998;28:551–558. doi: 10.1017/S0033291798006667. [DOI] [PubMed] [Google Scholar]
- 35.Baer RA, Smith GT, Allen KB. Assessment of mindfulness by self-report: the Kentucky inventory of mindfulness skills. Assessment. 2004;11:191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- 36.Judd LL, Rapaport MH, Yonkers KA, et al. Randomized, placebo-controlled trial of fluoxetine for acute treatment of minor depressive disorder. Am J Psychiatr. 2004;161:1864–1871. doi: 10.1176/appi.ajp.161.10.1864. [DOI] [PubMed] [Google Scholar]
- 37.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 38.Robinson FP, Mathews HL, Witek-Janusek L. Psycho-endocrine-immune response to mindfulness-based stress reduction in individuals infected with the human immunodeficiency virus: a quasiexperimental study. J Altern Complement Med. 2003;9:683–694. doi: 10.1089/107555303322524535. [DOI] [PubMed] [Google Scholar]
- 39.De Vries J, Van Heck GL. Nederlandse handleiding van de WHOQoL [Dutch manual of the WHOQoL] Tilburg: Tilburg University; 2000. [Google Scholar]
- 40.Carlson LE, Brown KW. Validation of the mindful attention awareness scale in a cancer population. J Psychosom Res. 2005;58:29–33. doi: 10.1016/j.jpsychores.2004.04.366. [DOI] [PubMed] [Google Scholar]
- 41.Hanestad BR, Albrektsen G. The stability of quality of life experience in people with type 1 diabetes over a period of a year. J Adv Nurs. 1992;17:777–784. doi: 10.1111/j.1365-2648.1992.tb01998.x. [DOI] [PubMed] [Google Scholar]
- 42.Kingston J, Chadwick P, Meron D, Skinner TC. A pilot randomized control trial investigating the effect of mindfulness practice on pain tolerance, psychological well-being, and physiological activity. J Psychosom Res. 2007;62:297–300. doi: 10.1016/j.jpsychores.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 43.Ramel W, Goldin PR, Carmona PE, McQuaid JR. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cogn Ther Res. 2004;28:433–455. doi: 10.1023/B:COTR.0000045557.15923.96. [DOI] [Google Scholar]
- 44.Weissbecker I, Salmon P, Studts JL, Floyd AR, Dedert EA, Sephton SE. Mindfulness-based stress reduction and sense of coherence among women with fibromyalgia. J Clin Psychol Med Settings. 2002;9:297–307. doi: 10.1023/A:1020786917988. [DOI] [Google Scholar]
- 45.Carlson LE, Ursuliak Z, Goodey E, Angen M, Speca M. The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Support Care Cancer. 2001;9:112–123. doi: 10.1007/s005200000206. [DOI] [PubMed] [Google Scholar]
- 46.Davidson RJ, Kabat-Zinn J, Schumacher J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosom Med. 2003;65:564–570. doi: 10.1097/01.PSY.0000077505.67574.E3. [DOI] [PubMed] [Google Scholar]
- 47.Ostafin BD, Chawla N, Bowen S, Dillworth TM, Witkiewitz K, Marlatt GA. Intensive mindfulness training and the reduction of psychological distress: a preliminary study. Cogn Behav Pract. 2006;13:191–197. doi: 10.1016/j.cbpra.2005.12.001. [DOI] [Google Scholar]